Professional Documents
Culture Documents
Inpatientpathway PDF
Uploaded by
Luis Fernando SaraviaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Inpatientpathway PDF
Uploaded by
Luis Fernando SaraviaCopyright:
Available Formats
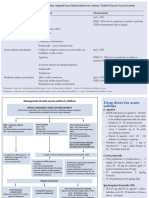
Pediatric Acute Asthma Pathway - Inpatient Care JUNE 2008
Inpatient Assessment Score (Modified PRAM†)
Signs 0 1 2 3
Suprasternal absent present
Indrawing
Scalene absent present
Retractions
Wheezing absent expiratory only inspiratory & expiratory audible without
stethoscope/silent chest
Air Entry normal decreased at bases widespread decrease absent/minimal
Phase Change Criteria: SCORE of < 3 at routine assessment or MD order on reassessment in
Phase I or Phase II (all phase changes require verbal or written MD order).
For β2 Agonist assessment: if SCORE ≥ 3 give β2 Agonist, if < 3 no β2 Agonist.
For any assessment SCORE ≥ 6, give β2 Agonist and notify MD. If in Phase II or Phase III
*Deterioration on Inpatient Ward: move back to previous phase. If in Phase I consider further investigations, reassess therapy (β2
Agonist frequency, IV, oxygen etc.) and consider ICU consultation if not responding to treatment. ABBREVIATIONS:
Consider the following treatment/investigations depending on patient status and response to therapy: ACH - Alberta Children’s Hospital; ED - Emergency Department; ICU - Intensive Care Unit;
Pathway Inclusion: Age 1-18 years with asthma; 1st time wheeze if diagnosis is likely
1. Aerosolized β2 Agonist +/– Ipratropium aerosols x 3 back to back or q20 minutes. asthma; NOT bronchiolitis; NOT pneumonia unless the pneumonia is felt to be a more MDI - Metered Dose Inhaler; ICS - Inhaled Corticosteroid; DPI - Dry Powder Inhaler
2. IV steroid (if on po) Dose: methylprednisolone 1-2mg/kg then 1-2mg/kg/day divided q6 hours minor issue compared to the asthma.
(max dose 80mg/day or 80mg/dose for first dose). DRUGS:
Pathway Entry on Admission: MD to determine Phase to enter on admission based on Fluticasone (Flovent) Ciclesonide (Alvesco)
3. Capillary blood gas and chest x-ray. response to treatment prior to admission.
ICU consultation suggested when patient continues to deteriorate despite interventions or if patient is Beclomethasone (QVAR) Budesonide + Formoterol (Symbicort)
† Excludes O2 saturation
continuing to require at least q30 minute aerosolized β2 Agonist for ≥ 2 hours. Budesonide (Pulmicort) Fluticasone + Salmeterol (Advair)
Pediatric Acute Asthma Pathway - Inpatient Care JUNE 2008
Summary of Orders and Inpatient Pathway for Phase I: Summary of Orders and Inpatient Pathway for Phase II: Summary of Orders and Inpatient Pathway for Phase III:
1. Diet / Fluids / Electrolytes 1. Diet / Fluids / Electrolytes 1. Diet / Fluids / Electrolytes
• Diet: If on q1 hour aerosolized β2 Agonist consider clear fluids until in Phase II. NPO if not • Diet as tolerated for most patients. • Diet as tolerated for most patients.
tolerating po intake or if deteriorating (possible ICU). Resume po intake as soon as possible. 2. Oxygen 2. Oxygen
• Fluids: If vomiting, dehydration, poor intake or prolonged need for q1 hour aerosolized β2 Agonist: IV • Suggest to keep sats ≥ 93% during Phase I and Phase II. Periodic saturation checks q8 hours and prn • Once in Phase III, O2 to keep sat ≥ 90% as long as there is no increased work of breathing.
fluid as needed. D5/0.45 with 20mEq KCl/L (30-40mEq KCl/L if K+ is low). Reduce and discontinue before aerosolized β2 Agonist. 3. Prednisone 1-2mg/kg (max 60mg) po for 5 days total or Dexamethasone
IV as soon as oral intake improves. • Once in Phase III, O2 to keep sat ≥ 90% as long as there is no increased work of breathing. 0.15-0.3mg/kg/dose (max 10mg). Five days of dexamethasone suggested although
• Electrolytes: If frequent aerosolized β2 Agonist in ED or on ward, consider labs to check K+.
3. Prednisone 1-2mg/kg (max 60mg) po for 5 days total or Dexamethasone literature is insufficient to support a particular length of treatment.
If needing at least maintenance IV fluid, electrolyte check q24 hours recommended.
0.15-0.3mg/kg/dose (max 10mg). Five days of dexamethasone suggested although • A longer course of therapy may be indicated for those on oral steroid recently prior to admission or if
2. Oxygen literature is insufficient to support a particular length of treatment. response to therapy has been slow.
• Suggest to keep sats ≥ 93% in Phase I and Phase II. Periodic saturation checks q8 hours and prn • Only if unable to tolerate po: IV methylprednisolone 1-2mg/kg load and then 1-2mg/kg/day 4. Pathway Entry/Assessment of Clinical Status
before aerosolized β2 Agonist. (max 80mg/day) divided q6 hours. Discontinue once oral tolerated and start oral steroids. • Modified PRAM score is used to determine if aerosolized β2 Agonist treatment needed.
• Once in Phase III, O2 to keep sat ≥ 90% as long as there is no increased work of breathing. • A longer course of therapy may be indicated for those on oral steroid recently prior to admission or if • Vital signs: RR, HR to be done with each assessment, BP routine.
3. Prednisone 1-2mg/kg (max 60mg) po for 5 days total or Dexamethasone response to therapy has been slow. • FEV1 recommended for patients ≥ age 6 for those capable of spirometry, suggest once or twice per
0.15-0.3mg/kg/dose (max 10mg). Five days of dexamethasone suggested although 4. Pathway Entry/ Assessment of Clinical Status day and prior to discharge.
literature is insufficient to support a particular length of treatment. • Modified PRAM score is used to determine if aerosolized β2 Agonist treatment is needed. • If patient is being admitted to Phase III Entry Point “A”. First assessment is 2 hours after
• Only if unable to tolerate po: IV methylprednisolone 1-2mg/kg load and then 1-2mg/kg/day • Vital signs: RR, HR to be done with each assessment, BP routine. last aerosolized β2 Agonist and then 4 hours after the last aerosolized β2 Agonist then every 4 hours.
(max 80mg/day) divided q6 hours. Discontinue once oral tolerated and start oral steroids. • FEV1 recommended for patients ≥ age 6 for those capable of spirometry, suggest once or twice per • If patient is being moved from Phase II to Phase III Entry Point “B”. First assessment is
• A longer course of therapy may be indicated for those on oral steroids recently prior to admission or day and prior to discharge. 4 hours after last aerosolized β2 Agonist then every 4 hours.
if response to therapy has been slow. • If patient is being admitted into Phase II Entry Point “A”. First assessment is one hour after last • Repeat assessment after aerosolized β2 Agonist (15-30 minutes post), noting response to treatment on
4. Pathway Entry/ Assessment of Clinical Status aerosolized β2 Agonist (prn assessment) then 2 hours after last aerosolized β2 Agonist then every assessment form.
• Modified PRAM score is used to determine if aerosolized β2 Agonist treatment is needed. 2 hours as long as aerosolized β2 Agonist required (score ≥ 3). • If on assessment 4 hours after last aerosolized β2 Agonist score is < 3, give aerosolized β2
• Vital signs: RR, HR to be done with each assessment, BP routine. • If patient is being moved from Phase I to Phase II Entry Point “B”. First assessment is done Agonist. Patient is ready for potential discharge (see below). If there is a delay in discharge – assess
• FEV1 recommended for patients ≥ age 6 for those capable of spirometry, suggest once or twice per 2 hours after last aerosolized β2 Agonist then every 2 hours as long aerosolized β2 Agonist every 4 hours and aerosolized β2 Agonist to be given every 4 hours as a minimum.
day and prior to discharge. required (score ≥ 3). • If score ≥ 6, notify MD and return to Phase II Entry Point “A”.
• If patient is being admitted into Phase I Entry Point “A”. • Repeat assessment after aerosolized β2 Agonist (15-30 minutes post), noting response to treatment on 5. β2 Agonist Therapy by MDI/Spacer is strongly recommended.
• First assessment is to be done 30 minutes after last aerosolized β2 Agonist then every 30 minutes or assessment form. • Dose: 100mcg/puff. Once in Phase III reduce to 5 puffs/dose for all weights.
1 hour as per pathway (see algorithm). • If on assessment 2 hours after aerosolized β2 Agonist, score is < 3, do not give aerosolized β2 Agonist. • If less effective, increase by 1-2 puff/dose; if increased side effects (HR, jittery), decrease by 1-2
• Repeat assessment after aerosolized β2 Agonist (15-30 minutes post), noting response to treatment on Patient is ready to move to Phase III Entry Point “B” (needs MD order). puff/dose.
assessment form. • If score ≥ 6, notify MD and return to Phase I Entry Point “A”. • Max MDI dose 10 puffs.
• If on assessment 1 hour after aerosolized β2 Agonist, score < 3, do not give aerosolized β2 Agonist. • Once in Phase III, can switch to home aerosolized β2 Agonist and ICS device if not being discharged
5. β2 Agonist Therapy by MDI/Spacer is strongly recommended. with MDI and spacer. Note: Ventolin Diskus and Bricanyl Turbuhaler 1 puff = 2 puffs aerosolized β2
Patient is ready to move to Phase II Entry Point “B” (needs MD order). • Dose: 100mcg/puff weight < 20kg 5 puffs/dose; ≥ 20kg 10 puffs/dose. Once in Phase III reduce to
• If on assessment patient is requiring aerosolized β2 Agonist every 30 minutes on 3 subsequent Agonist MDI (Alternate: Nebulization dose 2.5mg/dose for < 20kg and 5mg/dose for ≥ 20kg).
5 puffs/dose for all weights.
assessments or if on assessment score is ≥ 6, MD involvement is needed to decide course of therapy • If less effective, increase by 1-2 puff/dose; if increased side effects (HR, jittery), decrease by 6. Long Acting β2 Agonists or Leukotriene Receptor Antagonists
which will vary depending on the clinical situation (see algorithm for considerations when patient is 1-2 puff/dose. • Continue usual maintenance therapy.
deteriorating). • Max MDI dose 10 puffs 7. Inhaled Corticosteroid
5. β2 Agonist Therapy by MDI/Spacer is strongly recommended. (Alternate: Nebulization dose 2.5mg/dose for < 20kg and 5mg/dose for ≥ 20kg). • Usual therapy should continue in hospital. If no maintenance therapy, begin as soon as possible.
• Dose: 100mcg/puff weight < 20kg 5 puffs/dose; ≥ 20kg 10 puffs/dose. Once in Phase III reduce to 6. Long Acting β2 Agonists or Leukotriene Receptor Antagonists • Suggested dosing in hospital if not previously using daily ICS:
5 puffs/dose for all weights. • Continue usual maintenance therapy. Flovent MDI (125mcg) 2 puffs BID OR QVAR MDI (100mcg) 2 puffs BID OR Pulmicort Turbuhaler
• If less effective, increase by 1-2 puff/dose; if increased side effects (HR, jittery), decrease by 1-2 (200mcg) 2 puffs BID OR Flovent Diskus (100mcg) 2 puffs BID OR Alvesco MDI (200 mcg) 1 puff BID.
puff/dose. 7. Inhaled Corticosteroid
• Usual therapy should continue in hospital. If no maintenance therapy, begin as soon as possible. 8. Investigations/Antibiotics
• Max MDI dose 10 puffs (Alternate: Nebulization dose 2.5mg/dose for < 20kg and 5mg/dose for ≥ 20kg). • CXR – only if atypical presentation; deterioration after admission; suspected pneumonia.
• Suggested dosing in hospital if not previously using daily ICS:
6. Ipratropium • Capillary blood gas – if deterioration; altered mental status; underlying chronic lung disease.
Flovent MDI (125mcg) 2 puffs BID OR QVAR MDI (100mcg) 2 puffs BID OR Pulmicort Turbuhaler
• Not recommended routinely for inpatient therapy BUT may be used in asthmatic patient who is • CBC, cultures – if high fever; toxic appearance; clinical deterioration.
(200mcg) 2 puffs BID OR Flovent Diskus (100mcg) 2 puffs BID OR Alveso MDI (200 mcg) 1 puff BID
severe or deteriorating after admission. • Antibiotics – if definite pneumonia, sinusitis, otitis media.
• Dose: MDI 5 puffs/dose for all weights, one dose with each aerosolized β2 Agonist treatment x 3. 8. Investigations/Antibiotics 9. Asthma Education
• CXR – only if atypical presentation; deterioration after admission; suspected pneumonia.
7. Long Acting β2 Agonists or Leukotriene Receptor Antagonists • Capillary blood gas – if deterioration; altered mental status; underlying chronic lung disease.
• Should be completed for all inpatients, best done in Phase II or Phase III.
• Continue usual maintenance therapy. • Consider referral for asthma education.
• CBC, cultures – if high fever; toxic appearance; clinical deterioration.
8. Inhaled Corticosteroid • Antibiotics – if definite pneumonia, sinusitis, otitis media. 10. Discharge Criteria:
• Usual therapy should continue in hospital. If no maintenance therapy, begin as soon as possible. • Score < 3 on assessment 4 hours after last treatment or 12 hours in Phase III.
9. Asthma Education • Off oxygen, saturations > 90%.
• Suggested dosing in hospital if not previously using daily inhaled cortcosteroid (ICS): Flovent MDI • Should be ordered for all inpatients, best done in Phase II or Phase III.
(125mcg) 2 puffs BID OR QVAR MDI (100mcg) 2 puffs BID OR Pulmicort Turbuhaler (200mcg) 2 puffs • Asthma education completed.
• Consider referral for asthma education. • Family able to continue treatment at home.
BID OR Flovent Diskus (100mcg) 2 puffs BID OR Alvesco MDI (200 mcg) 1 puff BID.
10. Consultation – Pediatric Pulmonary Consultation if • Follow-up arranged.
9. Investigations/Antibiotics • ICU admission. • Discharge action plan completed and communicated to family and community physician.
• CXR – only if atypical presentation; deterioration after admission; suspected pneumonia. • Regularly followed by Pulmonary Service or Asthma Clinic. • Discharge instructions given to family (triplicate asthma form).
• Capillary blood gas – if deterioration; altered mental status; underlying chronic lung disease. • Prescriptions given (triplicate asthma form).
• CBC, cultures – if high fever; toxic appearance; clinical deterioration. Consider Consultation if
• Antibiotics – if definite pneumonia, sinusitis, otitis media. • Severe exacerbation.
• Historical features suggestive of poor outpatient management.
10. Asthma Education ABBREVIATIONS:
• Should be ordered for all inpatients, best done in Phase II or Phase III. ACH - Alberta Children’s Hospital; ED - Emergency Department; ICU - Intensive Care Unit;
• Consider referral for asthma education. MDI - Metered Dose Inhaler; ICS - Inhaled Corticosteroid; DPI - Dry Powder Inhaler
11. Consultation – Pediatric Pulmonary Consultation if
DEVICE RECOMMENDATIONS:
• ICU admission. DRUGS:
• Regularly followed by Pulmonary Service or Asthma Clinic.
• MDI/Spacer with mask 0-4 years Fluticasone (Flovent) Ciclesonide (Alvesco)
• MDI/Spacer with mouthpiece 4-6 years Beclomethasone (QVAR) Budesonide + Formoterol (Symbicort)
Consider Consultation if
• Severe exacerbation.
• DPI > 6 years Budesonide (Pulmicort) Fluticasone + Salmeterol (Advair)
• Historical features suggestive of poor outpatient management.
You might also like
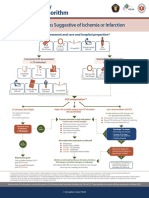
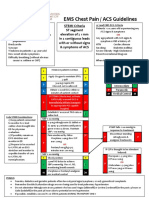
- Syndroms Suggestive of Ischemia or Infarction: EMS Assessment and Care and Hospital PrepartionDocument1 pageSyndroms Suggestive of Ischemia or Infarction: EMS Assessment and Care and Hospital PrepartionAnonymous CKAborxxwNo ratings yet
- Syndroms Suggestive of Ischemia or Infarction: EMS Assessment and Care and Hospital PrepartionDocument8 pagesSyndroms Suggestive of Ischemia or Infarction: EMS Assessment and Care and Hospital PrepartionNugroho TeguhNo ratings yet
- Syndromes Suggestive of Ischemia or Infarction: EMS Assessment and Care and Hospital PreparationDocument1 pageSyndromes Suggestive of Ischemia or Infarction: EMS Assessment and Care and Hospital Preparationgusti angri angalanNo ratings yet
- Posters For ClinicDocument80 pagesPosters For ClinicdenzkissaieNo ratings yet
- Acute Coronary Syndromes Algorithm: Patient Has Signs Suggestive of Ischemia or InfarctionDocument1 pageAcute Coronary Syndromes Algorithm: Patient Has Signs Suggestive of Ischemia or Infarctionjohndoe1995No ratings yet
- Acut Coronary SyndromesDocument1 pageAcut Coronary SyndromesMuhittin Selçuk ÖzkanNo ratings yet
- Algo Acs PDFDocument1 pageAlgo Acs PDFJim Christian EllaserNo ratings yet
- Algo Acs PDFDocument1 pageAlgo Acs PDFNety Pandung SalembanNo ratings yet
- Paediatric Guidelines Croup 2020Document4 pagesPaediatric Guidelines Croup 2020nimraNo ratings yet
- ASTHMA - SemisDocument4 pagesASTHMA - SemisInday BertaNo ratings yet
- Acute Asthma - Care in The Emergency DepartmentDocument5 pagesAcute Asthma - Care in The Emergency DepartmentTanitNo ratings yet
- Ventolin DrugstudyDocument1 pageVentolin DrugstudyMsOrangeNo ratings yet
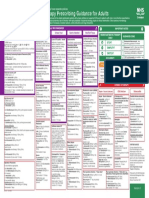
- Empirical Antimicrobial Therapy Prescribing Guidance For AdultsDocument1 pageEmpirical Antimicrobial Therapy Prescribing Guidance For AdultsPsychology TodayNo ratings yet
- Name of DrugDocument5 pagesName of DrugJoann BeriñoNo ratings yet
- Bronchospasm Child: PO 2-6 Y, 0.1-: 0.2 MG/KG T.I.D. (Max: 4 Mg/dose) 6-12 Y, 2 MG 3-4 Times/dDocument2 pagesBronchospasm Child: PO 2-6 Y, 0.1-: 0.2 MG/KG T.I.D. (Max: 4 Mg/dose) 6-12 Y, 2 MG 3-4 Times/dArnold De Guzman Jr.No ratings yet
- Syndromes Suggestive of Ischemia or Infarction: EMS Assessment and Care and Hospital PreparationDocument1 pageSyndromes Suggestive of Ischemia or Infarction: EMS Assessment and Care and Hospital PreparationIGOR SHEYNINNo ratings yet
- AsthmaDocument2 pagesAsthmaAndrei MurariuNo ratings yet
- Cardiology STEMIDocument1 pageCardiology STEMIAishwarya WadikarNo ratings yet
- Assignment On Antibiotics - ViosDocument8 pagesAssignment On Antibiotics - ViosIra Velle ViosNo ratings yet
- DRUG STUDY (Groupings) - YASMIEN MARIEDocument21 pagesDRUG STUDY (Groupings) - YASMIEN MARIEYasmien MarieNo ratings yet
- Medical Emergencies Handouts KhannaDocument15 pagesMedical Emergencies Handouts KhannaharryNo ratings yet
- Luka Bakar Poster PDFDocument1 pageLuka Bakar Poster PDFnurisumirizqiNo ratings yet
- Drug Study ICUDocument2 pagesDrug Study ICUErryl Justine AdvinculaNo ratings yet
- Acute Asthma ExacerbationDocument2 pagesAcute Asthma ExacerbationChinenye ModestaNo ratings yet
- Asystole/PEA: Epinephrine 0.1 ML/KG ASAPDocument1 pageAsystole/PEA: Epinephrine 0.1 ML/KG ASAPAlejandro MusaNo ratings yet
- Acs PDFDocument1 pageAcs PDFPowool LalaNo ratings yet
- Ncp-Drug StudyDocument2 pagesNcp-Drug StudyMark oliver GonzalesNo ratings yet
- GROUP1 Drug Therapeutic RecordDocument6 pagesGROUP1 Drug Therapeutic RecordYori Nicole Martine CuyosNo ratings yet
- Asthma and Inhaler 20201203Document29 pagesAsthma and Inhaler 20201203松山內科部No ratings yet
- NCP Rds 2Document1 pageNCP Rds 2Angelokeizer Gavino0% (1)
- Asthma WorksheetDocument5 pagesAsthma WorksheetÀi ZìjǐNo ratings yet
- Adenosine: Facial Flushing, SweatingDocument26 pagesAdenosine: Facial Flushing, SweatingAnna Sofia ReyesNo ratings yet
- Asthma (Acute) Management - Children (Pediatrics)Document2 pagesAsthma (Acute) Management - Children (Pediatrics)Itharshan IndreswaranNo ratings yet
- BCCH ED Croup Algorithm 2012Document1 pageBCCH ED Croup Algorithm 2012john morzNo ratings yet
- COVID - Management 14 April 2021Document20 pagesCOVID - Management 14 April 2021Zain ZaidiNo ratings yet
- Ecg ReadingsDocument11 pagesEcg ReadingsAnton Laurenciana100% (5)
- Emergency Department Procedural Sedation and Analgesia Physician ChecklistDocument2 pagesEmergency Department Procedural Sedation and Analgesia Physician ChecklistcalstudyNo ratings yet
- Nicolas, Krizha-Drug StudyDocument12 pagesNicolas, Krizha-Drug StudyKrizha Angela NicolasNo ratings yet
- Assessment Nursing Diagnosis Planning Intervention Rationale EvaluationDocument7 pagesAssessment Nursing Diagnosis Planning Intervention Rationale EvaluationEula ReyesNo ratings yet
- Drug Study: Sympathomime Tic, Beta2-Selective Adrenergic Agonist, Bronchodilator, AntiasthmaticDocument3 pagesDrug Study: Sympathomime Tic, Beta2-Selective Adrenergic Agonist, Bronchodilator, AntiasthmaticJichutreasure100% (1)
- Drug StudyDocument22 pagesDrug StudyShenna RegaspiNo ratings yet
- EMS Chest Pain / ACS GuidelinesDocument1 pageEMS Chest Pain / ACS GuidelinesJuanaly BadiolaNo ratings yet
- Respi Drugs 1Document10 pagesRespi Drugs 1TpdNo ratings yet
- AsthmaDocument2 pagesAsthmaNurliyana GhazaliNo ratings yet
- Procedural SedationDocument9 pagesProcedural SedationZayar SweNo ratings yet
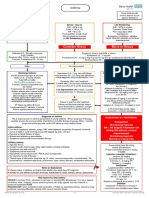
- Managing Acute Asthma in Adults - Final160123Document1 pageManaging Acute Asthma in Adults - Final160123Stri LokaNo ratings yet
- Risk For Ineffective Airway Clearance 1Document8 pagesRisk For Ineffective Airway Clearance 1kint manlangitNo ratings yet
- Croup Summary PDFDocument2 pagesCroup Summary PDFnurfitriaNo ratings yet
- Pediatric Guidelines: Head and Neck Infections - MastoiditisDocument3 pagesPediatric Guidelines: Head and Neck Infections - MastoiditisJr SparkNo ratings yet
- AclsDocument1 pageAclsJoice DasNo ratings yet
- F-IMNCI Chart BookletDocument45 pagesF-IMNCI Chart BookletGunda SrinivasNo ratings yet
- AAH v2 Acute AsthmaDocument81 pagesAAH v2 Acute AsthmaEssa SmjNo ratings yet
- Generalised Ultimate Loads For Pile GroupsDocument22 pagesGeneralised Ultimate Loads For Pile GroupsValerioNo ratings yet
- Course Specifications: Fire Investigation and Failure Analysis (E901313)Document2 pagesCourse Specifications: Fire Investigation and Failure Analysis (E901313)danateoNo ratings yet
- DGA Furan AnalysisDocument42 pagesDGA Furan AnalysisShefian Md Dom100% (10)
- Tours and Travel MNGTDocument16 pagesTours and Travel MNGTArpita Jaiswal100% (5)
- Trandsend 2Document3 pagesTrandsend 2dadiNo ratings yet
- Teacher Resource Disc: Betty Schrampfer Azar Stacy A. HagenDocument10 pagesTeacher Resource Disc: Betty Schrampfer Azar Stacy A. HagenRaveli pieceNo ratings yet
- Read The Text and Answer The QuestionsDocument5 pagesRead The Text and Answer The QuestionsDanny RuedaNo ratings yet
- GP 43-45-DRAFT - Site RestorationDocument48 pagesGP 43-45-DRAFT - Site Restorationmengelito almonte100% (1)
- Transportation Engineering Unit I Part I CTLPDocument60 pagesTransportation Engineering Unit I Part I CTLPMadhu Ane NenuNo ratings yet
- MY-SDK-10000-EE-005 - Method Statement For Concrete Pole Installation - GVB Rev1Document7 pagesMY-SDK-10000-EE-005 - Method Statement For Concrete Pole Installation - GVB Rev1Seeths NairNo ratings yet
- The Way of The Samurai, Shadowrun BookDocument19 pagesThe Way of The Samurai, Shadowrun BookBraedon Montgomery100% (8)
- E10.unit 3 - Getting StartedDocument2 pagesE10.unit 3 - Getting Started27. Nguyễn Phương LinhNo ratings yet
- What Is The Effective Method For Dissolution of HDPE and LDPE - PDFDocument12 pagesWhat Is The Effective Method For Dissolution of HDPE and LDPE - PDFAliNo ratings yet
- Jose André Morales, PH.D.: Ingeniería SocialDocument56 pagesJose André Morales, PH.D.: Ingeniería SocialJYMYNo ratings yet
- Opening The Third EyeDocument13 pagesOpening The Third EyekakamacgregorNo ratings yet
- Python PyDocument19 pagesPython Pyakhilesh kr bhagatNo ratings yet
- Perrys Chemical Engineering Handbook 7th Edition PriceDocument3 pagesPerrys Chemical Engineering Handbook 7th Edition PriceSteven Valentius0% (12)
- Esp-2000 BSDocument6 pagesEsp-2000 BSByron LopezNo ratings yet
- Practice Problems For Modulus and Logarithm Section-I: FiitjeeDocument8 pagesPractice Problems For Modulus and Logarithm Section-I: FiitjeePratham SharmaNo ratings yet
- Hung201 PDFDocument14 pagesHung201 PDFMua Dong Tuyet RoiNo ratings yet
- Updated PDPDocument540 pagesUpdated PDPnikulaaaasNo ratings yet
- My Report in Assessment 1Document67 pagesMy Report in Assessment 1Eddie Wilson BroquezaNo ratings yet
- Put Them Into A Big Bowl. Serve The Salad in Small Bowls. Squeeze Some Lemon Juice. Cut The Fruits Into Small Pieces. Wash The Fruits. Mix The FruitsDocument2 pagesPut Them Into A Big Bowl. Serve The Salad in Small Bowls. Squeeze Some Lemon Juice. Cut The Fruits Into Small Pieces. Wash The Fruits. Mix The FruitsNithya SweetieNo ratings yet
- E34-1 Battery Charging and Dishcharging BoardDocument23 pagesE34-1 Battery Charging and Dishcharging BoardGanesa MurthyNo ratings yet
- English ExerciseDocument2 pagesEnglish ExercisePankhuri Agarwal100% (1)
- Mineral Claim Purchase and Sale Agreement FinalDocument5 pagesMineral Claim Purchase and Sale Agreement Finaldaks4uNo ratings yet
- EverServ 7700 M77XX Quick Reference GuideDocument2 pagesEverServ 7700 M77XX Quick Reference GuidetangocharliepdxNo ratings yet
- Mechanical Power FormulaDocument9 pagesMechanical Power FormulaEzeBorjesNo ratings yet
- Lesson Plan Cot1Document9 pagesLesson Plan Cot1Paglinawan Al KimNo ratings yet
- W1 - V1 MultipleWorksheets SolnDocument3 pagesW1 - V1 MultipleWorksheets SolnAKHIL RAJ SNo ratings yet