Professional Documents
Culture Documents
AO - Dental Prophylaxis in A Dog
Uploaded by
Thamil ArasanOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
AO - Dental Prophylaxis in A Dog
Uploaded by
Thamil ArasanCopyright:
Available Formats
ANESTHESIA OPTIONS h ANESTHESIA h PEER REVIEWED
Dental Prophylaxis
in a Dog
Lisa Sams Ebner, DVM, MS, DACVAA, CVA
Lincoln Memorial University College of Veterinary Medicine
THE CASE 1.4 mg/dL). The urine specific gravity is 1.024. Systolic
blood pressure measurements on Doppler average 140
Benny, a 7-year-old spayed beagle, is presented
mm Hg (normal, 110-160 mm Hg). The ECG does not
for dental prophylaxis with possible extractions. reveal any significant abnormalities, and thoracic radio-
graphs do not show any cardiac enlargement or lung
Benny is up to date on vaccinations and monthly heart- changes associated with congestive heart failure.
worm, flea, and tick preventive and is fed a maintenance
dry food twice a day. She spends most time indoors and A premedication of acepromazine (0.02 mg/kg IM) and
only goes outside for short leash walks, which, according morphine (0.5 mg/kg IM) is administered. An IV cathe-
to the owner, tire her out quickly. Her BCS is 6/9. A heart ter is placed, and she is induced with propofol (3 mg/kg
murmur was detected at a veterinary examination the IV). She is intubated and placed on isoflurane for mainte-
previous month, and furosemide (1 mg/kg PO q12h) and nance. IV lactated Ringer’s solution (5 mL/kg/hr) is ini-
enalapril (0.25 mg/kg PO q12h) were prescribed. tiated. The pulse oximeter, ECG leads, Doppler, blood
pressure cuff, and sphygmomanometer are attached; an
A clinician had previously recommended against anes- anesthetic record is kept and a dental imaging study con-
thesia for the prophylaxis, but the client remains con- ducted. The procedure progresses well until Benny is
cerned about halitosis and a painful tooth that may repositioned from right to left lateral recumbency and
require extraction. A grade II/VI left systolic heart mur- systolic pressure drops to 70 mm Hg.
mur is confirmed on physical examination. Stage 3
periodontal disease is also present.
WHAT ARE THE
A thorough preanesthetic workup is recommended. The APPROPRIATE NEXT STEPS?
client agrees to a CBC, serum chemistry profile, urinaly- CHOICE 1
sis, blood pressure measurement, electrocardiogram Quickly administer a 10 mL/kg bolus of lactated
(ECG), and thoracic radiography but declines referral to Ringer’s solution.
a cardiologist for an echocardiogram. CBC and serum
chemistry profile show a slightly elevated blood urea CHOICE 2
BUN = blood urea nitrogen
nitrogen (BUN) of 39 mg/dL (reference range, 10-32 mg/ Assess the anesthetic depth, and
ECG = electrocardiogram
dL) and a creatinine of 1.8 mg/dL (reference range, 0.6- turn down the vaporizer.
March 2017 cliniciansbrief.com 97
ANESTHESIA OPTIONS h ANESTHESIA h PEER REVIEWED
CHOICE 1 CHOICE 2
Quickly administer a 10 mL/kg bolus Assess the anesthetic depth, and turn
of lactated Ringer’s solution. down the vaporizer.
A 10 mL/kg bolus of lactated Ringer’s solu- The anesthetic depth is assessed by checking
tion is administered over 5 minutes. Several jaw tone, palpebral reflexes, and eye rotation.
minutes postadministration, the pulse oxim- The patient appears to be in an adequate
eter reading drops from 97% to 90%. The plane of anesthesia, so the vaporizer setting
systolic pressure on the Doppler is 75 mm is decreased from 2% to 1.5% isoflurane. The
Hg. On closer examination of the endotra- blood pressure cuff and Doppler are also
cheal tube, white foamy fluid is noted. Aus- checked to ensure no inadvertent movement
cultation of the patient’s lungs reveals occurred when the patient was repositioned.
bilateral crackles and increased respiratory
rate. Furosemide (1 mg/kg IV) is adminis- After 5 minutes, systolic blood pressure
tered. Thoracic radiographs reveal interstitial remains 70 mm Hg. The patient has a slow
to alveolar infiltrates highly suggestive of palpebral reflex and increased jaw tone.
cardiogenic pulmonary edema due to iatro- Dobutamine is administered as a constant-
genic fluid overload. The patient’s respiratory rate infusion (CRI) at 5 µg/kg/min via a
rate slows, and the pulse oximeter reading syringe pump. Dobutamine has a rapid onset
rises to 95%. However, the decision is made of action (≈2 minutes), so blood pressure
to discontinue anesthesia and recover the should increase soon after the infusion is
patient for further evaluation of the degree of initiated.
cardiovascular disease.
At the next blood pressure reading ≈5 minutes
later, systolic pressure is 80 mm Hg. Although
this is an improvement, >90 mm Hg would
ensure a mean arterial pressure >60 mm Hg
and maintenance of perfusion of the vital
organs. Dental radiographs are almost com-
plete, but Benny swallows and starts to show
signs of being in a light plane of anesthesia. A
bolus of fentanyl (5 µg/kg IV) is administered
to allow a lower concentration of isoflurane.
The bolus was successful, so a CRI of fentanyl
(9 µg/kg/hr) is started; this rate has been
shown to decrease the mean alveolar concen-
tration of isoflurane in dogs by ≈50%.1
98 cliniciansbrief.com March 2017
A few minutes after starting the fentanyl infu-
sion, the vaporizer is adjusted to 0.75% isoflu-
DISCUSSION
rane. The patient develops sinus bradycardia
(heart rate, 52 bpm) and is still hypotensive,
potentially exacerbated by administration of
In this case, the recommendation for the
the opioid infusion. Glycopyrrolate (0.01 mg/
echocardiogram could have been more
kg) is administered, with one-half the dosage
strongly emphasized. Stressing the impor-
administered IV and one-half administered
tance of an accurate diagnosis and knowledge
IM. Within a few minutes, the patient’s heart
of the extent of cardiovascular compromise
rate rises to ≈90 bpm, and systolic blood pres-
based on a thorough cardiac diagnostic inves-
sure is 94 mm Hg.
tigation may help with selecting drugs used
in the anesthetic period and may lead to a
A caudal maxillary nerve block is adminis-
recommendation of avoiding anesthesia.
tered using 0.5 mL of bupivacaine (0.5%) with
a 25-gauge needle a few minutes before
Other potential changes for this case that
extraction of the third premolar on the left
could have been discussed on initial evalua-
upper maxilla (207). The extraction takes
tion include assessing BCS and discussing the
place with no further complications. Benny is
option of withholding enalapril on the day of
given carprofen (4.4 mg/kg SC) in recovery,
anesthesia. Drug doses should be based on
extubated within 15 minutes of discontinuing
lean body weight rather than actual body
anesthesia, and closely monitored for 2 hours.
weight. Because Benny had a BCS of 6/9, the
A forced-air warming blanket is used to return
final drug doses of acepromazine and propo-
body temperature to normal. After a few more
fol could have been scaled back to correlate
hours, Benny is alert and able to walk. She is
with her ideal body weight. Clinician prefer-
released. The owner is instructed to offer a
ence may dictate whether cardiac medications
small amount of soft food that evening, and a
should be administered on the day of anesthe-
follow-up phone call is scheduled for the next
sia. If cardiac medications are controlling a
afternoon to check on Benny’s recovery.
dysrhythmia or promoting cardiac contractil-
ity, these drugs should not be discontinued.
In the author’s experience, withholding an
angiotensin-converting enzyme inhibitor (eg,
enalapril, benazepril) on the day of anesthe-
sia prevents a detrimental decrease in after-
Knowledge of the extent load that is not well tolerated in anesthetized
dogs. In a recent study, enalapril adminis-
of cardiovascular tered to healthy dogs 90 minutes before iso-
compromise based flurane anesthesia increased the degree of
intra-anesthetic hypotension and the number
on a thorough cardiac of interventions required to correct moderate-
diagnostic investigation to-severe hypotension.2
may help with selecting Drug Selections
anesthetic drugs. On review of the anesthetic plan, the choice of
premedication with acepromazine and mor- CRI = constant-
rate infusion
phine followed by induction with propofol
March 2017 cliniciansbrief.com 99
ANESTHESIA OPTIONS h ANESTHESIA h PEER REVIEWED
could also be scrutinized. Acepromazine lar disease may be etomidate (1 mg/kg IV)
causes tranquilization but can also lead to because of its small effect on heart rate or
hypotension due to α-1 adrenergic blockade. blood pressure. It is often administered imme-
Because it is a long-lasting drug with no rever- diately following a dose of a benzodiazepine
sal agent, acepromazine is typically avoided in (eg, 0.2 mg/kg IV midazolam or diazepam) to
patients with cardiovascular disease. Mor- produce a smoother induction quality. Etomi-
phine used alone in older dogs and those with date is typically affordable and can be stocked
cardiovascular disease often produces ade- by general practitioners for induction of
quate sedation. An alternative opioid choice patients with cardiovascular disease.
for this patient would be an equivalent dose of
hydromorphone, which does not have the An alternative induction plan for Benny could
potential to cause vasodilation due to the have been fentanyl (5 µg/kg IV) with a benzo-
release of histamine that can occur with mor- diazepine (midazolam or diazepam at 0.2 mg/
phine, although vasodilation is usually only kg IV), ketamine (5 mg/kg IV) and midazolam
seen after IV morphine administration. or diazepam (0.2 mg/kg IV), or alfaxalone
(1-2 mg/kg IV). These drug combinations are
Propofol was not the ideal induction agent for typically more cardiovascular sparing than
this patient and should have been avoided if propofol alone. Maintenance anesthesia with
possible. Propofol can cause respiratory isoflurane can be cost effective but can cause
depression, cardiovascular depression, and dose-dependent hypotension. Sevoflurane is
marked vasodilation, which is transient and another choice of inhalant for anesthesia;
will not cause complications in most healthy adjustments to the vaporizer would occur
patients. However, in patients with pre-exist- more quickly, which can be beneficial in
ing cardiovascular disease, the reduction in patients with deep hypotension. However,
systemic vascular resistance and negative ino- opinion varies about whether the adjustability
tropic effects from propofol administration of sevoflurane is of significant benefit as com-
can lead to a dose-dependent hypotension that pared with isoflurane in such cases. Balanced
would be detrimental to the patient. A safer anesthesia using fentanyl CRI from the start of
induction agent for patients with cardiovascu- anesthesia could have offered minimum alveo-
lar concentration reduction and decreased the
likelihood for hypotension.
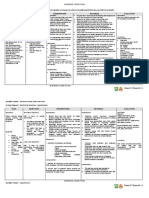
FACTORS THAT MAY REDUCE ANESTHETIC RISK Fluids
IN PATIENTS WITH CARDIOVASCULAR DISEASE Further review of this case could prompt the
h Accurate diagnosis of underlying cardiac disease before anesthesia anesthetist to select a lower IV fluid rate (eg,
h Avoiding drugs that have profound cardiovascular effects (eg, 3 mL/kg/hr), as there was no significant blood
α2-agonists, acepromazine, propofol) loss involved in the procedure. Physical exam-
ination should have detected any underlying
h Providing adequate physiologic monitoring before, during, and after
issues with hydration. BUN and creatinine
the procedure
were slightly elevated, but these changes are
h Preoxygenating patient ≈5 minutes before induction expected for a patient receiving furosemide.
h Adequately planning for a case and preoperative patient preparation Historically, low-sodium IV fluids (eg, 0.45%
NaCl/2.5% dextrose) were recommended;
h Considering a multimodal approach to reduce inhalant anesthesia
however, hypovolemic patients warrant a bal-
requirements
anced electrolyte solution (eg, lactated Ring-
h Using IV fluids conservatively er’s solution) instead of a hypotonic crystalloid
100 cliniciansbrief.com March 2017
during anesthesia at a conservative rate. Hypo- should not be given a fluid bolus. If a patient
tonic solutions have a large volume of distribu- with known but unclassified cardiac abnor-
tion and could potentially lead to cellular malities requires a fluid bolus, the dose should
swelling if given as a replacement fluid. be reduced significantly; it should be adminis-
tered over a longer period of time and carefully
Colloid solutions should be avoided, as they monitored.
will expand the intravascular volume for a lon-
ger period of time as compared with crystal- There are many ways to reduce anesthesia risk
loid solutions and therefore could lead to in veterinary patients (see Factors that May
volume overload in a patient with cardiac dys- Reduce Anesthetic Risk in Patients with Car- BUN = blood urea
function. Even a bolus of crystalloid solution diovascular Disease). A primary goal when nitrogen
should be carefully considered in this patient. administering anesthesia should be to decrease CRI = constant-
rate infusion
A patient that is euvolemic or hypervolemic the time under anesthesia when possible. n
References
1. Simões CR, Monteiro ER, Rangel JP, Nunes-Junior JS, isoflurane anesthesia in healthy dogs. Vet Anaesth Analg.
Campagnol D. Effects of prolonged infusion of fentanyl, with 2016;43(5):482-494.
or without atropine, on the minimum alveolar concentration
of isoflurane in dogs. Vet Anaesth Analg. 2016;43(2):134-144.
2. Coleman AE, Shepard MK, Schmiedt CW, Hofmeister EH, Suggested Reading
Brown SA. Effects of orally administered enalapril on blood Mama K, Ames M. Anesthesia for dogs with myxomatous mitral
pressure and hemodynamic response to vasopressors during valve disease. Clinician’s Brief. 2016;14(8):99-105.
You might also like
- The Michael Jackson Autopsy Insights Provided by A Forensic Anesthesiologist 2157 7145.1000138 PDFDocument8 pagesThe Michael Jackson Autopsy Insights Provided by A Forensic Anesthesiologist 2157 7145.1000138 PDFJimmy R. JosephNo ratings yet
- Vasoactive TherapyDocument26 pagesVasoactive Therapylidya agustin100% (1)
- PsychopharmacologyDocument64 pagesPsychopharmacologyGaurav Tandon100% (2)
- Appendix B: Clinical Institute Withdrawal Assessment For Alcohol (CIWA-A)Document2 pagesAppendix B: Clinical Institute Withdrawal Assessment For Alcohol (CIWA-A)Tracy100% (1)
- Markiii RM PDFDocument285 pagesMarkiii RM PDFveehneeNo ratings yet
- Acute Kidney Injury W/ Hyperkalemia NCPDocument5 pagesAcute Kidney Injury W/ Hyperkalemia NCPMyrvic Ortiz La OrdenNo ratings yet
- When To Pick The Nose: Out-of-Hospital and Emergency Department Intranasal Administration of MedicationsDocument9 pagesWhen To Pick The Nose: Out-of-Hospital and Emergency Department Intranasal Administration of MedicationsepraetorianNo ratings yet
- 7..intravenous Anaesthesia 2Document23 pages7..intravenous Anaesthesia 2Mwiliza BrendaNo ratings yet
- Premedicantdrugs1 170216071329Document49 pagesPremedicantdrugs1 170216071329Sagar BhardwajNo ratings yet
- 2022 - PINELLA Workbook - v08Document84 pages2022 - PINELLA Workbook - v08Ann FarstaNo ratings yet
- Comparative Animal AnatomyDocument324 pagesComparative Animal AnatomyMohammed Anuz80% (5)
- Management of Neonatal Seizures: AIIMS-NICU Protocols 2010Document18 pagesManagement of Neonatal Seizures: AIIMS-NICU Protocols 2010gitphillipNo ratings yet
- Azolla Success StoryDocument3 pagesAzolla Success StoryThamil ArasanNo ratings yet
- Azolla Study ReportDocument26 pagesAzolla Study ReportThamil ArasanNo ratings yet
- Drug StudyDocument10 pagesDrug StudyAbie Jewel Joy Roque100% (1)
- Duck PDFDocument21 pagesDuck PDFThamil ArasanNo ratings yet
- Imunologie MedicalaDocument224 pagesImunologie MedicalaTo Ma100% (10)
- Nursing Care Plan 6 Impaired Gas ExchangeDocument9 pagesNursing Care Plan 6 Impaired Gas Exchangedbryant0101100% (12)
- Drugs Generally Used On Veterinary Clinics in India PDFDocument17 pagesDrugs Generally Used On Veterinary Clinics in India PDFSwarup charan67% (3)
- TBR AclsDocument9 pagesTBR Aclsric_vir_014No ratings yet
- Minimally Invasive Monitoring Liver ResectionDocument2 pagesMinimally Invasive Monitoring Liver ResectionHENLEYNo ratings yet
- Application of The Continuous Autotransfusion System (CATS) To Prevent Transfusion-Related Hyperkalemia Following Hyperkalemic Cardiac Arrest in An Infant - A Case ReportDocument4 pagesApplication of The Continuous Autotransfusion System (CATS) To Prevent Transfusion-Related Hyperkalemia Following Hyperkalemic Cardiac Arrest in An Infant - A Case Reportmaria bethania martins leiteNo ratings yet
- IndianJAnaesth614359-4497437 122934Document2 pagesIndianJAnaesth614359-4497437 122934Meiriyani LembangNo ratings yet
- Doctors OrderDocument9 pagesDoctors OrderReal TetisoraNo ratings yet
- Jurnal AnestesiDocument3 pagesJurnal AnestesiDita TifaniadiNo ratings yet
- Monitoring Equine AnesthesiaDocument5 pagesMonitoring Equine AnesthesiaLaura RestrepoNo ratings yet
- Article About Drug CardiovascularDocument8 pagesArticle About Drug CardiovascularhandiNo ratings yet
- Anaesthesia For Carotid EndarterectomyDocument19 pagesAnaesthesia For Carotid EndarterectomyFahran HakeemNo ratings yet
- Jantung Dan PembuluhDocument5 pagesJantung Dan PembuluhBzma AdiyanaNo ratings yet
- Induction Using Fentanyl To Suppress The Intubation Response in The Cardiac Patient: What Is The Optimal Dose?Document7 pagesInduction Using Fentanyl To Suppress The Intubation Response in The Cardiac Patient: What Is The Optimal Dose?Bill RajagukgukNo ratings yet
- Effect of N-Methyl-D-Aspartate (NMDA) Receptor Antagonist Combination As Adjuvant To General Anesthesia in Functional Endoscopic Sinus SurgeryDocument10 pagesEffect of N-Methyl-D-Aspartate (NMDA) Receptor Antagonist Combination As Adjuvant To General Anesthesia in Functional Endoscopic Sinus SurgeryWanda WardhaniNo ratings yet
- 17 2021 CC PulmonaryDisordersIIDocument28 pages17 2021 CC PulmonaryDisordersIIRana Khaled AwwadNo ratings yet
- Neuro CaseDocument25 pagesNeuro CaseHainey GayleNo ratings yet
- Multiple Choice Question (True-False)Document10 pagesMultiple Choice Question (True-False)Gx NavinNo ratings yet
- Santhunew 160125063449 PDFDocument28 pagesSanthunew 160125063449 PDFPhyo Htay KyawNo ratings yet
- FARMAKOLOGI OBAT VASOPRESOR-dr DjujukDocument25 pagesFARMAKOLOGI OBAT VASOPRESOR-dr DjujukjavajavuNo ratings yet
- A Case of Central Diabetes Insipidus After Ketamine Infusion During An External To Internal Carotid Artery BypassDocument4 pagesA Case of Central Diabetes Insipidus After Ketamine Infusion During An External To Internal Carotid Artery Bypassalyssa azzahraNo ratings yet
- Farmakologi Obat VasopresorDocument25 pagesFarmakologi Obat Vasopresorhendrik taufikNo ratings yet
- Kjae 59 116Document3 pagesKjae 59 116Mushthafa HabiburrahmanNo ratings yet
- Inadvertent IV Administration of Epi and Not IMDocument4 pagesInadvertent IV Administration of Epi and Not IMsmith.kevin1420344No ratings yet
- Transfusion Related-Acute Lung Injury A Case Study: Dawn Barten MT (ASCP)Document53 pagesTransfusion Related-Acute Lung Injury A Case Study: Dawn Barten MT (ASCP)asclswisconsin0% (1)
- Epinephrine (Adrenaline)Document9 pagesEpinephrine (Adrenaline)Tushar GhuleNo ratings yet
- Anafilaxia MidazolamDocument3 pagesAnafilaxia MidazolamDiana PintorNo ratings yet
- Farmakologi Obat VasopresorDocument25 pagesFarmakologi Obat VasopresorNudyan BetharinaNo ratings yet
- Cu 7Document6 pagesCu 7VALERIANO TRISHANo ratings yet
- SKILL STATION Management of Critically Ill Patient With Septic Shock Provider GuideDocument27 pagesSKILL STATION Management of Critically Ill Patient With Septic Shock Provider GuidesrinidhiNo ratings yet
- Case Study On Critical CareDocument6 pagesCase Study On Critical CareJude Micko Bunyi AlipitNo ratings yet
- Objective Data Diagnosis Goals Interventions EvaluationDocument2 pagesObjective Data Diagnosis Goals Interventions EvaluationHira Akram Hira AkramNo ratings yet
- CASE STUDY PEDIA - SaavedraDocument15 pagesCASE STUDY PEDIA - SaavedraChryst Louise SaavedraNo ratings yet
- ClonidineDocument4 pagesClonidineDR RAVI ANANDNo ratings yet
- Topic 10 Internal Medicine Ali SaifDocument5 pagesTopic 10 Internal Medicine Ali SaifAnkit Kumar PatelNo ratings yet
- Ct7 Fluid, Electrolyte ImbalanceDocument9 pagesCt7 Fluid, Electrolyte ImbalanceAlondra VelascoNo ratings yet
- TURP SyndromeDocument5 pagesTURP SyndromeNugraha Septian BahrunNo ratings yet
- 31-Article Text-56-1-10-20190118Document7 pages31-Article Text-56-1-10-20190118Fatos KatanolliNo ratings yet
- Transfusion-Associated Circulatory Overload (TACO)Document2 pagesTransfusion-Associated Circulatory Overload (TACO)belongs2diah3058100% (1)
- Vasoactive TherapyDocument26 pagesVasoactive Therapylidya agustinNo ratings yet
- Activity No1 Case Study On CADDocument3 pagesActivity No1 Case Study On CADVictor StevenNo ratings yet
- CVVHDocument4 pagesCVVHSyarif UddinNo ratings yet
- Drug StudypppDocument42 pagesDrug Studyppp2022106284No ratings yet
- Kjae 59 S99Document4 pagesKjae 59 S99Adel AdielaNo ratings yet
- ECG WorksheetDocument4 pagesECG WorksheetNikki GuisonNo ratings yet
- Adult T-Cell Leukemia Lymphoma (Atll) A Rare Case Associated With Human T-Cell Virus (Htlv-1)Document19 pagesAdult T-Cell Leukemia Lymphoma (Atll) A Rare Case Associated With Human T-Cell Virus (Htlv-1)Priya ChandakNo ratings yet
- Poisoning Due To Abrus Precatorius (Jequirity Bean) : CasereportDocument3 pagesPoisoning Due To Abrus Precatorius (Jequirity Bean) : CasereportANDREA ESTEFANIA CUENCA CHIMBONo ratings yet
- Ventura County Medical Center: Mi Thrombolysis, Management ofDocument3 pagesVentura County Medical Center: Mi Thrombolysis, Management ofblackcat657No ratings yet
- Intravenous Dexmedetomidine Prolongs Bupivacaine Spinal Analgesia M Ma - M, I ZB, H Ma - A, B Aa - B, I MM S M. A - GDocument8 pagesIntravenous Dexmedetomidine Prolongs Bupivacaine Spinal Analgesia M Ma - M, I ZB, H Ma - A, B Aa - B, I MM S M. A - GMOHAMMED IQBALNo ratings yet
- PGDT Protocol Summary ReferenceDocument32 pagesPGDT Protocol Summary Referenceghg sddNo ratings yet
- Anaesthetic EmergenciesDocument11 pagesAnaesthetic EmergenciesSivasankaryNo ratings yet
- Intracardiac Epinephrine Injection During Open Thoracotomy and Circulatory ArrestDocument2 pagesIntracardiac Epinephrine Injection During Open Thoracotomy and Circulatory ArrestRaven DelargeNo ratings yet
- E Posters PDFDocument349 pagesE Posters PDFpriyadikkalaNo ratings yet
- Severe Preeclampsia BahanDocument7 pagesSevere Preeclampsia BahanelenNo ratings yet
- Anasarca Edema With Amlodipine TreatmentDocument4 pagesAnasarca Edema With Amlodipine TreatmentVeronikaNo ratings yet
- Negi 2014Document14 pagesNegi 2014Olivia LimNo ratings yet
- 01-10 2022 Pharm Acute Care in Cardiology 2022 R2Document62 pages01-10 2022 Pharm Acute Care in Cardiology 2022 R2Amira HelayelNo ratings yet
- Cardiac Arrest Upon Induction of General AnesthesiaDocument7 pagesCardiac Arrest Upon Induction of General AnesthesiaIlona HiariejNo ratings yet
- Unit - I: Managee's Potential Is Determined When A Set of Tasks Are Assigned To Him. It IsDocument233 pagesUnit - I: Managee's Potential Is Determined When A Set of Tasks Are Assigned To Him. It IsAmit BaruahNo ratings yet
- 5 OzkanDocument6 pages5 OzkanThamil ArasanNo ratings yet
- Anesthesia Guidelines For Dogs and CatsDocument9 pagesAnesthesia Guidelines For Dogs and CatsNatalie KingNo ratings yet
- Agriculture Knowledge Management: Advance Training Program OnDocument68 pagesAgriculture Knowledge Management: Advance Training Program OnThamil ArasanNo ratings yet
- Equine ExamDocument85 pagesEquine Examياسر قاتل البزونNo ratings yet
- Byagagaire - Xylazine Hydrochloride and Ketamine Hydrochloride Combinations For General Anaesthesia in SheepDocument182 pagesByagagaire - Xylazine Hydrochloride and Ketamine Hydrochloride Combinations For General Anaesthesia in SheepThamil ArasanNo ratings yet
- Anatomy of The Equine FootDocument14 pagesAnatomy of The Equine FootEdmilson Daneze100% (1)
- Bone Marrow Sampling: Bone Marrow Cytology (Aspiration) Vs Histology (Core Biopsy)Document5 pagesBone Marrow Sampling: Bone Marrow Cytology (Aspiration) Vs Histology (Core Biopsy)Thamil ArasanNo ratings yet
- Canine Chronic Hepatitis: Diagnosis & TreatmentDocument8 pagesCanine Chronic Hepatitis: Diagnosis & TreatmentThamil ArasanNo ratings yet
- How 20to 20perform 20a 20physical 20exam 20in 20your 20horseDocument50 pagesHow 20to 20perform 20a 20physical 20exam 20in 20your 20horseThamil ArasanNo ratings yet
- Interglobe Aviation LTDDocument2 pagesInterglobe Aviation LTDThamil ArasanNo ratings yet
- Infection and ImmunityDocument36 pagesInfection and ImmunityThamil ArasanNo ratings yet
- 3rd Yr CFC Handbook - 2 - Final 2010-11Document16 pages3rd Yr CFC Handbook - 2 - Final 2010-11Barbara LiNo ratings yet
- Caesarean SectionDocument1 pageCaesarean SectionThamil ArasanNo ratings yet
- How Estrogen Protects BonesDocument7 pagesHow Estrogen Protects BonesThamil ArasanNo ratings yet
- All Accounts Balance Details: S. No. Account Number Account Type Branch Rate of Interest (% P.a.) BalanceDocument1 pageAll Accounts Balance Details: S. No. Account Number Account Type Branch Rate of Interest (% P.a.) BalanceThamil ArasanNo ratings yet
- Hanuman Chalisa Lyrics in Tamil Font PDFDocument4 pagesHanuman Chalisa Lyrics in Tamil Font PDFThamil ArasanNo ratings yet
- Duck Housing and ManagementDocument7 pagesDuck Housing and ManagementThamil ArasanNo ratings yet
- Ivra Abstracts 2012Document42 pagesIvra Abstracts 2012Thamil ArasanNo ratings yet
- Azolla Cultivation and Feeding LivestockDocument1 pageAzolla Cultivation and Feeding LivestockThamil ArasanNo ratings yet
- Adoption of Azolla Cultivation Technology in The Farmers' Field: An AnalysisDocument7 pagesAdoption of Azolla Cultivation Technology in The Farmers' Field: An AnalysisThamil ArasanNo ratings yet
- MYD - Hematochezia in A DogDocument5 pagesMYD - Hematochezia in A DogThamil ArasanNo ratings yet
- Imcrj 9 241Document5 pagesImcrj 9 241Thamil ArasanNo ratings yet
- Proforma For Registration of Subjects For Dissertation: Appendix-IcDocument32 pagesProforma For Registration of Subjects For Dissertation: Appendix-IcRahul KambleNo ratings yet
- CNS Drugs PharmacologyDocument8 pagesCNS Drugs PharmacologyAenNo ratings yet
- 7780Document4 pages7780Cristina Elena NicuNo ratings yet
- Randomized Trial of Three Anticonvulsant Medications For Status EpilepticusDocument11 pagesRandomized Trial of Three Anticonvulsant Medications For Status EpilepticusGerson CoelhoNo ratings yet
- Human Drug IndexDocument403 pagesHuman Drug IndexJohanna NathasiaNo ratings yet
- P 0.171) - However, Outcomes As Alcohol Withdrawal Delirium, Symptom-Triggered Regimen Can Decrease The Chance of AlcoholDocument7 pagesP 0.171) - However, Outcomes As Alcohol Withdrawal Delirium, Symptom-Triggered Regimen Can Decrease The Chance of AlcoholSupanida UjjinNo ratings yet
- SH Ankh Push PiDocument10 pagesSH Ankh Push PiRavindra ChobariNo ratings yet
- Bagan KejangDocument10 pagesBagan KejangNie' MKNo ratings yet
- Antiepilepsy Drugs: Pharmacodynamics and Principles of Drug SelectionDocument22 pagesAntiepilepsy Drugs: Pharmacodynamics and Principles of Drug SelectionNaela RizqiNo ratings yet
- Anxiolytic DrugsDocument8 pagesAnxiolytic DrugsTony DawaNo ratings yet
- Definition of TermsDocument8 pagesDefinition of TermsJoshua D None-NoneNo ratings yet
- Medi 95 E2881Document5 pagesMedi 95 E2881Betari YoscarNo ratings yet
- 1 - Status EpilepticusDocument82 pages1 - Status EpilepticusfennycarlaNo ratings yet
- Chapter 13: Antiparkinsonian DrugsDocument5 pagesChapter 13: Antiparkinsonian DrugsKT100% (1)
- Drug Study DiazepamDocument1 pageDrug Study DiazepamjolibeecaldonaNo ratings yet
- Management of Hospitalized Patients Diagnosed With Alcohol Withdrawal SyndromeDocument4 pagesManagement of Hospitalized Patients Diagnosed With Alcohol Withdrawal SyndromeLoryChNo ratings yet
- Kee: Pharmacology, 6th Edition: Test Bank Chapter 4: Medications and Calculations Short AnswerDocument39 pagesKee: Pharmacology, 6th Edition: Test Bank Chapter 4: Medications and Calculations Short Answerthu_vu_2983% (6)
- Nursing Diagnosis: Acute Pain: NANDA Definition: Pain Is Whatever The ExperiencingDocument13 pagesNursing Diagnosis: Acute Pain: NANDA Definition: Pain Is Whatever The Experiencingasmika danaNo ratings yet
- DiazepamDocument2 pagesDiazepamRochelle DiezmoNo ratings yet
- To Study The Effect of Hypnotics in Mice PDFDocument2 pagesTo Study The Effect of Hypnotics in Mice PDFSuman DahalNo ratings yet