Professional Documents
Culture Documents
Hyponatremia in Diabetes Mellitus Clues To Diagnosis and Treatment 2155 6156 1000560
Uploaded by
Hastri AdheOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hyponatremia in Diabetes Mellitus Clues To Diagnosis and Treatment 2155 6156 1000560
Uploaded by
Hastri AdheCopyright:
Available Formats
Liamis et al.
, J Diabetes Metab 2015, 6:6
Diabetes & Metabolism http://dx.doi.org/10.4172/2155-6156.1000560
Commentary Open Access
Hyponatremia in Diabetes Mellitus: Clues to Diagnosis and Treatment
George Liamis, Vasilios Tsimihodimos* and Moses Elisaf
Department of Internal Medicine, School of Medicine, University of Ioannina, Ioannina, Greece
Hyponatremia is the most common electrolyte abnormality hypotonic losses (losses of water in excess of electrolytes), which tend
in clinical practice and is associated with increased morbidity and to increase serum sodium levels, and hypovolemia–induced decrease in
mortality [1,2]. Even small decreases of serum sodium are associated serum sodium levels [4].
with increased probability for adverse outcomes (cognitive impairment,
Drugs are a common cause of hyponatremia even in individuals
falls, osteoporosis and fractures) [3].
with diabetes [15]. In fact, a number of drugs used in this population
Decreased serum sodium levels are occasionally observed in could result in a decrease of serum sodium levels [mainly thiazides
patients with diabetes mellitus and can be attributed to numerous in combination with SSRIs [16], and first generation sulphonylureas
underlying pathogenetic mechanisms (Table 1) [4,5]. (such as tolbutamide and chlorpropamide)] [4,16]. However, a
growing list of drugs implicated in the development of hyponatremia
The direct measurement of serum osmolality (Posm) can
has been published [15], including NSAIDs, angiotensin converting
differentiate between hypotonic hyponatremia (with decreased
enzyme inhibitors, rosiglitazone or even amlodipine [15]. Patients
Posm) and hyponatremia associated with normal or even increased
with central nervous system disorders, pulmonary disorders including
tonicity. In the latter case hyponatremia is usually due to the coexistent
lung infections, and malignancies may exhibit hyponatremia due to
hyperglycemia [6]. In fact, glucose is an osmotic active substance.
the syndrome of inappropriate antidiuresis [4,6,16-18]. Patients with
Thus, in cases of marked hyperglycemia Posm is increased leading
diabetic nephropathy and chronic renal failure are very prone to
to movement of water out of cells and subsequently to a reduction
the development of hyponatremia due to decreased water excretion.
of serum sodium levels (dilutional hyponatremia). In such cases the
Additionally, diabetic patients with hyporeninemic hypoaldosteronism
corrected, for the degree of hyperglycemia, serum sodium value
commonly exhibit exaggerated natriuresis leading to volume depletion-
should be calculated. Thus, to obtain the “true” sodium level in cases
induced increase in ADH secretion, decreased water excretion and
of extreme hyperglycemia, the addition of 2.4 mEq/L to the measured
mild hyponatremia associated with asymptomatic hyperkalemia, and
concentration for every 100 mg/dl increment in plasma glucose above
hyperchloremic metabolic acidosis [19].
normal levels is required [7]. This corrected serum sodium level should
be used during treatment of severe hyperglycemic states [8]. In patients Interestingly, Liamis et al have recently shown that diabetes
with dilutional hyponatremia the treatment of hyperglycemia is usually mellitus per se is associated with hyponatremia, independently of the
followed by a normalization of serum sodium levels [4]. presence of hyperglycemia [2]. It has been suggested that the altered
vasopressin regulation in diabetes mellitus, the increased insulin-
No hypotonic hyponatremia (with a normal measured Posm) can
induced potentiation of vasopressin–induced acquaporin AQP2 water
also be due to pseudohyponatremia associated with hyperglycemia–
channels expression and the absorption of water from the GI tract due
induced severe hypertriglyceridemia and perhaps hypovolemia–
induced hyperproteinemia. It is well known that when the proportion A) Non hypotonic hyponatremia
of a serum sample occupied by substances other than water and With increased Posm: Hyperglycemia - induced (dilutional)
electrolytes (such as lipids and proteins) exceeds the usual value of With normal Posm: Pseudohyponatremia (marked hypertriglyceridemia and
7%, serum sodium levels measured by ion-selective electrodes using hyperproteinemia)
the indirect method are falsely lower than true values [9-13]. Thus, in B) Hypotonic hyponatremia
patients with lipemic serum and severe hypertriglyceridemia, sodium • Hypovolemia-induced
levels should be measured by direct potentiometry in blood gas panels. • Drug –induced hyponatremia (mainly with thiazides and first generation
This method does not include a predilution step and is not susceptible sulphonylureas)
to the aforementioned errors [13]. Diagnosis of pseudohyponatremia • Diabetes mellitus - associated hyponatremia
is necessary to avoid dangerous overtreatment. It should be mentioned • Syndrome of inappropriate antidiuresis associated with coexisting disorders or
that pseudohyponatremia does not produce any of the symptoms administered drugs
classically attributed to hyponatremia. Improvement in glycemic • Chronic renal failure (diabetic nephropathy) or associated with the syndrome of
hyporeninemic hypoaldosteronism
control is associated with a rapid decrease in serum triglycerides
resulting in the correction of pseudohyponatremia. Thus, no specific Table 1: Causes of hyponatremia in diabetic patients.
treatment is required [4,6].
The most common cause of hypotonic hyponatremia in patients *Corresponding author: Vasilis Tsimihodimos, Department of Internal
with diabetes is osmotic diuresis-induced hypovolemia [4]. It should Medicine, Medical School, University of Ioannina, 451 10 Ioannina, Greece, Tel:
be mentioned that in patients with diabetic ketoacidosis the excretion +302651007623; Fax: +302651007016; E-mail: tsimiho@gmail.com
of β-hydroxybutyrate and acetoacetate obligate urine sodium losses Received April 27, 2015; Accepted May 27, 2015; Published May 30, 2015
resulting in aggravation of hypovolemia [14]. Hypovolemia can also
Citation: Liamis G, Tsimihodimos V, Elisaf M (2015) Hyponatremia in Diabetes
be due to diabetes mellitus-associated complications, such as diarrhea Mellitus: Clues to Diagnosis and Treatment. J Diabetes Metab 6: 560.
and vomiting. doi:10.4172/2155-6156.1000560
Serum sodium levels in poorly controlled patients with diabetes Copyright: © 2015 Liamis G, et al. This is an open-access article distributed under
the terms of the Creative Commons Attribution License, which permits unrestricted
mellitus vary, since these levels are the result of hyperglycemia-induced use, distribution, and reproduction in any medium, provided the original author and
hyponatremia (dilutional hyponatremia), osmotic diuresis-induced source are credited.
J Diabetes Metab Volume 6 • Issue 6 • 1000560
ISSN: 2155-6156 JDM, an open access journal
Citation: Liamis G, Tsimihodimos V, Elisaf M (2015) Hyponatremia in Diabetes Mellitus: Clues to Diagnosis and Treatment. J Diabetes Metab 6: 560.
doi:10.4172/2155-6156.1000560
Page 2 of 3
to slower stomach emptying may play a role in the association between hypotonic fluids, whereas the administration of normal saline plus
diabetes mellitus and decreased serum sodium levels [20,21]. potassium chloride should be avoided in most circumstances [24].
Taking in to consideration the multifactorial origin of Hypertonic saline should be given only for severely symptomatic
hyponatremia in most patients with diabetes a cause-specific treatment hyponatremia (e.g., seizures) to rapidly increase serum sodium
is required. Discontinuation of culprit medications and avoidance of concentration until the symptoms subside whereas less symptomatic
readministration is advised. Administration of insulin drives glucose hyponatremia may be corrected at a slower pace. In all cases, however,
and water into the cells, reverses the initial direction of water movement the increase in serum sodium concentration should be limited to 10
and results in an increment of serum sodium levels. Treatment of mmol/l in the first 24h and 8 mmol/l during every 24 h thereafter.
underlying factors (e.g hypovolemia, infections) that can contribute to The therapeutic target should be even lower (i.e. <4–6 mmol/L)
or provoke hyponatramia is also of paramount importance. in the presence of risk factors for the development of the osmotic
The careful and proper management of hypovolemia (with saline demyelination syndrome [25]. It should be emphasized that patients
solutions and also potassium chloride solutions, if hypokalemia with diabetes are at high risk for the development of the osmotic
is present) can also increase serum sodium levels. It should be demyelination syndrome during rapid correction of hyponatremia. In
acknowledged that potassium ions should also be taken into account fact, they commonly exhibit risk factors that predispose to this disorder,
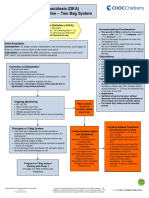
in the calculation of the tonicity of the administered fluids to avoid such as malnutrition, hypokalemia, and hypoxia [26]. In Figure 1 a
inappropriate overcorrection of hyponatremia as well as circulatory detailed algorithm for the differential diagnosis of hyponatremia in
overloading [22,23]. Thus, potassium chloride should be added in diabetic patients is illustrated.
Hyponatremia (serum sodium <136mEq/L)
Determination of sodium by direct ion selective
Presence of electrode [exclusion of pseudohyponatremia]
hypertriglyceridemia (on arterial blood gas panel)
(lipemic sera)
Normal Posm (280-295mosmol/kg)
Absence of hypertriglyceridemia
Measure Posm (by an osmometer if available)
Posm <280mosmol/kg Posm>280mosmol/kg
Hypertonic hyponatremia due to hyperglycemia calculate
Hypotonic hyponatremia
the corrected for the degree of hyperglycemia serum sodium
levels
Urine Sodium Or rarely
Uremia –induced hyponatremia in cases of
chronic renal failure (diabetic nephropathy)
<20mEq/L >40mEq/L
Hypovolemia+ SIADH
Hyporeninemic hypoaldosteronism
+It should be mentioned that in hypovolemic patients on diuretics or with increased osmotic diuresis urine
sodium may be higher than 20msEq/L
Figure 1: Diagnostic algorithm in diabetic individuals with hyponatremia.
J Diabetes Metab Volume 6 • Issue 6 • 1000560
ISSN: 2155-6156 JDM, an open access journal
Citation: Liamis G, Tsimihodimos V, Elisaf M (2015) Hyponatremia in Diabetes Mellitus: Clues to Diagnosis and Treatment. J Diabetes Metab 6: 560.
doi:10.4172/2155-6156.1000560
Page 3 of 3
References 14. Chiasson JL, Aris-Jilwan N, Belanger R (2003) Diagnosis and treatment of
diabetic ketoacidosis and the hyperglycemic hyperosmolar state. CMAJ 168:
1. Waikar SS, Mount DM, Curhan GC (2009) Mortality after hospitalization with 859-866.
mild, moderate, and severe hyponatremia. Am J Med 122: 857-865.
15. Liamis G, Milionis H, Elisaf M (2008) A review of drug-induced hyponatremia.
2. Liamis G, Rodenburg EM, Hofman A, Zietse R, Stricker BH, et al. (2013) Am J Kidney Dis 52: 144-153.
Electrolyte disorders in community subjects: prevalence and risk factors. Am
J Med 126: 256-263. 16. Blijderveen JC, Straus SM, Rodenburg EM, Zietse R, Stricker BH, et al. (2014)
Risk of hyponatremia with diuretics: chlorthalidone versus hydrochlorothiazide.
3. Podesta MA, Faravelli I, Cucchiari D, Reggiani F, Oldani S, et al. (2015) Am J Med 127: 763-771.
Neurological counterparts of hyponatremia: pathological mechanisms and
clinical manifestations. Curr Neurol Neurosci Rep 15: 18. 17. Liamis G, Milionis HJ, Elisaf M (2011) Hyponatremia in patients with infectious
diseases. J Infect 63: 327-335.
4. Liamis G, Liberopoulos E, Barkas F, Elisaf M (2014) Diabetes mellitus and
electrolyte disorders. World J Clin Cases 2: 488-496. 18. Liamis G, Milionis HJ, Elisaf M (2011) Endocrine disorders; causes of
hyponatremia not to neglect. Ann Med 43: 179-187.
5. Elisaf MS, Tsatsoulis AA, Katopodis KP, Siamopoulos KC (1996) Acid-base
and electrolyte disturbances in patients with diabetic ketoacidosis. Diabetes 19. DeFronzo RA (1980) Hyperkalemia and hyporeninemic hypoaldosteronism.
Res Clin Pract 34: 23-27. Kidney Int 17: 118-134.
6. Milionis HJ, Liamis GL, Elisaf MS (2012) The hyponatremic patient: a systematic 20. Bankir L, Bardoux nP, Ahloulay M (2001) Vasopressin and diabetes mellitus.
approach to laboratory diagnosis. CMAJ 166: 1056-1062. Nephron 87: 8-18.
7. Hillier TA, Abbott RD, Barrett EJ (1999) Hyponatremia: evaluating the correction 21. Bustamante M, Hasler U, Kotova O, Chibalin AV, Mordasini D, et al. (2005)
factor for hyperglycemia. Am J Med 106: 399-403. Insulin potentiates AVP-induced AQP2 expression in cultured renal collecting
duct principal cells. Am J Physiol Renal Physiol 288: F334-F344.
8. Liamis G, Gianoutsos C, Elisaf MS (2009) Hyperosmolar nonketotic syndrome
with hypernatremia: how can we monitor treatment? Diabetes Metab 26: 403- 22. Adrogue HJ, Madias NE (2012) The challenge of hyponatremia. J Am Soc
405. Nephrol 23: 1140-1148.
9. Goldwasser P, Ayoub I, Barth RH (2015) Pseudohypernatremia and 23. Adrogue HJ, Madias NE (2014) Diagnosis and treatment of hyponatremia. Am
pseudohyponatremia: a linear correction. Nephrol Dial Transplant 30: 252-257. J Kidney Dis 64: 681-684.
10. Liamis G, Liberopoulos E, Barkas F, Elisaf M (2013) Spurius electrolyte 24. Liamis G, Filippatos TD, Elisaf MS (2015) Correction of hypovolemia with
disorders: a diagnostic challenge for clinicians. Am J Nephrol 38: 50-57. crystalloid fluids: Individualizing infusion therapy. Postgrad Med 127: 405-412.
11. Weisberg LS (1989) Pseudohyponatremia: a reappraisal. Am J Med 86: 315- 25. Verbalis JG, Goldsmith SR, Greenberg A, Korzelius C, Schrier RW (2013)
318. Diagnosis, evaluation, and treatment of hyponatremia: expert panel
recommendations. Am J Med 126: S1-42.
12. Turchin A, Seifter JL, Seely EW (2003) Clinical problem-solving. Mind the gap.
N Engl J Med 349: 1465-1469. 26. Kallakatta RN, Radhakrishnan A, Fayaz RK, Unnikrishnan JP, Kesavadas C,
et al. (2011) Clinical and functional outcome and factors predicting prognosis
13. Lai MY, Lin CC, Chung SL, Wu CH, Yang WC, et al. (2009) Milky plasma, in osmotic demyelination syndrome (central pontine and / or extrapontine
diabetes, and severe hyponatremia. Kidney Int 75: 996. myelinolysis) in 25 patients. J Neurol Neurosurg Psychiatry 82: 326-331.
Submit your next manuscript and get advantages of OMICS
Group submissions
Unique features:
• User friendly/feasible website-translation of your paper to 50 world’s leading languages
• Audio Version of published paper
• Digital articles to share and explore
Special features:
• 400 Open Access Journals
• 30,000 editorial team
• 21 days rapid review process
• Quality and quick editorial, review and publication processing
• Indexing at PubMed (partial), Scopus, EBSCO, Index Copernicus and Google Scholar etc
• Sharing Option: Social Networking Enabled
Citation: Liamis G, Tsimihodimos V, Elisaf M (2015) Hyponatremia in Diabetes • Authors, Reviewers and Editors rewarded with online Scientific Credits
Mellitus: Clues to Diagnosis and Treatment. J Diabetes Metab 6: 560. • Better discount for your subsequent articles
doi:10.4172/2155-6156.1000560 Submit your manuscript at: www.editorialmanager.com/acrgroup
J Diabetes Metab Volume 6 • Issue 6 • 1000560
ISSN: 2155-6156 JDM, an open access journal
You might also like
- Notes: Mohon Untuk Tidak Mengedit Data Pada Cell Yang Berwarna Abu-Abu! No Po Nama No Mesin No PolisiDocument6 pagesNotes: Mohon Untuk Tidak Mengedit Data Pada Cell Yang Berwarna Abu-Abu! No Po Nama No Mesin No PolisiHastri AdheNo ratings yet
- Notes: Mohon Untuk Tidak Mengedit Data Pada Cell Yang Berwarna Abu-Abu! No Po Nama No Mesin No Polisi No STNKDocument2 pagesNotes: Mohon Untuk Tidak Mengedit Data Pada Cell Yang Berwarna Abu-Abu! No Po Nama No Mesin No Polisi No STNKHastri AdheNo ratings yet
- Notes: Mohon Untuk Tidak Mengedit Data Pada Cell Yang Berwarna Abu-Abu! No Po Nama No Mesin No Polisi No STNKDocument2 pagesNotes: Mohon Untuk Tidak Mengedit Data Pada Cell Yang Berwarna Abu-Abu! No Po Nama No Mesin No Polisi No STNKHastri AdheNo ratings yet
- JCN 5 11Document9 pagesJCN 5 11AlsyNo ratings yet
- Notes: Mohon Untuk Tidak Mengedit Data Pada Cell Yang Berwarna Abu-Abu! No Po Nama No Mesin No PolisiDocument2 pagesNotes: Mohon Untuk Tidak Mengedit Data Pada Cell Yang Berwarna Abu-Abu! No Po Nama No Mesin No PolisiHastri AdheNo ratings yet
- JCN 5 11Document9 pagesJCN 5 11AlsyNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Vijaya DiagnosticsDocument2 pagesVijaya DiagnosticsshelharNo ratings yet
- Anti Diabetic DrugDocument45 pagesAnti Diabetic DrugRahul LokhandeNo ratings yet
- De Guzman, Cameron Josh B. APRIL 26, 2021 2BSN-B RLENCM109Document4 pagesDe Guzman, Cameron Josh B. APRIL 26, 2021 2BSN-B RLENCM109Cameron De GuzmanNo ratings yet
- Home Management of Cats and Dogs With Diabetes Mellitus: Common Questions Asked Veterinarians and ClientsDocument7 pagesHome Management of Cats and Dogs With Diabetes Mellitus: Common Questions Asked Veterinarians and ClientsOnur BalNo ratings yet
- 406-Article Text-988-1-10-20191125Document6 pages406-Article Text-988-1-10-20191125Inggrid WijayantiNo ratings yet
- Centre ListDocument22 pagesCentre ListJaswant SinghNo ratings yet
- Prevention and Control of Diabetes MellitusDocument3 pagesPrevention and Control of Diabetes MellituspeterNo ratings yet
- Effects of Cucurbita Ficifolia Intake On Type 2 Diabetes: Review of Current EvidencesDocument4 pagesEffects of Cucurbita Ficifolia Intake On Type 2 Diabetes: Review of Current EvidencesAnindita Putri WardaniNo ratings yet
- Improving Elderly Care in The GambiaDocument7 pagesImproving Elderly Care in The GambiakoromakNo ratings yet
- Discussion QuestionsDocument2 pagesDiscussion QuestionsMary RiasNo ratings yet
- Nclex RN 2020 Nclex RN Study Guide Review and Practice Questions With RationalesDocument38 pagesNclex RN 2020 Nclex RN Study Guide Review and Practice Questions With Rationalespelftullibeecf7g100% (10)
- High Blood Pressure Screening PackageDocument1 pageHigh Blood Pressure Screening PackageAlita PalpialyNo ratings yet
- T2D Patient Impowerment PDFDocument11 pagesT2D Patient Impowerment PDFRafikNo ratings yet
- Management of Anesthesia: Diabetes MellitusDocument29 pagesManagement of Anesthesia: Diabetes MellitusHari PrasadNo ratings yet
- Herbal Medicine For DiabetesDocument5 pagesHerbal Medicine For Diabetesaguiar.rui9472No ratings yet
- Diabetic Ketoacidosis Care GuidelineDocument5 pagesDiabetic Ketoacidosis Care GuidelineRahma DhNo ratings yet
- Health Improvement Benefits ApprovalDocument1 pageHealth Improvement Benefits ApprovalPloverNo ratings yet
- GinsengDocument38 pagesGinsengBilici Ecaterina0% (1)
- Diabetes MellitusDocument17 pagesDiabetes MellitusRuqayya KobatteNo ratings yet
- Clinical Use of Insulin Degludec in T2DMDocument13 pagesClinical Use of Insulin Degludec in T2DMTaufiqurrokhman RofiiNo ratings yet
- Diabetes MellitusDocument2 pagesDiabetes MellitusElyas MehdarNo ratings yet
- Association Between Outdoor Light and High Risk of DiabetesDocument3 pagesAssociation Between Outdoor Light and High Risk of DiabetesSamaa ahmedNo ratings yet
- ALPRAZOLAM .-WPS OfficeDocument10 pagesALPRAZOLAM .-WPS OfficeMohamed TarekNo ratings yet
- Proceedings of the 36th World Small Animal Veterinary Congress on Canine Diabetes MellitusDocument6 pagesProceedings of the 36th World Small Animal Veterinary Congress on Canine Diabetes MellitusLauura Cristina BarriosNo ratings yet
- Diabetes Questionnaire GuideDocument1 pageDiabetes Questionnaire Guideashmeet bansalNo ratings yet
- Health Assessment - Case StudyDocument2 pagesHealth Assessment - Case StudySamantha Aquino100% (2)
- A Fuzzy Controller For Blood Glucose-Insulin SysteDocument7 pagesA Fuzzy Controller For Blood Glucose-Insulin SysteBrasoveanu Gheorghita100% (1)
- Managing Diabetes: Goals, Treatment, and Patient EducationDocument33 pagesManaging Diabetes: Goals, Treatment, and Patient EducationGodzilla555No ratings yet
- English Task 3Document6 pagesEnglish Task 3I Kadek Adi Putra Suandana 2005No ratings yet
- Insulin Pump Therapy Vs InjectionsDocument6 pagesInsulin Pump Therapy Vs InjectionsHakan KüçükerNo ratings yet