Professional Documents
Culture Documents
Rokok Turunkan Simptom Negatif
Uploaded by
RollandCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Rokok Turunkan Simptom Negatif
Uploaded by
RollandCopyright:
Available Formats
Investigation of Cigarette Smoking among Male
Schizophrenia Patients
Jundong Jiang1,2, Yuen Mei See1, Mythily Subramaniam1,3, Jimmy Lee1,3,4*
1 Research Division, Institute of Mental Health/Woodbridge Hospital, Singapore, Singapore, 2 Saw Swee Hock School of Public Health, National University of Singapore,
Singapore, Singapore, 3 Department of General Psychiatry 1, Institute of Mental Health/Woodbridge Hospital, Singapore, Singapore, 4 Duke-NUS Graduate Medical
School, National University of Singapore, Singapore, Singapore
Abstract
Male schizophrenia patients are known to have a heavier smoking pattern compared with the general population. However,
the mechanism for this association is not known, though hypothesis that smoking could alleviate symptomatology of
schizophrenia and reduce side effects of antipsychotics has been suggested. The aims of this study were to validate the
heavier smoking pattern among male schizophrenia patients and to investigate the possible mechanisms for the
association. To enhance the reliability of the study, we recruited two large independent samples with 604 and 535 male
Chinese schizophrenia patients, and compared their smoking pattern with that of 535 healthy male controls recruited from
general population. Validated multiple indicators and multiple causes structure equation model and regression models
were used to investigate the association of smoking with factors of schizophrenia symptomatology and with the usage of
antipsychotics and their extra-pyramidal side effects (EPS). Schizophrenia patients had significantly heavier smoking pattern
compared with healthy controls in our sample (42.4% vs. 16.8%, p,0.001 for current smoking prevalence; 23.5% vs. 43.3%,
p,0.001 for smoking cessation rate; 24.5% vs. 3.0%, p,0.001 for heavy smoker proportion). Their smoking status was also
found to be consistently and significantly associated with reduced negative factor scores for schizophrenia symptomatology
(b = 20.123, p = 0.051 for sample-A; b = 20.103, p = 0.035 for sample-B; b = 20.082, p = 0.017 for the combined sample).
However, no significant association was found between smoking and antipsychotics usage or risk of EPS. These results
support that smoking is associated with improved negative symptoms, which could account for the heavier smoking
pattern among schizophrenia patients.
Citation: Jiang J, See YM, Subramaniam M, Lee J (2013) Investigation of Cigarette Smoking among Male Schizophrenia Patients. PLoS ONE 8(8): e71343.
doi:10.1371/journal.pone.0071343
Editor: Josef Priller, Charité-Universitätsmedizin Berlin, Germany
Received February 17, 2013; Accepted July 1, 2013; Published August 15, 2013
Copyright: ß 2013 Jiang et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits
unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Funding: The Singapore Translational and Clinical Research in Psychosis is supported by the National Research Foundation Singapore under the National Medical
Research Council Translational and Clinical Research Flagship Programme (grant number NMRC/TCR/003/2008). The funders had no role in study design, data
collection and analysis, decision to publish, or preparation of the manuscript.
Competing Interests: The authors have declared that no competing interests exist.
* E-mail: jimmy_lee@imh.com.sg
Introduction cortex and could also increase hepatic clearance of antipsychotics
by activating cytochrome P450 enzymes [11]. As such, the EPS of
Schizophrenia patients have been widely reported to have antipsychotics, which are expressed as involuntary movement
heavier smoking pattern when compared with general population symptoms, are believed to be alleviated by smoking. Studies
and patients with other mental disorders. De Leon et al. [1] showing that schizophrenia patients with high dose of antipsy-
reviewed 42 studies across 20 nations and found that the current chotics tended to be heavier smokers appear to support this
smoking rate among male schizophrenia patients was constantly explanation [12–14]. However, studies that directly examine the
higher than that of general population. Numerous studies have effects of smoking on the EPS of antipsychotics (e.g., dyskinesia)
also found that schizophrenia patients tend to consume higher tar yield conflicting results [7,15], suggesting that this hypothesis
and higher nicotine containing cigarettes and to extract more needs further studies.
nicotine from smoking [2–4]. In addition, cessation rate of Another hypothesis for heavy smoking pattern among schizo-
smoking was also found to be significantly lower among male phrenia patients is that smoking could alleviate schizophrenia
schizophrenia patients [5–7]. This heavier smoking pattern may symptomatology, particularly negative symptoms, by improving
impose a significant burden on patients with schizophrenia since the sensory gating deficit and raising dopamine levels in brain
20% of reduction in life expectancy among patients with psychotic [16,17]. Experimental and observational studies have provided
disorders is thought to be contributed by smoking [8]. support for this explanation by finding an association between
The reason for the heavy smoking pattern among schizophrenia heavier smoking and improved negative symptoms [18,19].
patients is not known. One widely believed explanation was that However, evidence on the association is not consistent since
smoking could reduce the side effects of antipsychotics [9,10]. insignificant findings have also been reported [20–22]. Small
Antipsychotics act by blocking dopamine receptors and can trigger sample size might contribute to the insignificant findings as the
various side effects including extrapyramidal side effects (EPS). studies may lack the power to detect the difference if effects of
Nicotine in cigarette could induce dopamine release in pre-frontal smoking are small. In addition, the subscale scores (i.e., positive,
PLOS ONE | www.plosone.org 1 August 2013 | Volume 8 | Issue 8 | e71343
Smoking and Schizophrenia
negative, and general psychopathology) of the Positive and either current- or ex-smokers. Among the current smokers,
Negative Syndrome Scale (PANSS) are conventionally used to subjects were classified as light smoker if they smoked 10 cigarettes
represent the severity of symptoms. However, these three subscales or less per day and were classified as heavy smoker if they smoked
effectively represent a mixture of dimensions of symptoms since more than 10 cigarettes per day. The medication profile of
PANSS has been found to measure up to 5 dimensions of schizophrenia patients were collected from hospital records and
symptomatology [23]. Since smoking may not have the same the total daily antipsychotics dose was computed by summation of
effects on all the factors of the symptoms, not taking the structure the daily chlorpromazine equivalent dose of all prescribed
of PANSS into account may also affect the findings on the antipsychotics [25]. The EPS of antipsychotics were assessed by
association of smoking and symptomatology. two instruments: Abnormal Involuntary Movement Scale (AIMS)
The aims of this study were to examine the smoking pattern and Simpson-Angus Scale (SAS) instruments [26,27]. Based on
among male Chinese schizophrenia patients in Singapore. We also AIMS score, patients were classified as tardive dyskinesia, which is
attempted to investigate the possible mechanisms for their heavy a chronic movement disorder characterized by repetitive, invol-
smoking pattern by examining the association of smoking with untary and purposeless movements, according to the Schooler and
symptomatology of schizophrenia and with antipsychotics usage Kane criteria [28]. Based on SAS score, patients were classified to
and their side effects. To enhance the reliability of the study, two have drug-induced Parkinsonism, a syndrome characterized by
independent study samples of male schizophrenia patients were extrapyramidal rigidity, tremor at rest, and postural instability, if
recruited. We have previously reported a validated 5-factor the score is more or equal to 3.
structure model of the PANSS [24], which we applied to examine
the association of smoking with the symptom factors of schizo- Statistical Analysis
phrenia. The findings of this study could reveal the smoking In comparing the smoking pattern between patients with
pattern among male schizophrenia patients and could also help in schizophrenia and healthy controls, Chi-squared test was used in
understanding the mechanism for persistent smoking among them. assessing the significance for nominal and ordinal outcomes and t-
test with unequal variance was used to assess the significance for
Methods continuous outcomes. Adjusted p values for smoking rate were
computed by logistic regression to control for covariates including
Ethics Statement age, education, occupation and living apartment type, which
This study, including the consent process, was approved by the might have effects on smoking pattern.
National Healthcare Group Domain Specific Review Board of In elucidating the association of smoking with symptomatology
Singapore. Written informed consent was obtained from all study of schizophrenia, a multiple indicators and multiple causes
participants who were recruited into the study before any (MIMIC) structure equation model was used. The model was
assessments. Participation was voluntary and participants were derived based on the validated factor model of PANSS identified
allowed to reject or withdraw at any point with no disadvantage to in our previous study [24]. In the model, the 30 items of PANSS
their treatments. were deconstructed into 5 latent factors: positive factor, negative
factor, depression factor, excitement factor, and cognitive factor.
Sample Recruitments Each factor was measured by a subset of the 30 items, and
Male patients with schizophrenia were recruited from the represented a distinct dimension of schizophrenia symptoms. Each
Institute of Mental Health (IMH) in Singapore under the of the five factors was hypothesized to depend on current smoking
Singapore Translational & Clinical Research in Psychosis status (i.e., non-smoker, light smokers and heavy smokers) and
(STCRP) program. Two independent study samples were recruit- antipsychotics dose, which had a major effect in influencing
ed under this project: Sample-A was recruited between 2005 and current symptoms. The effect size of smoking on symptomatology
2008 and consisted of 604 male patients with schizophrenia; after controlling for antipsychotics usage could be assessed by its
Sample-B was recruited between 2008 and 2012 and consisted of loading and significance on the five latent factors. To achieve
535 male patients. In both samples, patients were included if they reliability, we applied the model on the two independent datasets
were of Chinese ethnicity and met DSM-IV-TR diagnostic criteria (i.e., Sample-A and Sample-B) separately and also on the
for schizophrenia, and if they consented to participate in our combined dataset to examine the consistency of the effects of
study. Patients were excluded from the study if they had organic smoking. In elucidating the association of smoking with antipsy-
brain causes for psychosis, mental retardation or a current chotics usage and its EPS, general linear model with log link (i.e.,
substance use disorder. A total of 535 healthy male controls were for antipsychotic dose) or logit link (i.e., for tardive dyskinesia and
also recruited from the community in Singapore between 2008 drug-induced Parkinsonism) was used to accommodate the
and 2012 to serve as a reference comparison group. The controls distribution of the dependent variables (i.e., antipsychotics dose
were included into the study if they were of Chinese ethnicity, and distribution was positively skewed; tardive dyskinesia or drug-
they were excluded from the study if they had a history of induced Parkinsonism was binomially distributed).
psychiatric disorders, except for nicotine related disorders. Comparisons of smoking pattern were performed under
STATA 10.0, and examination of the association of smoking with
Measures and Covariates the factors of schizophrenia symptomatology was performed under
All participants were assessed with the Structured Clinical Mplus 6.11.
Interview for DSM-IV-TR (SCID) and PANSS by clinicians and
research psychologists, who were trained on the administration of Results
the instruments. Demographic and smoking information were
collected during an interview. Both patients and controls were Descriptive Statistics of Study Samples
classified as current-smoker if they smoked at least one cigarette Descriptive statistics of the three study samples are showed in
per day at the point of assessment. They were classified as ex- Table 1. Healthy controls were younger than patients from both
smoker if they had smoked in the past but had quit smoking at the samples, and patients from Sample-B were younger than patients
time of assessment. Ever-smoker was defined as those who were from Sample-A. Patients had significantly lower socio-economic
PLOS ONE | www.plosone.org 2 August 2013 | Volume 8 | Issue 8 | e71343
Smoking and Schizophrenia
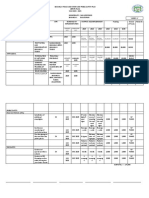
Table 1. Descriptive statistics of the three independent study samples.
Sample-A Cases1 Sample-B Cases2 Healthy Controls
N = 604 N = 535 N = 535 Nominal p value3
Age (yrs) 49.2613.1 41.8610.9 33.1610.2 ,0.001
Antipsychotics dose (CPZ equivalents, mg) 491.56527.1 424.56433.5 –
PANSS
Positive subscale 9.9163.79 11.865.74 –
Negative subscale 12.365.27 12.966.31 –
General psychopathology subscale 21.365.27 24.168.77 –
Tardive dyskinesia percentage 25.5% – –
Drug-induced Parkinsonism percentage 32.1% – –
Education ,0.001
Less than Primary4 – 0.39% 0.00%
Primary – 19.3% 1.33%
Secondary – 49.4% 25.3%
Junior College or polytechnic – 19.3% 27.6%
University or higher – 11.6% 45.7%
Living Apartment – ,0.001
1-room – 8.32% 0.23%
2/3-room – 31.3% 15.2%
4/5-room – 41.0% 64.8%
Private house – 3.46% 12.1%
Others4 – 15.5% 7.69%
Occupation ,0.001
Unemployed – 55.7% 7.94%
Manual labor – 4.47% 0.95%
Admin and sales – 3.89% 8.32%
Professional management – 0.78% 14.5%
Others4 – 35.2% 68.2%
1
Education, living apartment and occupation information were not collected for sample-A.
2
AIMS and SAS assessments were only performed on patients in Sample-A. Therefore, tardive dyskinesia and drug-induced Parkinsonism status were not available for
Sample-B.
3
Nominal p values were computed based on Sample-B cases and healthy controls.
4
The group was used as reference group in regression analysis.
doi:10.1371/journal.pone.0071343.t001
status than healthy controls (i.e., lower education, smaller patients from Sample-A had slightly lower smoking prevalence and
apartments and higher unemployment rate). About one quarter higher quitting rate.
(25.5%) of patients in Sample-A had tardive dyskinesia disorder
and about one third (32.1%) of them had drug-induced Association of Smoking with Antipsychotics Usage and
Parkinsonism. their Extra-pyramidal Side Effects
As shown in Table 3, the association of smoking with
Smoking Pattern of Schizophrenia Patients antipsychotics dose was inconsistent and insignificant after
As shown in Table 2, the prevalence of smoking in patients was adjusting for symptoms severity (p = 0.182, 0.058, 0.740, for
significantly higher than that of healthy controls (54.1% vs. 29.3% sample-A, sample-B, and combined sample). No significant
for life time prevalence, RR = 1.83, p,0.001; 42.4% vs. 16.8% for association was found between smoking and tardive dyskinesia
current prevalence, RR = 2.52, p,0.001; RR stands for relative or drug-induced Parkinsonism, which are due to EPS of
risk). The current cessation rate, which measures the proportion of antipsychotics.
smokers who had quit smoking by the time of assessment, was also
significantly lower for schizophrenia patients (23.5% vs. 43.3%, Association of Smoking with Symptomatology of
RR = 0.54, p,0.001). Both current smoking rate and cessation
rate remained to be highly significant even after controlling for Schizophrenia
age, education, occupation, and living apartment (p = 0.002 for The association of smoking on symptomatology were assessed
current smoking rate and p = 0.004 for cessation rate). All smoking based on the MIMIC structural equation model as depicted in
metrics between Sample-A and Sample-B were not significantly Figure 1. The 30 items of PANSS were deconstructed into 5
different (p value = 0.126, 0.707, 0.290, 0.277 for current-smoker, factors based on our previous validated factor analysis of PANSS
ex-smoker, ever-smoker and cessation rate, respectively), though [24]: Positive factor was measured by P1delusions, P3 hallucina-
PLOS ONE | www.plosone.org 3 August 2013 | Volume 8 | Issue 8 | e71343
Smoking and Schizophrenia
Table 2. Comparison of smoking patterns between schizophrenia male patients and male healthy controls.
Sample-A Sample-B Healthy controls Risk Ratio (RR)/ Adjusted p
N = 604 N = 535 N = 535 difference1 P value1 value2
Ever smoker 50.9% 54.1% 29.5% 1.83 ,0.001 0.129
Current smoker 37.9% 42.4% 16.8% 2.52 ,0.001 0.002
Ex-smoker 13.4% 12.7% 12.8% 1.00 0.957 0.143
Cessation rate 26.9% 23.5% 43.3% 0.54 ,0.001 0.004
Current smoking status ,0.001 ,0.001
Non-smoker 62.1% 55.3% 82.6%
Light smoker 13.4% 14.4% 11.6%
Heavy smoker 13.9% 24.5% 3.00%
Missing 10.6% 5.79% 2.80%
Smoking starting age3 – 24.1 24.0 0.1 0.920 0.042
Smoking starting age w.r.t – 0.045 – – 0.951 –
onset of psychosis (yrs)3
1
Measures were obtained based on Sample-B cases and healthy controls.
2
Adjusted p values were computed after controlling for age, education, living apartments and occupation.
3
Smoking starting age information was not collected for sample-A.
doi:10.1371/journal.pone.0071343.t002
tions, P6 suspiciousness and G9 unusual thought content; negative sample, respectively). Smoking seemed to increase the excitement
factor was measured by N2 emotional withdrawal, N3 poor dimension of the symptoms (b = 0.085, p,0.05 for the combined
rapport, N4 social withdrawal, N6 lack of spontaneity and G7 sample), but it did not reach significance in the individual study
motor retardation; excitement factor was measured by P4 samples.
excitement, P7 hostility, G14 poor impulse control; depression
factor was measured by G2 anxiety, G3 guilt feelings and G6 Discussion
depression; cognitive factor was measured by G10 disorientation
and G12 lack of judgement and insight. Two MIMIC models were Smoking Pattern of Schizophrenia Patients
built to assess the effects of smoking status. In model 1, current More than half of male Chinese patients with schizophrenia had
smoking status was hypothesized as the only factor that could smoked in their life time, and 40.0% of them were current smokers
affect symptomatology. In model 2, we further hypothesized that in our study (i.e., combined sample). Although these prevalence
antipsychotic dose could also affect current symptoms of estimates are significantly higher than that of healthy controls in
schizophrenia. Both models could fit the two independent study our samples, they are smaller than the prevalence in studies
samples as well as the combined sample well (CFI.0.9, conducted in other countries. De Leon & Diaz et al. [1] found that
RMSEA,0.08, Table S1). the average prevalence of current smokers among male schizo-
As shown in Table 4, negative dimension of symptomatology phrenia patients was 72% based on 14 studies conducted in 8
was the only factor that was consistently and significantly reduced countries. A recent Chinese study has also shown that 76% male
by smoking (b = 20.125, 20.096, 20.080; p value = 0.047, 0.052, schizophrenia patients were smokers in China [7]. The apparent
0.021 for Sample-A, Sample-B and combined sample, respective- lower smoking prevalence in our study might be attributed to the
ly). Statistical significance remained even after controlling for effective anti-smoking campaigns in Singapore (i.e., Health
antipsychotic usage (b = 20.123, 20.103, 20.082; p val- Promotion Board, Singapore) [29,30]. This is because the smoking
ue = 0.051, 0.035, 0.017 for Sample-A, Sample-B and combined prevalence among the male healthy controls in our study (i.e.,
Table 3. Association of smoking with antipsychotics dose and EPS in regression analysis.
Dependent variables Samples Smoking effect size (b) Nominal p value Adjusted p value1
Antipsychotics dose Sample-A 20.081 0.171 0.182
(CPZ equivalent)
Sample-B 0.094 0.035 0.058
Combined 20.013 0.939 0.740
Tardive dyskinesia2 Sample-A 20.067 0.100 0.668
Drug-induced Parkinsonism2 Sample-A 20.068 0.172 0.624
1
Severity of symptoms, total positive symptoms score, total negative symptom score, and total general symptoms score were adjusted as covariates for association
study of antipsychotic dose, and duration of illness were adjusted as covariates for association study of EPS.
2
AIMS and SAS assessments were only performed on patients in Sample-A. Therefore, tardive dyskinesia and drug-induced Parkinsonism status were not available for
Sample-B.
doi:10.1371/journal.pone.0071343.t003
PLOS ONE | www.plosone.org 4 August 2013 | Volume 8 | Issue 8 | e71343
Smoking and Schizophrenia
Figure 1. MIMIC model in assessing the effects of current smoking status on symptomatology of schizophrenia.
doi:10.1371/journal.pone.0071343.g001
16.8%) is also much lower than that in other countries (i.e., the Association of Smoking with Antipsychotics Usage and
smoking prevalence was 53% among healthy male controls in the EPS
14 studies reviewed by de Leon et al. [1]). In our study, we also It is suggested that smoking could enhance dopamine release
found that the cessation rate among male schizophrenia patients and metabolism of antipsychotics to reduce their EPS, which has
was only 0.54 of that among males in general population, been hypothesized to be one of the reasons for the heavier smoking
suggesting that schizophrenia patients have greater difficulty in pattern among schizophrenia patients [10,31,32]. Observations
quitting smoking despite the anti-smoking campaigns in Singa- that patients with schizophrenia who received higher dose of
pore. This observation is also in agreement with previous findings antipsychotics are more likely to be smokers appear to support this
that schizophrenia patients had significantly lower cessation rate hypothesis since they are exposed to more EPS [12–14]. However,
than general population [6,7,30]. in our samples, the association of smoking with antipsychotic dose
was neither consistent nor significant. While smokers appeared to
be associated with higher dose of antipsychotics in sample-B, the
Table 4. Association of smoking with the factors of PANSS.
variable Latent Factors Sample-A Sample-B Combined
1 1
b P value b P value b1 P value
Model 1: Smoking status Positive 0.024 0.723 0.031 0.595 0.062 0.153
Negative 20.125 0.047 20.096 0.052 20.080 0.021
Excitement 0.068 0.378 0.050 0.235 0.085 0.029
Depression 0.118 0.065 20.029 0.490 0.057 0.096
Cognitive 20.253 0.003 0.127 0.006 0.042 0.254
Model 2: Smoking status Positive 0.038 0.577 0.023 0.692 0.068 0.119
Negative 20.123 0.051 20.103 0.035 20.082 0.017
Excitement 0.077 0.335 0.048 0.243 0.085 0.028
Depression 0.127 0.053 20.036 0.395 0.058 0.097
Cognitive 20.248 0.004 0.126 0.006 0.043 0.251
1
b is the factor loading of smoking status on the five latent factors of symptomatology of schizophrenia in the MIMIC model.
doi:10.1371/journal.pone.0071343.t004
PLOS ONE | www.plosone.org 5 August 2013 | Volume 8 | Issue 8 | e71343
Smoking and Schizophrenia
direction of association was reversed in sample-A, and the underlying dimensions of the symptomatology of schizophrenia
associations were not statistically significant. Moreover, we did feasible. However, this study is also limited by the cross sectional
not find any association between smoking and tardive dyskinesia nature of the sample recruitment. Therefore, although we found a
or drug-induced Parkinsonism, which are due to EPS of significant and consistent association between smoking and
antipsychotics. Therefore, our results do not support the associ- improved negative symptoms of schizophrenia, it is still impossible
ation of smoking with antipsychotic dose or antipsychotic EPS. to prove definitively that the reduction in negative symptoms is
due to smoking. However, based on prior knowledge, especially
Associations of Smoking with Schizophrenia the experimentally controlled study conducted by Smith et al.
Symptomatology [18], we believe it is plausible that smoking improved the negative
Smoking was found to be associated with reduced negative symptoms.
factor of symptoms of schizophrenia, which is measured by N2,
N3, N4, N6, and G7 of PANSS in our dataset. However, no Conclusion
significant effects of smoking were found on the positive factor In conclusion, our results showed that male Chinese patients
measured by P1, P3, P6 and G9. This observation is consistent with schizophrenia had significantly higher smoking and lower
with the findings by Smith et al. [18], who conducted a double cessation rates than general population. We found that smoking is
blinded randomized control trial on male schizophrenia patients consistently and significantly associated with improved negative
and found that smoking could significantly reduce negative symptoms, while no significant association was found between
symptoms but not positive symptoms. Our observation is also in smoking and antipsychotics and their EPS. These observations
agreement with findings from two recent studies in China that support the hypothesis that smoking alleviates negative symptoms
current male smokers had milder negative symptoms than non- in schizophrenia patients, which may account for the heavier
smokers among male schizophrenia patients [7,33]. Similar smoking pattern among schizophrenia patients. Although smoking
observations of improvement in negative symptoms among has a wide range of well-established ill effects on human health,
smokers have also been reported in Caucasian population and these findings do raise the possibility of exploring nicotinic
Egyptian population [19,34]. Taking the evidence together, our pathways for novel treatments of schizophrenia. Indeed, transder-
results support the hypothesis that smoking could improve the mal nicotine treatment on non-smoking schizophrenia patients
negative symptoms of schizophrenia, which could possibly lead to was shown to significantly improve short term cognitive function
the heavier smoking pattern among schizophrenia patients [37]. Recent trials with nicotinic receptor agonists have also shown
[35,36]. The excitement dimension of schizophrenia symptom- promise in alleviating cognitive impairments and negative
atology also seemed to be increased by smoking. However, the symptoms in schizophrenia [38,39].
effect size was not significant in the individual samples.
Supporting Information
Strengths and Limitations
The main strength of this study is that two large independent Table S1 The fittings of the MIMIC models on the two
study samples were employed to explore the smoking pattern and independent and the combined study samples.
the possible mechanisms for the heavier smoking pattern among (DOCX)
male schizophrenia patients was also examined. The comparabil-
ity of the smoking pattern and the consistency of the smoking Author Contributions
effects on negative factors across the two studies suggest that our Conceived and designed the experiments: MS JL. Analyzed the data: JJ.
findings are reliable. In addition, we utilised a validated PANSS Wrote the paper: JJ YMS MS JL. Contributed to performing psychological
factor structure [24], which make the investigation of smoking on assessments: YMS.
References
1. de Leon J, Diaz FJ (2005) A meta-analysis of worldwide studies demonstrates an 11. Miksys S, Tyndale RF (2006) Nicotine induces brain CYP enzymes: relevance to
association between schizophrenia and tobacco smoking behaviors. Schizophr Parkinson’s disease. J Neural Transm Suppl: 177–180.
Res 76: 135–157. 12. Ziedonis DM, Kosten TR, Glazer WM, Frances RJ (1994) Nicotine dependence
2. Olincy A, Young DA, Freedman R (1997) Increased levels of the nicotine and schizophrenia. Hosp Community Psychiatry 45: 204–206.
metabolite cotinine in schizophrenic smokers compared to other smokers. Biol 13. de Leon J, Becona E, Gurpegui M, Gonzalez-Pinto A, Diaz FJ (2002) The
Psychiatry 42: 1–5. association between high nicotine dependence and severe mental illness may be
3. Williams JM, Ziedonis DM, Abanyie F, Steinberg ML, Foulds J, et al. (2005) consistent across countries. J Clin Psychiatry 63: 812–816.
Increased nicotine and cotinine levels in smokers with schizophrenia and 14. de Leon J, Dadvand M, Canuso C, White AO, Stanilla JK, et al. (1995)
schizoaffective disorder is not a metabolic effect. Schizophr Res 79: 323–335. Schizophrenia and smoking: an epidemiological survey in a state hospital.
4. Strand JE, Nyback H (2005) Tobacco use in schizophrenia: a study of cotinine Am J Psychiatry 152: 453–455.
concentrations in the saliva of patients and controls. Eur Psychiatry 20: 50–54. 15. Dalack GW, Healy DJ, Meador-Woodruff JH (1998) Nicotine dependence in
5. Kelly C, McCreadie RG (1999) Smoking habits, current symptoms, and schizophrenia: clinical phenomena and laboratory findings. Am J Psychiatry
premorbid characteristics of schizophrenic patients in Nithsdale, Scotland. 155: 1490–1501.
Am J Psychiatry 156: 1751–1757. 16. Potter D, Summerfelt A, Gold J, Buchanan RW (2006) Review of clinical
6. Gurpegui M, Martinez-Ortega JM, Aguilar MC, Diaz FJ, Quintana HM, et al. correlates of P50 sensory gating abnormalities in patients with schizophrenia.
(2005) Smoking initiation and schizophrenia: a replication study in a Spanish Schizophr Bull 32: 692–700.
sample. Schizophr Res 76: 113–118. 17. Lohr JB, Flynn K (1992) Smoking and schizophrenia. Schizophr Res 8: 93–102.
7. Zhang XY, Liang J, Chen da C, Xiu MH, He J, et al. (2012) Cigarette smoking 18. Smith RC, Infante M, Ali A, Nigam S, Kotsaftis A (2001) Effects of Cigarette
in male patients with chronic schizophrenia in a Chinese population: prevalence Smoking on Psychopathology Scores in Patients With Schizophrenia: An
and relationship to clinical phenotypes. PLoS One 7: e30937. Experimental Study. Subst Abus 22: 175–186.
8. Hennekens CH, Hennekens AR, Hollar D, Casey DE (2005) Schizophrenia and 19. Aguilar MC, Gurpegui M, Diaz FJ, de Leon J (2005) Nicotine dependence and
increased risks of cardiovascular disease. Am Heart J 150: 1115–1121. symptoms in schizophrenia: naturalistic study of complex interactions.
9. Winterer G (2010) Why do patients with schizophrenia smoke? Curr Opin Br J Psychiatry 186: 215–221.
Psychiatry 23: 112–119. 20. Barnes M, Lawford BR, Burton SC, Heslop KR, Noble EP, et al. (2006)
10. Salokangas RK, Vilkman H, Ilonen T, Taiminen T, Bergman J, et al. (2000) Smoking and schizophrenia: is symptom profile related to smoking and which
High levels of dopamine activity in the basal ganglia of cigarette smokers. antipsychotic medication is of benefit in reducing cigarette use?
Am J Psychiatry 157: 632–634. Aust N Z J Psychiatry 40: 575–580.
PLOS ONE | www.plosone.org 6 August 2013 | Volume 8 | Issue 8 | e71343
Smoking and Schizophrenia
21. Patkar AA, Gopalakrishnan R, Lundy A, Leone FT, Certa KM, et al. (2002) 32. Drew AE, Derbez AE, Werling LL (2000) Nicotinic receptor-mediated
Relationship between tobacco smoking and positive and negative symptoms in regulation of dopamine transporter activity in rat prefrontal cortex. Synapse
schizophrenia. J Nerv Ment Dis 190: 604–610. 38: 10–16.
22. Goff DC, Henderson DC, Amico E (1992) Cigarette smoking in schizophrenia: 33. Ma X, Li C, Meng H, Du L, Wang Q, et al. (2010) Premorbid tobacco smoking
relationship to psychopathology and medication side effects. Am J Psychiatry is associated with later age at onset in schizophrenia. Psychiatry Res 178: 461–
149: 1189–1194. 466.
23. Wallwork RS, Fortgang R, Hashimoto R, Weinberger DR, Dickinson D (2012) 34. Fawzi MH, Fawzi MM, Khedr HH (2007) Tobacco smoking in Egyptian
Searching for a consensus five-factor model of the Positive and Negative schizophrenia patients with and without obsessive-compulsive symptoms.
Syndrome Scale for schizophrenia. Schizophr Res 137(1–3): 246–250. Schizophr Res 95: 236–246.
24. Jiang J, Sim K, Lee J (2012) Validated five-factor model of Positive and Negative 35. Taiminen TJ, Salokangas RK, Saarijarvi S, Niemi H, Lehto H, et al. (1998)
Syndrome Scale for schizophrenia in Chinese population. Schizophr Res. Smoking and cognitive deficits in schizophrenia: a pilot study. Addict Behav 23:
Available: http://dx.doi.org/10.1016/j.schres.2012.10.019. In press. 263–266.
25. Woods SW (2003) Chlorpromazine equivalent doses for the newer atypical 36. Drew AE, Werling LL (2003) Nicotinic receptor-mediated regulation of the
antipsychotics. J Clin Psychiatry 64: 663–667.
dopamine transporter in rat prefrontocortical slices following chronic in vivo
26. Simpson GM, Angus JW (1970) A rating scale for extrapyramidal side effects.
administration of nicotine. Schizophr Res 65: 47–55.
Acta Psychiatr Scand Suppl 212: 11–19.
37. Barr RS, Culhane MA, Jubelt LE, Mufti RS, Dyer MA, et al. (2008) The effects
27. Munetz MR, Benjamin S (1988) How to examine patients using the Abnormal
of transdermal nicotine on cognition in nonsmokers with schizophrenia and
Involuntary Movement Scale. Hosp Community Psychiatry 39: 1172–1177.
28. Schooler NR, Kane JM (1982) Research diagnoses for tardive dyskinesia. Arch nonpsychiatric controls. Neuropsychopharmacology 33: 480–490.
Gen Psychiatry 39: 486–487. 38. Shim JC, Jung DU, Jung SS, Seo YS, Cho DM, et al. (2012) Adjunctive
29. Health Promotion Board website. Available: http://wwwhpbgovsg/smokefree/. varenicline treatment with antipsychotic medications for cognitive impairments
Accessed Jun 2012. in people with schizophrenia: a randomized double-blind placebo-controlled
30. de Leon J, Diaz FJ, Rogers T, Browne D, Dinsmore L (2002) Initiation of daily trial. Neuropsychopharmacology 37: 660–668.
smoking and nicotine dependence in schizophrenia and mood disorders. 39. Lieberman JA, Dunbar G, Segreti AC, Girgis RR, Seoane F, et al. (2013) A
Schizophr Res 56: 47–54. randomized exploratory trial of an alpha-7 nicotinic receptor agonist (TC-5619)
31. Kirch DG, Gerhardt GA, Shelton RC, Freedman R, Wyatt RJ (1987) Effect of for cognitive enhancement in schizophrenia. Neuropsychopharmacology 38:
chronic nicotine administration on monoamine and monoamine metabolite 968–975.
concentrations in rat brain. Clin Neuropharmacol 10: 376–383.
PLOS ONE | www.plosone.org 7 August 2013 | Volume 8 | Issue 8 | e71343
Reproduced with permission of the copyright owner. Further reproduction prohibited without
permission.
You might also like
- Behavior Intervention PlanDocument6 pagesBehavior Intervention Planapi-308475283No ratings yet
- Load Summary for Premise Under 100kVADocument2 pagesLoad Summary for Premise Under 100kVAMuhammad Zulhelmi ZawawiNo ratings yet
- Jurnal 1.4 yDocument20 pagesJurnal 1.4 yAmbarsari HamidahNo ratings yet
- Medicine: Association Between Smoking and Serum Uric Acid in Korean PopulationDocument7 pagesMedicine: Association Between Smoking and Serum Uric Acid in Korean PopulationAngely NovianaNo ratings yet
- Recreation Therapy Reduces Smoking and Symptoms in SchizophreniaDocument5 pagesRecreation Therapy Reduces Smoking and Symptoms in SchizophreniaTeodorNo ratings yet
- Predictors of Treatment Response in Substance Use DisordersDocument29 pagesPredictors of Treatment Response in Substance Use Disordersalexandra mariaNo ratings yet
- The Long-Term Effects of Antipsychotic Medication on 精神病病程Document9 pagesThe Long-Term Effects of Antipsychotic Medication on 精神病病程wen zhangNo ratings yet
- RelapseDocument10 pagesRelapseEmil Eduardo Julio RamosNo ratings yet
- Intervention For Smoking ReductionDocument15 pagesIntervention For Smoking Reductionben mwanziaNo ratings yet
- Jurnal Bing 3Document11 pagesJurnal Bing 3Abangnya Dea AmandaNo ratings yet
- Appi Ajp 2015 15010126Document9 pagesAppi Ajp 2015 15010126Novry DodyNo ratings yet
- Accepted_manuscriptDocument40 pagesAccepted_manuscriptsueffximenaNo ratings yet
- Combined Effects of Smoking and Systolic Blood Pressure On Risk of Coronary Heart Disease: A Cohort Study in Chinese WomenDocument7 pagesCombined Effects of Smoking and Systolic Blood Pressure On Risk of Coronary Heart Disease: A Cohort Study in Chinese Womenb10879832No ratings yet
- N Acetylcysteine For Therapy Resistant Tobacco Use Disorder A Pilot StudyDocument9 pagesN Acetylcysteine For Therapy Resistant Tobacco Use Disorder A Pilot Studytami syhabNo ratings yet
- Attention-Deficit/Hyperactivity Disorder and Nicotine Dependence in AdultsDocument6 pagesAttention-Deficit/Hyperactivity Disorder and Nicotine Dependence in AdultsFadliah FahriNo ratings yet
- RrlsDocument9 pagesRrlsJohnallenSyNo ratings yet
- A Systematic Review and Network Meta-Analysis To AssessDocument13 pagesA Systematic Review and Network Meta-Analysis To AssessastrogliaNo ratings yet
- How To Optimize The Treatment of Early Stage Parkinson 'S DiseaseDocument7 pagesHow To Optimize The Treatment of Early Stage Parkinson 'S DiseaseElisabethNo ratings yet
- Weed or WheelDocument15 pagesWeed or WheelVi KekaNo ratings yet
- Effect of Smoking and Smoking Cessation On Bone Mass, Bone Remodeling, Vitamin D, PTH and Sex HormonesDocument8 pagesEffect of Smoking and Smoking Cessation On Bone Mass, Bone Remodeling, Vitamin D, PTH and Sex HormonesPutri Kharisma DewiNo ratings yet
- Association of Smoking and Generalized ManifestatiDocument7 pagesAssociation of Smoking and Generalized ManifestatiA CASA CAIUNo ratings yet
- Evaluation of Smoking Cessation Success in AdultsDocument8 pagesEvaluation of Smoking Cessation Success in AdultsSISNo ratings yet
- Chen2017 - Similarities and Differences in PsychologyDocument11 pagesChen2017 - Similarities and Differences in Psychologyhilda.marselaNo ratings yet
- Factors Correlated With Smoking Cessation Success in Older Adults: A Retrospective Cohort Study in TaiwanDocument9 pagesFactors Correlated With Smoking Cessation Success in Older Adults: A Retrospective Cohort Study in TaiwanKhaziatun NurNo ratings yet
- Cigarette Smoking and Heart FailureDocument9 pagesCigarette Smoking and Heart FailureArunDevaNo ratings yet
- Relationship Between Smoking and Parkinson's DiseaseDocument6 pagesRelationship Between Smoking and Parkinson's DiseaseNovita Anggun Permata SariNo ratings yet
- Chapter 3Document3 pagesChapter 3Cayanong Joel Jr I.No ratings yet
- Evaluation of The Impact of Cigarette Smoking OnDocument6 pagesEvaluation of The Impact of Cigarette Smoking OnBerenice SánchezNo ratings yet
- Anxiety and Agitation in Smoking Schizophrenic Patient1Document1 pageAnxiety and Agitation in Smoking Schizophrenic Patient1sushena50No ratings yet
- Severity of Nicotine Withdrawal Symptoms After Smoking CessationDocument6 pagesSeverity of Nicotine Withdrawal Symptoms After Smoking CessationfggNo ratings yet
- Shantal Mang InasalDocument7 pagesShantal Mang InasalShantal EsperaNo ratings yet
- Elevated Striatal Dopamine Function Linked To Prodromal Signs of SchizophreniaDocument8 pagesElevated Striatal Dopamine Function Linked To Prodromal Signs of SchizophreniaDalia CisnerosNo ratings yet
- Psoriasis and Smoking: A Systematic Review and Meta-AnalysisDocument11 pagesPsoriasis and Smoking: A Systematic Review and Meta-AnalysisArum DiannitasariNo ratings yet
- AJGP 10 2019 Focus Manger Lifestyle Interventions Mental Health WEBDocument4 pagesAJGP 10 2019 Focus Manger Lifestyle Interventions Mental Health WEBisitugasnandasekarbuanaNo ratings yet
- PERCEIVED EFFECT OF PHYSICAL EXERCISE ON SMOKING STATUS AMONG SAUDI POPULATION IN THE EASTERN PROVINCE OF KSA: A CROSS-SECTIONAL STUDYDocument9 pagesPERCEIVED EFFECT OF PHYSICAL EXERCISE ON SMOKING STATUS AMONG SAUDI POPULATION IN THE EASTERN PROVINCE OF KSA: A CROSS-SECTIONAL STUDYIJAR JOURNALNo ratings yet
- The Effect of Tobacco Smoking On Septoplasty OutcomesDocument11 pagesThe Effect of Tobacco Smoking On Septoplasty OutcomesMatra Adi PrawiraNo ratings yet
- Cognitive Status of Young and Older Ciga PDFDocument9 pagesCognitive Status of Young and Older Ciga PDFNurmawati AtNo ratings yet
- The Most Effective Smoking Addiction TreatmentDocument15 pagesThe Most Effective Smoking Addiction TreatmentAzreZephyrNo ratings yet
- Psychological Effect F NicotineDocument6 pagesPsychological Effect F NicotinehelfiNo ratings yet
- Title: Prevalence and Factors Associated With Extrapyramidal Side Effects Among Inpatients at A Tertiary Care Setting: A Cross-Sectional StudyDocument7 pagesTitle: Prevalence and Factors Associated With Extrapyramidal Side Effects Among Inpatients at A Tertiary Care Setting: A Cross-Sectional StudyAbdul Mannan ChatthaNo ratings yet
- Smoking Linked to Higher Depression Risk in 26-Year StudyDocument7 pagesSmoking Linked to Higher Depression Risk in 26-Year StudyLumeiko LukaNo ratings yet
- Rajiv P. Sharma Et Al - CSF Neurotensin Concentrations and Antipsychotic Treatment in Schizophrenia and Schizoaffective DisorderDocument3 pagesRajiv P. Sharma Et Al - CSF Neurotensin Concentrations and Antipsychotic Treatment in Schizophrenia and Schizoaffective DisorderLonkesNo ratings yet
- Modelling Continuous Abstinence Rates Over Time FromDocument11 pagesModelling Continuous Abstinence Rates Over Time FromConstantin PopescuNo ratings yet
- 2018 Article 1999 PDFDocument8 pages2018 Article 1999 PDFyusma haranisNo ratings yet
- Atypical antipsychotics for schizophrenia and substance abuseDocument14 pagesAtypical antipsychotics for schizophrenia and substance abusecupin 69PKNo ratings yet
- Factors Relating To Failure To Quit Smoking A Prospective Cohort StudyDocument7 pagesFactors Relating To Failure To Quit Smoking A Prospective Cohort StudySilas SilvaNo ratings yet
- Drugs and Treatment: Pharmacological InterventionDocument6 pagesDrugs and Treatment: Pharmacological InterventionJairah CandaoNo ratings yet
- Review Article: Prolactin and Psychopathology in Schizophrenia: A Literature Review and ReappraisalDocument13 pagesReview Article: Prolactin and Psychopathology in Schizophrenia: A Literature Review and ReappraisalJoelEspinolaLozanoNo ratings yet
- Uso de Sustancias y EsquizofreniaDocument10 pagesUso de Sustancias y Esquizofreniaracm89No ratings yet
- Psychopharmacological Treatment of Obsessive-Compulsive Disorder (OCD)Document27 pagesPsychopharmacological Treatment of Obsessive-Compulsive Disorder (OCD)godolfintorentNo ratings yet
- Pembelajaran Penyakit Terkait Perilaku Merokok Dan Edukasi Untuk Berhenti Merokok Di Pendidikan Dokter Fakultas Kedokteran UgmDocument16 pagesPembelajaran Penyakit Terkait Perilaku Merokok Dan Edukasi Untuk Berhenti Merokok Di Pendidikan Dokter Fakultas Kedokteran UgmkiranaNo ratings yet
- Petit (2015) ERP Study - Processing of Alcohol Cues Predicts AbstinenceDocument11 pagesPetit (2015) ERP Study - Processing of Alcohol Cues Predicts AbstinenceJulieht RodriguezNo ratings yet
- Feeling GreatDocument243 pagesFeeling GreatSunny LamNo ratings yet
- HEALTH IMPROVEMENT AFTER SMOKING CESSATIONDocument5 pagesHEALTH IMPROVEMENT AFTER SMOKING CESSATIONAmin Mohamed Amin DemerdashNo ratings yet
- A Preliminary Trial: Double-Blind Comparison of Nefazodone, Bupropion-SR, and Placebo in The Treatment of Cannabis DependenceDocument12 pagesA Preliminary Trial: Double-Blind Comparison of Nefazodone, Bupropion-SR, and Placebo in The Treatment of Cannabis DependenceJai KunvarNo ratings yet
- Final PaperDocument5 pagesFinal Paperapi-260309514No ratings yet
- Kazkas Su Alcohol PDFDocument5 pagesKazkas Su Alcohol PDFMartis JonasNo ratings yet
- Synthesispaperebpsummative AnjouligerezDocument9 pagesSynthesispaperebpsummative Anjouligerezapi-325112936No ratings yet
- A Systematic Review of Tobacco Use in First-Episode PsychosisDocument11 pagesA Systematic Review of Tobacco Use in First-Episode PsychosisVivi DeviyanaNo ratings yet
- 10 1016@j Ajp 2019 05 002Document7 pages10 1016@j Ajp 2019 05 002Dwi Rachma MeilinaNo ratings yet
- Strategies For Breaking Free From Smoking, Vaping And Smokeless Tobacco - Based On The Teachings Of Dr. Andrew Huberman: Kicking The HabitFrom EverandStrategies For Breaking Free From Smoking, Vaping And Smokeless Tobacco - Based On The Teachings Of Dr. Andrew Huberman: Kicking The HabitNo ratings yet
- M96SC05 Oleo StrutDocument6 pagesM96SC05 Oleo Strutchaumont12345No ratings yet
- Mitsubishi v500 VFD IB NA 0600065-F FR-V500-NA Instruction Manual-DetailedDocument221 pagesMitsubishi v500 VFD IB NA 0600065-F FR-V500-NA Instruction Manual-DetailedMROstop.comNo ratings yet
- Experienced Waiter ResumeDocument3 pagesExperienced Waiter ResumeArchford ManyereNo ratings yet
- Strategies and Tactics for Collecting on Overdue AccountsDocument9 pagesStrategies and Tactics for Collecting on Overdue AccountsAkii WingNo ratings yet
- State-of-the-Art Reactor Consequence Analyses (SOARCA) ReportDocument200 pagesState-of-the-Art Reactor Consequence Analyses (SOARCA) ReportKingba OlayemiNo ratings yet
- Employment Law Lubs 3915Document4 pagesEmployment Law Lubs 3915ogunsatoNo ratings yet
- Curtain WallDocument11 pagesCurtain WallZameer AhmedNo ratings yet
- Excel - All Workout Routines Exercises Reps Sets EtcDocument10 pagesExcel - All Workout Routines Exercises Reps Sets EtcJanus Blacklight100% (1)
- Dimensions-Mm (Inch) : Valve Regulated Lead Acid Battery (VRLA)Document2 pagesDimensions-Mm (Inch) : Valve Regulated Lead Acid Battery (VRLA)orunmila123No ratings yet
- Brian Cody Mcgonegal ResumeDocument2 pagesBrian Cody Mcgonegal Resumeapi-348833348No ratings yet
- A Comparative Study Between Various Models of Eco-Brick and Hollow BlocksDocument9 pagesA Comparative Study Between Various Models of Eco-Brick and Hollow BlocksMykaila Ysa ValdezNo ratings yet
- Barangay Peace and Order and Public Safety Plan Bpops Annex ADocument3 pagesBarangay Peace and Order and Public Safety Plan Bpops Annex AImee CorreaNo ratings yet
- Electric Vehicle BatteryDocument15 pagesElectric Vehicle BatteryTotal Acess100% (1)
- History of Medicine - Alexander WilderDocument555 pagesHistory of Medicine - Alexander WilderMark R. JaquaNo ratings yet
- Personal and Group Trainer Juan Carlos GonzalezDocument2 pagesPersonal and Group Trainer Juan Carlos GonzalezDidier G PeñuelaNo ratings yet
- Atlas Tool Specs SummaryDocument3 pagesAtlas Tool Specs SummaryWaleed Barakat MariaNo ratings yet
- Chap-20 - Locomotion & MovementDocument52 pagesChap-20 - Locomotion & MovementMittal SavaniNo ratings yet
- Persuasive Speech On Behalf of Inspector GooleDocument4 pagesPersuasive Speech On Behalf of Inspector GooleSahanaNo ratings yet
- MIDWIFE1115ra Tugue e PDFDocument9 pagesMIDWIFE1115ra Tugue e PDFPhilBoardResultsNo ratings yet
- Drug Study Pre OpDocument6 pagesDrug Study Pre OpgiaNo ratings yet
- Project Report On Biodegradable Plates, Glasses, Food Container, Spoon Etc.Document6 pagesProject Report On Biodegradable Plates, Glasses, Food Container, Spoon Etc.EIRI Board of Consultants and Publishers0% (1)
- Port Works Design Manual Part 2 PDFDocument124 pagesPort Works Design Manual Part 2 PDFhessian123No ratings yet
- Book 1Document100 pagesBook 1Devasyruc100% (1)
- Jeremy Tan Resume and CVDocument3 pagesJeremy Tan Resume and CVapi-359540985No ratings yet
- 23soft Starter HandbookDocument36 pages23soft Starter HandbookCarlos_Duque1958No ratings yet
- Ra 9520 Chapter VDocument8 pagesRa 9520 Chapter VLorribelle OcenarNo ratings yet
- QS - HM - Freight Express Indonesia - Cipta HarapanDocument4 pagesQS - HM - Freight Express Indonesia - Cipta HarapanAKHMAD SHOQI ALBINo ratings yet
- Arthropods: A Guide to the Diverse PhylumDocument10 pagesArthropods: A Guide to the Diverse Phylumpkkalai112No ratings yet