Professional Documents
Culture Documents
Hep B Vaccine
Uploaded by
Jeremy SuhardiOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Hep B Vaccine
Uploaded by
Jeremy SuhardiCopyright:
Available Formats
Incidence
- ~ 1000 new cases of perinatal hep B infection annually in the USA
- Transmission ranges from 30 % when HbeAg negative to ~ 85 % when mother HBeAg positive
- Chronic Hep B affects 90% of infants infected with Hep B at birth or within first year of life.
- 25 % mortality due to hepatocellular carcinoma or liver cirrhosis if untreated
Efficacy:
- Vaccine alone is 75-95 % effective in preventing perinatal hepatitis B transmission when given
within 24 hr of birth
- When postexposure prophylaxus with both hepatitis B vaccine and HBIG given, infection range
from 0.7-1.1 %
Recommendation:
- In 2005, ACIP and CDC allowed delay of hepatitis B vaccine
- In 2014, QI study found that only 72 % of infants received birth dose of hep B vaccine, less than
the Healthy People 2020 target of 85 %.
- In 2016, ACIP stated that infants >= 2000 gram at birth and born to HBsAg neg mothers should
receive hep B vaccine within 24 hr of birth.
- Birth dose hepatitis B vaccine is a critical safety net to protect infants born to hepatitis B-
infected mothers not identified at the time of birth, misinterpreted, false negative, reported
inaccurately, or not communicated at all.
- Birth dose also provides protection to infants at risk from household exposure after the
perinatal period.
- In general no significant differences among different doses, different schedules, and different
forms of plasma derived vaccine and recombinant vaccine on hepatitis B occurrence.
- No strong association between timing of injection (within 12, 24, or 48 hours) and magnitude of
effects. The number of infants evaluated in these comparisons was small. Therefore larger trials
are needed before equivalence or non-inferiority can be claimed.
- No difference between plasma derived and yeast derived vaccine (Heptavax vs Recombivax)
Result:
- After completion of 3-4 dose of He B vaccine, 98 % achieve protective antibody concentration
- Test serology 1-2 months after final hep B vaccine
- For infants born to HBsAg-positive mothers, postvaccination serologic testing by measuring hepatitis
B surface antibody (anti-HBs) to document protection and HBsAg to rule out perinatal infection now
is recommended at 9 to 12 months of age instead of 9 to 18 months.
- Infants who are HBsAg negative with anti-HBs levels less than 10 mIU/mL (nonprotective) require
additional vaccine doses.
- HBsAg-negative infants with anti-HBs levels less than 10 mIU/mL receive a single additional dose of
hepatitis B vaccine and be retested for anti-HBs 1 to 2 months after that vaccine dose.
- If the anti-HBs level is still less than 10 mIU/mL, the infant should receive 2 additional doses of
hepatitis B vaccine followed by retesting 1 to 2 months later.
- Infants with anti-HBs levels less than 10 mIU/mL after 2 3-dose series of hepatitis B vaccine are
nonresponders, and available data do not suggest benefit from additional vaccinations.
- The ACIP noted that, on the basis of clinical circumstance or family preference, HBsAg-negative
infants with anti-HBs levels less than 10 mIU/mL may be vaccinated instead with a second complete
series followed by postvaccination testing 1 to 2 months after the final dose.
Vaccine Adverse Effects:
- Pain (3%–29%), erythema (3%), swelling (3%), fever (1%–6%), and headache (3%).
- No evidence of a causal association between receipt of hepatitis B vaccine and neonatal sepsis or
death, rheumatoid arthritis, Bell’s palsy, autoimmune thyroid disease, hemolytic anemia in
children, anaphylaxis, optic neuritis, Guillain-Barré syndrome, sudden-onset sensorineural
hearing loss, or other chronic illnesses has been demonstrated through analysis of data from the
Vaccine Safety Datalink
References:
Committee on Infectious Disease, Committee on Fetus and Newborn. Elimination of Perinatal Hepatitis
B: Providing the First Vaccine Within 24 hours of Birth. Pediatrics, 2017, 140(3)
Lee C, Gong Y, Brok J, Boxall EH, Gluud C. Effect of Hepatitis B immunization in newborn infants of
mothers positive for hepatitis B surface antigen: systematic review and meta-analysis. BMJ,
2006;332(7537):328–336pmid:16443611
You might also like
- Hep B in NewbornDocument6 pagesHep B in NewbornPutu Reza Sandhya PratamaNo ratings yet
- HepB Provider Tipsheet 508Document2 pagesHepB Provider Tipsheet 508Jamshaid AhmedNo ratings yet
- Hepatitis B Vaccines: Susan Goldstein, M.D. Division of Viral Hepatitis Centers For Disease Control and PreventionDocument30 pagesHepatitis B Vaccines: Susan Goldstein, M.D. Division of Viral Hepatitis Centers For Disease Control and Prevention99manu99No ratings yet
- Hepatitis B Vaccination PresDocument21 pagesHepatitis B Vaccination PresmaponlooNo ratings yet
- Immune Persistence After Infant Hepatitis-B Vaccination: A Systematic Review and Meta-AnalysisDocument8 pagesImmune Persistence After Infant Hepatitis-B Vaccination: A Systematic Review and Meta-AnalysisValentin CalugareanuNo ratings yet
- Twinrix Product MonographDocument27 pagesTwinrix Product Monographandy175No ratings yet
- Hepatitis B (HepB) Vaccine - Infectious Diseases - MSD Manual Professional EditionDocument4 pagesHepatitis B (HepB) Vaccine - Infectious Diseases - MSD Manual Professional EditiondianavemNo ratings yet
- Immunizations: Policies and Procedures: Intensive Care Nursery House Staff ManualDocument2 pagesImmunizations: Policies and Procedures: Intensive Care Nursery House Staff ManualSedaka DonaldsonNo ratings yet
- Book One ExcerptDocument8 pagesBook One Excerptdrakola61No ratings yet
- HHS Public AccessDocument21 pagesHHS Public AccessA AnonimyNo ratings yet
- Jurnal Al-ImDocument19 pagesJurnal Al-ImIis Rica MustikaNo ratings yet
- Hepatitis B in PregnancyDocument6 pagesHepatitis B in PregnancyherryNo ratings yet
- Hepatitis B QuizDocument2 pagesHepatitis B QuizBianca Watanabe - RatillaNo ratings yet
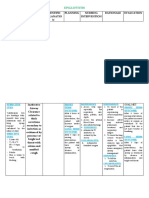
- Drug Study 12Document4 pagesDrug Study 12Nathalie kate petallarNo ratings yet
- Preventing Hiv Infection in InfantsDocument3 pagesPreventing Hiv Infection in Infantskareem92No ratings yet
- CDC Vaccination of Preterm Infants RecommendationsDocument1 pageCDC Vaccination of Preterm Infants Recommendationskevin hernandezNo ratings yet
- Vertical Transmission of HBV: Stephan Ehrhardt MD, MPHDocument15 pagesVertical Transmission of HBV: Stephan Ehrhardt MD, MPHDr-Mohamed KadleNo ratings yet
- Vaccine Indication and ContraindicationDocument34 pagesVaccine Indication and ContraindicationMusa yohanaNo ratings yet
- Tenofovir Untuk Mencegah Transmisi Mother To Child Pada Ibu Dengan Viral Load TinggiDocument18 pagesTenofovir Untuk Mencegah Transmisi Mother To Child Pada Ibu Dengan Viral Load TinggiMarthaLhtNo ratings yet
- Hepatitis B Vaccine Alone May Be Enough For Preventing Hepatitis B Virus Transmission in Neonates of Hbsag (+) /hbeag (-) MothersDocument24 pagesHepatitis B Vaccine Alone May Be Enough For Preventing Hepatitis B Virus Transmission in Neonates of Hbsag (+) /hbeag (-) MothersRafika RaraNo ratings yet
- Hepatitis Viruses and The Newborn - Clinical Manifestations and Treatment - UpToDateDocument17 pagesHepatitis Viruses and The Newborn - Clinical Manifestations and Treatment - UpToDateTan Fransisca DianNo ratings yet
- Piis0025619619305737 220530 065558Document11 pagesPiis0025619619305737 220530 065558Garcia Yepez Stephanie GraceNo ratings yet
- Typhoid Fever Follow-Up PDFDocument16 pagesTyphoid Fever Follow-Up PDFPlot BUnniesNo ratings yet
- Adult Immunization: It's Your Best Shot!Document40 pagesAdult Immunization: It's Your Best Shot!minerva_stanciuNo ratings yet
- Diagnosis/vaccination/: Hepatitis B VaccineDocument6 pagesDiagnosis/vaccination/: Hepatitis B Vaccinereza satriaNo ratings yet
- Hilary Butler Hep B VaxDocument14 pagesHilary Butler Hep B VaxMeryl DoreyNo ratings yet
- Jourdain (2018)Document13 pagesJourdain (2018)nam dinhNo ratings yet
- National Perinatal Hepatitis B Prevention Program: 2009 - 2017Document10 pagesNational Perinatal Hepatitis B Prevention Program: 2009 - 2017Suwandi ChangNo ratings yet
- Hep BDocument47 pagesHep BMia Mia MiaNo ratings yet
- Foaud 2015Document8 pagesFoaud 2015Glabela Christiana PandangoNo ratings yet
- BCG and Hepatitis BDocument23 pagesBCG and Hepatitis BMichael LinebargerNo ratings yet
- Kepi Vaccines (2) - Gi - 1Document30 pagesKepi Vaccines (2) - Gi - 1okwadha simionNo ratings yet
- Chronic He PB Testing FL W UpDocument2 pagesChronic He PB Testing FL W UpSumit MitraNo ratings yet
- CPG On Immunization For WomenDocument28 pagesCPG On Immunization For WomenYnoli DiosomitoNo ratings yet
- Dr. Ali's Uworld Notes For Step 2 CKDocument30 pagesDr. Ali's Uworld Notes For Step 2 CKuyesNo ratings yet
- Jama Sha 2019 It 190019Document2 pagesJama Sha 2019 It 190019xtineNo ratings yet
- Give Birth Dose PDFDocument2 pagesGive Birth Dose PDFLuzNo ratings yet
- Immunization and Prophylaxis: Childhood Immunization Has Reduced The Impact - Active Immunization Is TheDocument18 pagesImmunization and Prophylaxis: Childhood Immunization Has Reduced The Impact - Active Immunization Is TheCabdiNo ratings yet
- Hepatitis in PregnancyDocument8 pagesHepatitis in PregnancyAfiat Wijaya100% (1)
- Congenital Syphilis Treatment and PreventionDocument1 pageCongenital Syphilis Treatment and PreventionMuhammad Naufal FadhillahNo ratings yet
- Dr. Elham Bukhari: Aediatri Nfectious IseaseDocument56 pagesDr. Elham Bukhari: Aediatri Nfectious IseaseJim Jose AntonyNo ratings yet
- Community Health Nursing (Learning Feedback Diary (LFD #25)Document3 pagesCommunity Health Nursing (Learning Feedback Diary (LFD #25)Angelica Malacay RevilNo ratings yet
- Hiv in PregnancyDocument8 pagesHiv in Pregnancyjh6svdhxmxNo ratings yet
- Effect of Viral Load On Pregnancy Outcomes in Chronic Hepatitis B InfectionDocument6 pagesEffect of Viral Load On Pregnancy Outcomes in Chronic Hepatitis B Infectionnisaa 2000No ratings yet
- Hepatitis B VaccineDocument6 pagesHepatitis B VaccineAziil LiizaNo ratings yet
- Hepatitis BBB PDFDocument12 pagesHepatitis BBB PDFRizki Cah KeratonNo ratings yet
- Hepatitisbinpregnant Womenandtheirinfants: Alicia M. Cryer,, Joanne C. ImperialDocument12 pagesHepatitisbinpregnant Womenandtheirinfants: Alicia M. Cryer,, Joanne C. Imperialafriany syamsirNo ratings yet
- C. 48-Year-Old Man Who Has Sex With Men: AlasanDocument12 pagesC. 48-Year-Old Man Who Has Sex With Men: AlasanAjeng WidyastutiNo ratings yet
- 07 Childschd 6x4.5 1-Page PRDocument2 pages07 Childschd 6x4.5 1-Page PRSteluta GalbenusNo ratings yet
- LabCorpTestingProtocol6 08Document4 pagesLabCorpTestingProtocol6 08Olga CîrsteaNo ratings yet
- Adult ImmunizationDocument6 pagesAdult ImmunizationAmit GoelNo ratings yet
- 3vaccin Hepatitic BDocument9 pages3vaccin Hepatitic BCristina BalanNo ratings yet
- Paed Prelim SummaryDocument10 pagesPaed Prelim SummaryNatukunda DianahNo ratings yet
- Viral Hepatitis BDocument15 pagesViral Hepatitis BRahul GaudhamNo ratings yet
- Recombivax HB®: Hepatitis B Vaccine (Recombinant)Document13 pagesRecombivax HB®: Hepatitis B Vaccine (Recombinant)Mimô SANo ratings yet
- JR Paediatric HIVDocument8 pagesJR Paediatric HIVAbdul Hakim Abdul KadirNo ratings yet
- Neonatal Immunization: Hepatitis B Vaccine Can Prevent Hepatitis B and Its ConsequencesDocument3 pagesNeonatal Immunization: Hepatitis B Vaccine Can Prevent Hepatitis B and Its ConsequencesMahmoud AbouelsoudNo ratings yet
- Health Advice and Immunizations for TravelersFrom EverandHealth Advice and Immunizations for TravelersNo ratings yet
- USMLE Step 3 Lecture Notes 2021-2022: Internal Medicine, Psychiatry, EthicsFrom EverandUSMLE Step 3 Lecture Notes 2021-2022: Internal Medicine, Psychiatry, EthicsRating: 5 out of 5 stars5/5 (9)
- Vaccines: Does herd immunity justify permanent impairment for a few?From EverandVaccines: Does herd immunity justify permanent impairment for a few?No ratings yet
- 2011 Urine Therapy J of NephrolDocument3 pages2011 Urine Therapy J of NephrolCentaur ArcherNo ratings yet
- BNMHGDocument34 pagesBNMHGAnonymous lt2LFZHNo ratings yet
- Bicon Product Catalog 2013Document12 pagesBicon Product Catalog 2013Bicon Implant InaNo ratings yet
- Patrick Callaghan, Helen Waldock-Emergencies in Mental Health Nursing-Oxford University Press (2013)Document195 pagesPatrick Callaghan, Helen Waldock-Emergencies in Mental Health Nursing-Oxford University Press (2013)VidákZsigmond100% (2)
- R4 HealthfacilitiesDocument332 pagesR4 HealthfacilitiesCarl Joseph BarcenasNo ratings yet
- Vstep Tests B1 B2 C1 Full KeyDocument162 pagesVstep Tests B1 B2 C1 Full KeyLe Hoang LinhNo ratings yet
- Epiglottitis: Assessment Nursing Diagnosis Scientific Explanatio N Planning Nursing Intervention Rationale EvaluationDocument3 pagesEpiglottitis: Assessment Nursing Diagnosis Scientific Explanatio N Planning Nursing Intervention Rationale EvaluationfifiNo ratings yet
- National Programme For Prevention and Control of FluorosisDocument49 pagesNational Programme For Prevention and Control of FluorosisveereshNo ratings yet
- 3f PDFDocument4 pages3f PDFYidne GeoNo ratings yet
- Acetylsalicylic AcidDocument6 pagesAcetylsalicylic AcidAdmin DownloadNo ratings yet
- TPF00391-3 Hotline BrochureDocument6 pagesTPF00391-3 Hotline BrochureAphichetNo ratings yet
- As 3789.2-1991 Textiles For Health Care Facilities and Institutions Theatre Linen and Pre-PacksDocument9 pagesAs 3789.2-1991 Textiles For Health Care Facilities and Institutions Theatre Linen and Pre-PacksSAI Global - APACNo ratings yet
- How To Sleep BetterDocument9 pagesHow To Sleep BetterMariaNo ratings yet
- Pork TocinoDocument1 pagePork TocinoMaria Ivz ElborNo ratings yet
- How To Write A Case Report PDFDocument6 pagesHow To Write A Case Report PDFironNo ratings yet
- Disaster Readiness Risk Reduction: Quarter 2-Module 13: DRR-related Laws and PoliciesDocument16 pagesDisaster Readiness Risk Reduction: Quarter 2-Module 13: DRR-related Laws and PoliciesUel Cabz LaquihonNo ratings yet
- Case Group 1Document10 pagesCase Group 1JASMEEN RAVALNo ratings yet
- Module 3 - Health-Optimizing Physical EducationDocument13 pagesModule 3 - Health-Optimizing Physical EducationLazyy TanakaNo ratings yet
- Todentj 9 250 PDFDocument7 pagesTodentj 9 250 PDFRSU DUTA MULYANo ratings yet
- 10 - The Generics Act of 1988Document22 pages10 - The Generics Act of 1988rhydelNo ratings yet
- Internet Addiction Kids and The South Korean Govt Boot CampsDocument5 pagesInternet Addiction Kids and The South Korean Govt Boot Campslgheorma0No ratings yet
- Knee Pain and The Internal Arts: Correct Alignment (Standing)Document7 pagesKnee Pain and The Internal Arts: Correct Alignment (Standing)Gabriel PedrozaNo ratings yet
- Effectiveness of Maitland vs. Mulligan Mobilization Techniques in (Ingles)Document4 pagesEffectiveness of Maitland vs. Mulligan Mobilization Techniques in (Ingles)mauricio castroNo ratings yet
- NT90004212Document58 pagesNT90004212Jelena ĆukNo ratings yet
- Environmental Law Transcription Atty BatacanDocument30 pagesEnvironmental Law Transcription Atty BatacanMa Gloria Trinidad Arafol100% (1)
- Common Core Principles and Competences For Social Care and Health Workers Working With Adults at The End of LifeDocument20 pagesCommon Core Principles and Competences For Social Care and Health Workers Working With Adults at The End of LifeEng Stephen ArendeNo ratings yet
- Objectives of The Nairobi SummitDocument12 pagesObjectives of The Nairobi SummitJoachim ChijideNo ratings yet
- Agri SBA (Broiler)Document20 pagesAgri SBA (Broiler)Shanti KissoondyalNo ratings yet
- Health EducationDocument8 pagesHealth EducationJamie Rose FontanillaNo ratings yet
- Dokumen - Tips Biology Investigatory Project 561e79b91f5a0Document17 pagesDokumen - Tips Biology Investigatory Project 561e79b91f5a0Upendra LalNo ratings yet