Professional Documents
Culture Documents
Frontline Gastroenterol 2014 Dyson Flgastro 2013 100404
Uploaded by
CunCunAlAndraCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Frontline Gastroenterol 2014 Dyson Flgastro 2013 100404
Uploaded by
CunCunAlAndraCopyright:
Available Formats
Downloaded from http://fg.bmj.com/ on May 28, 2015 - Published by group.bmj.
com
LIVER
REVIEW
Non-alcoholic fatty liver disease:
a practical approach to treatment
J K Dyson,1 Q M Anstee,1,2 S McPherson1,2
1
Liver Unit, Freeman Hospital, ABSTRACT PRINCIPLES OF MANAGEMENT
Newcastle Upon Tyne Hospitals Non-alcoholic fatty liver disease (NAFLD) OF NAFLD
NHS Foundation Trust,
Newcastle upon Tyne, UK affects up to a third of the population in many Management of patients with NAFLD
2
Institute of Cellular Medicine, developed countries. Between 10% and 30% of depends largely on the stage of disease,
Newcastle University, Newcastle patients with NAFLD have non-alcoholic emphasising the importance of careful
upon Tyne, UK
steatohepatitis (NASH) that can progress to risk stratification.10 There are four main
Correspondence to cirrhosis. There are metabolic risk factors areas to focus on when thinking about
Dr Jessica Dyson, Liver Unit, common to both NAFLD and cardiovascular management strategies in NAFLD: life-
Freeman Hospital, Newcastle disease, so patients with NASH have an style modification, targeting the compo-
upon Tyne Hospitals NHS
Foundation Trust, High Heaton, increased risk of liver-related and cardiovascular nents of the metabolic syndrome,
Newcastle upon Tyne, NE77DN, death. Management of patients with NAFLD liver-directed pharmacotherapy for high
UK; jessicadyson@doctors.org.uk depends largely on the stage of disease, risk patients and managing the complica-
emphasising the importance of careful risk tions of cirrhosis (figure 1).
Received 12 October 2013
Revised 26 December 2013 stratification. There are four main areas to focus All patients with NAFLD require advice
Accepted 1 January 2014 on when thinking about management about lifestyle modification aimed at
strategies in NAFLD: lifestyle modification, weight loss and increased physical activity,
targeting the components of the metabolic as well as treatment of any associated
syndrome, liver-directed pharmacotherapy for metabolic risk factors (diabetes, hyperten-
high risk patients and managing the sion and dyslipidaemia). For patients with
complications of cirrhosis. simple steatosis, which carries a relatively
benign liver-related prognosis, this can be
done in a primary care setting. Patients
with steatohepatitis and fibrosis are at
highest risk of developing progressive
INTRODUCTION liver disease so require more aggressive
Non-alcoholic fatty liver disease (NAFLD) lifestyle modification and if this fails can
is now the commonest cause of chronic be considered for liver-directed pharma-
liver disease in many developed coun- cotherapy with pioglitazone or vitamin E.
tries.1 Up to a third of the population For patients who have progressed to
have evidence of steatosis on imaging,2 3 cirrhosis, surveillance for hepatocellular
with the majority (70%–90%) having carcinoma (HCC) is essential and some
simple steatosis. However, 10%–30% of treatments have been shown to reduce the
subjects with NAFLD have non-alcoholic risk of HCC. Interventions for the treat-
steatohepatitis (NASH) that can progress ment of NAFLD are summarised in
to cirrhosis, which puts patients at risk of table 1.
liver-related complications.4–6 Due to the
metabolic risk factors that are common to
both NAFLD and cardiovascular disease, LIFESTYLE MODIFICATION
patients with NASH have an increased Lifestyle modification aimed at weight
risk of cardiovascular death as well as loss and increased physical activity is vital
To cite: Dyson JK, liver-related mortality.7 8 In the first part in managing all patients with NAFLD irre-
Anstee QM, McPherson S. of this review, we discussed the diagnosis spective of their underlying liver hist-
Frontline Gastroenterology
Published Online First: [ please
and staging of patients with NAFLD and ology. Patients should be encouraged to
include Day Month Year] the importance of risk stratification.9 avoid a sedentary lifestyle by increasing
doi:10.1136/flgastro-2013- Here we will discuss the management of daily activities, undertaking regular exer-
100404 patients with NAFLD. cise and eating healthily. Overall, lifestyle
Dyson JK, et al. Frontline Gastroenterology 2014;0:1–10. doi:10.1136/flgastro-2013-100404 1
Downloaded from http://fg.bmj.com/ on May 28, 2015 - Published by group.bmj.com
LIVER
the same weight) should be recommended aiming to
lose 0.5–1 kg per week until the target weight is
achieved.11 Patients with NAFLD should be advised
to avoid saturated fats, simple carbohydrates and
sweetened drinks.25 26 A ‘fast food diet’ (high in chol-
esterol, saturated fats and fructose) is associated with
progressive fibrosis in mice models.27
A Mediterranean diet (high in monounsaturated
fatty acids), as compared with a diet low in fat and
high in carbohydrates, has been shown to reduce
hepatic steatosis and improve insulin sensitivity in
non-diabetic subjects with NAFLD.28 Dietary supple-
mentation with ω-3 polyunsaturated fatty acids (n-3
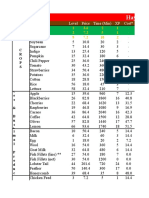
Figure 1 Management strategies in non-alcoholic fatty liver PUFAs) has also been shown to decrease liver fat,29 so
disease (NAFLD).
fish oil supplementation could be a simple therapeutic
option but further studies are needed.
interventions including behavioural, dietary and exer- Intensive 12-month dietician-led lifestyle interven-
cise changes can be very effective in reducing body tions are more effective than standard care for patients
weight. In one study, patients who received dietary with NAFLD in terms of weight loss (5.6 vs 0.6 kg)
advice and undertook 200 min moderate physical and achieving remission of NAFLD (64% vs 20%).30
activity per week for 48 weeks had an overall 9.3% Previous studies have shown that >7%12 and ≥9%13
reduction in body weight (versus 0.2% in the control loss of body weight was associated with reduced stea-
arm) and had improvement in hepatic steatosis and tosis, hepatocellular injury and hepatic inflammation.
inflammation on liver biopsy.12 The optimum amount of weight loss to reduce fibrosis
is not known, but studies in subjects undergoing baria-
Diet tric surgery where larger weight losses are seen
The optimum diet to treat NAFLD is not known. (average reduction 30% of Body Mass Index (BMI) at
Until further evidence is available, a calorie restricted 5 years) indicate that fibrosis regression occurs in the
diet (600 Kcal less than a person needs to remain at majority (65%),19 although minor increases in fibrosis
Table 1 Summary of management of NAFLD
Treatment Intervention/indication Target/outcome
Diet Calorie restricted diet (600 calories less than daily requirement) >7%12 and ≥9%13 loss of body weight reduces steatosis,
ballooning and hepatic inflammation
Aim to lose 0.5–1.0 kg/week11
Avoid saturated fats, simple carbohydrates and sweetened drinks
Aim to lose >10% body weight and maintain loss
Exercise Increasing physical activity Lower levels of steatosis14
Reduce total sedentary time Aerobic exercise improves insulin sensitivity15 16
30 min moderate exercise 5×/week Improved liver enzymes and reduced liver fat17 18
‘Aerobic’, ‘resistance’ and ‘high intensity’ exercise are all effective
Aim >10 000 steps/day (pedometer)
Orlistat (enteric lipase Achieve weight11loss in conjunction with lifestyle modification if Improves ALT and steatosis13
inhibitor) BMI>30 kg/m2
Only continue if >5% loss of body weight in 3 months is
achieved
Bariatric surgery Not a primary treatment for NASH Improve insulin sensitivity and lipid profile
Treatment for obesity if BMI >40 kg/m2 or between 35 and Reduced steatosis, steatohepatitis and fibrosis19
40 kg/m2 with other significant disease11
11
Consider as first-line option if BMI greater >50 kg/m2 Gastric bypass procedures are most effective in producing
sustained weight loss20
Pioglitazone Recommended for patients with more aggressive NASH who have Reduces hepatocellular injury and fibrosis21–23
failed lifestyle interventions
Consider increased risk of congestive cardiac failure, bladder
cancer and reduced bone density
Vitamin E Reserved for selected patients with more advanced precirrhotic Improves steatohepatitis22 24
NASH who have failed lifestyle interventions
ALT, alanine transaminase; BMI, body index mass; NAFLD, non-alcoholic fatty liver disease; NASH, non-alcoholic steatohepatitis.
2 Dyson JK, et al. Frontline Gastroenterology 2014;0:1–10. doi:10.1136/flgastro-2013-100404
Downloaded from http://fg.bmj.com/ on May 28, 2015 - Published by group.bmj.com
LIVER
were seen 5 years post-bariatric surgery in 20% Bariatric surgery
(>90% of these were worsening from stage 0 to 1).31 Bariatric surgery has an increasing role in the manage-
Ideally, patients should be encouraged to lose >10% ment of patients with obesity and the metabolic syn-
(but more is probably better) of body weight and main- drome. Restrictive procedures such as the gastric band,
tain the weight loss or bring their waist circumference gastric balloon and sleeve gastrectomy decrease stomach
or BMI into their ethnicity specific ‘normal’ range (eg, size leading to early satiety. Malabsorptive procedures
for Caucasians: waist circumference <94 cm for men such as gastric bypass limit the absorption of food.
and <80 cm for women or BMI <25 m/kg2). Weight loss after bariatric surgery has beneficial effects
on the components of the metabolic syndrome includ-
Exercise ing improving insulin sensitivity, lipid profile as well as
People with NAFLD engage in less physical activity reducing long-term mortality.20 36 It also has specific
than their healthy counterparts32 33 and higher levels effects on liver histology including reduced steatosis,
of habitual physical activity are associated with lower steatohepatitis and fibrosis.19 The majority of the histo-
levels of steatosis.14 Aerobic exercise increases skeletal logical benefits occur within the first year post-
muscle insulin sensitivity and as a result reverses one surgery.31 The optimum type of bariatric surgery for the
of the key pathophysiological mechanisms that causes treatment of NASH is not known. Although gastric
NAFLD (insulin resistance).15 16 Although the bypass surgery produces the largest sustained weight
optimum exercise to treat NAFLD is not known, loss compared with other bariatric procedures,
studies examining moderate intensity training, high Mathurin et al found no significant differences among
intensity training and resistance exercise have shown the gastric band, bilio-intestinal and gastric bypass
improvement in liver enzymes and reduction in liver groups in terms of global NAFLD activity score (NAS),
fat, independent of weight loss, but the effects on hist- steatosis, inflammation or ballooning.31 As there is a
ology remain unknown.17 18 34 Therefore, all patients lack of long-term outcome data about bariatric surgery
with NAFLD should be advised to increase physical as a specific treatment for NAFLD, bariatric surgery
activity and undertake regular exercise. Until further cannot be considered as a primary treatment for
evidence is available, one approach is to recommend NASH.37 However, NICE guidance suggests that
30 min of moderate exercise five times weekly.11 In surgery should be considered as a treatment for obesity
reality though, a significant proportion of patients for patients with BMI >40 kg/m2 or between 35 and
with NAFLD do not comply with these recommenda- 40 kg/m2 with other significant disease that could be
tions. In such patients, the use of pedometers can be improved with weight loss. All appropriate non-surgical
quite helpful. We recommend that patients increase measures must be tried first and patients must receive
their daily step count to >10 000 steps/day. intensive specialist management and be prepared to
commit to long-term follow-up. Surgery can be consid-
Orlistat as an aid to weight loss ered as a first-line option for the treatment of obesity in
Orlistat is an enteric lipase inhibitor that leads to malab- adults with a BMI greater than 50 kg/m2.11
sorption of dietary fat and can aid weight loss in subjects Bariatric surgery should be avoided in subjects with
with obesity in conjunction with lifestyle modification. advanced cirrhosis with portal hypertension as there is a
One study demonstrated that orlistat treatment for risk of hepatic decompensation with the rapid weight
NAFLD improved alanine transaminase (ALT) and stea- loss.38 Patients with decompensated cirrhosis have par-
tosis,35 but a subsequent RCT conducted by Harrison ticularly high mortality rates post-bariatric surgery com-
et al showed that orlistat in combination with calorie pared with compensated cirrhotics and non-cirrhotic
restriction and vitamin E (800 IU/day) did not enhance patients (16.3% vs 0.9% and 0.3%, respectively,
weight loss, improve liver enzymes or improve histo- p=0.0002).39 In carefully selected patients with Child–
pathology compared with calorie restriction and Pugh A cirrhosis, gastric bypass and sleeve gastrectomy
vitamin E. In that study, they found that ≥9% weight have been shown to achieve weight loss and improve
loss resulted in improved histology irrespective of obesity-related comorbidities.40 However, patients with
whether they received orlistat or placebo.13 National cirrhosis should undergo bariatric surgery at centres that
Institute of Health and Care Excellence (NICE) guide- perform large numbers of these procedures.39
lines11 for obesity recommend that orlistat can be con-
sidered as an aid to weight loss in subjects who have not Liver-directed pharmacotherapy
achieved their target weight by lifestyle intervention and For patients with biopsy-proven NASH, where life-
have a BMI>30 kg/m2, so it seems reasonable to con- style intervention has failed, liver-directed pharmaco-
sider this treatment in patients with obesity and therapy with pioglitazone or vitamin E can be
NAFLD. If orlistat is initiated, only patients who considered.
achieve >5% loss of body weight in 3 months should
continue the medication. Treatment duration should not Pioglitazone
be greater than 1 year as there is potential for fat soluble Several studies have demonstrated benefit from the
vitamin deficiency if continued for longer. thiazolidinediones in patients with NASH both with
Dyson JK, et al. Frontline Gastroenterology 2014;0:1–10. doi:10.1136/flgastro-2013-100404 3
Downloaded from http://fg.bmj.com/ on May 28, 2015 - Published by group.bmj.com
LIVER
and without diabetes.21 22 41 Aithal et al showed that TARGETING COMPONENTS OF
12 months of treatment with pioglitazone 30 mg/day THE METABOLIC SYNDROME
reduced hepatocellular injury and fibrosis compared Management of diabetes mellitus in patients with NAFLD
with placebo.21 More recently, the PIVENS study Approximately 40%–50% of patients with NAFLD
showed significantly more patients receiving pioglita- attending secondary care clinics have T2DM and the
zone had resolution of steatohepatitis (a secondary majority have evidence of insulin resistance.50 51 T2DM
endpoint) than with placebo (47% vs 21% p=0.001), is associated with more progressive fibrosis in NASH. It
although the treatment arm narrowly failed to meet is therefore essential that all patients with NAFLD are
the very strict primary endpoint (improvement in regularly screened for diabetes. Once diagnosed, dia-
NAS ≥2 with at least 1-point improvement in hepato- betes should be managed initially with dietary interven-
cyte ballooning without increase in fibrosis score).22 A tion. Although metformin has not been shown to
recent meta-analysis has demonstrated that pioglita- improve histology in NASH, it is recommended as the
zone treatment in NASH significantly improves stea- first-line pharmacological treatment for T2DM as it aids
tosis, inflammation and to a lesser degree, fibrosis.23 weight loss and reduces the risk of any diabetes-related
While pioglitazone appears to be an effective treat- endpoint, microvascular disease, myocardial infarction
ment for NASH, there are also some concerns about (large vessel disease) and all-cause mortality.52–54
its long-term safety. Treatment with pioglitazone is Treatment of diabetes should be escalated if the glyco-
associated with weight gain (4.7% in the PIVENS sylated haemoglobin (HbA1c) rises to >7.5%. NICE
study)22 and there have been reports of increased risk guidelines suggest a sulfonylurea (such as gliclazide) as
of congestive cardiac failure,42 bladder cancer43 and second-line treatment for subjects with T2DM.52
reduced bone density.44 However, a meta-analysis of However, sulfonylureas increase insulin secretion and
16 390 patients with type 2 diabetes mellitus (T2DM) can cause weight gain, which might be detrimental in
treated with pioglitazone demonstrated an 18% reduc- NAFLD. Therefore, the insulin sensitiser, pioglitazone,
tion in death, myocardial infarction and stroke.45 should be considered as a second-line agent in subjects
Therefore, after assessing risk and benefit, treatment with NASH as studies have demonstrated its potential
with pioglitazone can be recommended for patients to improve insulin sensitivity as well as reduce hepatic
with more aggressive NASH who have failed lifestyle steatosis and inflammation in subjects with NASH and
interventions.46 Caution should clearly be exercised in T2DM.22 41 However, the potential risks of bladder
patients with cardiac disease (a common comorbidity cancer, increased bone loss and cardiac failure need to
in patients with NAFLD) and echocardiography per- be considered.
formed prior to considering treatment with pioglita- Glucagon-like peptide-1 (GLP-1) analogues (such as
zone. The optimum dose and duration of treatment liraglutide or exenatide) should be considered as an
are not known. alternative to insulin as a third-line agent to control
diabetes where the HbA1c is >7.5% in subjects with
Vitamin E obesity. GLP-1 is an incretin secreted by ileal L-cells
Vitamin E is an antioxidant that has recently been dependent on the presence of food in the small intes-
shown to have beneficial effects on histology in non- tine. It increases insulin sensitivity, inhibits gastric
diabetic patients with NASH. In the large PIVENS emptying and decreases food intake by increasing
trial, significantly more patients had improvement in satiety in the brain.55 On average, they reduce HbA1c
steatohepatitis following 96 weeks of vitamin E by 1% and patients frequently lose weight (overall
800 IU/day compared with placebo (42% vs 19% average 3 kg). In a meta-analysis of the phase III
p<0.001).22 This was confirmed in a study of child- studies of liraglutide for the treatment of type 2 dia-
hood NASH, where vitamin E was shown to reduce betes (n=4442), 26 weeks treatment with liraglutide
steatohepatitis in a subgroup who had follow-up liver 1.8 mg was associated with an improvement in liver
biopsies.24 Although vitamin E looks like a promising enzymes as well as a trend towards reduced steatosis
treatment for NASH, there are concerns about the measured by CT.56 This effect appeared to be
long-term effects of vitamin E with a meta-analysis mediated by its effect on weight loss and glycaemic
showing a small overall increase in all-cause mortality control. Studies are underway to determine the effect
at doses >400 IU/day.47 It has also been reported that of liraglutide on liver histology. However, as with all
there might be an increased risk of haemorrhagic the antidiabetic drugs, a careful assessment of the risk
stroke48 and prostate cancer49 with high dose treat- and benefits should be undertaken as there is recent
ment. Vitamin E has not been evaluated in patients evidence to suggest that GLP-1 agonists might induce
with cirrhosis or diabetes and NASH. Therefore, it pancreatitis ( particularly in those with very high tri-
should currently be reserved for selected patients with glycerides) and increase the potential for pancreatic
more advanced pre-cirrhotic NASH who have failed cancer.55
lifestyle interventions. The optimum dose and dur- Table 2 summarises the treatment of type 2 diabetes
ation of treatment are not known. and the metabolic syndrome in NAFLD.
4 Dyson JK, et al. Frontline Gastroenterology 2014;0:1–10. doi:10.1136/flgastro-2013-100404
Downloaded from http://fg.bmj.com/ on May 28, 2015 - Published by group.bmj.com
LIVER
Table 2 Treatment of type 2 diabetes and the metabolic syndrome in NAFLD
Treatment Indication Outcome
Dietary intervention See table 1 Escalate treatment if HbA1c >7.5%
Metformin First-line treatment of T2DM Aids weight loss
Reduces risk of any diabetes-related endpoint, microvascular disease, myocardial
infarction (large vessel disease) and all-cause mortality52 53
Reduced HCC risk57 58
Pioglitazone Second-line treatment of T2DM in NASH Improve insulin sensitivity and reduces hepatic steatosis/steatohepatitis41
18% reduction in death, myocardial infarction and stroke in T2DM45
Consider risks of bladder cancer,43 increased bone loss44 and cardiac failure42
GLP-1 analogue Third-line treatment of T2DM in NASH Reduce HbA1c by 1% and average 3 kg weight loss
Improve liver enzymes and reduce steatosis56
Risk of pancreatitis55
Insulin/sulfonylureas Fourth-line treatment of T2DM in NASH Lead to weight gain that can be detrimental in NAFLD
GLP-1, glucagon-like peptide-1; HbA1c, glycosylated haemoglobin; HCC, hepatocellular carcinoma; NAFLD, non-alcoholic fatty liver disease; NASH, non-
alcoholic steatohepatitis; T2DM, type 2 diabetes mellitus.
Hypertension Dyslipidaemia
Approximately 70% of patients with NAFLD have Dyslipidaemia is very common in patients with
hypertension59 60 and so it is imperative to screen all NAFLD and the metabolic syndrome. Effective treat-
patients. If the blood pressure is >140/90 mm Hg, ment of dyslipidaemias is vital in the management of
patients should be managed according to NICE hyper- NAFLD to reduce patients’ cardiovascular risk profile.
tension guidelines.61 ACE inhibitors (ACEIs) or angio- NICE guidelines66 recommend simvastatin treatment
tensin receptor blockers (ARBs) are recommended as primary prevention for cardiovascular disease in
first-line for patients less than 55 years old, but calcium adults with a ≥20% 10-year risk of developing cardio-
channel blockers are recommended in people over vascular disease (using a risk calculator such as the
55 years and those of Afro-Caribbean origin. However, Framingham risk calculator). More aggressive lipid
targeting the renin–angiotensin system (RAS) might be control is recommended for secondary prevention of
beneficial in all patients with NAFLD as the RAS plays a cardiovascular disease, aiming for a total cholesterol
role in liver fibrogenesis and blocking the RAS reduces <4 mmol/L. A meta-analysis confirmed that statin
fibrosis in experimental models of hepatic fibrosis.62 63 therapy safely reduces the 5-year incidence of all-cause
A previous study of 54 hypertensive patients with mortality, major coronary events, coronary revascular-
NASH demonstrated that both telmisartan 20 mg and isation and stroke by about 20% per mmol/L reduc-
valsartan 80 mg improved transaminase levels and tion in LDL cholesterol.67
insulin sensitivity, and telmisartan also showed a signifi- Raised transaminases are frequently seen in patients
cant decrease in NASH activity score and fibrosis.64 receiving statins (usually due to coexistent NAFLD)
Further larger studies are needed to confirm these obser- but they are safe in patients with liver disease, and
vations, but ACEI or ARBs seem a logical choice in the serious liver injury is rarely seen in clinical practice.46
management of hypertension in subjects with NAFLD. In a large cardiovascular outcomes study, statins were
They may also have the added benefit of reducing the shown to improve liver enzymes and cardiovascular
incidence of T2DM. A previous meta-analysis of more outcomes in patients with raised liver function tests
than 100 000 patients also showed a 20% reduction in (LFTs) due to NAFLD.68
the incidence of new onset diabetes with the use of Table 3 summarises the management of hyperten-
ACEI or ARBs.65 sion and dyslipidaemia in NAFLD.
Table 3 Management of hypertension and dyslipidaemia in NAFLD
Risk factor Treatment/indication Outcome
Hypertension ACEI and ARBs first-line if BP >140/90 mm Hg61 Blocking RAS reduces hepatic fibrosis62 63
Escalate treatment according to NICE hypertension ARBs improve transaminase levels and insulin sensitivity64
guidelines 20% reduction in new onset T2DM with ACEI or ARBs65
Dyslipidaemia Primary prevention with statin if ≥20% 10-year risk Statins reduce 5-year incidence of all-cause mortality, major coronary events,
of developing cardiovascular disease66 coronary revascularisation and stroke by about 20% per mmol/L reduction in LDL
cholesterol67
If secondary prevention, aim total cholesterol
<4 mmol/L May reduce incidence of HCC69
ACEI, ACE inhibitor; ARB, angiotensin receptor blocker; BP, blood pressure; HCC, hepatocellular carcinoma; LDL, low-density lipoprotein; NAFLD, non-
alcoholic fatty liver disease; NASH, non-alcoholic steatohepatitis; T2DM, type 2 diabetes mellitus; RAS, renin–angiotensin system.
Dyson JK, et al. Frontline Gastroenterology 2014;0:1–10. doi:10.1136/flgastro-2013-100404 5
Downloaded from http://fg.bmj.com/ on May 28, 2015 - Published by group.bmj.com
LIVER
Obstructive sleep apnoea of nutrient deprivation,82 83 and reducing proliferation
Due to the high prevalence of obesity in subjects with of cancer cell lines.83
NAFLD, obstructive sleep apnoea (OSA) is very Donadon et al found that metformin treatment was
common and often unrecognised. OSA is associated associated with a statistically significant reduction of
with an increased risk of NAFLD as well as more HCC risk (OR 0.33; CI 0.1 to 0.7, p=0.006) in dia-
advanced fibrosis due to NASH.70 Clinicians should betic patients.84 The benefit of metformin was con-
have a high index of suspicion for OSA and can firmed by Hassan et al who found the use of
screen patients in the clinic using the STOP BANG metformin or thiazolidinediones in diabetic patients
questionnaire that encompasses eight factors: Snoring, was associated with a 70% risk reduction of HCC
Tiredness, Observed apnoeas, Elevated blood pres- compared with the use of insulin or sulfonylureas.85 A
sure, BMI (>35 kg/m2), Age (>50 years), Neck cir- recent large Taiwanese nationwide case-control study
cumference (>40 cm) and Gender (male). Patients demonstrated a 7% risk reduction per year for HCC
who score ≥3 points (a point is given for each positive in diabetics treated with metformin (adjusted
risk factor) have a high likelihood of having OSA. OR=0.93, 95% CI 0.91 to 0.94, p<0.0001).58
This questionnaire has 83.6%, 92.9% and 100% sen- There is also evidence that statins might reduce the
sitivity for mild, moderate and severe sleep apnoea, incidence of HCC. An American case-control study
respectively.71 It is not known whether treatment of examining HCC in diabetic patients found an adjusted
OSA slows or halts progression of fibrosis in NASH. OR for statin use of 0.74 (95% CI 0.64 to 0.87). There
were no significant associations with non-statin
MANAGING THE COMPLICATIONS cholesterol- or triglyceride-lowering medications.86 A
OF CIRRHOSIS Taiwanese population-based case-control study found
Hepatocellular carcinoma an adjusted OR of 0.62 (95% CI 0.42 to 0.91) for HCC
Patients with NASH cirrhosis are at risk of the same in patients prescribed statins.87 Singh et al conducted a
complications of cirrhosis as with any other aetiology of systematic review and meta-analysis and found that
liver disease. The yearly cumulative incidence of HCC is statin users were less likely to develop HCC than
2.6% per year in patients with NASH cirrhosis.72 non-users (adjusted OR, 0.63; 95% CI 0.52 to 0.76).
Therefore, surveillance with abdominal ultrasonography The risk reduction was most marked in Asian popula-
(USS) should be performed every 6 months.73 74 In tions but was also observed in Western populations.69
unselected cirrhotic patients, USS has a sensitivity Statins appear to have anticancer effects through
ranging from 58% to 89% with a specificity >90% both 3-hydroxy-3-methyl-glutaryl-CoA (HMG-CoA)
when used as a surveillance test.75 76 Ultrasound can be reductase dependent and HMG-CoA reductase inde-
technically difficult in obese patients so it is likely that pendent pathways. They have a variety of actions
ultrasound is less sensitive as a surveillance modality in including: anti-inflammatory and immunomodulatory
patients with NAFLD, but currently there are no data to effects, inhibiting downstream production of media-
support the routine use of CTor MRI for surveillance.74 tors of cell growth88 and promoting programmed cell
CT or MRI could be considered in subjects where ultra- death.89 Studies have shown that inactivation of Myc
sound has failed to produce adequate examination of can induce remission of HCC and atorvastatin blocks
the liver, but these modalities have their own limitations Myc activation resulting in suppression of tumour
in obese patients. growth.90 91
α-Fetoprotein is a tumour biomarker and has
recently been removed from the European guidelines Varices
but is still widely used in clinical practise alongside Cirrhotic patients with NASH are at risk of varices as
6-monthly ultrasound. Although rare, HCC can occur with other liver diseases and their presence correlates
on a background of non-cirrhotic NAFLD.77 with the severity of liver disease (40%–44% if Child–
There is a clear association between obesity and malig- Pugh grade A, 75%–85% if Child–Pugh grade C).92
nancy78 and hyperinsulinaemia is well recognised as an Therefore, patients with NASH cirrhosis should
independent risk factor for many malignancies.79 80 undergo endoscopic screening for oesophageal and
Aberrant genes involved in metabolic pathways, such as gastric varices at the time of diagnosis and at regular
the AMP-activated protein kinase (AMPK)–LKB1 intervals according to British Society of
pathway, are emerging as therapeutic targets in cancer Gastroenterology or American Association for the
treatment.81 Metformin acts by inhibiting hepatic Study of Liver Diseases guidelines93 94 (see table 4).
glucose production through an LKB1–AMPK-mediated
mechanism. There is emerging evidence that metformin Osteoporosis and fracture risk
reduces the risk of cancer (including HCC) in patients Patients with cirrhosis are at increased risk of osteo-
with diabetes in a dose-dependent manner.57 The porosis and fractures. Cirrhotic patients should have a
mechanisms of the anticancer effects of metformin may dual x-ray absorptiometry scan to assess bone mineral
include triggering of the LKB1-mediated AMPK density and have their fracture risk assessed using the
pathway, resulting in cancer cell death under conditions FRAX tool (http://www.shef.ac.uk/FRAX/tool). The
6 Dyson JK, et al. Frontline Gastroenterology 2014;0:1–10. doi:10.1136/flgastro-2013-100404
Downloaded from http://fg.bmj.com/ on May 28, 2015 - Published by group.bmj.com
LIVER
Table 4 Managing the complications of cirrhosis
Complication Risk Management
Hepatocellular Yearly cumulative incidence 2.6% per year50 6 monthly abdominal USS± α-fetoprotein
carcinoma
Varices 40%–44% if Child–Pugh grade A Endoscopic surveillance and management according to BSG or
75%–85% if Child–Pugh grade C92 AASLD guidelines94 93
Osteoporosis Cirrhotic patients are at increased risk of osteoporosis Correction of vitamin D insufficiency with oral daily vitamin D3
and fractures and calcium95
Larger studies assessing the effects of vitamin D Dual x-ray absorptiometry scan to assess BMD
supplementation on BMD are lacking Assess fracture risk using FRAX tool (http://www.shef.ac.uk/
FRAX/tool)
AASLD, American Association for the Study of Liver Diseases; BMD, bone mineral density; BSG, British Society of Gastroenterology; USS, ultrasonography.
FRAX tool has an easy online link to the National Commercial (CC BY-NC 3.0) license, which permits others to
Osteoporosis Guideline Group website which provides distribute, remix, adapt, build upon this work non-commercially,
and license their derivative works on different terms, provided
management advice according to the patient’s risk of the original work is properly cited and the use is non-
fracture. Table 4 summarises the management of the commercial. See: http://creativecommons.org/licenses/by-nc/3.0/
complications of NASH cirrhosis.
REFERENCES
Liver transplantation 1 Bedogni G, Miglioli L, Masutti F, et al. Prevalence of and risk
NASH cirrhosis is now the third commonest indication factors for nonalcoholic fatty liver disease: the Dionysos
for liver transplantation in the USA and accounted for nutrition and liver study. Hepatology 2005;42:44–52.
12% of patients listed for transplantation in the UK in 2 Browning JD, Szczepaniak LS, Dobbins R, et al. Prevalence of
2009.96 Patient and graft survival in liver transplantation hepatic steatosis in an urban population in the United States:
for NASH are comparable with other indications.96 97 Impact of ethnicity. Hepatology 2004;40:1387–95.
Although recurrence of NASH is common post- 3 Wong VW, Chu WC, Wong GL, et al. Prevalence of
non-alcoholic fatty liver disease and advanced fibrosis in
transplant, occurring in 4%–25% of patients, it does
Hong Kong Chinese: a population study using
not appear to impact on graft survival.98 99 Patients who
proton-magnetic resonance spectroscopy and transient
are transplanted for NASH cirrhosis frequently have elastography. Gut 2012;61:409–15.
multiple cardiovascular risk factors that should be 4 Matteoni CA, Younossi ZM, Gramlich T, et al. Non alcoholic
managed aggressively post-transplant to prevent fatty liver disease: a spectrum of clinical and pathological
cardiovascular-related mortality.100 UK guidelines on severity. Gastroenterology 1999;116:1413–19.
liver transplantation suggest that bariatric surgery can be 5 Wanless IR, Lentz JS. Fatty liver hepatitis (steatohepatitis) and
considered at the time of liver transplantation for obesity: an autopsy study with analysis of risk factors.
patients with NASH and morbid obesity.100 Hepatology 1990;12:1106–10.
6 Williams CD, Stengel J, Asike MI, et al. Prevalence of
Summary nonalcoholic fatty liver disease and nonalcoholic
steatohepatitis among a largely middle-aged population
Lifestyle interventions aimed at weight loss and
utilizing ultrasound and liver biopsy: a prospective study.
increased activity are essential for all patients with
Gastroenterology 2011;140:124–31.
NAFLD and if sustained are effective in the treatment 7 Ekstedt M, Franzen LE, Mathiesen UL, et al. Long-term
of NAFLD. For patients who fail lifestyle intervention, follow-up of patients with NAFLD and elevated liver
liver-directed pharmacotherapy with pioglitazone or enzymes. Hepatology 2006;44:865–73.
vitamin E can be considered for those with advanced, 8 Anstee QM, Targher G, Day CP. Progression of NAFLD to
but pre-cirrhotic, NASH. Features of the metabolic diabetes mellitus, cardiovascular disease or cirrhosis. Nat Rev
syndrome and cardiovascular risk factors are very Gastroenterol Hepatol 2013;10:330–44.
common in NAFLD, so all patients should be screened 9 Dyson JK, Anstee QM, Mcpherson S. Non-alcoholic fatty
for these and have them managed aggressively. For liver disease: a practical approach to diagnosis and staging.
patients who develop advanced disease, they require Frontline Gastro Published OnlineFirst: 24 Dec 2013.
doi:10.1136/flgastro-2013-100403
surveillance for and management of the complications
10 Anstee QM, McPherson S, Day CP. How big a problem is
of cirrhosis (HCC, varices, osteoporosis). non-alcoholic fatty liver disease? BMJ 2011;343:d3897.
11 NICE. NICE Clinical guidelines. CG43 Obesity: the
Contributors JD, QA and SM have all contributed to this review. prevention, identification, assessment and management of
Competing interests None. overweight and obesity in adults and children. In: Care
Provenance and peer review Not commissioned; externally NIfHaCEaNCCfP, ed., 2006.
peer reviewed. 12 Promrat K, Kleiner DE, Niemeier HM, et al. Randomized
Open Access This is an Open Access article distributed in controlled trial testing the effects of weight loss on
accordance with the Creative Commons Attribution Non nonalcoholic steatohepatitis. Hepatology 2010;51:121–9.
Dyson JK, et al. Frontline Gastroenterology 2014;0:1–10. doi:10.1136/flgastro-2013-100404 7
Downloaded from http://fg.bmj.com/ on May 28, 2015 - Published by group.bmj.com
LIVER
13 Harrison SA, Fecht W, Brunt EM, et al. Orlistat for a systematic review and meta-analysis. J Hepatol
overweight subjects with nonalcoholic steatohepatitis: a 2012;56:944–51.
randomized, prospective trial. Hepatology 2009;49:80–6. 30 Wong VW, Chan RS, Wong GL, et al. Community-based lifestyle
14 Perseghin G, Lattuada G, De Cobelli F, et al. Habitual modification programme for non-alcoholic fatty liver disease: a
physical activity is associated with intrahepatic fat content in randomized controlled trial. J Hepatol 2013;59:536–42.
humans. Diabetes Care 2007;30:683–8. 31 Mathurin P, Hollebecque A, Arnalsteen L, et al. Prospective
15 Kirwan JP, Solomon TP, Wojta DM, et al. Effects of 7 days of study of the long-term effects of bariatric surgery on liver
exercise training on insulin sensitivity and responsiveness in injury in patients without advanced disease. Gastroenterology
type 2 diabetes mellitus. Am J Physiol Endocrinol Metab 2009;137:532–40.
2009;297:E151–6. 32 Zelber-Sagi S, Nitzan-Kaluski D, Goldsmith R, et al. Role of
16 Van Der Heijden GJ, Wang ZJ, Chu Z, et al. Strength exercise leisure-time physical activity in nonalcoholic fatty liver disease: a
improves muscle mass and hepatic insulin sensitivity in obese population-based study. Hepatology 2008;48:1791–8.
youth. Med Sci Sport Exerc 2010;42:1973–80. 33 Hsieh SD, Yoshinaga H, Muto T, et al. Regular physical
17 Thoma C, Day CP, Trenell MI. Lifestyle interventions for the activity and coronary risk factors in Japanese men. Circulation
treatment of non-alcoholic fatty liver disease in adults: a 1998;97:661–5.
systematic review. J Hepatol 2012;56:255–66. 34 Little JP, Gillen JB, Percival ME, et al. Low-volume
18 Hallsworth K, Fattakhova G, Hollingsworth KG, et al. high-intensity interval training reduces hyperglycemia and
Resistance exercise reduces liver fat and its mediators in increases muscle mitochondrial capacity in patients with type
non-alcoholic fatty liver disease independent of weight loss. 2 diabetes. J Appl Physiol 2011;111:1554–60.
Gut 2011;60:1278–83. 35 Zelber-Sagi S, Kessler A, Brazowsky E, et al. A double-blind
19 Mummadi RR, Kasturi KS, Chennareddygari S, et al. Effect randomized placebo-controlled trial of orlistat for the
of bariatric surgery on nonalcoholic fatty liver disease: treatment of nonalcoholic fatty liver disease. Clin
systematic review and meta-analysis. Clin Gastroenterol Gastroenterol Hepatol 2006;4:639–44.
Hepatol 2008;6:1396–402. 36 Sjostrom L, Narbro K, Sjostrom CD, et al. Effects of bariatric
20 Sjostrom L, Lindroos AK, Peltonen M, et al. Lifestyle, surgery on mortality in Swedish obese subjects. NEJM
diabetes, and cardiovascular risk factors 10 years after 2007;357:741–52.
bariatric surgery. NEJM 2004;351:2683–93. 37 Chavez-Tapia NC, Tellez-Avila FI, Barrientos-Gutierrez T, et al.
21 Aithal GP, Thomas JA, Kaye PV, et al. Randomized, Bariatric surgery for non-alcoholic steatohepatitis in obese
placebo-controlled trial of pioglitazone in nondiabetic subjects patients. Cochrane Database System Rev 2010:CD007340.
with nonalcoholic steatohepatitis. Gastroenterology 38 D’Albuquerque LA, Gonzalez AM, Wahle RC, et al. Liver
2008;135:1176–84. transplantation for subacute hepatocellular failure due to
22 Sanyal AJ, Chalasani N, Kowdley KV, et al. Pioglitazone, massive steatohepatitis after bariatric surgery. Liver Transpl
vitamin E, or placebo for nonalcoholic steatohepatitis. NEJM 2008;14:881–5.
2010;362:1675–85. 39 Mosko JD, Nguyen GC. Increased perioperative mortality
23 Boettcher E, Csako G, Pucino F, et al. Meta-analysis: following bariatric surgery among patients with cirrhosis. Clin
pioglitazone improves liver histology and fibrosis in patients Gastroenterol Hepatol 2011;9:897–901.
with non-alcoholic steatohepatitis. Aliment Pharmacol Ther 40 Shimizu H, Phuong V, Maia M, et al. Bariatric surgery in
2012;35:66–75. patients with liver cirrhosis. Surg Obes Relat Dis 2013;9:1–6.
24 Lavine JE, Schwimmer JB, Van Natta ML, et al. Effect of 41 Belfort R, Harrison SA, Brown K, et al. A placebo-controlled
vitamin E or metformin for treatment of nonalcoholic fatty trial of pioglitazone in subjects with nonalcoholic
liver disease in children and adolescents: the TONIC steatohepatitis. NEJM 2006;355:2297–307.
randomized controlled trial. JAMA 2011;305:1659–68. 42 Lago RM, Singh PP, Nesto RW. Congestive heart failure and
25 Zivkovic AM, German JB, Sanyal AJ. Comparative review of cardiovascular death in patients with prediabetes and type 2
diets for the metabolic syndrome: implications for nonalcoholic diabetes given thiazolidinediones: a meta-analysis of
fatty liver disease. Am J Clin Nutr 2007;86:285–300. randomised clinical trials. Lancet 2007;370:1129–36.
26 Musso G, Gambino R, Pacini G, et al. Prolonged saturated 43 Piccinni C, Motola D, Marchesini G, et al. Assessing the
fat-induced, glucose-dependent insulinotropic polypeptide association of pioglitazone use and bladder cancer through
elevation is associated with adipokine imbalance and liver drug adverse event reporting. Diabetes Care
injury in nonalcoholic steatohepatitis: dysregulated 2011;34:1369–71.
enteroadipocyte axis as a novel feature of fatty liver. Am J 44 Lecka-Czernik B. Bone loss in diabetes: use of antidiabetic
Clin Nutr 2009;89:558–67. thiazolidinediones and secondary osteoporosis. Curr
27 Charlton M, Krishnan A, Viker K, et al. Fast food diet mouse: Osteoporos Rep 2010;8:178–84.
novel small animal model of NASH with ballooning, 45 Lincoff AM, Wolski K, Nicholls SJ, et al. Pioglitazone and
progressive fibrosis, and high physiological fidelity to the risk of cardiovascular events in patients with type 2 diabetes
human condition. Am J Physiol Gastrointest Liver Physiol mellitus: a meta-analysis of randomized trials. JAMA
2011;301:G825–34. 2007;298:1180–8.
28 Ryan MC, Itsiopoulos C, Thodis T, et al. The Mediterranean 46 Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and
diet improves hepatic steatosis and insulin sensitivity in management of non-alcoholic fatty liver disease: practice
individuals with non-alcoholic fatty liver disease. J Hepatol guideline by the American Gastroenterological Association,
2013;59:138–43. American Association for the Study of Liver Diseases, and
29 Parker HM, Johnson NA, Burdon CA, et al. Omega-3 American College of Gastroenterology. Gastroenterology
supplementation and non-alcoholic fatty liver disease: 2012;142:1592–609.
8 Dyson JK, et al. Frontline Gastroenterology 2014;0:1–10. doi:10.1136/flgastro-2013-100404
Downloaded from http://fg.bmj.com/ on May 28, 2015 - Published by group.bmj.com
LIVER
47 Miller ER 3rd, Pastor-Barriuso R, Dalal D, et al. 65 Al-Mallah M, Khawaja O, Sinno M, et al. Do angiotensin
Meta-analysis: high-dosage vitamin E supplementation may converting enzyme inhibitors or angiotensin receptor blockers
increase all-cause mortality. Ann Intern Med 2005;142:37–46. prevent diabetes mellitus? A meta-analysis. Cardiology J
48 Schurks M, Glynn RJ, Rist PM, et al. Effects of vitamin E on 2010;17:448–56.
stroke subtypes: meta-analysis of randomised controlled trials. 66 NICE. NICE clinical guidelines. CG67 Lipid modification:
BMJ 2010;341:c5702. Cardiovascular risk assessment and the modification of blood
49 Lippman SM, Klein EA, Goodman PJ, et al. Effect of lipids for the primary and secondary prevention of
selenium and vitamin E on risk of prostate cancer and other cardiovascular disease. In: NICE, ed., 2010.
cancers: the Selenium and Vitamin E Cancer Prevention Trial 67 Baigent C, Keech A, Kearney PM, et al. Efficacy and safety of
(SELECT). JAMA 2009;301:39–51. cholesterol-lowering treatment: prospective meta-analysis of
50 McPherson S, Stewart SF, Henderson E, et al. Simple data from 90,056 participants in 14 randomised trials of
non-invasive fibrosis scoring systems can reliably exclude statins. Lancet 2005;366:1267–78.
advanced fibrosis in patients with non-alcoholic fatty liver 68 Athyros VG, Tziomalos K, Gossios TD, et al. Safety and
disease. Gut 2010;59:1265–9. efficacy of long-term statin treatment for cardiovascular
51 McPherson S, Anstee QM, Henderson E, et al. Are simple events in patients with coronary heart disease and abnormal
noninvasive scoring systems for fibrosis reliable in patients liver tests in the Greek Atorvastatin and Coronary Heart
with NAFLD and normal ALT levels?. Eur J Gastroenterol Disease Evaluation (GREACE) Study: a post-hoc analysis.
Hepatol 2013;25:652–8. Lancet 2010;376:1916–22.
52 NICE. NICE clinical guidelines. CG87 Type 2 diabetes: The 69 Singh S, Singh PP, Singh AG, et al. Statins Are Associated With
management of type 2 diabetes. In: NICE, ed., 2010. a Reduced Risk of Hepatocellular Cancer: a Systematic Review
53 Stratton IM, Adler AI, Neil HA, et al. Association of and Meta-analysis. Gastroenterology 2013;144:323–32.
glycaemia with macrovascular and microvascular 70 Musso G, Cassader M, Olivetti C, et al. Association of
complications of type 2 diabetes (UKPDS 35): prospective obstructive sleep apnoea with the presence and severity of
observational study. BMJ 2000;321:405–12. non-alcoholic fatty liver disease. A systematic review and
54 UK Prospective Diabetes Study (UKPDS) Group. Effect of meta-analysis. Obes Rev 2013;14:417–31.
intensive blood-glucose control with metformin on 71 Chung F, Yegneswaran B, Liao P, et al. STOP questionnaire: a
complications in overweight patients with type 2 diabetes tool to screen patients for obstructive sleep apnea.
(UKPDS 34). Lancet 1998;352:854–65. Anesthesiology 2008;108:812–21.
55 Nauck MA. A critical analysis of the clinical use of 72 Ascha MS, Hanouneh IA, Lopez R, et al. The incidence and
incretin-based therapies: the benefits by far outweigh the risk factors of hepatocellular carcinoma in patients with
potential risks. Diabetes Care 2013;36:2126–32. nonalcoholic steatohepatitis. Hepatology 2010;51:1972–8.
56 Armstrong MJ, Houlihan DD, Rowe IA, et al. Safety and 73 Bruix J, Sherman M, American Association for the Study of
efficacy of liraglutide in patients with type 2 diabetes and Liver. Management of hepatocellular carcinoma: an update.
elevated liver enzymes: individual patient data meta-analysis Hepatology 2011;53:1020–2.
of the LEAD program. Aliment Pharmacol Ther 74 European Association For The Study Of The Liver, European
2013;37:234–42. Organisation For Research And Treatment Of Cancer.
57 Bo S, Benso A, Durazzo M, et al. Does use of metformin EASL-EORTC clinical practice guidelines: management of
protect against cancer in Type 2 diabetes mellitus? J hepatocellular carcinoma. J Hepatol 2012;56:908–43.
Endocrinol Invest 2012;35:231–5. 75 Bolondi L. Screening for hepatocellular carcinoma in
58 Chen HP, Shieh JJ, Chang CC, et al. Metformin decreases cirrhosis. J Hepatol 2003;39:1076–84.
hepatocellular carcinoma risk in a dose-dependent manner: 76 Kim CK, Lim JH, Lee WJ. Detection of hepatocellular
population-based and in vitro studies. Gut 2013;62:606–15. carcinomas and dysplastic nodules in cirrhotic liver: accuracy
59 Marchesini G, Bugianesi E, Forlani G, et al. Nonalcoholic of ultrasonography in transplant patients. J Ultrasound Med
fatty liver, steatohepatitis, and the metabolic syndrome. 2001;20:99–104.
Hepatology 2003;37:917–23. 77 Kawada N, Imanaka K, Kawaguchi T, et al. Hepatocellular
60 Dixon JB, Bhathal PS, O’Brien PE. Nonalcoholic fatty liver carcinoma arising from non-cirrhotic nonalcoholic
disease: predictors of nonalcoholic steatohepatitis and liver steatohepatitis. J Gastroenterol 2009;44:1190–4.
fibrosis in the severely obese. Gastroenterology 78 Calle EE, Rodriguez C, Walker-Thurmond K, et al.
2001;121:91–100. Overweight, obesity, and mortality from cancer in a
61 NICE. NICE clinical guidelines. CG127 Hypertension: prospectively studied cohort of U.S. adults. NEJM
Clinical management of primary hypertension in adults. In: 2003;348:1625–38.
NICE, ed., 2011. 79 Gunter MJ, Hoover DR, Yu H, et al. Insulin, insulin-like
62 Bataller R, Sancho-Bru P, Gines P, et al. Activated human growth factor-I, and risk of breast cancer in postmenopausal
hepatic stellate cells express the renin-angiotensin system women. J Natl Cancer Inst 2009;101:48–60.
and synthesize angiotensin II. Gastroenterology 80 Giovannucci E. Metabolic syndrome, hyperinsulinemia, and
2003;125:117–25. colon cancer: a review. Am J Clin Nutr 2007;86:s836–42.
63 Paschos P, Tziomalos K. Nonalcoholic fatty liver disease and 81 Pollak M. Energy metabolism, cancer risk, and cancer
the renin-angiotensin system: implications for treatment. prevention. Recent Results Cancer Res 2009;181:51–4.
World J Hepatol 2012;4:327–31. 82 Choi YK, Park KG. Metabolic roles of AMPK and metformin
64 Georgescu EF, Ionescu R, Niculescu M, et al. in cancer cells. Mol Cells 2013;36:279–87.
Angiotensin-receptor blockers as therapy for 83 Zhou G, Myers R, Li Y, et al. Role of AMP-activated protein
mild-to-moderate hypertension-associated non-alcoholic kinase in mechanism of metformin action. J Clin Invest
steatohepatitis. World J Gastroenterol 2009;15:942–54. 2001;108:1167–74.
Dyson JK, et al. Frontline Gastroenterology 2014;0:1–10. doi:10.1136/flgastro-2013-100404 9
Downloaded from http://fg.bmj.com/ on May 28, 2015 - Published by group.bmj.com
LIVER
84 Donadon V, Balbi M, Ghersetti M, et al. Antidiabetic therapy history of variceal hemorrhage. Arch Intern Med
and increased risk of hepatocellular carcinoma in chronic liver 2001;161:2564–70.
disease. World J Gastroenterol 2009;5:2506–11. 93 Garcia-Tsao G, Sanyal AJ, Grace ND, et al. Prevention and
85 Hassan MM, Curley SA, Li D, et al. Association of diabetes management of gastroesophageal varices and
duration and diabetes treatment with the risk of variceal hemorrhage in cirrhosis. Hepatology
hepatocellular carcinoma. Cancer 2010;116:1938–46. 2007;46:922–38.
86 El-Serag HB, Johnson ML, Hachem C, et al. Statins are 94 Jalan R, Hayes PC. UK guidelines on the management of
associated with a reduced risk of hepatocellular carcinoma in variceal haemorrhage in cirrhotic patients. British Society of
a large cohort of patients with diabetes. Gastroenterology Gastroenterology. Gut 2000;46(Suppl 3–4):III1–III15.
2009;136:1601–8. 95 Collier JD, Ninkovic M, Compston JE. Guidelines on the
87 Chiu HF, Ho SC, Chen CC, et al. Statin use and the risk of management of osteoporosis associated with chronic liver
liver cancer: a population-based case-control study. Am J disease. Gut 2002;50(Suppl 1):i1–9.
Gastroenterol 2011;106:894–8. 96 Charlton MR, Burns JM, Pedersen RA, et al. Frequency and
88 Demierre MF, Higgins PD, Gruber SB, et al. Statins and outcomes of liver transplantation for nonalcoholic steatohepatitis
cancer prevention. Nat Rev Cancer 2005;5:930–42. in the United States. Gastroenterology 2011;141:1249–53.
89 Wu J, Wong WW, Khosravi F, et al. Blocking the Raf/MEK/ 97 Ratziu V, Bellentani S, Cortez-Pinto H, et al. A position
ERK pathway sensitizes acute myelogenous leukemia cells to statement on NAFLD/NASH based on the EASL 2009 special
lovastatin-induced apoptosis. Cancer Res 2004;64:6461–8. conference. J Hepatol 2010;53:372–84.
90 Shachaf CM, Kopelman AM, Arvanitis C, et al. MYC 98 Malik SM, Devera ME, Fontes P, et al. Recurrent disease
inactivation uncovers pluripotent differentiation and following liver transplantation for nonalcoholic steatohepatitis
tumour dormancy in hepatocellular cancer. Nature cirrhosis. Liver Transpl 2009;15:1843–51.
2004;431:1112–7. 99 Yalamanchili K, Saadeh S, Klintmalm GB, et al. Nonalcoholic
91 Cao Z, Fan-Minogue H, Bellovin DI, et al. MYC fatty liver disease after liver transplantation for cryptogenic
phosphorylation, activation, and tumorigenic potential in cirrhosis or nonalcoholic fatty liver disease. Liver Transpl
hepatocellular carcinoma are regulated by HMG-CoA 2010;16:431–9.
reductase. Cancer Res 2011;71:2286–97. 100 Newsome PN, Allison ME, Andrews PA, et al. Guidelines for
92 Zaman A, Becker T, Lapidus J, et al. Risk factors for the liver transplantation for patients with non-alcoholic
presence of varices in cirrhotic patients without a steatohepatitis. Gut 2012;61:484–500.
10 Dyson JK, et al. Frontline Gastroenterology 2014;0:1–10. doi:10.1136/flgastro-2013-100404
Downloaded from http://fg.bmj.com/ on May 28, 2015 - Published by group.bmj.com
Non-alcoholic fatty liver disease: a practical
approach to treatment
J K Dyson, Q M Anstee and S McPherson
Frontline Gastroenterol published online January 22, 2014
Updated information and services can be found at:
http://fg.bmj.com/content/early/2014/01/22/flgastro-2013-100404
These include:
References This article cites 94 articles, 22 of which you can access for free at:
http://fg.bmj.com/content/early/2014/01/22/flgastro-2013-100404
#BIBL
Open Access This is an Open Access article distributed in accordance with the Creative
Commons Attribution Non Commercial (CC BY-NC 3.0) license, which
permits others to distribute, remix, adapt, build upon this work
non-commercially, and license their derivative works on different terms,
provided the original work is properly cited and the use is
non-commercial. See: http://creativecommons.org/licenses/by-nc/3.0/
Email alerting Receive free email alerts when new articles cite this article. Sign up in the
service box at the top right corner of the online article.
Topic Articles on similar topics can be found in the following collections
Collections Open access (32)
Notes
To request permissions go to:
http://group.bmj.com/group/rights-licensing/permissions
To order reprints go to:
http://journals.bmj.com/cgi/reprintform
To subscribe to BMJ go to:
http://group.bmj.com/subscribe/
You might also like
- Process Plant Layout - Seán Moran 3-4Document2 pagesProcess Plant Layout - Seán Moran 3-4CunCunAlAndraNo ratings yet
- GF Signet 515 2536 Manual01Document1 pageGF Signet 515 2536 Manual01CunCunAlAndraNo ratings yet
- Process Plant Layout - Seán Moran 1-2Document2 pagesProcess Plant Layout - Seán Moran 1-2CunCunAlAndra100% (1)
- DA38 Safety Data Shett FAME (Fatty Acid Methyl Ester) V4 - en - DEDocument14 pagesDA38 Safety Data Shett FAME (Fatty Acid Methyl Ester) V4 - en - DECunCunAlAndraNo ratings yet
- Management Gathering 0718 - Distribution - v5 CoverDocument1 pageManagement Gathering 0718 - Distribution - v5 CoverCunCunAlAndraNo ratings yet
- RicoDocument62 pagesRicoCunCunAlAndraNo ratings yet
- Problem 5 Git: Ivan MichaelDocument68 pagesProblem 5 Git: Ivan MichaelCunCunAlAndraNo ratings yet
- Early Liver TransplantationDocument11 pagesEarly Liver TransplantationCunCunAlAndraNo ratings yet
- Pitri - GI.Pemicu 4. GE+ Tifus AbdominalisDocument154 pagesPitri - GI.Pemicu 4. GE+ Tifus AbdominalisCunCunAlAndraNo ratings yet
- Hay Day Price Profit AnalysisDocument112 pagesHay Day Price Profit AnalysisCunCunAlAndraNo ratings yet
- Breather Valve - Pressure-Vaccuem Relief ValveDocument2 pagesBreather Valve - Pressure-Vaccuem Relief Valvevphor85No ratings yet
- Hay Day Price Profit AnalysisDocument112 pagesHay Day Price Profit AnalysisCunCunAlAndraNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Insulin and IncretinsDocument6 pagesInsulin and IncretinspykkoNo ratings yet
- Controlling Blood Sugar With Cinnamon and Coffee Berry PDFDocument7 pagesControlling Blood Sugar With Cinnamon and Coffee Berry PDFLinda CarpenterNo ratings yet
- Science Behind Sunnah - Anas KhanDocument104 pagesScience Behind Sunnah - Anas KhanUsaid HussainNo ratings yet
- Cardiometabolic Syndrome: & DR Dhafir A. MahmoodDocument62 pagesCardiometabolic Syndrome: & DR Dhafir A. MahmoodJacob AlphaNo ratings yet
- Pleg CheckDocument46 pagesPleg CheckSehrish BajwaNo ratings yet
- Obesity Management As A Primary Treatment Goal For Type 2 DiabetesDocument12 pagesObesity Management As A Primary Treatment Goal For Type 2 DiabetesGonzalo Francisco Miranda ManriqueNo ratings yet
- Thibaudeau's Guide To Hypertrophy-Clean Health Fitness InstituteDocument219 pagesThibaudeau's Guide To Hypertrophy-Clean Health Fitness InstituteVíctor Tarín100% (13)
- Ibarra 2023 Safety and Effectiveness of A Standardized IntravenousDocument7 pagesIbarra 2023 Safety and Effectiveness of A Standardized IntravenousEdward ElBuenoNo ratings yet
- Obesity PathophysiologyDocument23 pagesObesity PathophysiologykotraeNo ratings yet
- Report DraftDocument100 pagesReport DraftishupandiNo ratings yet
- Module For Students 1 - 2 - 3-1 EditDocument15 pagesModule For Students 1 - 2 - 3-1 EditJanuardi IndraNo ratings yet
- Thomas2016 PDFDocument10 pagesThomas2016 PDFDr. Kaushal Kishor SharmaNo ratings yet
- EDITED ENDO50items 1Document12 pagesEDITED ENDO50items 1Darren Vargas100% (1)
- Eras ProtocolsDocument7 pagesEras ProtocolsSyed NusrathNo ratings yet
- Week 1 CH 48 DiabetesDocument115 pagesWeek 1 CH 48 DiabetesNeal PatelNo ratings yet
- 4 Cycle Rapid Fat Loss SolutionDocument22 pages4 Cycle Rapid Fat Loss SolutionRey Johnson100% (3)
- Journal A. Arviani Desianti NurDocument9 pagesJournal A. Arviani Desianti NurPengetikan ARVNo ratings yet
- Saturated Fats and Health: A Reassessment and Proposal For Food-Based RecommendationsDocument14 pagesSaturated Fats and Health: A Reassessment and Proposal For Food-Based RecommendationsMónika BokorNo ratings yet
- Sag 47 3 42 1503 90Document6 pagesSag 47 3 42 1503 90TanveerNo ratings yet
- FACULTATEA DE MEDICINĂ VETERINARĂ Lucrari StiintificeDocument148 pagesFACULTATEA DE MEDICINĂ VETERINARĂ Lucrari StiintificeCorina AlinaNo ratings yet
- Xylitol For HealthDocument24 pagesXylitol For HealthDonald WehmeyerNo ratings yet
- Geriatric EndocrinologyDocument65 pagesGeriatric EndocrinologyZaidanNo ratings yet
- 2501027Document9 pages2501027vishal makadiaNo ratings yet
- Insulin Resistance TestsDocument3 pagesInsulin Resistance TestsEsmeralda HerreraNo ratings yet
- Human NutritionDocument42 pagesHuman Nutritionila03100% (2)
- DM OAD 14 - RevDocument36 pagesDM OAD 14 - RevAri AsriniNo ratings yet
- Diabetes Mellitus in Children (Pedi Clinics of N. America Vol 52, No 6) WW PDFDocument275 pagesDiabetes Mellitus in Children (Pedi Clinics of N. America Vol 52, No 6) WW PDFEliMihaelaNo ratings yet
- Shahad 2Document5 pagesShahad 2Mohammed OmarNo ratings yet
- Egregious Eleven of Type 2 Diabetes Mellitus - My Endo ConsultDocument20 pagesEgregious Eleven of Type 2 Diabetes Mellitus - My Endo Consultakbar011512No ratings yet
- Lecture No:10 Diabetes Mellitus: - at The End of This Lecture, Student Will Be Able To ExplainDocument33 pagesLecture No:10 Diabetes Mellitus: - at The End of This Lecture, Student Will Be Able To ExplainAntoNo ratings yet