Professional Documents
Culture Documents
Improving Patient Safety in Radiotherapy by Learning From Near Misses, Incidents and Errors
Uploaded by
rosanaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Improving Patient Safety in Radiotherapy by Learning From Near Misses, Incidents and Errors
Uploaded by
rosanaCopyright:
Available Formats
The British Journal of Radiology, 80 (2007), 297–301
COMMENTARY
Improving patient safety in radiotherapy by learning from near
misses, incidents and errors
M V WILLIAMS, MD, FRCP, FRCR
Faculty of Clinical Oncology, The Royal College of Radiologists, 38 Portland Place, London W1B 1JQ, UK
ABSTRACT. Radiotherapy incidents involving a major overdose such as that which
affected a patient in Glasgow in 2006 are rare. The publicity surrounding this patient’s
treatment and the subsequent publication of the enquiry by the Scottish Executive
have led to a re-evaluation of procedures in many departments. However, other
incidents and near misses that might also generate learning are often surrounded by
obsessive secrecy. With the passage of time, even those incidents that have been
subject to a public enquiry are lost from view. Indeed, the report on the incident in
Glasgow draws attention to strong parallels with that in North Staffordshire, the report
of which is not freely available despite being in the public domain. A web-based system
to archive and make available previously published reports should be relatively simple
to establish. A greater challenge is to achieve open reporting of near misses, incidents
and errors. The key elements would be the effective use of keywords, a system of Received 13 January 2007
classification and a searchable anonymized database with free access. There should be Revised 26 February 2007
a well designed system for analysis, response and feedback. This would ensure the Accepted 9 March 2007
dissemination of learning. The development of a more open culture for reports under
DOI: 10.1259/bjr/29018029
the Ionising Radiation (Medical Exposure) Regulations (IR(ME)R) is essential: at the very
least, their main findings and recommendations should be routinely published. These ’ 2007 The British Institute of
changes should help us to achieve greater safety for our patients. Radiology
Radiotherapy is seen as a mysterious procedure by important to understand the fine detail of the mechan-
patients and the public alike. Treatments vary in their isms by which a latent error was established [10, 11]: a
intent, and in the number and size of fractions series of mistakes then resulted in the delivery of an
administered. Because radiation is involved and because incorrect treatment. As technology develops, there will
it can neither be seen nor felt, there is an air of mystery be new possibilities for mistakes, but the root cause
that adds to the perception of danger. usually lies not in the individual but in organizational
Staff recognize radiotherapy as a high risk procedure procedures, structure and governance [10–15]. These
because the process is complex and involves a large details and their continual review in the light of incidents
number of different steps and staff groups: each hand- and non-conformances are the key to safety [10, 14, 16].
over or data transfer offers the opportunity for mis-
communication and error. The risks are compounded
because radiotherapy is usually a repetitive procedure. Open reporting and the ‘‘no blame’’ culture
Treatment is administered as a series of fractions and
error can be perpetuated [1, 3–5]. Alternatively, a Open reporting of near misses, incidents and errors is
dosimetry or calculation error can affect a series of established as a key safety step in other high risk
patients [2, 6–9]. Despite this, radiotherapy has a good industries [12, 14]. Aviation has seen a dramatic fall in
safety record and patient injury caused by error is rare. the incidence of accidents over the last 30 years, and this
Several international organizations have reviewed has been attributed to the safety and reporting culture
major radiotherapy incidents [8, 9] and one might [14, 16]. Anaesthesia has made safety a priority and has
conclude that it is now difficult to invent a new error. replicated the achievements of aviation, significantly
Indeed, recently reported errors from Leeds [3–5] and reducing the risk of death from accidents [17]. Near
Glasgow [1] were repetitions of previous mistakes, misses do not have legal implications and thus there are
namely omission of a wedge compensator during fewer barriers to reporting. In addition, near misses are
treatment [8] incorporated when a computer treatment 3–300 times more common than adverse events and offer
planning system was introduced [2]. However, it is learning opportunities without patient injury [16].
However, medicine has lagged behind other industries
in establishing a safety culture [12, 14, 16]. Reducing risk
Address correspondence to: Dr Michael Williams, Faculty of Clinical
Oncology, The Royal College of Radiologists, 38 Portland Place, requires a determination to achieve improvement, open
London W1B 1JQ, UK. E-mail: michael-williams@rcr.ac.nhs.uk reporting and a ‘‘no blame’’ culture [14, 16–20]. It has
The British Journal of Radiology, May 2007 297
M V Williams
been observed that all reporting is in some sense should not be open to professional or even public
voluntary and that, to be effective, it needs to be linked scrutiny.
to a system for analysis, response and feedback [18].
For the NHS, these principles were enunciated in the
two publications ‘‘Organisation with a memory’’ [12] Reports under the Ionising Radiation (Medical
and its successor ‘‘Building a safer NHS for patients’’ Exposure) Regulations
[13], which led to the establishment of the National
Patient Safety Agency (NPSA). The difficulty for radio- In the UK, radiotherapy errors that result in a dose
therapy is that we are far removed from the ideal greater than intended are reportable to the inspectorate
solution that these reports describe. We are still locked under the Ionising Radiation (Medical Exposure)
into a ‘‘past’’ where attention focuses on individual Regulations (IR(ME)R) [23]. The regulations were laid
error, leading to scapegoating and fear of reprisals; before parliament to fulfil our obligations under a
adverse events are regarded as ‘‘one-offs’’, subject to a European Council directive [24]. This gave member
short-term fix; and other staff do not hear the outcome of states the responsibility for implementing a system of
investigations that are considered to be only relevant to inspection to enforce the provisions of the directive. In
the team involved [12]. We are still a long way from the particular, there is a requirement that:
‘‘future’’ where individuals are held accountable for
their actions within a system approach to hazards, Member states shall ensure that all reasonable steps to
blame-free reporting is encouraged with regular feed- reduce the probability and the magnitude of accidental
back, the potential for replication is recognized and or unintended dose of patients from radiological
lessons are disseminated to others [12]. practices are taken, economic and social factors being
There is still a strong blame culture: indeed, the report taken into account.
on the Glasgow incident devoted considerable effort to The main emphasis in accident prevention should be
apportioning blame to different individuals [1]; although on the equipment and procedures in radiotherapy, but
managerial failures were documented, there was little some attention should be paid to accidents with
emphasis on overall responsibility at a high level [1]. It diagnostic equipment. ((Article 11) [24])
has been argued that leaders should take personal
responsibility for the safety of the processes and systems One can draw two conclusions about the implementa-
in which individuals work if sustained improvement is tion of this directive through the IR(ME)R in the UK.
to be achieved [20]. First, there seems to be an inappropriate focus on very
small misexposures in diagnostic practice, which clearly
was not the intention of those drafting the directive.
Internal reporting of radiotherapy incidents Raising the reporting and external investigation thres-
and the NPSA hold for incidents to encompass only those carrying a
risk of carcinogenesis of greater than 1 in 10 000 has been
Radiotherapy departments in the UK are required to proposed [25]. Second, the wording ‘‘accidental or
have a quality management system [21] and, within this, unintended doses’’ includes both over- and underdoses,
quality assurance programmes specific to the various but only the former are reportable in the UK, despite the
processes are required, implicitly or explicitly, by UK major detriment that can follow an underdose [2, 7].
legislation. It is usual to seek accreditation by an outside Interestingly, despite the legal position, the new
body. Quality assurance systems require internal report- Healthcare Commission form permits the reporting of
ing and audit of incidents and non-conformances: such underdoses.
events are reviewed at weekly or monthly meetings. Enquiries under the Freedom of Information Act have
Trends can be identified and remedial action put in elicited the fact that over the last 6 years there have been
place. In England, these reports are fed into NHS Trust 211 radiotherapy incidents reported under the IR(ME)R
risk reporting systems and then forwarded to the NPSA, [26, 27]. The data do not include underdoses (which are
where they are anonymized and fed into a database held not reportable under these regulations) or overdoses that
on a separate server [22]. The difficulty with this were recoverable by revising the radiotherapy plan or
laudable system is that it contains some 50 000 oncology did not breach the reporting threshold. There is no public
incidents, half of which are trips, slips and falls. These or professional access to any of these data other than
are not usually informative about the radiotherapy under the Freedom of Information Act.
process and, although important to the patient and the Investigations under the IR(ME)R are conducted
hospital, are essentially a byproduct of collecting data under criminal law and usually under caution [1, 23].
through risk management systems. The database is not The results of the IR(ME)R investigations are therefore
searchable and there is no use of keywords. It may be confidential and are not disseminated unless unusual
difficult to deduce whether a dose error refers to a steps are taken. This is not a specified feature of the core
chemotherapy or a radiotherapy event. This may explain European legislation [24] as the details of the legislation,
why the NPSA stated that it possessed no data on any regulation and administrative provisions are a matter for
adverse incidents that could have been of assistance to each country (Article 14(1) of [24]). In Denmark, things
the panel reviewing the Leeds incident [4]. Only a single are very different: the Danish Act on Patient Safety came
clinical oncologist has access to the NPSA database, and into force on 1 January 2004 [28]. It obliges frontline
feedback mechanisms have yet to be established. If it is to personnel to report adverse events to a national system.
be useful in the future, these limitations need to be The purpose is to learn, not punish, and the act contains a
addressed: as it is anonymized, there is no reason why it paragraph protecting staff from sanctions: an individual
298 The British Journal of Radiology, May 2007
Improving patient safety in radiotherapy
who reports an adverse event cannot as a result of that Hospitals fear the public disclosure of reports that may
report be subjected to investigation or disciplinary action damage their reputation [31]. However, the media
by the employer, the Board of Health, or the Court of usually learn about embarrassing accidents from other
Justice [28]. Similar protection is offered in Australia and sources [31], and this occurred in the Leeds case when
New Zealand, and in other industries. In Denmark, the error was reported the in local press [4]; the article is
hospital owners are obliged to act on the reports, and the available on the internet [30]. Others have wrestled more
national Board of Health is obliged to communicate the effectively with the dilemma posed for a hospital by the
learning nationally. The punitive system adopted by public management of medical error [19]: at Sturdy
the UK was a matter of choice, made doubly strange by Memorial Hospital mistakes in prostate biopsy reporting
the earlier publication of ‘‘Organisation with a memory’’ were discovered, patients were notified and a review of
[12]. 6000 specimens was commissioned. There was little
support from professional bodies and a flurry of media
attention, but overall the experience was judged to have
Reports of inquiries into major incidents been positive and there was no impact on the hospital’s
workload or finances. Openness reaffirmed the hospital’s
Major incidents in which a patient comes to harm or reputation for putting patients first. Patients accepted the
where there is a system failure, such that a series of inevitability of human error and were impressed that
patients are exposed to risk, are investigated to deter- something was being done about it [19].
mine what went wrong. But it is also essential that the
results be made public and the lessons disseminated. The
Scottish Executive is to be congratulated for publishing International reporting systems
the report on the investigation into the unintended
overdose in Glasgow [1]. This action had a huge impact Lessons learned from the investigation of therapy
on the radiotherapy community in the UK and has misadministration events have been reported by the
certainly banished complacency. In contrast, in 2004 a United States Nuclear Regulatory Commission (NRC)
radiotherapy incident occurred in Leeds whereby a [32]. They reviewed seven events, involving radioiso-
patient received treatment to the breast without a wedge topes, investigated in 1991–92, and emphasised the
compensator in place for a series of 14 fractions [3, 4]. An importance of a comprehensive safety culture. The
alert was published by the Department of Health [5] and International Atomic Energy Agency (IAEA) has pub-
disseminated through the risk management system, lished a report on ‘‘Lessons learned from accidental
rather than directly to radiotherapy departments. The exposures in radiotherapy’’, reviewing 92 anonymized
document is striking for its brevity and it had little radiotherapy incidents together with a classification of
impact. This has been identified as a common failing of causes and recommendations on prevention [8]. The
such alerts [29]. The only report that has been published International Commission on Radiological Protection
deals with ‘‘involuntary automaticity’’, the psychological (ICRP) has published ‘‘Prevention of accidental expo-
mechanism proposed by the authors to explain the sures to patients undergoing radiation therapy’’, review-
repetitive error made by a series of staff members [3]. ing seven case histories of major large scale accidental
The issue of how the incorrect data were entered into the exposures [9]. Their main recommendations were for
treating linear accelerator in the first place was not quality assurance systems and a programme of in vivo
addressed at all. A full enquiry was commissioned by the dosimetry within departments [9]. A taxonomy of
radiation incidents has been proposed to support risk
Trust, but the report has been kept confidential. Access
analysis and organizational learning: 437 incidents from
under the Freedom of Information Act reveals that it
databases held by the NRC, the IAEA and the Radiation
contains significant recommendations for national prac-
Oncology Safety Information System (ROSIS) were
tice [27]; for example, on workload, training, working
reviewed and classified into systemic and sporadic,
practices, manual data transfer, checking procedures and
and by the process domain in which they occurred [33].
the replacement of outdated computer programs [4]. It is
The reporting of adverse events in healthcare has been
very disheartening that the Trust that commissioned it
reviewed by Leape [31]. He argues that to be effective it
has not seen fit to publish the report. However, this
is necessary to mimic the aviation safety system so that
behaviour is inkeeping with the findings of the Leeds
reporting is simple, safe (for the reporter) and worth-
report itself, which states that:
while. Successful reporting systems are non-punitive,
confidential, independent, timely, responsive and subject
Very little information seems to be collected or to expert analysis [31]. Recommendations should focus
publicly shared on radiotherapy adverse events either on changes in systems, processes or products rather than
nationally or internationally. Indeed keeping such on individual performance [31]. Both the IAEA and ICRP
information confidential seems to take a higher reports draw attention to the virtues of the open
priority than finding a way to use it to prevent similar reporting systems in aviation [8, 9] and the desirability
accidents from taking place. [4] of anonymous reporting and dissemination to the wider
community [8]. Nevertheless, there is no such compre-
There are a large number of other serious incidents hensive system in the UK or elsewhere. The nearest
that have been identified under the Freedom of approximation is ROSIS, which was established in 2001
Information Act and published both in the press [26] with pump-priming funds from the European Society for
and on websites [30]. For the most part, these have not Therapeutic Radiology and Oncology (ESTRO). It is a
been fed back to other departments in an effective way. voluntary reporting system that now holds on its website
The British Journal of Radiology, May 2007 299
M V Williams
over 700 incidents from 37 departments across 19 the Health Protection Agency, working with the professions
countries [34]. The data are anonymized, made fully involved in radiotherapy delivery to provide specialist
searchable and are in the public domain. Details of expertise. Detailed investigation of selected near misses and
incidents and their causes are given in an abbreviated other incidents that are not statutorily reportable would
form, and it is not possible to analyse them in detail. maximize learning. The results must then be linked to an
In response to reports of harm to patients caused by effective system of dissemination that would reassure staff
radiotherapy, a new initiative has been launched by the that reporting is worthwhile.
World Health Organization World Alliance for Patient Third, the development of a more open culture for
Safety [35, 36]. There are two primary issues of concern. reports under the IR(ME)R is essential. Since 1 November
First, can a set of standardized safety interventions be 2006, the Healthcare Commission has been the responsible
developed to reduce harm to patients? Second, can authority; this change may provide the opportunity for
lessons from errors be translated into international greater openness. The Scottish Executive has already
learning? A timely and worldwide response to safety shown that reports initiated under these regulations can
incidents has been achieved in aviation but not in be published. The Healthcare Commission’s vision is ‘‘to
medicine [37]. One of the aims of the World Alliance make a difference to the delivery and quality of healthcare
for Patient Safety is that the learning from the inad- by inspecting, informing and improving’’. To fulfil their
vertent death of a patient in a hospital in one country informing role, they should routinely publish the results of
could save the lives of many others around the world enquires under the IR(ME)R. This would be consistent
[37]. with their policy on the reports of other investigations and
would help to ensure that errors are not repeated
elsewhere. This could be facilitated by establishing a
Recommendations website to host anonymized reports of enquiries, or at the
very least their main findings and recommendations.
First, learning from the past should be consolidated by In conclusion, if these objectives could be achieved,
setting up a publicly available website to hold copies of then the UK could become a world leader in reporting
the reports of previous radiotherapy incident enquiries. and learning from radiotherapy incidents. This should
This should help to ensure that the learning from them is improve the safety of our patients and would take us a
not forgotten. In the UK alone, there have been a number step nearer to passing the ‘‘orange wire test’’, whereby a
of public enquiries about radiotherapy incidents that safety incident results in a rapid worldwide response as
affected a series of patients. These include those at Exeter in aviation [37].
[6] and North Staffordshire [2]. These are in the public
domain, but the incident at Glasgow showed us that very
similar errors can still occur [1].
References
Second, dissemination of learning from near misses 1. Scottish Executive Publications. Report into unintended
and non-reportable incidents should be improved. This overexposure of Lisa Norris at Beatson Oncology Centre,
could be achieved by changing the way in which the Glasgow in January 2006. Report of an investigation by the
NPSA database works and by providing effective inspector appointed by the Scottish Ministers under
analysis and feedback [18]. At present, radiotherapy Ionising Radiation (Medical Exposures) Regulations -
IRMER. October 2006. Available from: http://www.
incidents are submitted internally and then sent to a
scotland.gov.uk/Publications/2006/10/27084909/0.
central server where they are anonymized [22]; no 2. Baldwin Report. Report of an investigation into the conduct
analysis has been published. Lack of feedback was one of isocentric radiotherapy at the North Staffordshire Royal
of several criticisms made by the National Audit Office Infirmary between 1982 and 1991. Birmingham, West
[29], and the Department of Health has responded with a Midlands Health Authority. First report, August 1992.
plan to remedy the deficiencies [38]. The NPSA system as Second report, March 1994.
it applies to radiotherapy could be improved if a 3. Toft B, Mascie-Taylor H. Involuntary automaticity: a work
classification of radiotherapy incidents could be agreed system induced risk to safe healthcare. Health Serv Manage
and if reports included: Res 2005;18:211–16.
4. Independent review of the circumstances surrounding a
serious adverse incident that occurred in the Cookridge
N Agreed key words
Hospital. [Redacted copy obtained under the Freedom of
N A description of how the error occurred Information Act.]
N Identification of how the error was detected 5. Department of Health. DH Alert 4181. Safe delivery of
N Patient outcome and corrective action taken radiotherapy treatment. 19 November 2004. Available from:
N Lessons to be learnt http://www.dh.gov.uk/en/index.htm.
N Free text for further comments. 6. Report of the Committee of Inquiry into the incident in the
radiotherapy department. Exeter, UK: Exeter Health
The Royal College of Radiologists has established a Authority, 1988.
multidisciplinary working party whose remit includes these 7. BBC News. Hospital admits cancer mistakes. Plymouth
Hospital NHS Trust, 7 January 2002. Available from:
issues; it will also make recommendations on error
http://news.bbc.co.uk/1/hi/england/1746774.stm.
prevention and detection. The report will be completed by 8. International Atomic Energy Agency. Lessons learned from
the end of 2007 and should provide the basis for developing accidental exposures in radiotherapy. Safety reports series
an open reporting system for radiotherapy incidents. We no. 17. Vienna, Austria: International Atomic Energy
hope to work with the NPSA to achieve this objective. In Agency, 2000.
addition, it is hoped that full analysis of these complex 9. Valentin J, editor. International Commission on
incidents could be assisted by support services provided by Radiological Protection. Prevention of accidental exposures
300 The British Journal of Radiology, May 2007
Improving patient safety in radiotherapy
to patients undergoing radiation therapy. ICRP publication radiation in relation to medical exposure, and repealing
86. Oxford, UK: Elsevier Science, 2001. directive 84/466/Euratom. Available from: http://
10. Helmreich RL. On error management: lessons from avia- www.bnsa.bas.bg/eurolex/31997L0043_en.pdf.
tion. Br Med J 2000;320:781–5. 25. Clewer PR, Jackson PC. Reporting overexposures and
11. Reason J. Human error: models and managements. Br Med unintended exposures in diagnostic procedures. Br J
J 2000;320:768–70. Radiol 2006;79:866–9.
12. Department of Health. An organisation with a memory. 26. Lois Rogers. Over 200 hurt or killed by botched radiation.
Report of an expert group on learning from adverse events in Sunday Times. London, UK: Times Newspapers Ltd. 30
the NHS chaired by the Chief Medical Officer. London, UK: April 2006.
Stationery Office, 2000. Available from: http://www.dh.gov. 27. Tylko K, Blennerhassett M. How the NHS could better
uk/assetRoot/04/08/89/48/04088948.pdf. protect the safety of radiotherapy patients. Health Care Risk
13. Department of Health. Building a safer NHS for patients – Rep 2006;12:18–19.
implementing an organisation with a memory. London, UK: 28. Act on patient safety in the Danish health care system. Act
Stationery Office, 2001. Available from: http://www.dh.gov. No. 429 of 10/6/2003 (current). Available from: http://
uk/assetRoot/04/05/80/94/04058094.pdf. www.patientsikkerhed.dk/admin/media/pdf/133907
14. Vincent C. Patient safety. London, UK: Elsevier, 2006. d0940e4d5f751852ec8f6b1795.pdf.
15. Williams MV. Radiotherapy near misses, incidents and 29. National Audit Office. A safer place for patients: learning to
errors: radiotherapy incident at Glasgow. Clin Oncol improve patient safety. London, The Stationery Office, 2005.
2007;90:1–3. Available from: http://www.nao.org.uk/publications/
16. Barach P, Small SD. Reporting and preventing medical nao_reports/05-06/0506456.pdf.
mishaps: lessons from non-medical near miss reporting
30. ‘‘Radiotherapy Damaged Me’’ website. http://www.
systems. Br Med J 2000;320:759–63.
radiotherapydamaged.me.uk/newspapers.htm.
17. Gaba M. Anaesthesiology as a model for patient safety in
31. Leape LL. Reporting of adverse events. N Engl J Med
health care. Br Med J 2000;320:785–8.
2002;347:1633–8.
18. Cohen MR. Why error reporting systems should be
32. Ostrom LT, Rathbun P, Cumberlin R, Horton J, Gastorf R,
voluntary. They provide better information for reducing
errors. Br Med J 2000;320:728–9. Leahy TJ. Lessons learned from investigations of therapy
19. Pietro DA, Shyavitz LJ, Smith RA, Auerbach BS. Detecting misadministration events. Int J Radiat Oncol Biol Phys
and reporting medical errors: why the dilemma? Br Med J 1996;34:227–34.
2000;320:794–6. 33. Ekaette EU, Lee RC, Cooke DL, Kelly K-L, Dunscombe PB.
20. Reinertsen JL. Let’s talk about error. Br Med J 2000;320:730. Risk analysis in radiation treatment: application of a new
21. Bleehen Report. Quality assurance in radiotherapy: a taxonomic structure. Radiother Oncol 2006;80:282–7.
quality management system for radiotherapy. PL/CMO 34. Radiation Oncology Safety Information System (ROSIS).
(94).7. London, UK: Department of Health, 1994. Available from: http://www.clin.radfys.lu.se/default.asp.
22. National Patient Safety Agency. Building a memory: 35. Donaldson L. Reducing harm from radiotherapy. Br Med J
preventing harm, reducing risks and improving patient 2007;334:272.
safety. The first report of the National Reporting and 36. World Health Organization. Patient Safety: harm to patients
Learning System and the Patient Safety Observatory. NPSA, caused by radiotherapy. Available from: http://www.
July 2005. Available from: http://www.npsa.nhs.uk/site/ who.int/patientsafety/activities/technical/radiotherapy/
media/documents/1269_PSO_Report_FINAL.pdf. en/index.html.
23. Department of Health, The Ionising Radiation (Medical 37. Donaldson L. When will health care pass the orange-wire
Exposure) Regulations 2000. London, UK: Department of test? Lancet 2004;364:1567–8.
Health, 2001. Available from: http://www.opsi.gov.uk/si/ 38. Department of Health. Safety first. A report for patients,
si2000/20001059.htm. clinicians and healthcare managers. London, UK: The
24. Council Directive 97/43/Euratom of 30 June 1997 on health Stationery Office, 2006. Available from: http://www.dh.
protection of individuals against the dangers of ionizing gov.uk/assetRoot/04/14/14/41/04141441.pdf
The British Journal of Radiology, May 2007 301
You might also like
- Accidents in Radiotherapy: Xa9846624 Lack of Quality Assurance?Document16 pagesAccidents in Radiotherapy: Xa9846624 Lack of Quality Assurance?PartyNowNo ratings yet
- Bmri2014 392596Document7 pagesBmri2014 392596Gaby ValenzuelaNo ratings yet
- Radiological Error: Analysis, Standard Setting, Targeted Instruction and TeamworkingDocument8 pagesRadiological Error: Analysis, Standard Setting, Targeted Instruction and TeamworkingJaclyn Naranjo VillarroelNo ratings yet
- Radiation Oncology Patient Safety FinalDocument4 pagesRadiation Oncology Patient Safety Finalapi-645453685No ratings yet
- Use of Contrast Media in Diagnostic Imaging: Medico Legal ConsiderationsDocument8 pagesUse of Contrast Media in Diagnostic Imaging: Medico Legal Considerationscrisvbarros8865No ratings yet
- Radiation Safety For General Public WordDocument5 pagesRadiation Safety For General Public Wordapi-527782385No ratings yet
- Safety Measures in Radiation OncologyDocument4 pagesSafety Measures in Radiation Oncologyapi-695939591No ratings yet
- Dos 516 Radiation Safety PaperDocument4 pagesDos 516 Radiation Safety Paperapi-530270156No ratings yet
- Critical Incident Reporting and Learning: Key PointsDocument7 pagesCritical Incident Reporting and Learning: Key PointsRavikiran SuryanarayanamurthyNo ratings yet
- Mckane Radsafety PaperDocument4 pagesMckane Radsafety Paperapi-569589889No ratings yet
- Shahad Al-Ward Radiation Safety PaperDocument3 pagesShahad Al-Ward Radiation Safety Paperapi-691667702No ratings yet
- Radiation Safety PaperDocument4 pagesRadiation Safety Paperapi-633102425No ratings yet
- Minimally Invasive Urologic Surgery Is Safe During COVID 19: Experience From Two High Volume Centers in ItalyDocument3 pagesMinimally Invasive Urologic Surgery Is Safe During COVID 19: Experience From Two High Volume Centers in ItalyMasrun FatanahNo ratings yet
- Final Draft-Muna 1Document4 pagesFinal Draft-Muna 1api-693187588No ratings yet
- Near-Miss Incident Management Framework in Chemical IndustryDocument15 pagesNear-Miss Incident Management Framework in Chemical Industrychujiyo100% (1)
- Medical RadiationDocument5 pagesMedical RadiationNadeem NadeemNo ratings yet
- Critical Incidence Reporting & Learning PDFDocument7 pagesCritical Incidence Reporting & Learning PDFNenny Puji LestariNo ratings yet
- Radiation SafetyDocument4 pagesRadiation Safetyapi-696520673No ratings yet
- Optimization in Radiology Eur J Med PhysDocument6 pagesOptimization in Radiology Eur J Med PhysobbebbiNo ratings yet
- IAEA Actions to Protect Patients from Radiation in Medical ProceduresDocument8 pagesIAEA Actions to Protect Patients from Radiation in Medical ProceduresSimu JemwaNo ratings yet
- Can Incident Reporting Improve Safety? Healthcare Practitioners ' Views of The Effectiveness of Incident ReportingDocument10 pagesCan Incident Reporting Improve Safety? Healthcare Practitioners ' Views of The Effectiveness of Incident ReportingsatmayaniNo ratings yet
- Current Issues and Actions in Radiation Protection of PatientsDocument5 pagesCurrent Issues and Actions in Radiation Protection of PatientsSusryandini NovraswindaNo ratings yet
- Radiation Safety Paper - Copy 1Document4 pagesRadiation Safety Paper - Copy 1api-693382622No ratings yet
- The Lessons To Be Learned From Incidents and AccidentsDocument15 pagesThe Lessons To Be Learned From Incidents and Accidentsabdulaziz saadNo ratings yet
- UC Davis: Dermatology Online JournalDocument8 pagesUC Davis: Dermatology Online JournalANo ratings yet
- The Problem With Incident ReportingDocument5 pagesThe Problem With Incident ReportingSusy SuwantiNo ratings yet
- Radiation Safety PaperDocument3 pagesRadiation Safety Paperapi-635186395No ratings yet
- Protection From RadiationDocument8 pagesProtection From Radiationapi-270822363No ratings yet
- Implementation Fidelity of A Nurse-Led Falls Prevention Program in Acute Hospitals During The 6-PACK TrialDocument10 pagesImplementation Fidelity of A Nurse-Led Falls Prevention Program in Acute Hospitals During The 6-PACK TrialDedes SahpitraNo ratings yet
- Clinical Risk Management For Anaesthetists - CeaDocument6 pagesClinical Risk Management For Anaesthetists - CeaLucas CabreraNo ratings yet
- Radiation SafetyDocument4 pagesRadiation Safetybraith7811No ratings yet
- Prevention of Ventilator-Associated Pneumonia in Intensive Care Units: An International Online SurveyDocument8 pagesPrevention of Ventilator-Associated Pneumonia in Intensive Care Units: An International Online SurveymochkurniawanNo ratings yet
- Roils 1Document4 pagesRoils 1api-574059920No ratings yet
- Clinical Risk ManagementDocument6 pagesClinical Risk ManagementJaparaj PeterNo ratings yet
- Complications and Failure of Airway ManagementDocument18 pagesComplications and Failure of Airway ManagementRilano UmbohNo ratings yet
- Radiationsafety by StaceysongDocument3 pagesRadiationsafety by Staceysongapi-634067897No ratings yet
- BJR 20219004Document4 pagesBJR 20219004Camilo SotomayorNo ratings yet
- Week2 Submitter PaperDocument3 pagesWeek2 Submitter Paperapi-299189797No ratings yet
- Patient Safety Thesis PDFDocument6 pagesPatient Safety Thesis PDFasiagroverprovo100% (2)
- Mitigating Isolation Study 2021.12.23.21268326v1.fullDocument10 pagesMitigating Isolation Study 2021.12.23.21268326v1.fullmart0830No ratings yet
- Radiation Safety Literature Review - 121123Document5 pagesRadiation Safety Literature Review - 121123api-693335992No ratings yet
- Radiation Safety Paper - Kristen DezellDocument4 pagesRadiation Safety Paper - Kristen Dezellapi-568316609No ratings yet
- Danger Points, Complications and Medico-Legal Aspects in Endoscopic Sinus SurgeryDocument61 pagesDanger Points, Complications and Medico-Legal Aspects in Endoscopic Sinus SurgeryMyrellaAlexandraNo ratings yet
- Icrp 104Document104 pagesIcrp 104herbert domingoNo ratings yet
- Trichiasis Surgery: Rapid AssessmentDocument2 pagesTrichiasis Surgery: Rapid AssessmentShella JamilahNo ratings yet
- Communicating Benefit and Risk To Patients Under IrmerDocument19 pagesCommunicating Benefit and Risk To Patients Under IrmerNiero VillaNo ratings yet
- Tele 2Document10 pagesTele 2Sajin AlexanderNo ratings yet
- Barriers To Ultrasound GuidanceDocument9 pagesBarriers To Ultrasound GuidanceHarm ScholtenNo ratings yet
- Patient Safety in Medical ImagingDocument13 pagesPatient Safety in Medical ImagingC JoanesNo ratings yet
- Patient Shielding Guidance Executive SummaryDocument1 pagePatient Shielding Guidance Executive SummaryPrabinNo ratings yet
- AnnThoracMed93134-4810599 132145Document4 pagesAnnThoracMed93134-4810599 132145Mihaela-Alexandra PopNo ratings yet
- Radiation Safety Paper - 1Document3 pagesRadiation Safety Paper - 1api-270166579No ratings yet
- Reducing Risks, Protecting People - A Harmonised ApproachDocument6 pagesReducing Risks, Protecting People - A Harmonised ApproachSANDEEP KUMARNo ratings yet
- Artigo - Crew Resource Management in The ICUDocument5 pagesArtigo - Crew Resource Management in The ICUorquidia jaquimNo ratings yet
- Rad SafetyDocument5 pagesRad Safetyapi-336647605No ratings yet
- MDL 111 269Document16 pagesMDL 111 269Rizka SuhartiniNo ratings yet
- The Measurement and Monitoring of SafetyDocument92 pagesThe Measurement and Monitoring of SafetycicaklomenNo ratings yet
- Safety Within The Field of Radiation TherapyDocument3 pagesSafety Within The Field of Radiation Therapyapi-694839765No ratings yet
- 680 FullDocument9 pages680 FullRye CalderonNo ratings yet
- Attribution of Radiation Health Effects and Inference of Radiation Risks: Considerations for Application of the IAEA Safety StandardsFrom EverandAttribution of Radiation Health Effects and Inference of Radiation Risks: Considerations for Application of the IAEA Safety StandardsNo ratings yet
- Scientific American explores what makes humans uniqueDocument1 pageScientific American explores what makes humans uniquerosanaNo ratings yet
- ASTM STP-1354. Evolution of Dislocation and Precipitate Structure in ZR Alloys Under Long-Term IrradiationDocument17 pagesASTM STP-1354. Evolution of Dislocation and Precipitate Structure in ZR Alloys Under Long-Term IrradiationrosanaNo ratings yet
- Astm E32Document5 pagesAstm E32rosana0% (1)
- Astm-E 1558-09Document13 pagesAstm-E 1558-09rosanaNo ratings yet
- ASTM-D 5144 - 08. Standard Guide For Use of Protective Coating Standards in Nuclear Power PlantsDocument6 pagesASTM-D 5144 - 08. Standard Guide For Use of Protective Coating Standards in Nuclear Power Plantsrosana100% (2)
- 1583rd Conference. Sustainable Energies 2018Document14 pages1583rd Conference. Sustainable Energies 2018rosanaNo ratings yet
- A Method To Reduce Space-Time Effects inDocument16 pagesA Method To Reduce Space-Time Effects inrosanaNo ratings yet
- Chemical Characterization of Large Size Archaeological Clay Bricks For Grouping Study by Internal Mono-Standard Neutron Activation AnalysisDocument7 pagesChemical Characterization of Large Size Archaeological Clay Bricks For Grouping Study by Internal Mono-Standard Neutron Activation AnalysisrosanaNo ratings yet
- Development and Standardization of Cyst Based Liquid Formulation of Azospirillum BioinoculantDocument11 pagesDevelopment and Standardization of Cyst Based Liquid Formulation of Azospirillum BioinoculantrosanaNo ratings yet
- A Retrospective Cohort Study of Cancer Incidence Among Patients Treated With RadiosynoviorthesisDocument5 pagesA Retrospective Cohort Study of Cancer Incidence Among Patients Treated With RadiosynoviorthesisrosanaNo ratings yet
- Groundwater Recharge Estimation Methods for the Azul AquiferDocument4 pagesGroundwater Recharge Estimation Methods for the Azul AquiferrosanaNo ratings yet
- Major Incidents and Mass Casualty EventsDocument99 pagesMajor Incidents and Mass Casualty EventsJose Damian Cortes FernandezNo ratings yet
- Modern Management of Anal FistulaDocument11 pagesModern Management of Anal FistulaMayerlin CalvacheNo ratings yet
- Occlusal Contacts RetentionDocument9 pagesOcclusal Contacts RetentionRockey ShrivastavaNo ratings yet
- Nursing Process For Bipolar DisorderDocument37 pagesNursing Process For Bipolar DisorderDENVER CABADINNo ratings yet
- Colorectal Cancer Case StudyDocument1 pageColorectal Cancer Case StudyNur'aini Elita PutriNo ratings yet
- 01 A History of The Pharmaceutical IndustryDocument8 pages01 A History of The Pharmaceutical IndustryHayat NaqviNo ratings yet
- FDA narrative requirements for adverse event reportsDocument12 pagesFDA narrative requirements for adverse event reportskandulasatish100% (3)
- Understanding M. tuberculosis Morphology, Diagnosis and PropertiesDocument17 pagesUnderstanding M. tuberculosis Morphology, Diagnosis and Propertiesيارا المزيدNo ratings yet
- Assessing The Nails: Return Demonstration Tool Evaluation ForDocument2 pagesAssessing The Nails: Return Demonstration Tool Evaluation ForAlexandra DelizoNo ratings yet
- Literature Review Total Knee ReplacementDocument8 pagesLiterature Review Total Knee Replacementgvym06g6100% (1)
- NURSING CARE PLAN RealDocument3 pagesNURSING CARE PLAN RealJorossMabantaMarayanNo ratings yet
- T3 Short Implant Surgical Manual: Preservation by DesignDocument20 pagesT3 Short Implant Surgical Manual: Preservation by DesignMarco BarrosoNo ratings yet
- Lumbosacral Plexus # 6Document6 pagesLumbosacral Plexus # 6Arcel De Luca G.No ratings yet
- POC CHWO HW Solutions PDFDocument5 pagesPOC CHWO HW Solutions PDFakashkr619No ratings yet
- Unit 2 Mental Health AssessmentDocument60 pagesUnit 2 Mental Health AssessmentSuhana ShresthaNo ratings yet
- Bag-Mask Ventillation PDFDocument6 pagesBag-Mask Ventillation PDFHaris PapadopoulosNo ratings yet
- Cardiac Hepatopathy A Review of Liver Dysfunction in Heart Failure LROJ 1 101Document26 pagesCardiac Hepatopathy A Review of Liver Dysfunction in Heart Failure LROJ 1 101bagasNo ratings yet
- Essay LPDP English Study PlanDocument2 pagesEssay LPDP English Study PlanCindy BriaNo ratings yet
- Pediatrics QuestionsDocument22 pagesPediatrics QuestionsShaik AmreenNo ratings yet
- IPCR Form - Mos'Document2 pagesIPCR Form - Mos'Jay-Ann AlcideraNo ratings yet
- 4 - Drug Product Design ParametersDocument7 pages4 - Drug Product Design ParametersVinz AlvarezNo ratings yet
- The Geriatric Anxiety Inventory in Primary CareDocument4 pagesThe Geriatric Anxiety Inventory in Primary CareYudistiro Adi NugrohoNo ratings yet
- ITLS Patient EvaluationDocument15 pagesITLS Patient Evaluationjoepz1982100% (1)
- Aloe Vera as an Alternative Treatment for Wound HealingDocument5 pagesAloe Vera as an Alternative Treatment for Wound HealingJeffllanoNo ratings yet
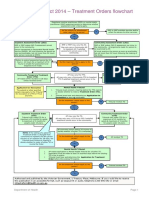
- Flowchart - Mental Health Act Treatment OrderDocument1 pageFlowchart - Mental Health Act Treatment OrderEdwin100% (1)
- Katz Activities of Daily LivingDocument2 pagesKatz Activities of Daily LivingGLORY MI SHANLEY CARUMBANo ratings yet
- Communicable Diseases 1Document12 pagesCommunicable Diseases 1Kristian Jane de JesusNo ratings yet
- Acne or Rosacea Infographic PDFDocument1 pageAcne or Rosacea Infographic PDFHegde sharma100% (1)
- Science 2013 Couzin Frankel 68 9Document2 pagesScience 2013 Couzin Frankel 68 9Ricardo ChavarriaNo ratings yet
- Critical Incident Reporting and Learning: Key PointsDocument7 pagesCritical Incident Reporting and Learning: Key PointsRavikiran SuryanarayanamurthyNo ratings yet