Professional Documents
Culture Documents
Cardaic Resynchronization
Uploaded by
Samatha BiotechOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Cardaic Resynchronization
Uploaded by
Samatha BiotechCopyright:
Available Formats
The new england journal of medicine
original article
The Effect of Cardiac Resynchronization
on Morbidity and Mortality in Heart Failure
John G.F. Cleland, M.D., Jean-Claude Daubert, M.D.,
Erland Erdmann, M.D., Nick Freemantle, Ph.D., Daniel Gras, M.D.,
Lukas Kappenberger, M.D., and Luigi Tavazzi, M.D.,
for the Cardiac Resynchronization — Heart Failure (CARE-HF) Study Investigators*
abstract
background
Cardiac resynchronization reduces symptoms and improves left ventricular function in From the Department of Cardiology, Castle
many patients with heart failure due to left ventricular systolic dysfunction and cardiac Hill Hospital, Kingston-upon-Hull, United
Kingdom (J.G.F.C.); the Department of
dyssynchrony. We evaluated its effects on morbidity and mortality. Cardiology, Hôpital Pontchaillou, Rennes,
France (J.-C.D.); Klinik III für Innere Medi-
methods zin der Universität zu Köln, Cologne, Ger-
many (E.E.); the University of Birmingham,
Patients with New York Heart Association class III or IV heart failure due to left ventricu- Edgbaston, United Kingdom (N.F.); Nou-
lar systolic dysfunction and cardiac dyssynchrony who were receiving standard pharma- velles Cliniques Nantaises, Nantes, France
cologic therapy were randomly assigned to receive medical therapy alone or with cardiac (D.G.); the Division of Cardiology, Centre
Hospitalier Universitaire Vaudois, Lau-
resynchronization. The primary end point was the time to death from any cause or an sanne, Switzerland (L.K.); and Istituto di
unplanned hospitalization for a major cardiovascular event. The principal secondary end Ricovero e Cura a Carattere Scientifico,
point was death from any cause. Policlinico San Matteo, Pavia, Italy (L.T.).
Address reprint requests to Dr. Cleland at
the Department of Cardiology, Castle Hill
results Hospital, University of Hull, Kingston-upon-
A total of 813 patients were enrolled and followed for a mean of 29.4 months. The pri- Hull, United Kingdom, or at j.g.cleland@
hull.ac.uk.
mary end point was reached by 159 patients in the cardiac-resynchronization group, as
compared with 224 patients in the medical-therapy group (39 percent vs. 55 percent; *The CARE-HF Study investigators are
hazard ratio, 0.63; 95 percent confidence interval, 0.51 to 0.77; P<0.001). There were listed in the Appendix.
82 deaths in the cardiac-resynchronization group, as compared with 120 in the medi- This article was published at www.nejm.
cal-therapy group (20 percent vs. 30 percent; hazard ratio 0.64; 95 percent confidence org on March 7, 2004.
interval, 0.48 to 0.85; P<0.002). As compared with medical therapy, cardiac resynchro-
N Engl J Med 2005;352:1539-49.
nization reduced the interventricular mechanical delay, the end-systolic volume index, Copyright © 2005 Massachusetts Medical Society.
and the area of the mitral regurgitant jet; increased the left ventricular ejection fraction;
and improved symptoms and the quality of life (P<0.01 for all comparisons).
conclusions
In patients with heart failure and cardiac dyssynchrony, cardiac resynchronization im-
proves symptoms and the quality of life and reduces complications and the risk of death.
These benefits are in addition to those afforded by standard pharmacologic therapy.
The implantation of a cardiac-resynchronization device should routinely be considered
in such patients.
n engl j med 352;15 www.nejm.org april 14, 2005 1539
The New England Journal of Medicine
Downloaded from www.nejm.org on September 23, 2010. For personal use only. No other uses without permission.
Copyright © 2005 Massachusetts Medical Society. All rights reserved.
The new england journal of medicine
organization (Quintiles, Dublin) that maintained
d espite improvements in pharma-
cologic treatment, many patients with
heart failure have severe and persistent
symptoms, and their prognosis remains poor.1,2
Such patients commonly have regions of delayed
the database, issued data-clarification forms, and
assisted by Medtronic employees, verified source
documents. The sponsor had no access to the data-
base and did not participate in the analysis of the re-
myocardial activation and contraction, leading to sults or the writing of the article. All analyses were
cardiac dyssynchrony. In a series of trials lasting up performed by one of the authors with the assistance
to six months, cardiac resynchronization decreased of an independent statistician. Three Medtronic rep-
symptoms and improved exercise capacity, the qual- resentatives commented on the manuscript before
ity of life, and ventricular function.3-7 The Compar- its submission. The study was approved by the local
ison of Medical Therapy, Pacing, and Defibrillation ethics committee of each participating institution
in Heart Failure (COMPANION) trial showed that and by appropriate national ethics committees. All
cardiac-resynchronization therapy alone or com- patients provided written informed consent.
bined with an implantable defibrillator reduced the
composite end point of death from any cause or hos- patients
pitalization during a mean follow-up of 16 months8; Eligible patients were at least 18 years of age, had
however, the decrease in the risk of death was not had heart failure for at least six weeks, and were in
significant with cardiac resynchronization therapy New York Heart Association (NYHA) class III or IV
alone (P=0.06). Meta-analyses have left lingering despite receipt of standard pharmacologic therapy,
uncertainty about the effects of cardiac resynchro- with a left ventricular ejection fraction of no more
nization on the risk of complications and death.9,10 than 35 percent, a left ventricular end-diastolic di-
We analyzed the effects of cardiac resynchroniza- mension of at least 30 mm (indexed to height), and
tion on the risk of complications and death among a QRS interval of at least 120 msec on the electro-
patients who were receiving standard medical ther- cardiogram. Patients with a QRS interval of 120 to
apy for moderate or severe heart failure and cardiac 149 msec were required to meet two of three addi-
dyssynchrony. tional criteria for dyssynchrony: an aortic preejec-
tion delay of more than 140 msec, an interventric-
methods ular mechanical delay of more than 40 msec, or
delayed activation of the posterolateral left ventric-
The Cardiac Resynchronization — Heart Failure ular wall.11-13
(CARE-HF) trial was a multicenter, international, Patients who had had a major cardiovascular
randomized trial comparing the effect on the risk event in the previous six weeks, those who had con-
of complications and death of standard pharmaco- ventional indications for a pacemaker or an im-
logic therapy alone with that of the combination of plantable defibrillator, and those with heart fail-
standard therapy and cardiac resynchronization ure requiring continuous intravenous therapy were
(without a defibrillator) in patients with left ventric- excluded. Also excluded were patients with atrial ar-
ular systolic dysfunction, cardiac dyssynchrony, and rhythmias, since such patients cannot benefit from
symptomatic heart failure.11-13 Patients were en- the atrial component of resynchronization.11-13
rolled at 82 European centers; enrollment began in
January 2001 and ended in March 2003. The study study procedures
was not blinded. The members of the end-points Randomization was stratified according to the
committee (see the Appendix), however, were not NYHA class and was carried out by Quintiles with
aware of patients’ treatment assignments. Patients the use of a minimization procedure. Patients who
in the control group were not scheduled to receive a were randomly assigned to undergo cardiac resyn-
device, both for ethical reasons and so that the trial chronization received a Medtronic InSync or InSync
could assess the entire effect of cardiac resynchro- III device, which provided atrial-based, biventricular
nization, including complications associated with stimulation with the use of standard right ventricu-
implantation of the device.11-13 lar and Attain (Medtronic) left ventricular leads. In-
The steering committee (see the Appendix) de- vestigators were asked to position the left ventricular
signed the trial. The Medtronic Corporation funded lead to pace the lateral or posterolateral left ventric-
the trial and provided a study manager to supervise ular wall transvenously and provide radiographic
its conduct. Data were sent by investigators to core documentation. Backup atrial pacing was set at 60
laboratories or to an independent clinical-research beats per minute. The interventricular delay was set
1540 n engl j med 352;15 www.nejm.org april 14 , 2005
The New England Journal of Medicine
Downloaded from www.nejm.org on September 23, 2010. For personal use only. No other uses without permission.
Copyright © 2005 Massachusetts Medical Society. All rights reserved.
effect of cardiac resynchronization on heart failure
to zero, and the atrioventricular delay was echocar- All hospitalizations were adjudicated in a blind-
diographically optimized.11 Patients were moni- ed fashion by the end-points committee. The first
tored overnight after receiving the device. If the hospitalization with documented worsening heart
initial procedure failed, repeated attempts at im- failure, myocardial infarction, unstable angina, ar-
plantation were encouraged, and expert assistance rhythmia, stroke, or other major cardiovascular
was provided. event (e.g., pulmonary embolism or ruptured aortic
aneurysm) or hospitalization owing to or prolonged
follow-up by a serious procedure-related event (e.g., infection,
Patients were evaluated at 1, 3, 6, 9, 12, and 18 pericardial hemorrhage, or tension pneumothorax)
months and every six months thereafter, and stan- was counted in the primary end point. Hospitaliza-
dard medications were adjusted as appropriate at tion with worsening heart failure was defined by the
these visits. Investigators were asked to report all occurrence of increasing symptoms and the need
adverse events, which were classified in a blinded for treatment with intravenous diuretics or a sub-
fashion by an end-points committee or, if they were stantial increase in oral diuretics (an increase of at
procedure-related or device-related, by an indepen- least 40 mg of furosemide per day, 1 mg of bumet-
dent expert who was not blinded to the study-group anide per day, or 10 mg of torsemide per day) or the
assignments (see the Appendix). initiation of a combination of a thiazide and a loop
The protocol required follow-up to continue for diuretic.
18 months after the last patient had been enrolled, Admissions for symptoms without a document-
unless the data and safety monitoring board stopped ed major cardiac event were not included in the
the study earlier or fewer than 300 patients had primary end point, nor were readmissions for lead
reached a primary end point at that time, in which displacement, unless it precipitated a cardiac emer-
case the trial could be extended. On March 6, 2004, gency, or admissions for initial implantation of the
the board recommended extending the study until device, since this was part of the protocol. To pre-
May 2005 without disclosing the reasons. However, vent bias in favor of cardiac resynchronization, hos-
since the prespecified criteria had been met, the pitalizations within 10 days after randomization in
steering committee decided to conclude the study either group did not count toward the primary end
as planned on September 30, 2004,11 and imple- point.
mented, without knowledge of the results, an exten- The principal secondary outcome was death
sion phase with death from any cause as the (nom- from any cause, which was classified according to
inal) primary outcome. On February 24, 2005, after mode and cause.11 Other secondary end points in-
this article had been submitted for publication, the cluded a composite of death from any cause and un-
data and safety monitoring board indicated that the planned hospitalization with heart failure and, at
main reasons for its recommendation were interim 90 days, the NYHA class and the quality of life as as-
analyses showing a trend toward more cardiovas- sessed by the patient with the use of the Minnesota
cular events in the first 10 days after randomization Living with Heart Failure questionnaire (scores can
among patients assigned to cardiac resynchroniza- range from 0 to 105, with higher scores reflecting a
tion than among those assigned to medical therapy poorer quality of life)14,15 and the European Quality
alone and a trend toward a favorable effect of re- of Life–5 Dimensions (EuroQoL EQ-5D) instrument
synchronization on long-term mortality that they (scores can range from –0.594 to 1.000, with lower
thought might fail to reach significance by the time numerical values indicating a poorer quality of life;
of the planned closure date. negative scores are associated with a quality of life
that is considered worse than death).16 Death was
end points given a notional NYHA class of V for the analysis of
The primary end point was a composite of death changes in functional class. Several echocardio-
from any cause or an unplanned hospitalization for graphic and biochemical variables were assessed in
a major cardiovascular event; only the first event in core laboratories, including the severity of cardiac
each patient was included in this analysis. Data on dyssynchrony, ventricular function, mitral regurgi-
patients who underwent elective heart transplanta- tation, and N-terminal pro–brain natriuretic peptide
tion were censored seven days after the procedure. (Elecsys, Roche Diagnostics), at baseline and at the
Emergency heart transplantation was counted as a 3-month and 18-month follow-up visits. Differenc-
death. es from baseline in heart rate and blood pressure
n engl j med 352;15 www.nejm.org april 14, 2005 1541
The New England Journal of Medicine
Downloaded from www.nejm.org on September 23, 2010. For personal use only. No other uses without permission.
Copyright © 2005 Massachusetts Medical Society. All rights reserved.
The new england journal of medicine
were also compared in the two groups at follow- Implantation of a device was attempted in 404
up.11 No data other than NYHA class were imputed of the 409 patients assigned to undergo cardiac re-
for patients who died. synchronization. One patient died before undergo-
ing the procedure, and in four instances, the patient
statistical analysis or investigator decided not to proceed. A cardiac-
All prespecified analyses were conducted according resynchronization device was implanted and activat-
to the intention-to-treat principle. P values other ed in 390 patients (95 percent), in 349 on the first
than for the primary end point are nominal. The attempt; the device was implanted a median of four
study had a statistical power17 of 80 percent to iden- days (interquartile range, two to seven) after ran-
tify a 14 percent relative reduction or a 5.7 percent- domization. The median duration of hospitalization
age point reduction in the rate of events, given a con- for implantation was five days (interquartile range,
ventional one-sided a value of 0.025 and a predicted two to eight). Before the device could be activated,
number of 300 events.11 The time to an event was six patients had an unplanned hospitalization for
calculated according to the Kaplan–Meier method cardiovascular reasons that qualified as a primary
and analyzed with the use of Cox proportional-haz- end point. Eight patients assigned to undergo car-
ards models, which included baseline NYHA class diac resynchronization had a device with an addi-
as a covariate.18 Continuous data were analyzed tional defibrillator function implanted during the
with the use of mixed models, which included base- study.
line variables as patient-level covariates and study In the medical-therapy group, implantation of
centers as random effects.19 Dichotomous out- a cardiac-resynchronization device alone was at-
comes were analyzed with the use of nonlinear tempted in 43 patients and implantation of a resyn-
mixed models, which included the NYHA class as a chronization device with a defibrillator was attempt-
patient-level covariate and study centers as random ed in 23 patients (both approaches were attempted
effects. The rates of adverse events were compared in 1 patient). The device was activated in 50 patients.
between groups by means of Fisher’s exact test. In 10 instances, a device was successfully implanted
Analyses were conducted with the use of SAS soft- but programmed to provide only standard pacemak-
ware (version 9.12, SAS Institute). The data and er or defibrillator functions to avoid crossover. In
safety monitoring board conducted two planned in- five patients, the attempt at implantation was un-
terim analyses with the use of nonsymmetric stop- successful. The device was activated in 19 patients
ping rules.20 (5 percent) before they reached the primary end
point. Eight of these patients subsequently reached
results a primary end point, six of whom died. Of 31 pa-
tients in whom the device was activated after they
A total of 404 patients were assigned to receive med- had reached the primary end point, 7 subsequent-
ical therapy alone and 409 to receive medical therapy ly died.
plus cardiac resynchronization. The mean duration
of follow-up was 29.4 months (range, 18.0 to 44.7). primary end point
By the end of the study, the survival status of all pa- By the end of the study, the primary end point had
tients was known, 383 patients had reached the pri- been reached in 159 patients in the cardiac-resyn-
mary end point, and 202 patients had died. chronization group, as compared with 224 patients
who received medical therapy alone (39 percent vs.
study population 55 percent; hazard ratio, 0.63; 95 percent confi-
Baseline characteristics were similar in the two dence interval, 0.51 to 0.77; P<0.001) (Fig. 1A and
groups (Table 1). Patients had well-treated moder- Table 2). There were 384 unplanned hospitaliza-
ate or severe heart failure and major left ventricular tions for a major cardiovascular event in the control
systolic dysfunction. Only 43 percent were taking group and 222 in the cardiac-resynchronization
high doses of diuretics (defined as at least 80 mg of group. Death was the primary event in 74 patients,
furosemide, at least 2 mg of bumetanide, or at least and hospitalization in 309. Prespecified subgroup
20 mg of torsemide). Beta-blockers were taken at analyses for the primary end point revealed no het-
some time during the study by 85 percent of the pa- erogeneity in the effect of cardiac resynchronization
tients in the medical-therapy group and 84 percent (Fig. 2). Twelve patients in the cardiac-resynchro-
of those in the cardiac-resynchronization group. nization group and 10 in the medical-therapy group
1542 n engl j med 352;15 www.nejm.org april 14 , 2005
The New England Journal of Medicine
Downloaded from www.nejm.org on September 23, 2010. For personal use only. No other uses without permission.
Copyright © 2005 Massachusetts Medical Society. All rights reserved.
effect of cardiac resynchronization on heart failure
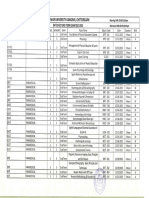
Table 1. Baseline Characteristics of the Patients.*
Medical Therapy Alone Medical Therapy plus Cardiac
Characteristic (N=404) Resynchronization (N=409)
Age (yr)
Median 66 67
Interquartile range 59–72 60–73
Male sex (%) 293 (73) 304 (74)
NYHA class IV (%) 27 (7) 23 (6)
Dilated cardiomyopathy (%) 193 (48) 177 (43)
Ischemic heart disease (%) 144 (36) 165 (40)
Heart disease of other causes (%) 67 (17) 67 (16)
Heart rate (beats/min)
Median 70 69
Interquartile range 61–78 60–78
Systolic blood pressure (mm Hg)
Median 110 110
Interquartile range 100–125 100–125
Diastolic blood pressure (mm Hg)
Median 70 70
Interquartile range 60–80 60–79
N-terminal pro–brain natriuretic peptide (pg/ml)†
Median 1806 1920
Interquartile range 719–3949 744–4288
Left ventricular ejection fraction (%)
Median 25 25
Interquartile range 22–29 21–29
Left ventricular end-systolic volume index (ml/m2)
Median 117 121
Interquartile range 94–147 92–151
QRS duration (msec)
Median 160 160
Interquartile range 152–180 152–180
Interventricular mechanical delay (msec)
Median 50 49
Interquartile range 30–66 32–67
Mitral-regurgitation area‡
Median 0.23 0.21
Interquartile range 0.11–0.34 0.12–0.33
Glomerular filtration rate (ml/min/1.73 m2)
Median 61 60
Interquartile range 46–73 46–73
Use of an ACE inhibitor or angiotensin-receptor blocker (%) 383 (95) 387 (95)
Use of a beta-blocker (%) 298 (74) 288 (70)
Use of spironolactone (%) 238 (59) 219 (54)
Use of a high-dose loop diuretic (%)§ 177 (44) 175 (43)
Use of digoxin (%) 181 (45) 165 (40)
* NYHA denotes New York Heart Association, and ACE angiotensin converting enzyme.
† To convert values for N-terminal pro–brain natriuretic peptide to picomoles per liter, divide by 8.457.
‡ The area was calculated as the area of the color-flow Doppler regurgitant jet divided by the area of the left atrium in sys-
tole, both in square centimeters.
§ A high-dose loop diuretic consisted of furosemide at a dose of 80 mg or more, bumetanide at a dose of 2 mg or more,
or torsemide at a dose of 20 mg or more.
n engl j med 352;15 www.nejm.org april 14, 2005 1543
The New England Journal of Medicine
Downloaded from www.nejm.org on September 23, 2010. For personal use only. No other uses without permission.
Copyright © 2005 Massachusetts Medical Society. All rights reserved.
The new england journal of medicine
30 percent; hazard ratio, 0.64; 95 percent confi-
A dence interval, 0.48 to 0.85; P<0.002) (Fig. 1B and
100
Table 2). The principal cause of death was cardio-
Percentage of Patients Free of Death
vascular in 167 patients (83 percent), noncardiovas-
from Any Cause or Unplanned
Hospitalization for a Major
75 cular in 34 patients (17 percent), and not classifi-
Cardiovascular Event
Cardiac resynchronization able in 1 patient (0.5 percent). The cause of death
was attributed to worsening heart failure in 56 of
50
the 120 patients who died in the medical-therapy
group (47 percent) and in 33 of the 82 patients who
25 Medical therapy
died in the cardiac-resynchronization group (40 per-
cent). The mode of death was classified as sudden
P<0.001 in 38 of the 120 patients who died in the medical-
0 therapy group (32 percent) and in 29 of the 82 pa-
0 500 1000 1500
tients who died in the cardiac-resynchronization
Days
group (35 percent). The mortality rate in the med-
No. at Risk
Cardiac resyn- 409 323 273 166 68 7 ical-therapy group was 12.6 percent at one year and
chronization 25.1 percent at two years, as compared with 9.7 per-
Medical therapy 404 292 232 118 48 3
cent and 18.0 percent, respectively, in the cardiac-
resynchronization group.
B
100
There were three emergency and six elective
heart transplantations in the medical-therapy group
Cardiac resynchronization and one emergency and nine elective heart trans-
Percentage of Patients Free
of Death from Any Cause
75 plantations in the cardiac-resynchronization group.
All the patients who underwent emergency heart
Medical therapy
transplantation died. None of the patients who un-
50
derwent elective transplantation had died within
seven days after transplantation, at which point their
25 follow-up data were censored from the analysis.
P<0.002
other secondary end points
0
0 500 1000 1500 As compared with medical therapy alone, cardiac
Days resynchronization reduced the risk of the composite
No. at Risk end point of death from any cause or hospitalization
Cardiac resyn- 409 376 351 213 89 8 for worsening heart failure (hazard ratio, 0.54; 95
chronization
Medical therapy 404 365 321 192 71 5
percent confidence interval, 0.43 to 0.68; P<0.001)
(Table 2). There were 252 hospitalizations for wors-
Figure 1. Kaplan–Meier Estimates of the Time to the Primary End Point ening heart failure among 133 patients in the
(Panel A) and the Principal Secondary Outcome (Panel B). medical-therapy group (33 percent) and 122 such
The primary outcome was death from any cause or an unplanned hospitaliza- hospitalizations among 72 patients in the cardiac-
tion for a major cardiovascular event. The principal secondary outcome was resynchronization group (18 percent).
death from any cause.
As compared with patients in the medical-ther-
apy group, patients in the cardiac-resynchronization
group had less severe symptoms (P<0.001) and a
had unplanned hospitalizations for a major cardio- better quality of life (P<0.001) at 90 days (Table 2).
vascular event that occurred within 10 days after At 90 days, 15 patients had died in the medical-ther-
randomization and were therefore not counted as apy group and 12 patients had died in the cardiac-
primary end points. resynchronization group. At 18 months, 105 of the
patients in the cardiac-resynchronization group
deaths were in NYHA class I, 150 were in NYHA class II,
In the cardiac-resynchronization group, 82 patients and 80 were in NYHA class III or IV; the respective
died, as compared with 120 patients who had been values in the medical-therapy group were 39, 112,
assigned to medical therapy alone (20 percent vs. and 152.
1544 n engl j med 352;15 www.nejm.org april 14 , 2005
The New England Journal of Medicine
Downloaded from www.nejm.org on September 23, 2010. For personal use only. No other uses without permission.
Copyright © 2005 Massachusetts Medical Society. All rights reserved.
effect of cardiac resynchronization on heart failure
Table 2. Study Outcomes in Analyses Stratified According to NYHA Class.*
Medical Therapy Medical Therapy plus
Alone Cardiac Resynchronization Hazard Ratio
Outcome (N=404) (N=409) (95% CI) P Value
no. of patients (%)
Primary outcome
Death or unplanned hospitaliza- 224 (55) 159 (39) 0.63 (0.51 to 0.77) <0.001
tion for a cardiovascular event
Unplanned hospitalization for a 184 (46) 125 (31) 0.61 (0.49 to 0.77) <0.001
cardiovascular event†
Secondary outcome
Death from any cause 120 (30) 82 (20) 0.64 (0.48 to 0.85) <0.002
Death from any cause or un- 191 (47) 118 (29) 0.54 (0.43 to 0.68) <0.001
planned hospitalization
with worsening heart failure
Unplanned hospitalization with 133 (33) 72 (18) 0.48 (0.36 to 0.64) <0.001
worsening heart failure†
Medical Therapy Medical Therapy plus
Alone Cardiac Resynchronization Difference in Means
(N=404) (N=409) (95% CI)‡ P Value
value at 90 days
Continuous outcome
NYHA class 2.7±0.9 2.1±1.0 0.6 (0.4 to 0.7) <0.001
Minnesota Living with Heart 40±22 31±22 ¡10 (¡8 to ¡12) <0.001
Failure score§
EuroQoL EQ-5D score¶ 0.63±0.29 0.70±0.28 0.08 (0.04 to 0.12) <0.001
* Plus–minus values are means ±SD. The analysis was adjusted according to study center. NYHA denotes New York Heart
Association, and CI confidence interval.
† These events contributed to the primary or secondary outcome.
‡ The difference shown is for the cardiac-resynchronization group as compared with the medical-therapy group.
§ Scores on the Minnesota Living with Heart Failure questionnaire range from 0 to 105, with higher scores reflecting a
poorer quality of life.
¶ Scores on the European Quality of Life–5 Dimensions (EuroQoL EQ-5D) instrument range from –0.594 to 1.000, with
1.000 indicating fully healthy and 0 dead.
echocardiographic, biochemical, serious adverse events
and hemodynamic assessments There was one device-related death in each group:
At both 3 months and 18 months, the left ventricular one patient in the cardiac-resynchronization group
ejection fraction was significantly greater, the left died of heart failure aggravated by lead displace-
ventricular end-systolic volume index was signifi- ment, and one patient in the medical-therapy group
cantly lower, the area of mitral regurgitation was died of septicemia after receiving a device. The
significantly smaller, and the interventricular me- most common adverse device- or procedure-related
chanical delay was significantly shorter in the car- events in the cardiac-resynchronization group were
diac-resynchronization group than in the medical- lead displacement (24 patients), coronary-sinus dis-
therapy group (Table 3). By 18 months, plasma section (10 patients), pocket erosion (8 patients),
levels of N-terminal pro–brain natriuretic peptide pneumothorax (6 patients), and device-related in-
were lower among patients in the cardiac-resyn- fection (3 patients). Worsening heart failure was
chronization group (Table 3). Systolic blood pres- more common in the medical-therapy group (affect-
sure was higher at both 3 months and 18 months ing 263 patients, as compared with 191 patients
among patients in the cardiac-resynchronization in the cardiac-resynchronization group; P<0.001),
group. whereas atrial arrhythmias or ectopy was more com-
n engl j med 352;15 www.nejm.org april 14, 2005 1545
The New England Journal of Medicine
Downloaded from www.nejm.org on September 23, 2010. For personal use only. No other uses without permission.
Copyright © 2005 Massachusetts Medical Society. All rights reserved.
The new england journal of medicine
mon in the cardiac-resynchronization group (af-
fecting 64 patients in that group, as compared with Figure 2 (facing page). Effect of Cardiac Resynchroniza-
tion on the Primary End Point in Predefined Subgroups.
41 in the medical-therapy group; P=0.02). The fre-
Hazard ratios and 95 percent confidence intervals (CIs)
quencies of respiratory tract infections, hypoten- are shown. The subgroups of age, systolic blood pres-
sion, falls or syncope, acute coronary syndromes, sure, mitral-regurgitation area (as defined in Table 1),
renal dysfunction, ventricular arrhythmias or ecto- interventricular mechanical delay, ejection fraction, end-
py, and neurologic events were similar in the two systolic volume index, and glomerular filtration rate are
groups. divided according to the median value in the study popu-
lation. All analyses were stratified according to the NYHA
class, except the subgroup analysis of NYHA class. To
discussion convert values for N-terminal probrain natriuretic pep-
tide (NT-BNP) to picomoles per liter, divide by 8.457. For
We found that cardiac resynchronization substan- some data (QRS width, for instance), many patients had
tially reduced the risk of complications and death results at the median value, and this led to some inequal-
ity in the sizes of the subgroups. Because of missing
among patients with moderate or severe heart fail- baseline data, not all subgroup numbers total 813.
ure owing to left ventricular systolic dysfunction and
cardiac dyssynchrony. The benefits were similar
among patients with ischemic heart disease and pa-
tients without ischemic heart disease and were in The extent to which risk can be modified may be
addition to those afforded by pharmacologic thera- greater among patients with less severe disease.
py. The data are consistent with a resynchronization- Cardiac resynchronization may be beneficial in pa-
induced reduction in cardiac dyssynchrony, leading tients with cardiac dyssynchrony even if their symp-
to a sustained increase in left ventricular perfor- toms are not severe, although we excluded patients
mance and a diminution of mitral regurgitation and, judged by the investigator to be in NYHA class I or II.
in turn, a rise in perfusion pressure, a fall in cardiac The hazard ratio for death among patients with a
filling pressure, and favorable left ventricular re- cardiac-resynchronization device, as compared with
modeling. These changes in function translate into those receiving medical therapy alone (0.64; 95 per-
improvements in well-being and decreases in symp- cent confidence interval, 0.48 to 0.85; P<0.002),
toms, complications, and the risk of death. was similar to that among patients who received
The favorable effects of cardiac resynchroniza- both a resynchronization device and a defibrillator,
tion on symptoms, the quality of life, ventricular as compared with medical therapy alone, in the
function, and blood pressure in our trial are similar COMPANION trial (0.64; 95 percent confidence in-
to those reported in previous trials.4-8 However, we terval, 0.48 to 0.86; P=0.003).8 The COMPANION
also found that cardiac resynchronization signifi- trial was not designed to investigate differences be-
cantly reduced the risk of death. Calculations based tween the use of a cardiac-resynchronization device
on hazard ratios suggest that, for every nine devic- alone and the combination of a resynchronization
es implanted, one death and three hospitalizations device and an implantable defibrillator, but much of
for major cardiovascular events are prevented. This the effect of the latter approach could be explained
effect is in addition to the benefits of pharmacolog- by the cardiac-resynchronization component. In our
ic therapy and is similar to the reduction in the risk study, the cardiac-resynchronization group had a
of death associated with beta-blocker therapy as decreased incidence of sudden death and a de-
compared with placebo in a similar population.21 creased incidence of death from worsening heart
The benefit of cardiac resynchronization therapy failure, both of which may reflect an improvement
in our study was due, at least in part, to the adher- in cardiac function. A defibrillator might further
ence of patients and investigators to the protocol reduce the risk of sudden death.25,26 Twenty-nine
and to the increasing effect of cardiac resynchroni- patients (7 percent) in the cardiac-resynchroniza-
zation over a long follow-up period, but it was not tion group died suddenly.
due to the recruitment of patients at higher risk for Retarding the progression of cardiac dysfunction
events than those in other studies. Indeed, the mor- to prevent malignant arrhythmias may be a better
tality rate was lower than that in many other studies, strategy than treating malignant arrhythmias once
possibly reflecting the high standard of care, the they occur, because defibrillation is stressful to the
presence of less severe heart failure, or both.22-24 patient and associated with an adverse prognosis,
1546 n engl j med 352;15 www.nejm.org april 14 , 2005
The New England Journal of Medicine
Downloaded from www.nejm.org on September 23, 2010. For personal use only. No other uses without permission.
Copyright © 2005 Massachusetts Medical Society. All rights reserved.
effect of cardiac resynchronization on heart failure
Group Patients with Event/Total No. of Patients Hazard Ratio (95% CI)
Overall 383/813 0.63 (0.51–0.77)
Age
<66.4 yr 163/406 0.55 (0.40–0.75)
≥66.4 yr 220/407 0.68 (0.52–0.89)
Sex
Male 290/597 0.62 (0.49–0.79)
Female 93/215 0.64 (0.42–0.97)
NYHA class
III 349/763 0.64 (0.52–0.80)
IV 34/50 0.50 (0.25–1.01)
Dilated cardiomyopathy
No 238/443 0.68 (0.53–0.88)
Yes 145/370 0.51 (0.36–0.73)
Systolic blood pressure
<117 mm Hg 208/401 0.60 (0.46–0.80)
≥117 mm Hg 170/402 0.66 (0.48–0.89)
NT-BNP
<214.5 pg/ml 122/366 0.53 (0.36–0.76)
≥214.5 pg/ml 224/366 0.70 (0.54–0.91)
Ejection fraction
<24.7% 205/372 0.65 (0.49–0.86)
≥24.7% 152/373 0.62 (0.44–0.85)
End-systolic volume index
<119.2 ml/m2 156/366 0.71 (0.52–0.98)
≥119.2 ml/m2 193/366 0.54 (0.40–0.73)
QRS interval
<160 msec 152/290 0.74 (0.54–1.02)
≥160 msec 222/505 0.60 (0.46–0.79)
Interventricular mechanical delay
<49.2 msec 199/367 0.77 (0.58–1.02)
≥49.2 msec 147/368 0.50 (0.36–0.70)
Mitral-regurgitation area
<0.218 114/302 0.86 (0.60–1.25)
≥0.218 175/303 0.56 (0.41–0.75)
Glomerular filtration rate
<60.3 ml/min/1.73 m2 196/369 0.67 (0.50–0.89)
≥60.3 ml/min/1.73 m2 142/370 0.57 (0.40–0.80)
Beta-blockers
No 131/227 0.72 (0.51–1.02)
Yes 252/586 0.59 (0.46–0.76)
Spironolactone
No 166/356 0.58 (0.43–0.79)
Yes 217/457 0.67 (0.51–0.88)
Loop diuretics
<80 mg of furosemide or equivalent 181/461 0.56 (0.42–0.76)
≥80 mg of furosemide or equivalent 202/352 0.69 (0.53–0.92)
Digoxin
No 218/467 0.66 (0.50–0.86)
Yes 165/346 0.59 (0.43–0.81)
0.2 0.5 1.0 2.0
Resynchronization Better Medical Therapy Better
n engl j med 352;15 www.nejm.org april 14, 2005 1547
The New England Journal of Medicine
Downloaded from www.nejm.org on September 23, 2010. For personal use only. No other uses without permission.
Copyright © 2005 Massachusetts Medical Society. All rights reserved.
The new england journal of medicine
Table 3. Hemodynamic, Echocardiographic, and Biochemical Assessments.*
Difference in Means Difference in Means
Variable at 3 Mo (95% CI) P Value at 18 Mo (95% CI) P Value
Heart rate (beats/min) +1.1 (¡1.2 to 3.4) 0.33 +1.0 (¡1.5 to 3.6) 0.43
Systolic blood pressure (mm Hg) +5.8 (3.5 to 8.2) <0.001 +6.3 (3.6 to 8.9) <0.001
Diastolic blood pressure (mm Hg) +1.5 (0.1 to 2.9) 0.03 +1.3 (¡1.8 to 4.4) 0.42
Interventricular mechanical delay (msec) ¡21 (¡25 to ¡18) <0.001 ¡21 (¡25 to ¡17) <0.001
Left ventricular ejection fraction (%) +3.7 (3.0 to 4.4) <0.001 +6.9 (5.6 to 8.1) <0.001
Left ventricular end-systolic volume ¡18.2 (¡21.2 to ¡15.1) <0.001 ¡26.0 (¡31.5 to ¡20.4) <0.001
index (ml/m2)
Mitral-regurgitation area† ¡0.051 (¡0.073 to ¡0.028) <0.001 ¡0.042 (¡0.070 to ¡0.014) 0.003
N-terminal pro–brain natriuretic peptide ¡225 (¡705 to 255) 0.36 ¡1122 (¡1815 to ¡429) <0.002
(pg/ml)‡
* Differences were not adjusted for the higher mortality rate in the medical-therapy group. A plus sign indicates a greater
value, and a minus sign a smaller value, in the cardiac-resynchronization group than in the medical-therapy group. CI de-
notes confidence interval.
† The area was calculated as the area of the color-flow Doppler regurgitant jet divided by the area of the left atrium in sys-
tole, both in square centimeters.
‡ To convert the values for N-terminal pro–brain natriuretic peptide to picomoles per liter, divide by 8.457.
owing either to the cause of the arrhythmia or to Hull and East Yorkshire Cardiac Trust, Medtronic, Vasomedical, and
Abbott. Dr. Daubert reports having served as a consultant for and
the effects of the shock.27 Assuming that the com- having received speakers’ honoraria from Medtronic and St. Jude
bination of a cardiac-resynchronization device and Medical. Dr. Erdmann reports having served as a consultant for and
a defibrillator could prevent two thirds of sudden having received speakers’ honoraria from Takeda, Merck (Darm-
stadt), Medtronic, and Guidant. Dr. Freemantle reports having
deaths, a future study would require 1300 patients served as a consultant for Medtronic and Pfizer and having received
per group and a follow-up period similar to ours to speakers’ honoraria from Medtronic and grant support from
have a statistical power of 90 percent to detect an ab- Medtronic, Aventis, Amgen (United Kingdom), and the British
Heart Foundation. Dr. Gras reports having served as a consultant for
solute reduction in the risk of death from any cause and having received speakers’ honoraria from Medtronic and
of 5 percent with the use of combination therapy, Guidant. Dr. Kappenberger reports having served as a consultant
as compared with the use of cardiac resynchroniza- for Medtronic, having received speakers’ honoraria from Medtron-
ic, Biotronik, and Guidant, and having received grant support from
tion alone. Medtronic and the Swiss National Foundation for Scientific Re-
In summary, we found that cardiac resynchroni- search, Commission for Technology and Innovation/Kommission
zation is an effective therapy for patients with left für Technologie und Innovation, and the Swiss Heart Foundation.
Dr. Tavazzi reports having served as a consultant for Medtronic, Me-
ventricular systolic dysfunction and cardiac dyssyn- narini, Servier, and Pfizer and having received speakers’ honoraria
chrony who have moderate or severe heart failure from Medtronic, Novartis, and Takeda.
and who are in sinus rhythm. This article is dedicated to the memory of Werner Klein, profes-
Supported by a grant from Medtronic. sor of cardiology at the University Hospital of Graz (Austria), a
Dr. Cleland reports having served as a consultant for Medtronic, member of the steering committee who died in 2004. He contribut-
Amgen, Menarini, and Pfizer and having received speakers’ hono- ed substantially to the design and conduct of the study but did not
raria from Medtronic, Takeda, AstraZeneca, and Pfizer and grant live to see it completed. His wise counsel is greatly missed by his col-
support from the Medical Research Council (United Kingdom), leagues.
ap p e n d i x
The following persons participated in the CARE-HF Study: Steering Committee — J.G.F. Cleland (chair), J.-C. Daubert, E. Erdmann, D.
Gras, L. Kappenberger, W. Klein, L. Tavazzi; Data and Safety Monitoring Board — P.A. Poole-Wilson, L. Rydén (chair), H. Wedel, H.J.J.
Wellens; End-Points Committee — B. Uretsky, K. Thygesen; Independent Device-Related Adverse-Event Assessor — D. Böcker; Study
Management — M.M.H. Marijianowski; Statistical Analysis — N. Freemantle, M.J. Calvert; Pharmacologic Vigilance and Data Manage-
ment — Quintiles; Investigators — Austria: G. Christ, F. Fruhwald, R. Hofmann, A. Krypta, F. Leisch, R. Pacher, F. Rauscha; Belgium: R. Tav-
ernier; Denmark: P.E. Bloch Thomsen, S. Boesgaard, H. Eiskjær, G.T. Esperen, J. Haarbo, A. Hagemann, E. Korup, M. Møller, P. Mortensen,
P. Søgaard, T. Vesterlund; Finland: H. Huikuri, K.I. Niemelä, L. Toivonen; France: F. Bauer, A. Cohen-Solal, C. Crocq, P. Djiane, J.L. Dubois-
Rande, P. de Groote, Y. Juilliere, G. Kirkorian, M. Komajda, T. Laperche, H. Le Marec, C. Leclercq, C. Tribouilloy; Germany: F. Er, E. Fleck,
U.C. Hoppe, F.X. Kleber, B. Maisch, J. Neuzner, C. Reithmann, T. Remp, C. Schmitt, C. Stahl, R.H. Strasser; Italy: M.C. Albanese, A. Bar-
toloni, M. Bocchiardo, A. Capucci, A. Carboni, A. Circo, M. Disertori, R. del Medico, T. Forzani, M. Frigerio, A. Gavazzi, M. Landolina, M.
1548 n engl j med 352;15 www.nejm.org april 14 , 2005
The New England Journal of Medicine
Downloaded from www.nejm.org on September 23, 2010. For personal use only. No other uses without permission.
Copyright © 2005 Massachusetts Medical Society. All rights reserved.
effect of cardiac resynchronization on heart failure
Lunati, S. Mangiameli, M. Piacenti, A. Pitì, P.A. Ravazzi, A. Raviele, M. Santini, A. Serio, G.P. Trevi, M. Volterrani, M. Zardini; the Netherlands:
F.A.L.E. Bracke, C.C. de Cock, A. Meijer, R. Tukkie; Spain: J. Casares Mediavilla, M. Concha, J.F. Delgado, A. González-García, R. Muñoz-
Aguilera, J. Martínez Ferrer, F. Ridocci; Sweden: B. Andren, J. Brandt, P. Blomström, M. Edner, K. Hellström, S. Jensen, B. Kristensson, F. Ma-
ru, S.J. Moller, F. Rönn, P. Smedgård, G. Wikström; Switzerland: J. Fuhrer, G. Girod; United Kingdom: G.H. Broomes, S. Chalil, H. Dargie, W.
Davies, A. Delaney, P. Elliott, G.K. Goode, G. Haywood, G.C. Kaye, A.S. Kurbaan, R. Lane, T. Levy, F. Leyva, H. Marshall, S. Muhyaldeen, N.
Nitikin, M.J.D. Roberts, J.D. Skehan, W.D. Toff, D.J. Wright; Core Echocardiography Laboratory (Pavia, Italy) — C. Bassi, S. Ghio, E. Ghiz-
zardi, G. Magrini, M. Pasotti, V. Pierota, E. Tellaroli, A. Serio, L. Scelsi; Core Neuroendocrine Laboratory (Graz, Austria) — A. Fahrleitner,
G. Leb, H. Wenisch; Therapy Delivery (Kingston-upon-Hull, United Kingdom) — A. Bennett, M. Cooklin, J. Ghosh, S. Hurren, G.C. Kaye,
N.K. Khan.
references
1. Khand A, Gemmel I, Clark AL, Cleland 10. Calvert M, Freemantle N, Cleland JG. 20. Lan KKG, DeMets DL. Discrete sequen-
JGF. Is the prognosis of heart failure im- Cardiac resynchronization therapy in heart tial boundaries for clinical trials. Biometrika
proving? J Am Coll Cardiol 2000;36:2284-6. failure. Ann Intern Med 2005;142:305-7. 1983;70:659-63.
2. Cleland JGF, Clark AL. Delivering the 11. Cleland JGF, Daubert JC, Erdmann E, et 21. CIBIS-II Investigators and Committee.
cumulative benefits of triple therapy to im- al. The CARE-HF study (Cardiac Resynchro- The Cardiac Insufficiency Bisoprolol Study
prove outcomes in heart failure: too many nisation in Heart Failure study): rationale, II (CIBIS-II): a randomised trial. Lancet
cooks will spoil the broth. J Am Coll Cardiol design and end-points. Eur J Heart Fail 1999;353:9-13.
2003;42:1234-7. 2001;3:481-9. 22. Packer M, Coats AJS, Fowler MB, et al.
3. Rogers JG, Cain ME. Electromechanical 12. Calvert MJ, Freemantle N, Cleland JGF. Effect of carvedilol on survival in severe
associations. N Engl J Med 2004;350:2193-5. The impact of chronic heart failure on chronic heart failure. N Engl J Med 2001;
4. Cazeau S, Leclercq C, Lavergne T, et al. health-related quality of life data acquired in 344:1651-8.
Effects of multisite biventricular pacing in the baseline phase of the CARE-HF study. 23. The CONSENSUS Trial Study Group.
patients with heart failure and intraventricu- Eur J Heart Fail 2005;7:243-51. Effects of enalapril on mortality in severe
lar conduction delay. N Engl J Med 2001; 13. Cleland JGF, Daubert JC, Erdmann E, et congestive heart failure: results of the Coop-
344:873-80. al. Baseline characteristics of patients re- erative North Scandinavian Enalapril Surviv-
5. Young JB, Abraham WT, Smith AL, et al. cruited into the CARE-HF study. Eur J Heart al Study (CONSENSUS). N Engl J Med 1987;
Combined cardiac resynchronization and Fail 2005;7:205-14. 316:1429-35.
implantable cardioversion defibrillation in 14. Rector TS, Tschumperlin LK, Kubo SH, 24. Pitt B, Zannad F, Remme WJ, et al. The
advanced chronic heart failure: the MIRACLE et al. Use of the Living With Heart Failure effect of spironolactone on morbidity and
ICD Trial. JAMA 2003;289:2685-94. questionnaire to ascertain patients’ per- mortality in patients with severe heart fail-
6. Abraham WT, Fisher WG, Smith AL, et al. spectives on improvement in quality of life ure. N Engl J Med 1999;341:709-17.
Cardiac resynchronization in chronic heart versus risk of drug-induced death. J Card 25. Bardy GH, Lee KL, Mark DB, et al.
failure. N Engl J Med 2002;346:1845-53. Fail 1995;1:201-6. Amiodarone or an implantable cardiovert-
7. Higgins SL, Hummel JD, Niazi IK, et al. 15. Rector TS, Kubo SH, Cohn JN. Validity er–defibrillator for congestive heart failure.
Cardiac resynchronization therapy for the of the Minnesota Living with Heart Failure N Engl J Med 2005;352:225-37.
treatment of heart failure in patients with in- questionnaire as a measure of therapeutic 26. Cleland JGF, Ghosh J, Freemantle N, et
traventricular conduction delay and malig- response to enalapril or placebo. Am J Car- al. Clinical trials update and cumulative
nant ventricular tachyarrhythmias. J Am diol 1993;71:1106-7. meta-analyses from the American College of
Coll Cardiol 2003;42:1454-9. 16. Brooks R. EuroQol: the current state of Cardiology: WATCH, SCD-HeFT, DINAMIT,
8. Bristow MR, Saxon LA, Boehmer J, et al. play. Health Policy 1996;37:53-72. CASINO, INSPIRE, STRATUS-US, RIO-Lip-
Cardiac-resynchronization therapy with or 17. Shih JH. Sample size calculation for ids and cardiac resynchronisation therapy in
without an implantable defibrillator in ad- complex clinical trials with survival end- heart failure. Eur J Heart Fail 2004;6:501-8.
vanced chronic heart failure. N Engl J Med points. Control Clin Trials 1995;16:395-407. 27. Moss AJ, Greenberg H, Case RB, et al.
2004;350:2140-50. 18. Collett D. Modelling survival data in Long-term clinical course of patients after
9. McAlister FA, Ezekowitz JA, Wiebe N, et medical research. London: Chapman & Hall, termination of ventricular tachyarrhythmia
al. Systematic review: cardiac resynchroni- 1994. by an implanted defibrillator. Circulation
zation in patients with symptomatic heart 19. McCulloch CE, Searle SR. Generalized, 2004;110:3760-5.
failure. Ann Intern Med 2004;141:381-90. linear, and mixed models. New York: John Copyright © 2005 Massachusetts Medical Society.
[Erratum, Ann Intern Med 2005;142:311.] Wiley, 2001.
n engl j med 352;15 www.nejm.org april 14, 2005 1549
The New England Journal of Medicine
Downloaded from www.nejm.org on September 23, 2010. For personal use only. No other uses without permission.
Copyright © 2005 Massachusetts Medical Society. All rights reserved.
You might also like
- Castle AfDocument11 pagesCastle AfgustavoNo ratings yet
- Catheter Ablationin in AF With CHFDocument11 pagesCatheter Ablationin in AF With CHFKristian Sudana HartantoNo ratings yet
- Madit CRTNEJMseot 09Document10 pagesMadit CRTNEJMseot 09binh doNo ratings yet
- Reverse Tria24 MolDocument12 pagesReverse Tria24 Molbinh doNo ratings yet
- Biventricular Pacing For Atrioventricular Block and Systolic DysfunctionDocument9 pagesBiventricular Pacing For Atrioventricular Block and Systolic DysfunctionRaul OrtegaNo ratings yet
- Catheter Ablation in End Stage Heart FailureDocument10 pagesCatheter Ablation in End Stage Heart FailureJose Gomez MorenoNo ratings yet
- Prognostic Value of Increased Soluble Thrornbornodulin and Increased Soluble E-Selectin in Ischaernic Heart DiseaseDocument6 pagesPrognostic Value of Increased Soluble Thrornbornodulin and Increased Soluble E-Selectin in Ischaernic Heart DiseaseIoanna Bianca HNo ratings yet
- Ne W Engl and Journal MedicineDocument14 pagesNe W Engl and Journal MedicineDaniel ClarkNo ratings yet
- Ontarget NEJM PaperDocument13 pagesOntarget NEJM Paperyona selvia ariesNo ratings yet
- CHARM Alt TrialDocument5 pagesCHARM Alt TrialCristian Villarroel SNo ratings yet
- Auricchio & Cols. (1999)Document6 pagesAuricchio & Cols. (1999)Luba D'AndreaNo ratings yet
- Ok Fame - II - NEJM - 2012Document11 pagesOk Fame - II - NEJM - 2012Christian OliveiraNo ratings yet
- Defibrilator in CardioDocument10 pagesDefibrilator in CardioNabila CpNo ratings yet
- New England Journal Medicine: The ofDocument12 pagesNew England Journal Medicine: The ofJjawo GinesNo ratings yet
- BLOCK HF Trial. JACC 2016Document10 pagesBLOCK HF Trial. JACC 2016Ernesto J. Rocha ReyesNo ratings yet
- Jurnal TerapiDocument5 pagesJurnal TerapiMuhammad Aulia FahmiNo ratings yet
- CapricornDocument6 pagesCapricornMarkanthony256No ratings yet
- Heart Failure Thesis PDFDocument6 pagesHeart Failure Thesis PDFafknwride100% (2)
- HyhyDocument8 pagesHyhyAkram KastiranNo ratings yet
- Journal Medicine: The New EnglandDocument9 pagesJournal Medicine: The New Englandrahma watiNo ratings yet
- Nejmoa2021372 PDFDocument10 pagesNejmoa2021372 PDFNiki MawraNo ratings yet
- Cardiac ResuscitationDocument24 pagesCardiac ResuscitationPaulinaNo ratings yet
- Nej Mo A 2306037Document10 pagesNej Mo A 2306037Shrey SinghNo ratings yet
- Nejm 199507133330201Document6 pagesNejm 199507133330201Muhammad AqlaNo ratings yet
- Colchicine in Coronary Artery Disease (NEJM, 2020) PDFDocument10 pagesColchicine in Coronary Artery Disease (NEJM, 2020) PDFthe_leoNo ratings yet
- Trombolisis en PCR ExtrahospitalarioDocument12 pagesTrombolisis en PCR ExtrahospitalarioMariangel PerezNo ratings yet
- HOPE StudyDocument9 pagesHOPE StudyRezaNo ratings yet
- 49 54 PDFDocument6 pages49 54 PDFray m deraniaNo ratings yet
- 1 Out of 7 WHODocument2 pages1 Out of 7 WHOgnaneshwar nNo ratings yet
- Race Ii 2010 NejmDocument11 pagesRace Ii 2010 NejmAxel Hiram Hernandez PinedaNo ratings yet
- Terapia de Resincronización en Pacientes Con Insuficiencia Cardiaca Experiencia Acumulada de 10 AñosDocument9 pagesTerapia de Resincronización en Pacientes Con Insuficiencia Cardiaca Experiencia Acumulada de 10 AñosKevin Alegre AguileraNo ratings yet
- Nejmoa1608029 PDFDocument10 pagesNejmoa1608029 PDFFhirastika AnnishaNo ratings yet
- Heartfailure FixDocument10 pagesHeartfailure FixdhikaNo ratings yet
- Heart FailureDocument15 pagesHeart FailurewayralibertadNo ratings yet
- PolipillDocument10 pagesPolipillSMIBA MedicinaNo ratings yet
- 02art8090web PDFDocument9 pages02art8090web PDFSyilla PriscilliaNo ratings yet
- Initial Invasive or Conservative Strategy For Stable Coronary DiseaseDocument12 pagesInitial Invasive or Conservative Strategy For Stable Coronary DiseaseDrMarcus KeyboardNo ratings yet
- Ic 1 PDFDocument15 pagesIc 1 PDFMontserrat ÁlvarezNo ratings yet
- ESCAPE Study - JAMA 2005Document9 pagesESCAPE Study - JAMA 2005MICHAEL AMARILLO CORREANo ratings yet
- Closure of Patent Foramen Ovale Versus Medical Therapy After Cryptogenic StrokeDocument9 pagesClosure of Patent Foramen Ovale Versus Medical Therapy After Cryptogenic StrokelaurasheerNo ratings yet
- 1993, EpsteinDocument5 pages1993, EpsteinRob AlexandersNo ratings yet
- NEJMoa NEJM Bundle The Articles and Place in EverandDocument12 pagesNEJMoa NEJM Bundle The Articles and Place in Everandlakshminivas PingaliNo ratings yet
- Nejmoa 2206606Document10 pagesNejmoa 2206606dipan diratuNo ratings yet
- High Versus Normal Blood Pressure Targets in Relation To Right Ventricular Dysfunction After Cardiac Surgery: A Randomized Controlled TrialDocument11 pagesHigh Versus Normal Blood Pressure Targets in Relation To Right Ventricular Dysfunction After Cardiac Surgery: A Randomized Controlled TrialDina RyantiNo ratings yet
- Early Rhythm-Control Therapy in Patients With Atrial FibrillationDocument11 pagesEarly Rhythm-Control Therapy in Patients With Atrial FibrillationMohammad AlmuhaiminNo ratings yet
- Advanced Heart Failure Treated With Continuous-Flow Left Ventricular Assist DeviceDocument11 pagesAdvanced Heart Failure Treated With Continuous-Flow Left Ventricular Assist DeviceValentina ErquiagaNo ratings yet
- Focus 1 Paper 4 Verheye Et Al 2015Document9 pagesFocus 1 Paper 4 Verheye Et Al 2015Jesson LuiNo ratings yet
- Cardiac Resynchronization Therapy With MultipointDocument7 pagesCardiac Resynchronization Therapy With MultipointnanNo ratings yet
- Cardiac Resynchronisation Therapy For Patients With Heart FailureDocument5 pagesCardiac Resynchronisation Therapy For Patients With Heart FailureIpar DayNo ratings yet
- Hipertrofia VD en HTADocument8 pagesHipertrofia VD en HTAgustavo reyesNo ratings yet
- NeprilisinaDocument12 pagesNeprilisinaAndreaBuitragoMalaverNo ratings yet
- Prasugrel Versus Clopidogrel in Patients With Acute Coronary SyndromesDocument15 pagesPrasugrel Versus Clopidogrel in Patients With Acute Coronary SyndromesDito LopezNo ratings yet
- Case Reports AbstractsDocument7 pagesCase Reports AbstractsNovie AstiniNo ratings yet
- DACAMI TrialDocument6 pagesDACAMI TrialAlberto CardenasNo ratings yet
- 1 s2.0 S1071916423003068 MainDocument13 pages1 s2.0 S1071916423003068 Mainevelyn.minichNo ratings yet
- Progressive Right Ventricular Dysfunction in Patients With Pulmonary Arterial Hypertension Responding To TherapyDocument9 pagesProgressive Right Ventricular Dysfunction in Patients With Pulmonary Arterial Hypertension Responding To TherapyinaNo ratings yet
- Fa Articulo 2020Document11 pagesFa Articulo 2020Liliana GuzmanNo ratings yet
- Eficacia de La Telemedicina en El Manejo de La Insuficiencia CardíacaDocument11 pagesEficacia de La Telemedicina en El Manejo de La Insuficiencia CardíacaSMIBA MedicinaNo ratings yet
- Fifteen-Year Experience: Open Heart Surgery in Patients With End-Stage Renal FailureDocument6 pagesFifteen-Year Experience: Open Heart Surgery in Patients With End-Stage Renal FailureDavid RamirezNo ratings yet
- Shco Toolkit PDFDocument14 pagesShco Toolkit PDFSatish JainNo ratings yet
- Informed Consent For Peripheral Iridotomy: Angle-Closure GlaucomaDocument2 pagesInformed Consent For Peripheral Iridotomy: Angle-Closure GlaucomaSamatha BiotechNo ratings yet
- Yag PiDocument2 pagesYag PiSamatha BiotechNo ratings yet
- Spillage ProcedureDocument5 pagesSpillage ProcedureSamatha BiotechNo ratings yet
- Consent Chalazion PDFDocument1 pageConsent Chalazion PDFSamatha BiotechNo ratings yet
- Spillage Management: Arrangements AND GuidanceDocument10 pagesSpillage Management: Arrangements AND GuidanceSamatha BiotechNo ratings yet
- Tips To Prevent The Spread of InfectionDocument2 pagesTips To Prevent The Spread of InfectionSamatha BiotechNo ratings yet
- Housekeeping Materials - Study in Indian HospitalsDocument13 pagesHousekeeping Materials - Study in Indian HospitalsDevi_CNo ratings yet
- Bioptron General Information LeafletDocument2 pagesBioptron General Information Leafletbbmvg100% (1)
- ESR TemplateDocument2 pagesESR TemplateDan Joseph AguilarNo ratings yet
- Bleeding Disorder (Paediatrics)Document95 pagesBleeding Disorder (Paediatrics)Nurul Afiqah Mohd YusoffNo ratings yet
- Psychopharmacology of AutismDocument17 pagesPsychopharmacology of AutismMichelle2No ratings yet
- Serum Creatinine: General CommentsDocument4 pagesSerum Creatinine: General CommentsYasir MushtaqNo ratings yet
- Antibabesial Treatment Protocols Against Canine Babesiosis: W.R. Bandula Kumara B.V.SC., PH.DDocument8 pagesAntibabesial Treatment Protocols Against Canine Babesiosis: W.R. Bandula Kumara B.V.SC., PH.DJehan Somasiri JayathungaNo ratings yet
- Get Vaccinated-Argument EssayDocument4 pagesGet Vaccinated-Argument Essayapi-489674055No ratings yet
- Peace Corps Vaccine Administration Schedule - TG 300 Medical Technical Guideline 300 - July 2008Document4 pagesPeace Corps Vaccine Administration Schedule - TG 300 Medical Technical Guideline 300 - July 2008Accessible Journal Media: Peace Corps Documents100% (1)
- A Comparative Study of Three PeriapicalDocument6 pagesA Comparative Study of Three PeriapicalRamona MateiNo ratings yet
- Methods of Pushing During Vaginal Delivery and Pelvic Floor and Perineal Outcomes: A ReviewDocument7 pagesMethods of Pushing During Vaginal Delivery and Pelvic Floor and Perineal Outcomes: A ReviewToqa DabbasNo ratings yet
- CG19 Dental Recall - Full Guideline MDocument68 pagesCG19 Dental Recall - Full Guideline MananthiNo ratings yet
- Stress WorkshopDocument14 pagesStress Workshopapi-297796125No ratings yet
- NP2 Pre Board Practice TestDocument12 pagesNP2 Pre Board Practice TestErickaNo ratings yet
- Toxic Anterior Segment SyndromeDocument13 pagesToxic Anterior Segment SyndromePrathibha M ChachadiNo ratings yet
- Complete Blood Picture: Master Degree in Clinical Pathology, Faculty of Medicine, Cairo University DR - Enas AzzazyDocument2 pagesComplete Blood Picture: Master Degree in Clinical Pathology, Faculty of Medicine, Cairo University DR - Enas AzzazyMohamed BadraNo ratings yet
- Systolic Heart FailureDocument66 pagesSystolic Heart FailureFerinaTarizaIINo ratings yet
- A.Chn As A Field of Nursing PracticeDocument1 pageA.Chn As A Field of Nursing PracticeHanna LopezNo ratings yet
- Tracy Batchelor, Ryo Nishikawa, Nancy Tarbell, Michael Weller - Oxford Textbook of Neuro-Oncology-Oxford University Press (2017)Document269 pagesTracy Batchelor, Ryo Nishikawa, Nancy Tarbell, Michael Weller - Oxford Textbook of Neuro-Oncology-Oxford University Press (2017)gaanbazar100% (1)
- Lec. Deep CariesDocument47 pagesLec. Deep CariesMaria EvergardenNo ratings yet
- Datesheet End Term Exam Dec-2023Document34 pagesDatesheet End Term Exam Dec-2023Neerock KhatriNo ratings yet
- Bipolar Disorder: Bipolar I Disorder - Defined by Manic Episodes That Last at Least 7 Days, or by ManicDocument3 pagesBipolar Disorder: Bipolar I Disorder - Defined by Manic Episodes That Last at Least 7 Days, or by ManicVincent Paul SantosNo ratings yet
- BHW Reference Manual and Playbook - TagalogDocument136 pagesBHW Reference Manual and Playbook - TagalogCarlen Mae L. YacapinNo ratings yet
- Or NCP (Risk For Infection)Document1 pageOr NCP (Risk For Infection)Nikki M. Arapol100% (1)
- Drink Air Therapy To Kill Diabetes - A Path To Self-Cure and Immortality PDF Scribd - Google SearchDocument1 pageDrink Air Therapy To Kill Diabetes - A Path To Self-Cure and Immortality PDF Scribd - Google SearchNugraha PratamaNo ratings yet
- Psychotherapy Progress NoteDocument1 pagePsychotherapy Progress NoteArmaan Malik100% (2)
- Complete Blood Picture: 73 Year Female 49320502554Document1 pageComplete Blood Picture: 73 Year Female 49320502554ahmed khalidNo ratings yet
- Community - Based NursingDocument16 pagesCommunity - Based NursingManu CvNo ratings yet
- To Whomsoever It May ConcernDocument7 pagesTo Whomsoever It May ConcernMuhammad IbrahimNo ratings yet
- Guideline 133FM PDFDocument13 pagesGuideline 133FM PDFPangestu DhikaNo ratings yet
- Resume of Shannon43613Document2 pagesResume of Shannon43613api-29418893No ratings yet
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (2)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (29)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (81)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (4)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (253)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (5)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (45)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- Summary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: Thinking, Fast and Slow: by Daniel Kahneman: Key Takeaways, Summary & Analysis IncludedRating: 4 out of 5 stars4/5 (61)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesFrom EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesRating: 4.5 out of 5 stars4.5/5 (1412)
- How to ADHD: The Ultimate Guide and Strategies for Productivity and Well-BeingFrom EverandHow to ADHD: The Ultimate Guide and Strategies for Productivity and Well-BeingRating: 1 out of 5 stars1/5 (1)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (59)