Professional Documents
Culture Documents
Community Acquired Pneumonia PDF
Uploaded by
chris_arc90Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Community Acquired Pneumonia PDF
Uploaded by
chris_arc90Copyright:
Available Formats
Community Acquired Pneumonia
Community Acquired Pneumonia –
Community acquired pneumonia (CAP) is an acute lower respiratory tract infection in a person who has not been admitted to hospital or a health
care facility in the previous 14 days for 48 hours or more. Residents of residential aged care facilities (RACF) acquire a variant of community
acquired pneumonia. Estimates indicate that approximately 2 in 1000 people in the adult population are diagnosed with CAP, and it accounts for
approximately 2% of all overnight hospital admissions. Residents of RACFs have a risk of acquiring CAP 10 times more than community living
adults, and admissions to hospital at a rate of 30 times more often. CAP accounts for 1/3 – 1/2 of all deaths in RACFs and is responsible for
increased rates in re-hospitalisation, mortality and morbidity.
Streptococcus pneumoniae is the commonest cause of CAP in RACFs Gram negative bacilli, Staphylococcus aureus and respiratory viruses are
predominant, whereas legionella, chlamydia and mycoplasma are uncommon pathogens.
The expected outcome of use of this protocol is rapid and effective relief from symptoms, improve/prevent respiratory distress, prevent
complications, eradicate infection in the respiratory tract, prevention of reoccurrence of infection, prevention of unnecessary hospitalisation, improve
morbidity and decrease the risk and rate of mortality. Alternatively, this clinical guideline may provide guidance in assisting with symptom relief in a
palliative care context for residents with severe complications. May include aspiration pneumonia or palliative care context.
Community Acquired Pneumonia.doc Page 1 of 16 Created on 7/11/2012 1:20:00 PM
Community Acquired Pneumonia
SCOPE OF PRACTICE
PRACTITIONER SCOPE OUTCOMES
Nurse Practitioner – • The expected outcome of use of this clinical
Aged Care guideline is effective relief from symptoms and
eradication of infection from the respiratory
tract, prevention of reoccurrence of infection,
reduction in hospitalisation rates, reduced
mortality or morbidity.
• Improve process of care variables and clinical
outcomes .
Medical Practitioner ± Nurse The NP will refer all Hall & Prior residents outside • Upon failure of treatment, complications of
Practitioner their scope of practice, to a medical practitioner. infection or recurrence of infection, referral to
a GP is required. Nurse practitioners should
consider referral to physiotherapy and a care
plan for nursing staff should be developed
incorporating management plan.
Community Acquired Pneumonia.doc Page 2 of 16 Created on 7/11/2012 1:20:00 PM
Community Acquired Pneumonia
RESIDENT’S ASSESSMENT
RESIDENT’S SCOPE OUTCOMES
HISTORY
Presenting symptoms Signs and symptoms of CAP: fever, rigors, flushed, • Gaining comprehensive and holistic data in
new-onset cough, change in sputum colour (if cough order to prescribe appropriate diagnostics and
chronic), chest discomfort, dyspnoea, confusion, sore interventions related to indicators identified in
throat, head cold symptoms, lethargy,3 elevated assessment.
temperature and heart rate, increased respiratory
rate, decreased oxygen saturation, respiratory • Constructing and ruling out related differential
distress, dullness on percussion (if consolidation diagnoses to specific pathophysiology
present), decreased air entry, inspiratory crackles, identified.
wheeze, bronchial breath sounds and pleural rub
(rare). C riteria/Confusion.Uremia.Respiratory Rate • Prevent interactions and further complications
.Blood Pressure . with interventions
Known risk factors for the Dysphagia, decreased physical & cognitive function,
presenting symptoms immunosupression, delirium, • Referrals will be considered in collaboration
malnutrition,COPD,asthma. with resident’s GP.
Previous medical history Relevant medical, surgical and obstetric history
Medications Current Medications
Other relevant information Allergies, previous respiratory tract infection history,
nutrition & hydration, mobility, cognition, behaviour
Community Acquired Pneumonia.doc Page 3 of 16 Created on 7/11/2012 1:20:00 PM
Community Acquired Pneumonia
PHYSICAL Ax SCOPE OUTCOMES
Usual physical examination Record findings: vital signs, respiratory assessment, • Correct diagnosis, provision of effective
cardiovascular assessment, pain assessment disease and symptomatic eradication/relief
INVESTIGATIONS
INDICATIONS INVESTIGATIONS OUTCOMES
Routine investigations Laboratory/diagnostics used in diagnosis and • Results from all investigations will be used
identification of organism: chest x-ray to identify when determining future management of the
diagnosis and consolidation in lungs and aid in resident’s.
diagnosis, pulse oximetry, sputum MCS to identify
pathogen and it’s sensitivities, blood chemistry and • Accurate diagnosis will be determined .
haematology (FBE, U & E, glucose) to help assist
defining severity and complications associated with • Refer to GP on result of investigation
CAP.
Pathology • Correct pharmacotherapy will be prescribed
To determine pathogen, Sputum MCS, based on sensitivity of organism.
severity & sensitivity of
organism.
Imaging
To determine location, extent Chest x-ray
and severity of infection
Haematology / Biochemistry
To confirm diagnosis & to FBC, U&E.
assist in determining severity
of infection
Community Acquired Pneumonia.doc Page 4 of 16 Created on 7/11/2012 1:20:00 PM
Community Acquired Pneumonia
SCOPE
INDICATIONS INVESTIGATIONS OUTCOMES
FOLLOW UP AND EDUCATION
INTERVENTION INFORMATION OUTCOMES
Pharmacotherapeutics Treatment of CAP involves pharmacological & non- • Eradication of infection
pharmacological treatment. Management of CAP • Prevention of recurrence of infection
involves antibiotic therapy, oxygen, analgesia, • Symptomatic relief
antipyretics & supportive nursing care & monitoring.
Antibiotic therapy is determined by determining the
causative pathogen and sensitivity.
Non-pharmacological Non-pharmacological, supportive nursing and
monitoring interventions include: regular observation
of vitals’ status (RR, HR, BP, SpO2, T ۫C), bed rest,
adequate hydration and nutrition, continuous oxygen
therapy, improving airway (i.e.posture, humidification,
suctioning, deep breathing & coughing exercises) and
assistance with activities of daily living.
Community Acquired Pneumonia
Community Acquired Pneumonia.doc Page 5 of 16 Created on 7/11/2012 1:20:00 PM
FOLLOW UP AND EDUCATION
INTERVENTION INFORMATION OUTCOMES
Follow up appointments Resident’s needs to be reviewed daily post • Underlying disease will be detected at follow
commencing antibiotic therapy to reassess symptoms up.
and monitor for any complications or adverse
reactions to therapy. A follow up consultation is • Upon failure of treatment, complications of
required 10 days post therapy for review of signs and infection or recurrence of infection, referral to a
symptoms and repeat sputum MCS approximately 10 medical specialist is required.1 Referral to an
days post completion date of antibiotic therapy is occupational therapist and/or physiotherapist
required to validate eradication of infection and should be considered if lack of mobility is a
determine if further antimicrobial treatment is contributing factor.
required.
Nurse practitioners are required to follow up on all • Consider referral to a speech pathologist if
referrals they made to allied health and medical dysphagia an issue.
specialists, provide and/or reinforce relevant
education regarding immunisation.
Letters Letter to residents GP Review of resident notes
Community Acquired Pneumonia.doc Page 6 of 16 Created on 7/11/2012 1:20:00 PM
Community Acquired Pneumonia -
PHARMACOTHERAPY
Treatment of CAP involves pharmacological and non-pharmacological treatment. Management of CAP involves antibiotic therapy, oxygen,
analgesia, antipyretics and supportive nursing care and monitoring.
Antibiotic therapy is determined by what the causative pathogen is, the pathogen’s sensitivities and resistance and the severity of the individual’s
clinical presentation and/or PSI. Note that the PSI is only a guide and nurse practitioners should consider clinical and social contexts.5
Antibiotic therapy –
First line treatment
amoxycillin 1g PO 8 hourly
and
roxithromycin 300mg PO daily
or
doxycycline 200mg initial dose then 100mg PO daily
Community Acquired Pneumonia.doc Page 7 of 16 Created on 7/11/2012 1:20:00 PM
Community Acquired Pneumonia -
PHARMACOTHERAPY
Non-tropical region Tropical region
benzylpenicillin 1.2g IV 6 hourly gentamicin 4-6mg/kg IV daily
or and
amoxy/ampicillin 1g IV 6 hourly ceftriaxone 2g IV daily
and
roxithromycin 300mg PO daily
or
doxycycline 200mg/100mg PO daily
and
gentamicin 4-6mg/kg IV daily if gram-
negative bacilli isolated
Community Acquired Pneumonia.doc Page 8 of 16 Created on 7/11/2012 1:20:00 PM
Community Acquired Pneumonia -
PHARMACOTHERAPY
Hypersensitivity to penicillin:
replace penicillin: cefotaxime 1g IV 8 hourly (or ceftriaxone 1g IV daily) until
significant improvement then cefuroxime 500mg PO 12 hourly
Immediate sensitivity to penicillin:
replace penicillin: gatifloxacin 400mg PO daily
or
moxifloxacin 400mg PO daily
or
refer to medical practitioner and transfer to hospital if severe
Community Acquired Pneumonia.doc Page 9 of 16 Created on 7/11/2012 1:20:00 PM
Community Acquired Pneumonia -
PHARMACOTHERAPY
Analgesia and antipyretic
paracetamol 500mg-1g 6 hourly (max. 4g/day) PO/PR
Oxygen therapy
oxygen 6-10 L/min via nasal prongs or Venturi Mask
to maintain oxygen saturation > 97%
Community Acquired Pneumonia -
Community Acquired Pneumonia.doc Page 10 of 16 Created on 7/11/2012 1:20:00 PM
PHARMACOTHERAPY
FORMULARY
amoxycillin trihydrate clarithromycin
Drug (generic name): amoxycillin trihydrate
Poisons schedule: schedule 4 Drug (generic name): roxithromycin
Therapeutic class: 8(a) penicillins Poisons schedule: schedule 4
Dosage range: 250-500mg 8 hourly , In severe infection Therapeutic class: 8(d) macrolides
(pneumonia) 1Gram 8 hourly. Dosage range: 250-500mg
Route: oral Route: oral
Frequency of administration: 8 hourly Frequency of administration: 12hourly
Duration of order: 7 days Duration of order: 7 days
Actions: intervene in cell wall peptidoglycan synthesis, is Actions: binds to 50S ribosomal sub-unit, inhibits bacterial protein
bactericidal synthesis, is bacteriostatic
Indications for use: chronic bronchitis, CAP, acute bacterial otitis Indications for use: upper & lower respiratory tract infections,
media, sinusitis, epididymo-orchitis, acute prostatitis, acute CAP, recurrent tonsillitis, skin infections
pyelonephritis, UTI, gonococcol inf., prophylaxis: endocarditis, Contraindications for use: serious allergy to macrolides,
acute cholecystitis, peritonitis, combination therapy for eradication: Adverse drug reactions: nausea, vomiting, diarrhoea, abdo.
H. pylori pain/cramps, headache, dyspnoea, cough, candidiasis, taste
Contraindications for use: allergy to penicillins, cephalosporins, disturbance.
carbapenems
Adverse drug reactions: nausea, diarrhoea, rash, allergy
Community Acquired Pneumonia.doc Page 11 of 16 Created on 7/11/2012 1:20:00 PM
Community Acquired Pneumonia -
PHARMACOTHERAPY
doxycycline gentamicin (medical practitioner)
Drug (generic name): doxycycline Drug (generic name): gentamicin
Poisons schedule: schedule 4 Poisons schedule: schedule 4
Therapeutic class: 8(c) tetracyclines Therapeutic class: 8(f) aminoglycosides
Dosage range: 100mg-200mg (200mg first dose, followed by Dosage range: 4-6mg/kg
100mg daily) Route: intravenous
Route: oral Frequency of administration: daily or as single dose , depends
Frequency of administration: daily on severity.
Duration of order: 6 days Duration of order: until significant improvement
Actions: reversibly binds to 50S ribosomal sub-unit, inhibits Actions: irreversibly binds to 50S ribosomal sub-unit, inhibits
bacterial protein synthesis, is bacteriostatic bacterial protein synthesis, causes cell membrane damage, is
Indications for use: acne, M. pneumonia, CAP, chronic bactericidal with concentration dependence
bronchitis, sinusitis, non-gonococcol genital tract infections, PID, Indications for use: gram-negative infections (empirical Rx),
rickettsial infections, prostatitis, prophylaxis and treatment of systemic enterococcal infections, surgical & non-surgical
malaria prophylaxis, cystic fibrosis, bronchiectasis
Contraindications for use: children < 8years, allergy to Contraindications for use: serious allergy to aminoglycoside
tetracycline Adverse drug reactions: renal impairment, ototoxicity
Adverse drug reactions: nausea, vomiting, heartburn, tooth
discolouration, enamel dysplasia, reduced bone growth (children),
photosensitivity
Community Acquired Pneumonia.doc Page 12 of 16 Created on 7/11/2012 1:20:00 PM
Community Acquired Pneumonia -
PHARMACOTHERAPY
benzylpenicillin (medical practitioner) amoxy / ampicillin (medical practitioner)
Drug (generic name): benzylpenicillin Drug (generic name): amoxy / ampicillin
Poisons schedule: schedule 4 Poisons schedule: schedule 4
Therapeutic class: 8(a) penicillins Therapeutic class: 8(a) penicillins
Dosage range: 1.2g Dosage range: 1g
Route: intravenous Route: intravenous amoxicillin sodium for IV
Frequency of administration: 6 hourly Frequency of administration: 6 hourly
Duration of order: until significant improvement Duration of order: 5days
Actions: intervene in cell wall peptidoglycan synthesis, is Actions: intervene in cell wall peptidoglycan synthesis, is
bactericidal bactericidal
Indications for use: bacterial endocarditis, meningitis, aspiration Indications for use: chromic bronchitis, CAP, acute bacterial
pneumonia, lung abscess, CAP, syphilis, septicaemia in children otitis media, sinusitis, epididymo-orchitis, acute prostatitis, acute
Contraindications for use: allergy to penicillins, cephalosporins, pyelonephritis, UTI, gonococcol infection, prophylaxis of
carbapenems endocarditis, acute cholecystitis, peritonitis, combination therapy
Adverse drug reactions: irritation at injection/IV site, nausea, for eradication H. pylori, shigellosis
diarrhoea, urticaria, rash, superinfection, allergy (fever, chills, Contraindications for use: allergy to penicillins, cephalosporins,
headache and exacerbation of lesions when used in carbapenems
syphilis/spirochete infections Jarisch-Herxheimer reaction) Adverse drug reactions: irritation at injection/IV site, nausea,
diarrhoea, urticaria, rash, superinfection, allergy
Community Acquired Pneumonia.doc Page 13 of 16 Created on 7/11/2012 1:20:00 PM
Community Acquired Pneumonia -
PHARMACOTHERAPY
ceftriaxone (medical practitioner) paracetamol
Drug (generic name): ceftriaxone Drug (generic name): paracetamol
Poisons schedule: schedule 4 Poisons schedule: unscheduled
Therapeutic class: 8(b) cephalosporins Therapeutic class: 4(b) simple analgesics and antipyretics, non-
Dosage range: 2g opiod analgesic.
Route: intravenous Dosage range: 500mg-1g
Frequency of administration: daily Route: oral/rectal
Duration of order: until significant improvement Frequency of administration: 4- 6 hourly
Actions: intervenes in bacteria cell wall peptidoglycan synthesis Duration of order: as required max 4g daily
Indications for use: severe pneumonia, orbital cellulitis, bacterial Actions: inhibition of prostaglandin synthesis
meningitis, gonococcal infection, PID, epiglottitis, septicaemia, Indications for use: mild-moderate pain, migraine, headache,
prophylaxis: meningococcal disease, H. influenzae, cholecystitis, fever, muscular pain
peritonitis, Salmonella, typhoid, sexually transmitted epididymo- Contraindications for use: nil –caution for resident with liver
orchitis disease.
Contraindications for use: allergy to penicillins, cephalosporins, Adverse drug reactions: (rare) rash, drug fever, mucosal lesions,
carbapenems neutro/pancyto/thrombocytopenia
Adverse drug reactions: nausea, diarrhoea, electrolyte
imbalance, rash, pancreatitis, cholecystitis, pseudolithiasis,
nephrolithiasis
Community Acquired Pneumonia.doc Page 14 of 16 Created on 7/11/2012 1:20:00 PM
Community Acquired Pneumonia -
PHARMACOTHERAPY
moxifloxacin cefotaxime (medical practitioner)
Drug (generic name): moxifloxacin Drug (generic name): cefotaxime
Poisons schedule: schedule 4 Poisons schedule: schedule 4
Therapeutic class: 8(e) quinolones Therapeutic class: 8(b) cephalosporins
Dosage range: 400mg Dosage range: 1g
Route: oral Route: intravenous
Frequency of administration: daily Frequency of administration: 8 hourly
Duration of order: 7 days Duration of order: until significant improvement
Actions: blocks DNA gyrase & topoisomerase IV, thus inhibiting Actions: intervenes in bacteria cell wall peptidoglycan synthesis
DNA synthesis, is bactericidal Indications for use: severe pneumonia, orbital cellulitis, bacterial
Indications for use: severe CAP, acute bacterial chronic meningitis, gonococcal infection, PID, epiglottitis, septicaemia,
bronchitis & sinusitis (where other Rx failed or contraindicated), acute cholecystitis, acute peritonitis
gonorrhoea, severe mixed aerobic & anaerobic infections, Contraindications for use: allergy to penicillins, cephalosporins,
resistant tuberculosis carbapenems
Contraindications for use: allergy to quinolones, prolongation of Adverse drug reactions: nausea, diarrhoea, electrolyte
QT interval, or Rx with drugs that prolong QT interval. imbalance, irritation at injection/IV site
Adverse drug reactions: nausea, vomiting diarrhoea, abdo. pain,
dyspepsia, rash, itch, dizziness, taste change
Community Acquired Pneumonia.doc Page 15 of 16 Created on 7/11/2012 1:20:00 PM
REFERENCES
1. Clinical Practice Guidelines for Nurses in Primary Care [monograph online]. 2000 [cited 2006 Apr 12]. Available from: http://www.hc-sc.gc.ca/msb/fnihp.
2. Tal S, Guller V, Levi S, Bardenstein R, Berger D, Gurevich I, Gurevich A. Profile and prognosis of febrile elderly resident’s with bacteremic urinary tract infection. Journal of Infection [serial online]. 2005 [cited 2006
Oct 20]; 50:296-305. Available from: ScienceDirect.
3. The Royal Australian College of General Practitioners. Medical Care of Older Persons in Residential Aged Care Facilities. 4th ed. South Melbourne: The Royal Australian College of General Practitioners; 2005.
4. Wagenlehner FM, Naber KG. Treatment of bacterial urinary tract infections: presence and future. European Urology [serial online]. 2006 [cited 2006 Oct 20]; 49:235-244. Available from: ScienceDirect.
5. Dartnell JG, editor. Therapeutic guidelines: antibiotic. 12th ed. Victoria: Therapeutic Guidelines Limited; 2003.
6. Rossi S, editor. Australian medicines handbook. Adelaide SA: Australian Medicines Handbook Pty Ltd; 2011.
7. eMIMS MIMS. MIMS medicine information [standard online]. c2005 [cited 2006 Oct 20]. Available from: eMIMS MIMS Online.
8. Hughes J. Urinary tract infections. Proceedings from The Infectious Diseases Module Lectures; 2006 Oct 9-16; Bentley, Perth: Curtin University of Technology; n.d.
9. McMurdo M, Bissett L, Price R, Phillips G, Crombie I. Does ingestion of cranberry juice reduce symptomatic urinary tract infections in older people in hospital? A double-blind, placebo-controlled trial. Age and
Ageing. 2005; 34: 256-261.
10. etg complete( internet ). Melbourne : Therapeutic Guidelines Limited; 2011 Nov Accessed 2001at http://etg.com.au/ref/re
11. Grayson ML, McDonald M, Gibson K, Athan E, Munckhof WJ, Paull P, et al. Once-daily intravenous cefazolin plus oral probenecid is equivalent to once-daily intravenous ceftriaxone plus oral placebo for the
treatment of moderate-to-severe cellulitis in adults. Clinical Infectious Diseases. 2002; 34(11): 1440-1448.
12. Ginsberg MB. Cellulitis: analysis of 101 cases and review of the literature. Southern Medical Journal. 1981; 74(5): 530-533.
13. Fleisher G, Ludwig S. Cellulitis: a prospective study. Annals of Emergency Medicine. 1980; 9(5): 246-249.
14. Kennedy M L, Fletcher KR, Plank LM. Management guidelines for nurse practitioners working with older adults. 2nd ed. Philadelphia: F. A. Davis; 2004.
15. Reuben DB, Herr KA, Pacala JT. Geriatrics at your fingertips. 6th ed. Malden, MA: Blackwell; 2004.
16. McKinnon PS, Paladino JA, Grayson ML, Gibbons GW, Karchmer AW. Cost-effectiveness of ampicillin/su;bactam versus imipenum/cilastatin in the treatment of limb-threatening foot infections in diabetic
resident’s. Clinical Infection Diseases. 1997; 24(1): 57-63.
17. Friedlaender MH. A review of the causes and treatment of bacterial and allergic conjunctivitis. Clinical Therapeutics. 1995; 17(5): 800-810.
18. Wan W L, Farkas GC, May WN, Robin JB. The clinical characteristics and course of adult gonococcal conjunctivitis. American Journal of Ophthalmology. 1986; 102(5): 575-583.
Community Acquired Pneumonia.doc Page 16 of 16 Created on 7/11/2012 1:20:00 PM
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- ACS Nursing Care PlanDocument21 pagesACS Nursing Care Planchris_arc90100% (6)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Apea Review QuestionDocument51 pagesApea Review Questionlisa100% (9)
- MRCP Recall May 19Document10 pagesMRCP Recall May 19Mariam YousifNo ratings yet
- RHU Blue Book 6 - 070852 1Document14 pagesRHU Blue Book 6 - 070852 1Jm Jm100% (1)
- Discharge Instructions For Your NewbornDocument10 pagesDischarge Instructions For Your Newbornbeauty100% (1)
- ACSDocument21 pagesACSchris_arc90100% (1)
- Formulary For VeterinariesDocument245 pagesFormulary For VeterinariesAhmad Raza100% (4)
- AntibioticsDocument122 pagesAntibioticsdentistry24100% (1)
- Breast Feeding - Teaching PlanDocument3 pagesBreast Feeding - Teaching Planpikishxxxx100% (5)
- Drug Study AmoxiclavDocument3 pagesDrug Study AmoxiclavIzza DeloriaNo ratings yet
- CO ch5Document38 pagesCO ch5chris_arc90No ratings yet
- Caesarean Section - PDFDocument13 pagesCaesarean Section - PDFchris_arc90No ratings yet
- What Is The Purpose of Oxygen Therapy For CesarianDocument3 pagesWhat Is The Purpose of Oxygen Therapy For Cesarianchris_arc90No ratings yet
- What Is The Purpose of Oxygen Therapy For CesarianDocument3 pagesWhat Is The Purpose of Oxygen Therapy For Cesarianchris_arc90No ratings yet
- AkiDocument16 pagesAkichris_arc90No ratings yet
- Existentialism2 140724182307 Phpapp01Document43 pagesExistentialism2 140724182307 Phpapp01chris_arc90No ratings yet
- Ethiopia SAM Guideline. March2007Document122 pagesEthiopia SAM Guideline. March2007pastizal123456No ratings yet
- ProductsDocument106 pagesProductsbochieng404No ratings yet
- Sto MeproDocument18 pagesSto Meprosyah yuandraNo ratings yet
- Anti Biotics & Lactam Antibiotics Visit For More Ppt'sDocument44 pagesAnti Biotics & Lactam Antibiotics Visit For More Ppt'sGANESH KUMAR JELLANo ratings yet
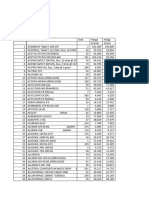
- Asia3 Product List 2 PDFDocument17 pagesAsia3 Product List 2 PDFYoussef KaidNo ratings yet
- Augmentin IV 600mg 1.2gDocument14 pagesAugmentin IV 600mg 1.2gkhangsiean89No ratings yet
- Augmentin EffectsDocument39 pagesAugmentin EffectsJasmeen SutariyaNo ratings yet
- AmoxicillinDocument2 pagesAmoxicillinKasandra Dawn Moquia BerisoNo ratings yet
- CURS ENGLEZA Boli InfectioaseDocument246 pagesCURS ENGLEZA Boli InfectioaseKiran LetrangeNo ratings yet
- Journal Reading Impetigo BulosaDocument16 pagesJournal Reading Impetigo BulosaFery LamperoughNo ratings yet
- Pharmacy News Capsule: Update On Drug AllergyDocument6 pagesPharmacy News Capsule: Update On Drug AllergyMajd ShakerNo ratings yet
- AmoxicillinDocument8 pagesAmoxicillinMariusNeicuNo ratings yet
- Amoxil: What Is in This LeafletDocument3 pagesAmoxil: What Is in This LeafletPrince AliNo ratings yet
- Drug Study PsychiaDocument10 pagesDrug Study PsychiaIRA MONIQUE CABADENNo ratings yet
- Dose CalculationsDocument39 pagesDose CalculationsAsma BakheitNo ratings yet
- Amoxil 3Document9 pagesAmoxil 3sisnaingaungNo ratings yet
- Description of AntibacterialDocument102 pagesDescription of AntibacterialChristopher SongoroNo ratings yet
- Aden Healthcare Product ListDocument12 pagesAden Healthcare Product Listsachin.maxzenNo ratings yet
- Health Centre Stgs - Federal Government of SomaliaDocument102 pagesHealth Centre Stgs - Federal Government of SomaliaAhmed MohamedNo ratings yet
- Amoxicillin Tri Hydrate Table FormatDocument2 pagesAmoxicillin Tri Hydrate Table FormatNico DonatoNo ratings yet
- Breathing Problems in A NewbornDocument2 pagesBreathing Problems in A NewbornMuhammad Danantyo HimawanNo ratings yet
- PenicillinsDocument7 pagesPenicillinsZain BaderNo ratings yet
- Glomox PilDocument1 pageGlomox Pilpharmacia1.comNo ratings yet
- 11 2 23 New-1Document34 pages11 2 23 New-1Selviana ArdiyantiNo ratings yet