Professional Documents
Culture Documents
Frequency of Risk Factors of Stroke in Patients Presenting To Public Sector Hospitals of Lahore
Uploaded by
iajpsOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Frequency of Risk Factors of Stroke in Patients Presenting To Public Sector Hospitals of Lahore
Uploaded by
iajpsCopyright:
Available Formats
IAJPS 2018, 05 (05), 3884-3893 Ammara Ijaz Rana et al ISSN 2349-7750
CODEN [USA]: IAJPBB ISSN: 2349-7750
INDO AMERICAN JOURNAL OF
PHARMACEUTICAL SCIENCES
http://doi.org/10.5281/zenodo.1248876
Available online at: http://www.iajps.com Research Article
FREQUENCY OF RISK FACTORS OF STROKE IN PATIENTS
PRESENTING TO PUBLIC SECTOR HOSPITALS OF LAHORE
1
Ammara Ijaz Rana, 2Dr. Ammarah Safdar, 3Junaid Khan Kundi
1
DHQ Hospital Kasur
2
Lahore General Hospital, Lahore
3
Accident and Emergency Unit, DHQ, D.I Khan
Abstract:
Stroke also called as Cerebrovascular accident is a syndrome of rapid onset of cerebral deficit (usually focal)
lasting >24 h or leading to death, with no cause apparent other than a vascular one. It is currently the third leading
cause of death worldwide. It is also the first leading cause of disability globally.
Objective: To find out the frequency of various risk factors of stroke in patients presenting to Medical and
Neurology wards of various public sector hospitals of Lahore.
Study Design: Analytical Cross sectional study.
Study Place: Medical and Neurology wards of public sector hospitals of Lahore.
Study Duration: 4 months (May 2014 to August 2014).
Subjects and Methods:
A Cross-sectional study was conducted in various public sector hospitals of Lahore. A total of hundred subjects
were recruited in the study. Selection was made on laid down criteria, after taking informed consent. Interviews
were conducted through a pretested questionnaire. Data was collected, compiled and analyzed through SPSS.
Keywords: Stroke, transient ischemic attack, hypertension, diabetes, hypercholesterolemia, cardiovascular disease,
obesity, smoking, unhealthy diet, physical inactivity.
Corresponding author:
Ammara Ijaz Rana, QR code
DHQ Hospital,
Kasur
Please cite this article in press Ammara Ijaz Rana et al., Frequency of Risk Factors of Stroke in Patients
Presenting To Public Sector Hospitals of Lahore, Indo Am. J. P. Sci, 2018; 05(05).
www.iajps.com Page 3884
IAJPS 2018, 05 (05), 3884-3893 Ammara Ijaz Rana et al ISSN 2349-7750
INTRODUCTION: oral contraceptives, hypercoaguable states,lifestyle
According to WHO stroke (cerebrovascular accident) factors like reduced physical activity and unhealthy
can be defined as “a syndrome of rapid onset of diet.11Age is the one of the most important risk
cerebral deficit (usually focal) lasting >24 h or factors for stroke. For each successive 10 years after
leading to death, with no cause apparent other than a age 55, stroke rate becomes more than double.
vascular one” [1]. This differentiates a stroke from a Incidence of stroke is 1.25 time higher in men than in
mini stroke or TIA(Transient Ischemic Attack), women. Family history, both paternal and maternal
which lasts less than 24h.Stroke is also called as leads to increased stroke risk [11]. Hypertension
cerebrovascular insult (CVI) or brain attack.A stroke (high blood pressure) increases the risk of stroke by
can be Ischemic (which may be due to any thrombo- 35-50% [18].. Among Hawaiian Japanese men in the
embolic or cardio-embolic event, carotid artery Honolulu Heart Program, those with diabetes had
atherosclerosis, arterial stenosis, arterial dissections, twice the risk of thromboembolic stroke of persons
various types of arteritis, venous sinus thrombosis, without diabetes that was independent of other risk
and hyper-coagulable states) or it can be of the factors [19]. Cigarette smoking increases risk (RR) of
hemorrhagic type in which the actual rupture of a ischemic stroke nearly two times [20]. In a study
blood vessel is taking place. There are two types of done on Korean men there was a positive association
hemorrhagic strokes; intracerebral (within the brain) across the whole range of BMI and ischemic stroke,
hemorrhage or subarachnoid hemorrhage. Two types with a confounder-adjusted hazard of 11% for 1
of weakened blood vessels usually cause kg/m2 higher BMI [15]. Multiple Risk Factor
hemorrhagic stroke: aneurysms and arteriovenous Intervention Trial demonstrated risk ratio of 1.8 for
malformations (AVMs) however the most common those with serum cholesterol 240 to 279 mg/dL and
cause of hemorrhagic stroke is uncontrolled 2.6 for those with cholesterol levels ≥280 mg/Dl [21].
hypertension (high blood pressure).2Stroke is a The Framingham Heart Study noted a dramatic
medical emergency and can result in permanent increase in stroke risk associated with atrial
defecit. fibrillation with advancing age, from 1.5% for those
50 to 59 years of age to 23.5% for those 80 to 89
About 15 million people suffer from stroke each year years of age [14].
worldwide [3]. It is currently the third leading cause
of death worldwide. It is also the first leading cause Despite the advent of treatment, the best approach to
of disability globally [4]. minimize the risk of stroke remains prevention.
Hence there is need to study the frequency of major
According to WHO estimates for the year 2020, modifiable and non modifiable risk factors of stroke
stroke will remain the second leading cause of death for the purpose of highlighting individuals prone to
worldwide [5,6]. Estimated annual incidence of stroke. Although some factors like age, gender and
stroke in Pakistan is 250/100,000 which is projected family history cannot be modified, their presence
to an estimate of 350,000 new cases every year [7]. helps identify those at greatest risk, enabling prompt
According to a World Health Organization (WHO) prevention and treatment of those risk factors that can
report from 2002, the total mortality from stroke in be modified; saving many individuals from one of the
Pakistan is more than 75,000 [8]. A handful of leading causes of death while reducing its outcomes
Pakistani hospital based studies, in settings using like paralysis and coma.
advanced investigative approaches such as CT- scan,
have revealed 31-40% cases of stroke due to cerebral OPERATIONAL DEFINITIONS:
hemorrhage, and 60-90% due to ischemia [9,10]. Stroke: A syndrome of rapid onset of cerebral deficit
Mortality data from 2007 indicate that stroke (usually focal) lasting >24 h or leading to death, with
accounted for ≈1 of every 18 deaths in the United no cause apparent other than a vascular one.1
States. On average, every 40 seconds, someone in the Hypertension: A chronic medical condition in which
United States has a stroke [11]. the blood pressure in the arteries is elevated. High
blood pressure is said to be present if it is often at or
Risk factors for stroke can be modifiable and not above 140/90 mmHg.22
modifiable [12]. Non modifiable factors or risk Diabetes: Fasting blood glucose >126mg/dL or
markers include Age, gender, race, ethnicity, and Random blood glucose > 200mg/dL [23]
heredity [11]. Modifiable factors are hypertension Obesity: it is defined as Waist circumference greater
[13], cardiac disease; the most important of which is than 88cm(35 inches) in females and greater than
atrial fibrillation [14] increased BMI [15] diabetes 102cm( 40 inches ) in males measured by standard
[11] TIA [16] cigarette smoking [17] ,hyperlipidemia, plastic tape a point halfway between lowest end of
alcohol consumption,use of illicit drugs, migraine,
www.iajps.com Page 3885
IAJPS 2018, 05 (05), 3884-3893 Ammara Ijaz Rana et al ISSN 2349-7750
ribs and upper end of hipbone that is iliac crest , at Unhealthy diet: Diet which is unhealthy according
the end of gentle expiration [24] to Healthy Diet Score (as defined by American Heart
Hypercholesterolemia: It is defined a blood Association’s strategic impact goal through 2020)that
cholesterol level above 240mg/dL [25] is: it not meeting at least 4 out of 5 components of
Cigarette smoker: US Centers for Disease Control healthy diet. (ideal is score of 4_5 that is 4–5
and Prevention have developed and updated the components of diet are met; e.g., >4.5 cups/day of
following definitions: Former Smokers – Adults who fruits and vegetables) [27]
have smoked at least 100 cigarettes in their lifetime, Family history: Includes both paternal and maternal
but say they currently do not smoke. Current history of stroke that either one or both of the parents
Smokers – Adults who have smoked 100 cigarettes in have had stroke [11].
their lifetime and currently smoke cigarettes every
day (daily) or some days (nondaily). OBJECTIVE:
Lack of ideal physical activity: Lack of minimum To find out the frequency of various risk factors
of 150min of moderate physical activity(for example among stroke patients presenting to medical and
fast walking) or minimum of 75 min of vigorous neurology wards of various public sector hospitals of
intensity physical activity (for example running) a Lahore.
week [27].
MATERIALS AND METHODS:
• Study Design:
Analytical Cross sectional study
• Study Universe:
Population of Punjab
• Study Population:
Lahore
• Study Area:
Medical and Neurological wards of various public sector hospitals of Lahore.
• Study Duration:
Three months
Sample Size:
100
Sampling Technique:
Non-probability convenience sampling
Sampling Selection:
Inclusion Criteria
o Males and females (>25years)
o Diagnosis confirmed with CT scan.
Exclusion Criteria
o People having previous focal lesions in brain will not be included.
o People having non cerebrovascular causes for their symptoms mimicking stroke
will not be included ; for example:
Seizure.
Systemic infection.
Brain tumor.
Toxic metabolic disorder like hypoglycemia and hyponatremia.
Positional vertigo.
Conversion disorder.
Social And Ethical Consideration:
We will observe cultural ethics.
Written informed consent will be taken from individuals before interview.
Information about name, address etc. will not be disclosed and will be kept confidential.
www.iajps.com Page 3886
IAJPS 2018, 05 (05), 3884-3893 Ammara Ijaz Rana et al ISSN 2349-7750
history of stroke. Obesity as defined by waist
DATA COLLECTION PROCEDURE: circumference measured by a standard plastic tape at
Name, age, sex,religion,address, ethnicity, marital a site halfway between lowest end of ribs and upper
status, occupation,education level and monthly end of hipbone that is iliac crest with at the end of
income will be obtained by self-report at the baseline gentle expiration, and hips at the greater trochanters.
visit. Education will be categorized as “intermediate Diet will be assessed using Healthy Diet Score
and onwards”, “formal” and “informal”. Individual defined by American Heart Association’s strategic
monthly income will be reported as: “Less than impact goal through 2020. Physical activity assessed
Rs10,000”, “10,000-<50,000”, “Greater than by questioning about weekly moderate or vigorous
Rs50,000)”. Occupation will be self reported as: physical activity.
“professional”,“unemployed/retired”, “self
employed”.
We will use the same methods to determine and
validate studies by different researchers.Data will be
Participants will self-report a history of clinical collected by all batch members by visiting medical
cardiovascular disease(atrial fibrillation,valvular and neurology wards of various public sector
heart disease, heart attack), hypertension, hospitals and asking questions from stroke patients or
hypercholesterolemia, diabetes mellitus, previous their guardians after informed consent.
history of stroke/TIA, cigarette smoking, family
o Study Variables:
Non-Modifiable
1.Age
2.Gender
3.Family History
Modifiable
4.Hypertension
5.Cardiac Diseases( atrial fibrillation, valvular heart diseases,
heart attack/myocardial infarction)
6.Diabetes
7.Obesity
8.Hypercholesterolemia
9.Cigarette smoking
10.Physical inactivity(lack of ideal physical activity)
11. Unhealthy diet
o SamplingTool:
A questionnaire will be given.
DATA ANALYSIS PROCEDURE:
Data analysis will be done by using SPSS version 16.Initial analysis will include
frequency distribution and calculation of descriptive statistics e.g. mean, median, mode and
standard deviation.
PRETESTING:
Before carrying out the actual exercise of data collection, the questionnaire would be pre-
tested on some subjects on experimental basis in order to observe:
o Any deficiency in questionnaire.
o The social and ethical acceptability of the questions.
OUTCOME AND UTILIZATOION: for cardiovascular health and promotion and this may
The data will be disseminated through research paper act as model for other developing nations of the
publications in national and international papers, world.It will create awareness in public about their
conferences, seminars and meetings. This project will health issues and will highlight the individuals prone
help the administration, policy makers, health to suffer from stroke so that early preventive
planners to initiate programs according to the needs measures can be taken.
and demands to improve the health status of the
community. It will help in defining and setting goals
www.iajps.com Page 3887
IAJPS 2018, 05 (05), 3884-3893 Ammara Ijaz Rana et al ISSN 2349-7750
It will open the new horizons to the research cause of disability and death worldwide.
scientists and epidemiologists to explore leading
ADMINISTRATIVE PLAN AND IMPACT
Responsibility Responsible
Department of Community Medicine, King Edward
Selection of Problem
Medical University, Lahore
Protocol Development All Batch Members
Data Collection All Batch Members
Data Compilation All Batch Members
Data Analysis All Batch Members
Report Writing All Batch Members
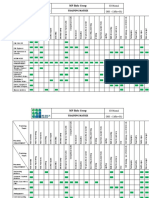
SCHEDULE/PHASING:
WEEK
Task
1st 2nd 3rd 4th 5th 6th 7th 8th 9th 10th 11th 12th
Prepare
Protocol
Data
Collection
Data Analysis
Report
Writing
Presentation
Data Analysis and Interpretation
Table No. 1:Distribution of respondents by Gender
Gender Frequency Percentage
Male 64 64%
Female 36 36%
Total 100 100%
With regard to gender composition of sample respondents as to the finding of study indicated in the above table 1,
while 64% of them are male and the rest of them 36% are female.
Table No. 2:Distribution of Respondents by Age
www.iajps.com Page 3888
IAJPS 2018, 05 (05), 3884-3893 Ammara Ijaz Rana et al ISSN 2349-7750
Age Frequency Percentage
>55 82 82%
<55 18 18%
Total 100 100%
As it can be seen from table 2 above, age composition of total 100 respondents, while the age of 82% of the
respondents are >55 and the age of 18% of the respondents are <55 years.
Table No. 3; Distribution of respondents by Family history of Stroke
Family History Frequency Percentage
Yes 33 33%
No 67 67%
Total 100 100%
As can be inferred from the table 3, the 33% of the respondents have family history of stroke and the 67% of the
respondents have not family history of stroke. The above data revealed that family history of stroke has less
influence on the patient.
Table No. 4: Distribution of respondents by types of Stroke
Types Frequency Percentage
Ischemic Stroke 74 74%
Hemorrhagic Stroke 26 26%
Total 100 100%
As it has been indicated from table 4 that 74% of the respondents have Ischemic stroke and 26% of the respondents
have Hemorrhagic stroke. It can be observed that Ischemic stroke is more prevalent among the patients.
Table No. 5: Distribution of respondents by hypertension
Hypertension Frequency Percentage
Yes 82 82%
No 18 18%
Total 100 100%
The above table 5 revealed that 82% of the respondents have hypertension and 18% of the respondents have not
hypertension.
Table No. 6: Distribution of respondents by diabetes
Diabetes Frequency Percentage
Yes 39 39%
No 61 61%
Total 100 100%
The above data depicted that 39% of the respondents have diabetes and 61% of the respondents have not diabetes. In
this present study, most of the respondents are non-diabetic.
Table No. 7: Distribution of respondents by Hypercholesterolemia
Hypercholesterolemia Frequency Percentage
Yes 41 41%
No 59 59%
Total 100 100%
www.iajps.com Page 3889
IAJPS 2018, 05 (05), 3884-3893 Ammara Ijaz Rana et al ISSN 2349-7750
The above table 7 showed that 41% of the respondents have Hypercholesterolemia and 59% of the respondents have
not Hypercholesterolemia. Most of the respondents have hypercholesterolemia.
Table No. 8: Distribution of respondents by smoking
Smoking Frequency Percentage
Yes 36 36%
Non 64 64%
Total 100 100%
As it has been shown in the table 8 above that 36% of the respondents are regular smokers and 64% of the
respondents are non-smokers.
Table No. 9:Distribution of respondents by obese and non-obese
Obese and Non-obese Frequency Percentage
Obese 29 29%
Non-Obese 71 71%
Total 100 100%
As it has been indicted in the table 9 above, the 29% of the respondents have obesity and 71% of the respondents are
non-obese. Most of the respondents are non-obese.
Table No. 10: Distribution of respondents by physically active and Inactive
Physically active and Non-active Frequency Percentage
Physically active 71 71%
Physically Inactive 29 29%
Total 100 100%
As it has been indicated in the table 10, 71% of the respondents are physically active and 29% of the respondents are
physically inactive. Most of the respondents are physically active.
Table No. 11: Distribution of respondents by Healthy Diet and Unhealthy dietary intake
Dietary Condition Frequency Percentage
Healthy Diet 44 44%
Unhealthy dietary Intake 56 56%
Total 100 100%
As it is can be seen from table 11 above, 44% of the respondents have healthy diet and 56% of the respondents have
unhealthy dietary intake. Most of the respondents have unhealthy dietary intake.
Table No. 12: Distribution of respondents by cardiovascular diseases
Cardiovascular Diseases Frequency Percentage
Valvular Diseases 7 7%
Atrial Fibrillation 8 8%
Myocardial Infraction 24 24%
Patients have not CVS Diseases 67 67%
Total 100 100%
As it has been shown in the table 12, 7% of the respondents have valvular diseases, 8% of the respondents have
atrial fibrillation, 24% of the respondents have myocardial infraction and 67% of the patients have not CVS
diseases.
www.iajps.com Page 3890
IAJPS 2018, 05 (05), 3884-3893 Ammara Ijaz Rana et al ISSN 2349-7750
Table No. 13: Distribution of respondents by previous history of stroke
Previous History Frequency Percentage
Yes 15 15%
No 85 85%
Total 100 100%
As it can be observed from table 13, 15% of the respondents have previous history of stroke and 85% of the
respondents have not previous history of respondents. Most of the respondents have not previous history of stroke.
Table No. 14: Distribution of respondents by Transient Ischemic attacks n Past
Transient Attacks in Past Frequency Percentage
Yes 20 20%
No 80 80%
Total 100 100%
The above table 14 revealed that, 20% of the respondents have Transient Attacks in past and 80% of the respondents
have no Transient Attacks in past.
SUMMARY OF FINDINGS:
Based on data analysis, the following major findings CONCLUSION:
have been drawn: In our study it was found that stroke was more
Out of 100 patients of stroke, 64% of prevalent in males as compared to females. Most of
patients were males and 36% were females. the patients were above 55years of age. Ischemic type
82% were above 55 years of age and 18% of stroke was more common than hemorrhagic type.
were below 55 years of age. In the descending order most frequent risk factors
33% were found to have Family History of were hypertension, physical inactivity, unhealthy
Stroke while 67% didn’t have any Family diet, hypercholesterolemia, diabetes, cigarette
History. smoking, cardiovascular diseases, family history of
74% were found to have Ischemic stroke stroke, obesity, history of transient ischemic attack
and 26% had Hemorrhagic type of stroke. and previous history of stroke.
Hypertension was found in 82% of patients
and 18% were non hypertensive. REFERENCES:
Diabetes was found in 39% of patients while 1. Kumar P. Clark M. Clinical Medicine. ed8th.
61% were non-diabetic. Spain: Elsevier; 2012: p1096.
Hypercholesterolemia was found in 41% of 2. Longo D.L. Hauser S.L. Fauci A.S. Principles of
patients while 59% were non- Internal Medicine.ed18th.India .The McGraw Hill
hypercholesterolemic. Companies; 2012: p3274.
Cigarette smoking was found in 36% of the 3. Alam I, Haider I, Wahab F, Khan W, Taqweem
patients while 64% were non-smokers. AM, Nosherwan. Risk factors stratification in
Obesity was found in 29% of patients while 100 patients of acute stroke. JPMI, Internet
71% were non-obese. 2004;2014.2.10;18(4):583-591. Available
71% were physically inactive while 29% from:URL:http://www.jpmi.org.pk/index.php/jp
were physically active. mi/article/
56% were found to have Unhealthy dietary 4. Feigin VL. Stroke epidemiology in the
Intake while 44% had Healthy Diet. developing world. The Lancet. [internet]
33% were found to have following 20052014.2.10;365(9478):2160–1 Available
Cardiovascular Diseases (Valvular diseases 7%, from:
Atrial Fibrillation 8%, Myocardial Infarction URL:http://www.thelancet.com/journals/lancet/a
24%), while 67% didn’t have any CVS disease. rticle.
15% were found to have previous Stroke history 5. Khan SF, Zafar A, Malik A. Stroke in Pakistan:
while 85% didn’t have any previous Stroke reality, challenges and a call for action. PKJNS.
history. [internet] 2008 2014.2.10.3(1):14-19. Available
20% were found to have Transient Ischemic from:URL:http://pkjns.com/Previous/Archived/J
Attacks in past while 80% didn’t have any TIAs an-Mar-08/Contents/docs/PerspectiveStroke.pdf
in past.
www.iajps.com Page 3891
IAJPS 2018, 05 (05), 3884-3893 Ammara Ijaz Rana et al ISSN 2349-7750
6. Vohra EA. Stroke. The challenge and response. and stroke in patients diagnosed with TIA.
Pak J Med sci. [internet]2001 Neurology.[Internet] 2003.1.28. 2014.2.8. 60(2)
2014.2.10;17(2):65-66. Avaialble 280-285 Available From:
from:URL:http://www.kmuj.kmu.edu.pk/article/ URL:http://www.neurology.org/content/60/2/280
view/10505 .short
7. Khealani BA, Wasay M. The burden of stroke in 17. Ueshima H,Choudhary SR,Okayama
Pakistan. Int J Stroke. [internet] 2008 A,Hayakawa T,Kita Y et al.Cigeratte smoking as
2014.2.10;3(4):293-6. Available from: a risk factor for stroke death.AHA [internet]
URL:http://www.ncbi.nlm.nih.gov/pubmed/1881 2004.5.27 2014.2.8.available
1747 from:URL:http://stroke.ahajournals.org/content/3
8. Singh RB, Suh IL, Singh VP, Chaithiraphan S, 5/8/1836.short
Laothavorn P, Sy RG, et al. Hypertension and 18. Whisnat JP.Effictiveness v/s efficacy of
stroke in Asia: prevalence, control and strategies treatment of hypertension for stroke
in developing countries for prevention. JHH. prevention.Neurology. [internet] 1996
[internet] 2000 2014.2.10. 14(10):749-763. 2014.02.10.46(2):301-7 Avalible
Available from: from:URL:http://www.ncbi.nlm.nih.gov/pubmed
URL:http://www.nature.com/jhh/journal/v14/n10 /8614485
/abs/1001057a.html 19. Burchfiel CM, Curb JD, Rodriguez BL, Abbott
9. Marwat MA, Usman M, Hussain M. Stroke and RD, Chiu D, Yano K. Glucose intolerance and
its relationship to risk factors. GJMS. [internet] 22-year stroke incidence: the Honolulu Heart
2009 2014.2.10;7(1):17-21. Available from: Program. Stroke. [internet] 1994
URL:http://www.gjms.com.pk/ojs786/index.php/ 2014.2.10;25:951-957.available
gjms/article/view/151 from:http://stroke.ahajournals.org/content/25/5/
10. Basharat RA, Elahi A, Tariq M, Saeed A. One 951.
month audit of stroke at PIMS. Pak J Neurol. 20. Shinton R, Beevers G. Meta-analysis of relation
[internet] 1999 2014.2.10;56(1):12–5. Available between cigarette smoking and stroke. BMJ
from:URL:http://www.pjms.com.pk/issues/octde [internet]1989 2014.02.10;298:789-
c208/article/article15.html 794.available from
11. Sacco RL, Benjamin EJ, Brodreck JD, Dyken M, URL:http://www.ncbi.nlm.nih.gov/pubmed/2496
Easton JD, Feinberg WM, et al, Risk Factors, 858
AHA. [internet] 1997 2014.2.8. 28(7):1507-1517 21. Iso H, Jacobs DR Jr, Wentworth D, et al. Serum
Available from: cholesterol levels and six-year mortality from
URL:http://stroke.ahajournals.org/content/28/7/1 stroke in 350,977 men screened for the Multiple
507.short Risk Factor Intervention Trial. N Engl J Med
12. ColledgeN.R. Walker B.R. Ralston S.H. [internet] 1989 2014.02.10;320:904–
Davidson’s Principle and Practice of Medicine. 910.available from:
China. Elsevier. ed21st. p1180. URL:http://www.ncbi.nlm.nih.gov/pubmed/2619
13. Kannel WB, Wolf PA, Verter J, McNamara PM. 783?dopt=Abstract
Epidemiologic Assessment of the Role of Blood 22. Chobanian AV, Bakris JL, Black HR, Cushman
Pressure in Stroke. JAMA. [internet] 1996 WC, Green LA, Jones DW , et all.JNC 7
2014.2.8. 276(15) 1269-1278 Available From: [internet] 2003 2014.2.10;42:p1206-1252
URL:http://jama.jamanetwork.com/article.aspx?a available from
rticleid=409700 https://hyper.ahajournals.org/content/42/6/1206.f
14. Wolf PA, Abbott RD, Kannel WBAtrial ull
Fibrillation: A Major Contributor to Stroke in the 23. Harrison.Diabetes Mellitus.In:Longo DL,Kasper
Elderly. JAMA. [internet] 1987 2014.2.10. DL,Jameson JL,Fauci AS,Hauser SL,Loscalzo
147(9):1561-1564. Available J,et all.Harrison’s principle of internal
From:URL:http://archinte.jamanetwork.com/arti medicine.ed18th. New York :Mc Graw
cle.aspx?articleid=608730 Hill;2012:p2986
15. Song YM,Sung J, Smith GD, Shah E,BMI and 24. Longmore M,Wilkinson I,Turmezei T,Cheung
ischemic and hemorrhagic stroke.AHA. KC.Oxford Handbook of Clinical Medicine.ed
[internet] 2003.11.21 2014.2.8.available 7th.New York:Oxford University
from:URL:http://stroke.ahajournals.org/content/3 Press;2007:p64.
5/4/831.short 25. Behrenbeck T.Mayoclinic. Cholesterol ratio: Is
16. Johnston SC,Sidney S,Bernstein AL,Gress DR. it important? - Mayo Clinic. [Online] 2012 02 11
A comparison of risk factors for recurrent TIA Available from:
www.iajps.com Page 3892
IAJPS 2018, 05 (05), 3884-3893 Ammara Ijaz Rana et al ISSN 2349-7750
URL:http://www.mayoclinic.org/diseases- GF, Arnett DK, Fonarow GC, Ho PM, Lauer
conditions/high-blood-cholesterol/expert- MS, Masoudi FA, Robertson RM, Roger
answers/cholesterol-ratio/faq-20058006 V,Schwamm LH, Sorlie P, Yancy CW,
26. US Centers for Disease Control and Prevention Rosamond WD; on behalf of the American Heart
(2010). Health behaviors of adults: United Association Strategic Planning Task Force and
States, 2005-2007. Vital and Health Statistics, StatisticsCommittee. Defining and setting
Series 10, Number 245, Appendix II, p. national goals for cardiovascular health
80.available from: promotion and disease reduction: the American
URL:http://www.salimetrics.com/articles/smokin Heart Association’s StrategicImpact Goal
g-definitions through 2020 and beyond.Circulation. [internet]
27. Lloyd-Jones DM, Hong Y, Labarthe D, 2010 2014.2.10;121:586 – 613.availalble from
Mozaffarian D, Appel LJ,Van Horn L, https://circ.ahajournals.org/content/121/4/586.ful
Greenlund K, Daniels S, Nichol G, Tomaselli l.pdf+html
www.iajps.com Page 3893
You might also like
- Pharmaceutical Sciences: Pregnancy Outcomes of Covid-19 Positive Patients A Systematic Review of LiteratureDocument6 pagesPharmaceutical Sciences: Pregnancy Outcomes of Covid-19 Positive Patients A Systematic Review of LiteratureiajpsNo ratings yet
- 193 Iajps193092020-1 PDFDocument8 pages193 Iajps193092020-1 PDFiajpsNo ratings yet
- 195 Iajps195092020 PDFDocument5 pages195 Iajps195092020 PDFiajpsNo ratings yet
- 197 Iajps197092020 PDFDocument5 pages197 Iajps197092020 PDFiajpsNo ratings yet
- 46 Iajps46102020Document7 pages46 Iajps46102020iajpsNo ratings yet
- 191 Iajps191092020Document8 pages191 Iajps191092020iajpsNo ratings yet
- Pharmaceutical Sciences: Flipping Impacts of Middle School Laboratory in Health School EducationDocument4 pagesPharmaceutical Sciences: Flipping Impacts of Middle School Laboratory in Health School EducationiajpsNo ratings yet
- 196 Iajps196092020 PDFDocument4 pages196 Iajps196092020 PDFiajpsNo ratings yet
- 193 Iajps193092020-1 PDFDocument8 pages193 Iajps193092020-1 PDFiajpsNo ratings yet
- 194 Iajps194092020 PDFDocument7 pages194 Iajps194092020 PDFiajpsNo ratings yet
- Pharmaceutical Sciences: The Impact of Ox Like Lactoferrin (BLF) On Prevention of The Diarrhoea in YoungstersDocument7 pagesPharmaceutical Sciences: The Impact of Ox Like Lactoferrin (BLF) On Prevention of The Diarrhoea in YoungstersiajpsNo ratings yet
- 44 Iajps44102020Document4 pages44 Iajps44102020iajpsNo ratings yet
- 192 Iajps192092020 PDFDocument5 pages192 Iajps192092020 PDFiajpsNo ratings yet
- Pharmaceutical Sciences: Observation of Metabolism According To The Growth Hormone Control in Mayo Hospital LahoreDocument6 pagesPharmaceutical Sciences: Observation of Metabolism According To The Growth Hormone Control in Mayo Hospital LahoreiajpsNo ratings yet
- 50 Iajps50102020Document13 pages50 Iajps50102020iajpsNo ratings yet
- Pharmaceutical Sciences: Management of Proximal Ureteric Stone (10 - 15 MM Size) Via Urs & EswlDocument6 pagesPharmaceutical Sciences: Management of Proximal Ureteric Stone (10 - 15 MM Size) Via Urs & EswliajpsNo ratings yet
- Pharmaceutical Sciences: Study To Determine The Pattern of Primary Glomerulonephritis in PakistanDocument5 pagesPharmaceutical Sciences: Study To Determine The Pattern of Primary Glomerulonephritis in PakistaniajpsNo ratings yet
- Pharmaceutical Sciences: Urinary Sodium and Potassium Discharge and Danger of Hypertension in Pakistani PopulationDocument4 pagesPharmaceutical Sciences: Urinary Sodium and Potassium Discharge and Danger of Hypertension in Pakistani PopulationiajpsNo ratings yet
- 42 Iajps42102020Document8 pages42 Iajps42102020iajpsNo ratings yet
- 35 Iajps35102020Document4 pages35 Iajps35102020iajpsNo ratings yet
- Pharmaceutical Sciences: Psychophysiological Features of Students Aerobic Abilities and Maintaining A Healthy LifestyleDocument6 pagesPharmaceutical Sciences: Psychophysiological Features of Students Aerobic Abilities and Maintaining A Healthy LifestyleiajpsNo ratings yet
- Pharmaceutical Sciences: A Young Male With Splenic Vein and SMV Thrombosis and Jak 22 MutationDocument12 pagesPharmaceutical Sciences: A Young Male With Splenic Vein and SMV Thrombosis and Jak 22 MutationiajpsNo ratings yet
- Pharmaceutical SciencesDocument5 pagesPharmaceutical SciencesiajpsNo ratings yet
- 40 Iajps40102020Document4 pages40 Iajps40102020iajpsNo ratings yet
- Pharmaceutical Sciences: Cognitive Schemes For Clinical Diagnostic Reasoning by Medical StudentsDocument8 pagesPharmaceutical Sciences: Cognitive Schemes For Clinical Diagnostic Reasoning by Medical StudentsiajpsNo ratings yet
- 33 Iajps33102020Document6 pages33 Iajps33102020iajpsNo ratings yet
- 37 Iajps37102020Document9 pages37 Iajps37102020iajpsNo ratings yet
- 34 Iajps34102020Document7 pages34 Iajps34102020iajpsNo ratings yet
- Pharmaceutical Sciences: Massive Inguinal Hernia-A Rare Presentation of Common DiseaseDocument4 pagesPharmaceutical Sciences: Massive Inguinal Hernia-A Rare Presentation of Common DiseaseiajpsNo ratings yet
- Pharmaceutical Sciences: Teneligliptin Induced Persistent DiarrheaDocument3 pagesPharmaceutical Sciences: Teneligliptin Induced Persistent DiarrheaiajpsNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5782)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (72)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- 2G Call FlowDocument71 pages2G Call Flowm191084No ratings yet
- FM200 Clean Agent System Installation GuideDocument6 pagesFM200 Clean Agent System Installation Guidehazro lizwan halimNo ratings yet
- The UFO MonthlyDocument21 pagesThe UFO MonthlySAB78No ratings yet
- Soal Big A Tukpd 2011-2012 RevisiDocument5 pagesSoal Big A Tukpd 2011-2012 RevisiTriana WatiNo ratings yet
- Oneccc Detection Assignment Grupo1.Ipynb - ColaboratoryDocument9 pagesOneccc Detection Assignment Grupo1.Ipynb - ColaboratoryAna VelezNo ratings yet
- Overview of US Investment in NanotechnologyDocument19 pagesOverview of US Investment in NanotechnologyMaterials Research InstituteNo ratings yet
- Design Basis Events FOR Pressurised Heavy Water Reactor: Aerb Safety Guide No - Aerb/Sg/D-5Document36 pagesDesign Basis Events FOR Pressurised Heavy Water Reactor: Aerb Safety Guide No - Aerb/Sg/D-5Anuj DeoNo ratings yet
- Interpretation of Static Load Tests On The Burj Khalifa's FoundationDocument9 pagesInterpretation of Static Load Tests On The Burj Khalifa's FoundationMALIKNo ratings yet
- CHM4943 Wastewater TreatmentDocument7 pagesCHM4943 Wastewater TreatmentUsman GhaniNo ratings yet
- Introduction To The Philosophy of Science First PartDocument138 pagesIntroduction To The Philosophy of Science First PartChandra Sekhar Sahu100% (1)
- Mtech Geotechnical Engineering 2016Document48 pagesMtech Geotechnical Engineering 2016Venkatesh ThumatiNo ratings yet
- FMDocument12 pagesFMGajera HarshadNo ratings yet
- Mathematics: Full Marks Zero Marks: 0 in All Other CasesDocument31 pagesMathematics: Full Marks Zero Marks: 0 in All Other CasesAbhishek KumarNo ratings yet
- Galaxy NanoporeDocument11 pagesGalaxy NanoporeDeborah ShirleenNo ratings yet
- MP Birla Group: Training MatrixDocument3 pagesMP Birla Group: Training MatrixAprilia kusumaNo ratings yet
- Presentation 1Document26 pagesPresentation 1Vaibhav Hireraddi100% (1)
- Zip Grade 100 Question V2Document1 pageZip Grade 100 Question V2Jesus Daniel Anaya AlvaradoNo ratings yet
- Mahamrityunjaya MantraDocument8 pagesMahamrityunjaya MantraBalakrishnan KannanNo ratings yet
- BT Word FormsDocument11 pagesBT Word FormsNguyên TrungNo ratings yet
- Doctors Appointment - 4!14!17 Acid RefluxDocument11 pagesDoctors Appointment - 4!14!17 Acid RefluxRay Edwin Anderson IIINo ratings yet
- Tajima Usb Linker User's GuideDocument35 pagesTajima Usb Linker User's GuideFermin MuñozNo ratings yet
- Toxicology Compendium PDFDocument602 pagesToxicology Compendium PDFJUANNo ratings yet
- TTBR 10 January 2024 LDocument22 pagesTTBR 10 January 2024 Lfossil.tractor0sNo ratings yet
- Table of PenaltiesDocument2 pagesTable of PenaltiesEzekiel FernandezNo ratings yet
- Renal Cortical CystDocument2 pagesRenal Cortical Cystra222j239No ratings yet
- MA 102 Tutorial Sheet No. 2 on Limits and ContinuityDocument1 pageMA 102 Tutorial Sheet No. 2 on Limits and ContinuityKanan KumarNo ratings yet
- AWWA Bacterial Regrowth in Distr Sys PDFDocument368 pagesAWWA Bacterial Regrowth in Distr Sys PDFsaishankarlNo ratings yet
- Elcometer Wet-Film Gage 115 Spec SheetDocument2 pagesElcometer Wet-Film Gage 115 Spec SheetMary CasillasNo ratings yet
- E5971 m4n68t-m Series ManualDocument0 pagesE5971 m4n68t-m Series ManualcamiloelosadaNo ratings yet
- Effect of Usage of Sinter in BOF Steelmaking As A Replacement To Iron Ore As Coolant For Thermal BalanceDocument11 pagesEffect of Usage of Sinter in BOF Steelmaking As A Replacement To Iron Ore As Coolant For Thermal BalancesomnathNo ratings yet