Professional Documents
Culture Documents
Modern Management of Traumatic Hemothorax 2167 1222 1000326
Uploaded by
anon_12953532Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Modern Management of Traumatic Hemothorax 2167 1222 1000326
Uploaded by
anon_12953532Copyright:
Available Formats
uma &
Tra Tr
of
ea
l
Journal of Trauma & Treatment
Journa
tme
nt
Mahoozi, et al., J Trauma Treat 2016, 5:3
DOI: 10.4172/2167-1222.1000326
ISSN: 2167-1222
Review Article Open Access
Modern Management of Traumatic Hemothorax
Hamid Reza Mahoozi, Jan Volmerig and Erich Hecker*
Thoraxzentrum Ruhrgebiet, Department of Thoracic Surgery, Evangelisches Krankenhaus, Herne, Germany
*Corresponding author: Erich Hecker, Thoraxzentrum Ruhrgebiet, Department of Thoracic Surgery, Evangelisches Krankenhaus, Herne, Germany, Tel:
0232349892212; Fax: 0232349892229; E-mail: e.hecker@evk-herne.de
Rec date: Jun 28, 2016; Acc date: Aug 17, 2016; Pub date: Aug 19, 2016
Copyright: © 2016 Mahoozi HR. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use,
distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Hemothorax is defined as a bleeding into pleural cavity. Hemothorax is a frequent manifestation of blunt chest
trauma. Some authors suggested a hematocrit value more than 50% for differentiation of a hemothorax from a
sanguineous pleural effusion. Hemothorax is also often associated with penetrating chest injury or chest wall blunt
chest wall trauma with skeletal injury. Much less common, it may be related to pleural diseases, induced iatrogenic
or develop spontaneously. In the vast majority of blunt and penetrating trauma cases, hemothoraces can be
managed by relatively simple means in the course of care.
Keywords: Traumatic hemothorax; Internal chest wall; Cardiac Hemodynamic response
injury; Clinical manifestation; Blunt chest-wall injuries; Blunt
As above mentioned the hemodynamic response is a multifactorial
intrathoracic injuries; Penetrating thoracic trauma
response and depends on severity of hemothorax according to its
classification. Hemothorax is classified according to the amount of
Introduction blood loss: minimal, moderate, or massive.
Hemothorax is one of the most frequent consequences of thoracic A minimal hemothorax is defined as a blood loss without significant
traumas. Early detection and treatment of hemothorax is of utmost hemodynamic changes. Blood loss in a 75-kg patient without
importance in prognosis of the patient. About 60% of polytraumas are underlying disease up to 750 ml is usually without any significant
associated with thoracic trauma. 150,000 Americans die due to trauma hemodynamic response and classified as minimal hemothorax. The
every year and it is the most common cause of death in the population hemodynamic response is adjusted usually to amount of blood loss,
<40 years age. One fourth of deaths are particularly related to chest underlying disease and location of injury.
trauma.
If the patient has pre-existing pleural bonding, the adhesions may
Mortality associated with a great vessel or cardiac injury is limit the amount of blood loss, particularly from low-pressure sources
significant, with >50% of patients dying immediately and less than and may be lifesaving.
10-15% surviving until hospital admittance with critical vital signs.
Blood loss of more than 30% of blood volume (1500-2000 ml) is
usually associated with hemorrhagic shock (massive hemothorax)
Etiology [8,9].
The etiology of hemothorax is commonly subdivided into traumatic
and non-traumatic. The traumatic hemothorax is a result of blunt or Respiratory response
penetrating trauma. Non traumatic hemothorax may develop by
various diseases or disorders such as neoplasia, lung sequester, Numerous factors affect the respiratory response. A trauma
ruptured pleural adhesion in the case of pneumothorax, pulmonary associated respiratory failure may occur directly or indirectly. An
infarction, tuberculosis, pulmonary infection (e.g. Dengue indirectly associated respiratory failure occurs because of pulmonary
hemorrhagic fever), pulmonary arteriovenous fistulae and abdominal infection, fibrothorax as a late complication and trauma in a patient
anomaly and pathology [1-7]. with underlying disease.
A directly trauma associated failure occurs as a result of direct
Pathophysiology pulmonary, chest wall and cardiac injury or systemic response in form
of ARDS resulting from diffuse alveolar damage with increasing
Intrapleural or extrapleural injuries can lead to a hemothorax. The capillary permeability [9,10].
physiologic response to a hemothorax contains an early and a late
response. The early response is manifested in two major aspects:
Physiologic resolution of hemothorax
hemodynamic and respiratory. The late response is manifested in two
forms: empyema and fibrothorax. Defibrination of hemothorax commences some hours after
formation of hemothorax. Some degree in defibrination of hemothorax
The severity of pathophysiological response is dependent on
concludes incomplete clotting. After lysis of hemothorax by the pleural
location of injury, the functional reserve of patient and amount of
enzymes increases the concentration of protein. An intrapleural
blood loss.
hyperosmotic pressure produces a positive osmotic gradient and
promotes formation of a pleural effusion. By this, relatively small
J Trauma Treat, an open access journal Volume 5 • Issue 3 • 1000326
ISSN:2167-1222
Citation: Mahoozi HR, Volmerig J, Hecker E (2016) Modern Management of Traumatic Hemothorax. J Trauma Treat 5: 326. doi:
10.4172/2167-1222.1000326
Page 2 of 5
amounts of blood in the pleural space may have a similar effect to that A small hemothorax may be overlooked during physical
of chronic subdural hematomas, drawing in fluids over time and examination and even chest radiography.
causing a large effusion with little actual blood content [1,9,11].
The chest wall injuries are subdivided to simple and complex chest
wall injuries.
Late physiologic systemic reaction
A simple chest wall injury consists of less than three single rib
Late physiologic reactions of hemothorax consist of empyema and fractures and superficial soft tissue injuries. This type of injury usually
fibrothorax. can be handled by conservative treatment.
Primary or secondary contamination of hemothorax concludes Fractures of three or more sequential ribs and a flail chest are
empyema. Bronchio-tracheal lesions, esophageal injuries, categorized as complex chest wall injuries and frequently associated
diaphragmatic and subdiaphragmatic injuries, accumulation of fluid in with a significant degree of hemothorax.
the subdiaphragmatic area and postsurgical contamination contribute
to development of posttraumatic empyema (Figure 1). A hemothorax can develop after some interval of trauma. Possible
mechanisms of development of delayed hemothorax are displacement
Fibrothorax results from fibrin deposition in the pleural surfaces of fractured ribs with pulmonary parenchymal laceration, lesion of the
[12]. An undrained pleural fluid regardless of its origin induces an diaphragm or intercostal vessel disruption [15,16].
inflammatory response and leads to inflammatory coating of visceral
and parietal pleura. The chest wall and diaphragm are affected in a
Blunt intrathoracic injuries
similar process, which in total leads to entrapment of the lung. The
entrapment of the lung restricts the ventilatory function and typically Vascular injuries usually lead to large hemothoraces. Laceration of
reduces lung volume [12]. great vessels and heart injuries may result in hemorrhage into the
pleural space and subsequent exsanguination. In rare conditions,
Clinical Manifestations partial tears of vessels create hematomas that may help to arrest the
hemorrhage.
Clinical manifestations of patients with chest trauma are dependent
on mechanism of injury and the organs involved. Patients who suffer Symptoms vary widely from mild to severe, depending on pattern
blunt thoracic trauma are at considerable risk of associated injuries, and location of injury. Respiratory manifestations related to large
deterioration and mortality [13]. In contrast to penetrating thoracic hemothorax as well as dullness to percussion and absent breath sounds
trauma, the biomechanical force required to produce significant blunt are noted as typical signs and symptoms [6,14,16].
thoracic injury often results in multiple injuries including abdominal,
head and extremity injuries [14]. Penetrating trauma
The most common reason for hemothorax after penetration is direct
laceration of arteries of the chest. Other intrathoracic structures,
including heart and pulmonary parenchymal injury should be
considered (Figure 2).
Pulmonary parenchymal injury in penetration of the chest wall is
very common and usually self-limiting, but these injuries usually result
in a hemo-pneumothorax [10,16].
Clinical manifestation in traumatic hemothorax
In case of trauma, thorough and accurate physical examination
should be exercised. Bloody pleural effusion distributes in supine
position and can be easily missed during the physical examination. It is
strongly advised to perform physical examination in upright position
or a slight reverse Trendelenburg position of the patient in order to
identify smaller hemothoraces. Less than 500 ml bloody pleural
effusion in the costophrenic angle may be overlooked in physical
examination (Figure 3).
Figure 1: Chest X-ray; left-sided hemothorax after blunt trauma. The origin of hemothorax may arise from an intra-abdominal
injury. The possibility of intra-abdominal injury e.g. of spleen, liver,
stomach and vessels should be considered in every case of hemothorax
Blunt chest wall injuries and particularly in case of encountered diaphragmatic injury [8,16].
Blunt chest wall traumas may cause hemothorax, pulmonary
contusion, pulmonary laceration, traumatic pulmonary pseudocyst, Treatment
pulmonary hematoma, traumatic asphyxia and bony skeletal injuries. The treatment of hemothorax contains an early phase e.g.
Multiple rib fractures are the most common blunt chest injuries and hemorrhagic shock, respiratory compromise or retained clot and a late
occur in about 36-50% of cases (about 36% on the right side, and 51% phase e.g. fibrothorax and empyema.
on the left side).
J Trauma Treat, an open access journal Volume 5 • Issue 3 • 1000326
ISSN:2167-1222
Citation: Mahoozi HR, Volmerig J, Hecker E (2016) Modern Management of Traumatic Hemothorax. J Trauma Treat 5: 326. doi:
10.4172/2167-1222.1000326
Page 3 of 5
Minimal collection of blood (defined as <300 ml) in the pleural Video-Assisted Thoracoscopy (VATS)
cavity requires no treatment; the blood is usually resorbed over several
weeks. If the patient is stable and presents with minimal respiratory Video-assisted thoracoscopy (VATS) provides entire vision of the
distress, operative intervention is not required. This group of patients complete pleural cavity with the possibility to correct chest tube –
can be treated by analgesia as needed and observed with repeated chest placement, control of bleeding and removal of retained clot [20,21].
radiographs at 4-6 hours and 24 hours [17]. In case of pulmonary Most authors advise a VATS in the case of hemothorax with more than
parenchymal fistulae after insertion of thoracostomy tube a possibility 300 ml because of more favorable outcomes compared to patients who
of thoracoscopic approach should be evaluated and considered. did not receive a VATS [20-22].
According to the Advanced Trauma Life Support (ATLS) guidelines, Thoracotomy
1500 ml of blood drainage in 24 hours or >250 ml of blood drainage
hourly for three consecutive hours after chest tube insertion are the The procedure of choice in critical situation with massive
criteria for surgical exploration after penetrating chest trauma. These hemothorax and suspicion of injury of heart and great vessels is
criteria, however, are not mandatory. Other accepted indications for thoracotomy. When urgent thoracotomy is required in emergency, the
surgical exploration are management and prevention of the late choice of incision is influenced by many factors including operative
complications such as fibrothorax and empyema [6,18-20]. If emergent indications, mechanism of injury and the radiographic findings.
thoracotomy is indicated adequate exposure of the entire pleural cavity The indications for urgent thoracotomy as outlined by the ATLS
is required. protocol:
Closed tube thoracostomy • Chest drainage >1500 ml initial or >200 ml/hr
• Large unevacuated clotted hemothorax
Needle aspiration as a definitive treatment of a hemothorax is an • Developing cardiac tamponade
obsolete intervention. The adequate approach to a hemothorax is a
• Chest wall defect
complete evacuation of retained clots either by tube thoracotomy or
videoassisted thoracoscopy (VATS) [6,8,17-19]. • Massive air leak or incomplete lung expansion despite adequate
drainage
Adequate management of hemothorax mandates complete • Great vessel injury
evacuation of the blood collection. A 24- or 28-french chest tube is
• Esophageal injury
commonly sufficient to accomplish this goal.
• Diaphragmatic injury
Incomplete or ineffective drainage particularly in the case of severe • Cardiac injury (traumatic septal or valvular injury)
pleural adhesions is contraindicated. In such cases, VATS or
thoracotomy with dissection of adhesions is a safer approach [8,17-20]. Intubation in urgent situations should be commenced rapidly to
prevent aspiration. Thoracotomy is sometimes required in the case of
empyema stage III according to ATS (American Thoracic Society)
Drainage in patients with coagulopathy
classification.
Drainage of hemothorax in case of coagulopathy should be
performed carefully with consideration of the underlying disease.
Correction of coagulation function prior to surgical intervention
should be performed if permitted by clinical patient status. Needle
aspiration in case of untreated coagulopathy is contraindicated [6,18].
Figure 3: Left-sided hemothorax and atelectasis of left lower lobe.
Figure 2: Hemothorax in penetrating trauma.
Management of retained clot
Management of retained clot comprises controversy opinions from
conservative therapy to surgical approach. Frequent current opinion
advocates an early thoracoscopic approach (VATS) and removal of
J Trauma Treat, an open access journal Volume 5 • Issue 3 • 1000326
ISSN:2167-1222
Citation: Mahoozi HR, Volmerig J, Hecker E (2016) Modern Management of Traumatic Hemothorax. J Trauma Treat 5: 326. doi:
10.4172/2167-1222.1000326
Page 4 of 5
retained clot with mobilization of the lung for re-expansion. Early answer this question but in a retrospective analysis, VATS was found to
video-assisted thoracoscopy (VATS) has greatly diminished the late be superior to IPFT, both in terms of decreased hospital stay and
complication of hemothorax with positive impact on the length of stay necessity thoracotomy (Figure 4).
in the hospital and survival of patients particularly in elderly.
Published studies revealed clinical outcomes in patients who received Complications
early VATS were more favorable compared to patients who did not
receive early VATS [6,18-23]. Inadequate or incorrect placement of chest tubes leads to
insufficient hemothorax drainage. Bacterial contamination of long-
Video-assisted thoracoscopic surgery (VATS) is believed to be the term retained clot in tube thoracostomy or undrained hemothorax can
best available modality for the management of clotted hemothorax. promote empyema [26]. Fibrothorax develops as a late complication
However, VATS is not routinely available in many centres. One easily due to inflammatory coating of visceral and parietal pleura and
available and effective alternative to VATS is the use of intrapleural reduces the ventilatory function. Decortication of visceral pleura is the
fibrinolysis (IPF) [24-31]. There have not been any prospective trials to therapy of choice to provide lung reexpansion [15,24,25].
Figure 4: Algorithm for diagnostic and therapeutic approach to hemothorax.
Outlook and Discussion hemothorax. Abdominal sonography in case of chest trauma should be
performed routinely [6,15,18-21].
The decision for early removal of retained hemothorax/ blood clots
per VATS greatly reduces late complications such as empyema,
fibrothorax, morbidity and necessity of late secondary thoracotomy. In
References
addition, early VATS approach reduces the length of hospital stay 1. Cohen RG, DeMeester TR, LaFontaine E (1995) The Pleura. In: Sabiston
compared to sole tube thoracostomy or conservative management of DC, Spencer FC (eds.) Surgery of the chest. Vol 1 (6thedn). Philadelphia,
Pa: WB Saunders, pp: 523-575.
J Trauma Treat, an open access journal Volume 5 • Issue 3 • 1000326
ISSN:2167-1222
Citation: Mahoozi HR, Volmerig J, Hecker E (2016) Modern Management of Traumatic Hemothorax. J Trauma Treat 5: 326. doi:
10.4172/2167-1222.1000326
Page 5 of 5
2. Morikawa H, Hirota K, Kito K, Fujita H, Mishima S (1994) Re-expansion 19. Meyer DM, Jessen ME, Wait MA, Estrera AS (1997) Early evacuation of
pulmonary oedema following removal of intrathoracic haematoma. Acta traumatic retained hemothoraces using thoracoscopy: a prospective,
Anaesthesiol Scand 38: 518-520. randomized trial. Ann Thorac Surg 64:1396-1400.
3. May J, Ades A (2013) Porous diaphragm syndrome: haemothorax 20. Cobanoglu U, Sayir F, Mergan D (2011) Should videothoracoscopic
secondary to hemoperitoneum following laparoscopic hysterectomy. BMJ surgery be the first choice in isolated traumatic hemothorax? A
Case Rep Pii: BCR 2013201088. prospective randomized controlled study. Ulus Travma Acil Cerrahi Derg
4. Thekkudan J, Luckraz H, Ng A, Norell M (2012) Tricuspid valve chordal 17:117-122.
rupture due to airbag injury and review of pathophysiological 21. Chang YT, Dai ZK, Kao EL, Chuang HY, Cheng YJ, et al. (2007) Early
mechanisms. Interact Cardiovasc Thorac Surg 15: 555-557. video-assisted thoracic surgery for primary spontaneous
5. Liman ST, Kuzucu A, Tastepe AI, Ulasan GN, Topcu S (2003) Chest hemopneumothorax. World J Surg 31: 19-25.
injury due to blunt trauma. Eur J Cardiothorac Surg 23: 374-378. 22. Huang WY, Lu iY, Yang C, Chou YP, Lin HL (2016) Efficiency analysis of
6. Hecker E, Welcker K, Schlolaut B (2006) Video-assisted thoracoscopy direct video-assisted thoracoscopic surgery in elderly patients with blunt
(VATS) for the management of traumatic hemothorax. Chest 130: 277S-a. traumatic hemothorax without an initial thoracostomy. BioMed Research
7. LoCicero J III, Mattox KI (1989) Epidemiology of chest trauma. Surg Clin International.
North Am 69: 15-19. 23. 23. Chou YP, Lin HL, Wu TC (2015) Video-assisted thoracoscopic surgery
8. American College of Surgeons, committee on Trauma (2013) Thoracic for retained hemothorax in blunt chest trauma. Curr Opin Pulm Med 21:
trauma. In: Advanced trauma life support for doctors. Instructor Course 393-398.
Manual. Chicago III: American college of Surgeons. 24. Sinha P, Sarkar P (1998) Late clotted haemothorax after blunt chest
9. Kinasewitz GT (1998) Pleural fluid dynamics and effusions. In: Fishmann trauma. J Accid Emerg Med 15: 189-191.
AP (ed.) Pulmonary diseases and disorders, (3rdedn). Mc Gaw- Hill, New 25. Yeam I, Sassoon C (1997) Hemothorax and chylothorax. Curr Opin Pulm
York. med 3: 310-314.
10. Rusch VW, Ginsberg RJ (1999) Chest wall, pleura, lung and mediastinum. 26. Kwiatt M, Tarbox A, Seamon MJ, Swaroop M, Cipolla J, et al. (2014)
In: Schwartz SI, (ed.) Principles of Surgery. (7thedn). New York, NY: Thoracostomy tubes: A comprehensive review of complications and
McGraw-Hill, pp: 667-790. related topics. Int. J Crit ILLn Inj Sci 4: 143-155.
11. Inci I, Ozcelik C, Ulku R, Tuna A, Eren N (1998) Intrapleural fibrinolytic 27. Pillai RS, Prasad P, Nair RG, Pillai SB, Puthenveetil BT, et al. (2013)
treatment of traumatic clotted hemothorax. Chest 114: 160-165. Multiple ventricular septal rupture after blunt trauma. Ann Thorac Surg
12. Jantz MA, Antony VB (2006) Pleural fibrosis. Clin Chest Med 27:181-191. 96: 297-298.
13. Weyant MJ, Fullerton DA (2008) Blunt thoracic trauma. Semin Thorac 28. Agarwal R, Aggarwal AN, Gupta D (2006) Intrapleural fibrinolysis in
clotted haemothorax. Singapore Med J 47: 984-986.
Cardiovasc Surg 20: 26-30.
14. Hurt R (1996) The management of fractured ribs and wounds of the 29. Jerjes-Sanchez C, Ramirez-Rivera A, Elizalde JJ, Delgado R, Cicero R, et
al. (1996) Intrapleural fibrinolysis with streptokinase as an adjunctive
chest. In: The History of Cardiothoracic Surgery. London, UK: Parthenon
treatment in hemothoraxand empyema: a multicenter trial. Chest 109:
Publishing Group, pp: 231-265.
1514-1519.
15. Karmy-Jones R, Jurkovich GJ (2004) Blunt chest trauma. Curr Probl Surg
41: 223-380. 30. Cangir AK, Yuksel C, Dakak M, Ozgencil E, Genc O, et al. (2005) Use of
intrapleural streptokinase in experimental minimal clotted hemothorax.
16. Richardson JD, Miller FB, Carrillo EH, Spain DA (1996) Complex Eur J Cardiothorac Surg 27: 667-670.
thoracic injuries. Surg Clin North Am 76: 725-748.
31. Oguzkaya F, Akcali Y, Bilgin M (2005) Videothoracoscopy versus
17. Heniford BT, Carrillo EH, Spain DA, Sosa JL, Fulton RL, et al. (1997) The intrapleural streptokinase for management of post traumatic retained
role of thoracoscopy in the management of retained thoracic collections hemothorax: a retrospective study of 65 cases. Injury 36: 526-529.
after trauma. Ann Thorac Surg 63: 940-943.
18. Liu DW, Liu HP, Lin PJ, Chang CH (1997) Video-assisted thoracic surgery
in treatment of chest trauma. J Trauma 42: 670-674.
J Trauma Treat, an open access journal Volume 5 • Issue 3 • 1000326
ISSN:2167-1222
You might also like
- Spiderman Invitation & Thank You CardDocument1 pageSpiderman Invitation & Thank You Cardanon_12953532No ratings yet
- Spiderman Cupcake ToppersDocument1 pageSpiderman Cupcake Toppersanon_12953532No ratings yet
- Spiderman Bottle LabelDocument1 pageSpiderman Bottle Labelanon_12953532No ratings yet
- Rekomendasi Antibiotik Rute Pemberian (Po / Drip/ Bolus) Dosis/ Interval Pemberian Lama Pemberian (Hari) Sumber Referensi KeteranganDocument4 pagesRekomendasi Antibiotik Rute Pemberian (Po / Drip/ Bolus) Dosis/ Interval Pemberian Lama Pemberian (Hari) Sumber Referensi Keterangananon_12953532No ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Exp 4 Centrifugal CompressorDocument11 pagesExp 4 Centrifugal CompressorFaris HamirNo ratings yet
- Heat Transfer Lab AssignmentDocument5 pagesHeat Transfer Lab AssignmentChristyNo ratings yet
- The Well (Version 2.4)Document3 pagesThe Well (Version 2.4)Thaís EspinosaNo ratings yet
- GS Module 3 ConcessionDocument3 pagesGS Module 3 ConcessionManolacheNo ratings yet
- 900 ADA - Rev13Document306 pages900 ADA - Rev13Miguel Ignacio Roman BarreraNo ratings yet
- INTERWELL Anchored Production Straddle Product SheetDocument2 pagesINTERWELL Anchored Production Straddle Product SheetDavid Pit FermiereNo ratings yet
- Biological Activity of Bone Morphogenetic ProteinsDocument4 pagesBiological Activity of Bone Morphogenetic Proteinsvanessa_werbickyNo ratings yet
- Chapter 4 - Medical Aspects of Food SafetyDocument17 pagesChapter 4 - Medical Aspects of Food SafetyasushkNo ratings yet
- Jurnal Aquaponik Jada BahrinDocument36 pagesJurnal Aquaponik Jada BahrinbrentozNo ratings yet
- Behavior Modification: Presented By: Wajeeha Iqbal BS in Psychology, MS (SLP/T) Riphah College of Rehabilitation SciencesDocument28 pagesBehavior Modification: Presented By: Wajeeha Iqbal BS in Psychology, MS (SLP/T) Riphah College of Rehabilitation Sciencesmazahir hussainNo ratings yet
- Standardization 1 PDFDocument7 pagesStandardization 1 PDFmazharul HasanNo ratings yet
- EcodesDocument2 pagesEcodesValentin IonutNo ratings yet
- Human Nutritional RequirementsDocument3 pagesHuman Nutritional RequirementsAgnesMagadiaNo ratings yet
- Mechanism of Enzyme ActionDocument19 pagesMechanism of Enzyme ActionRubi AnnNo ratings yet
- User Manual 4372070Document80 pagesUser Manual 4372070EDENILSON CORDEIRONo ratings yet
- JSA - Bolt TensioningDocument5 pagesJSA - Bolt TensioningRaju KhalifaNo ratings yet
- Financial Problems Are Commonly Faced by EveryoneDocument2 pagesFinancial Problems Are Commonly Faced by EveryoneGrace Ann Mancao PototNo ratings yet
- Grades 4-10: Search Jobs in IndiaDocument2 pagesGrades 4-10: Search Jobs in IndiaMD AKIL AHMEDNo ratings yet
- Lesson 3.3 Inside An AtomDocument42 pagesLesson 3.3 Inside An AtomReign CallosNo ratings yet
- ACRE2a Non Elementary Reaction Kinetics RevDocument53 pagesACRE2a Non Elementary Reaction Kinetics RevRathish RagooNo ratings yet
- Good Boys Go To Heaven, Bad Boys Go EverywhereDocument32 pagesGood Boys Go To Heaven, Bad Boys Go Everywherealcantaravic2006No ratings yet
- Owners Manual NCSP3CM (En)Document47 pagesOwners Manual NCSP3CM (En)yurii volNo ratings yet
- Plante BatteriesDocument16 pagesPlante Batteriessureshnfcl0% (1)
- Summary of Germ LayersDocument2 pagesSummary of Germ Layersaichiii.bearNo ratings yet
- GAD OrientationDocument58 pagesGAD OrientationKevin Dalangin100% (2)
- Gardobond 24d Imu Sds Ver1Document6 pagesGardobond 24d Imu Sds Ver1stuart3962No ratings yet
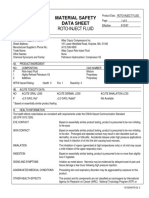
- Material Safety Data Sheet Roto-Inject FluidDocument5 pagesMaterial Safety Data Sheet Roto-Inject FluidQuintana JoseNo ratings yet
- DBM MonetizationDocument2 pagesDBM MonetizationrsdiamzNo ratings yet
- Polycystic Ovary Syndrome (PCOS) - Symptoms, Causes, and TreatmentDocument19 pagesPolycystic Ovary Syndrome (PCOS) - Symptoms, Causes, and TreatmentAkshay HarekarNo ratings yet
- Jurnal Kasus Etikolegal Dalam Praktik KebidananDocument13 pagesJurnal Kasus Etikolegal Dalam Praktik KebidananErni AnggieNo ratings yet