Professional Documents
Culture Documents
Missed Monteggia FX
Uploaded by
Eric RothOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Missed Monteggia FX
Uploaded by
Eric RothCopyright:
Available Formats
|
Missed Pediatric Monteggia Fractures
James Hubbard, MD Abstract
» Careful scrutiny of radiographs is important in the assessment of
Aakash Chauhan, MD, MBA
pediatric elbow injuries. Disruption of the radiocapitellar line and an
Ryan Fitzgerald, MD increased bow of the posterior ulnar border are sometimes subtle
signs of a Monteggia injury.
Reid Abrams, MD
Scott Mubarak, MD » An attempt at closed reduction up to 4 weeks after injury has been
cited in the literature as successfully treating some missed injuries.
Mark Sangimino, MD
» Operative reduction of chronic radial-head dislocation provides good
to excellent range of motion and functional outcome in the setting of
Investigation performed at the Division irreducible chronic radial-head dislocation.
of Hand, Upper Extremity, and
Microvascular Surgery, Department of » Ulnar osteotomy and correction of the ulnar deformity component of
Orthopaedic Surgery, University of the missed Monteggia injury are the key to indirect anatomic
California, San Diego (UCSD), San reduction of the radiocapitellar joint.
Diego, California
» Supplemental procedures aimed at increasing the stability of the
radiocapitellar joint (e.g., annular ligament reconstruction, radiocapitellar
Kirschner wire fixation, radioulnar Kirschner wire fixation) should be
directed by a thorough assessment of radiocapitellar stability following
ulnar osteotomy and correction of the ulnar deformity.
Background and Epidemiology scenario, exposing the patient to potential
F
irst described by Giovanni morbidity and increasing the complexity of
Monteggia in 1814, the epony- management for the treating surgeon as early
mous Monteggia lesion as 2 weeks after the initial injury. Morbidity
describes a fracture of the ulna is primarily associated with persistent dislo-
associated with dislocation of the radio- cation of the radioulnar and radiocapitellar
capitellar joint and disruption of the prox- joints and includes restricted elbow motion,
imal radioulnar joint1. These are rare particularly in flexion and pronation7, pro-
injuries in children, constituting ,1% of gressive valgus deformity and valgus insta-
all pediatric forearm fractures with an bility8, pain, degenerative arthritis9, and
annual incidence of ,1:100,0002. When tardy ulnar and radial nerve palsies10-12.
the Monteggia lesion is identified in the
acute setting and is treated with stable Anatomy
anatomic reduction of the ulna and radio- The elbow consists of 3 articulations: the
capitellar joint, long-term outcomes are ulnohumeral joint, the radiocapitellar
generally excellent1,3,4. However, 16% to joint, and the proximal radioulnar joint.
50% of these injuries are missed at initial The annular ligament and the quadrate
presentation, with reasons cited being ligament are the primary static stabilizers of
inadequate radiographs, subtle greenstick the proximal radioulnar joint. Other liga-
fractures of the ulna, and the complexity of mentous structures that play an ancillary
evaluating the pediatric elbow with its role in stability of the proximal radioulnar
multiple ossification centers3-6. A missed joint include the oblique cord (or Weit-
diagnosis presents a challenging clinical brecht ligament), present in 52.6% of
COPYRIGHT © 2018 BY THE Disclosure: There was no source of external funding for this study. The Disclosure of Potential
JOURNAL OF BONE AND JOINT Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/
SURGERY, INCORPORATED JBJSREV/A344).
JBJS REVIEWS 2018;6(6):e2 · http://dx.doi.org/10.2106/JBJS.RVW.17.00116 1
| Missed Pediat r ic Monteg g ia Fractures
forearms, which originates just distal to
the radial notch on the ulna and inserts TABLE I The Letts Classification for Pediatric Monteggia Injuries
and the Bado Classification for Monteggia Injuries
distal to the bicipital tuberosity on the
radius13, and the interosseous mem- Classification Description
brane originating on the radial aspect of
Letts classification
the ulna and inserting on the ulnar
Type A* Anterior radial-head dislocation and apex-anterior
aspect of the radius. These structures plastic ulnar deformation
are most taut in supination as a function Type B* Anterior radial-head dislocation and apex-anterior
of the shape of the radial head and the greenstick ulnar fracture
bow of the radius. The radial head is Type C* Anterior radial-head dislocation and complete ulnar
elliptical in axial cross-section, with the fracture
long axis of the ellipse perpendicular to Type D† Similar to Bado type II
the radial notch of the ulna in supina- Type E‡ Lateral radial-head dislocation and greenstick
tion14. This functions to maximally fracture of ulna
tension the annular ligament as well as Bado classification
the thick anterior portion of the quad- Type I* Anterior radial-head dislocation and apex anterior
rate ligament in supination. ulnar fracture
Type II† Posterior radial-head dislocation and apex posterior
Classification and Mechanism ulnar fracture
of Injury Type III‡ Lateral radial-head dislocation and apex lateral
ulnar fracture
The Bado classification of Monteggia
Type IV§ Dislocation of radial head in any direction and ulnar
fracture-dislocations is the most com- and radial-shaft fractures
monly used and describes 4 types of
ulnar fracture patterns with the associ- *Letts types A, B, and C represent Bado type-I pattern injuries with anterior dis-
ated direction of radial-head disloca- location of the radial head and increasing degrees of completeness of the ulnar
fracture. †Letts type-D injuries represent the classical Bado type-II pattern. ‡Letts
tion4 (Table I). Type-I injuries are the type-E lesions represent Bado type-III injuries with a greenstick fracture rather than
most common fracture-dislocation pat- a compete fracture of the ulna. §Bado type-IV injuries do not have a corresponding
tern seen in children, representing 75% type in the Letts classification.
of acute pediatric Monteggia injuries15.
Accordingly, type-I lesions represent
approximately 85% of pediatric Mon- falling patient and subsequently fails are resultant of a hyperpronation
teggia lesions in case series describing anteriorly in tension with the fracture mechanism4.
chronic missed injuries7,9,11,12,16-35. propagating in shear, resulting in the Letts et al. subsequently adapted the
Predictably, the mechanism of classical apex-anterior short-oblique Bado classification with a system more
injury varies with the direction of frac- fracture of the ulna seen in Bado type-I specific to pediatric injuries, describing 5
ture and dislocation. There are several injuries. Type-II injuries are proposed fracture patterns, types A to E37 (Table I).
proposed mechanisms by which type-I to be the result of a fall onto an out- Importantly, their classification recog-
lesions are produced, with the most stretched hand with the elbow in nizes the tendency of pediatric long bone
accepted being the hyperextension approximately 60° of flexion. This injuries to result in plastic deformation
theory proposed by Tompkins36. He results in longitudinal loading of the rather than complete fracture as seen in
proposed that type-I injuries likely forearm parallel to the long axis of the the adult population and identifies radial-
result from a patient falling with for- radius and ulna, and subsequent pos- head dislocation in the absence of a
ward momentum onto an outstretched terior dislocation of the elbow or, if the complete ulnar fracture as representing a
arm resulting in hyperextension of the ulna is weaker than the surrounding Monteggia equivalent. It has subse-
elbow. This hyperextension produces capsuloligamentous structures, a Bado quently been recognized that a truly iso-
reflexive contracture of the biceps bra- type-II injury15. Type-III injuries are lated traumatic radial-head dislocation is
chii, resulting in anterior dislocation of thought to result from a forced varus likely an exceedingly rare injury and that,
the radial head. The radius normally stress resulting in failure of the proximal on close inspection, one can usually
bears 80% of the load transmitted part of the ulna in varus and lateral or identify an ulnar injury in even the most
through the carpus to the forearm, and anterolateral dislocation of the radial subtle cases38.
when the radial head dislocates, the head15. Type-IV injuries have little
ulna becomes the primary load-bearing description of mechanism of injury in Natural History
structure in the forearm. The ulna is not the literature; however, in Bado’s initial The natural history of Monteggia injuries
equipped to bear the full weight of the description, he hypothesized that they is largely secondary to chronic radial-head
2 JUNE 2018 · VOLUME 6, ISSUE 6 · e2
Missed Pediatr ic Monteg gia Fractures |
dislocation, as the ulnar component of the may present as early as 3 months after Diagnosis
fracture will commonly heal and remodel radial-head dislocation39. Patients may present with a history of
as the child ages. With the initial disloca- With the loss of the radiocapitellar remote elbow injury, persistent pain,
tion of the radial head, the annular liga- articulation, the elbow loses approxi- decreased elbow motion, limited func-
ment and associated anterior capsular mately 33% of its valgus stability42, and tion, a fullness in the antecubital
structures fall posterior to the radial patients demonstrate instability and an space26, and, rarely, progressive cubitus
head and into the radiocapitellar joint, increase in the valgus carrying angle of the valgus deformity. An examination of the
calcifying over time and providing a elbow39. This has been reported to con- full range of motion at the elbow
block to anatomic reduction39,40. With tribute to late ulnar nerve palsy in rare including flexion, extension, pronation,
longer durations of radial-head dislo- cases43. Tardy median and posterior and supination should be undertaken as
cation, the radial head, capitellum, and interosseous nerve palsies have also been these patients often present with limited
radial notch of the ulna have been noted described secondary to tenting of the range of motion15. A full distal neuro-
to undergo dysplastic changes3,39-41. nerve over the dislocated radial head10,43. vascular examination should also be
The dislocated radial head hypertro- The loss of the normal anatomic rela- performed as posterior interosseous,
phies and the normally concave artic- tionships of the radiocapitellar joint and anterior interosseous, and ulnar nerve
ular surface becomes convex. The proximal radioulnar joint results in the palsies have been reported in cases of
capitellum is also reported to lose its loss of normal range of motion, the chronic radial-head dislocation10,43.
normal contour, demonstrating a flat- development of contractures, and Standard orthogonal radiographs
tened appearance39,40. Kim et al. dem- abnormal loading of these joints, ulti- of the injured elbow should be obtained
onstrated that these dysplastic changes mately resulting in late osteoarthritis9,12. and inspected for radiocapitellar joint
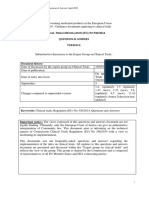
Fig. 1
Figs. 1-A through 1-D Missed Monteggia injury. (Reproduced, with permission, from San Diego Pediatric Orthopedics [SD PedsOrtho].) A 9-year-old,
right-hand-dominant boy fell onto the outstretched left forearm while skateboarding. He was evaluated by an outside facility where he was treated in a long
arm cast for elbow pain for 6 weeks. The long arm cast was discontinued afterwards, and the patient continued to report elbow stiffness and limited motion.
He was treated with activity modifications and physical therapy with no improvement. Fig. 1-A He was then eventually evaluated by another outside
orthopaedic surgeon who recognized a missed Monteggia injury 11 months after the initial injury on a lateral radiograph. Fig. 1-B The patient was then
referred for pediatric orthopaedic surgery evaluation and was evaluated 12 months after the initial injury, again with the radiograph demonstrating an
anterior radial-head dislocation consistent with a missed Monteggia injury. Figs. 1-C and 1-D Full-length lateral radiographs of the bilateral forearms
demonstrate a positive ulnar bow sign (denoted by an asterisk) of the left proximal part of the ulna (Fig. 1-C) compared with the right side (Fig. 1-D). As seen
in Figures 1-A and 1-B, the anterior radial-head dislocation is clearly noted on initial and follow-up injury radiographs as the radiocapitellar line is not colinear.
JUNE 2018 · VOLUME 6, ISSUE 6 · e2 3
| Missed Pediat r ic Monteg g ia Fractures
congruity. Images should be scrutinized should be ,2 to 3 mm in the uninjured no treatment in the setting of radial-head
by a practitioner with experience in ulna, and that deviation greater than this in dislocations that have been present for
reading pediatric elbow radiographs. the setting of radial-head dislocation rep- .3 months as he believed that the
The complexity of the pediatric elbow resented a likely traumatic etiology and postoperative loss of elbow function was
with its numerous ossification centers mild Monteggia equivalent injury38. a greater hindrance than the instability
has been cited as a potential reason for Radiographs of the contralateral forearm associated with a chronically dislocated
why Monteggia injuries are not diag- provide a useful comparison in attempting radial head47. It has since been noted
nosed in the acute setting among emer- to identify subtle injuries and should also that, with increasing functional
gency room physicians and junior be obtained. demands on the elbow as patients age,
orthopaedic residents6. Given the vari- patients can be expected to experience
able radiographic appearance of the Treatment increasing pain, deformity, and unsat-
pediatric elbow depending on the Treatment of the pediatric Monteggia isfactory range of motion39.
patient’s age, images of the contralateral injury is ideally performed in the acute
elbow may be useful in children ,10 setting. The preferred method of treat- Operative Treatment
years of age as a reference for the child’s ment in the acute setting is closed Operative treatment of missed Mon-
normal anatomy. Radiocapitellar joint reduction and long arm casting in supi- teggia lesions has been undertaken in
congruity is assessed on a true lateral nation with a focus on anatomic ulnar cases in which the radiocapitellar joint
radiograph of the elbow (Figs. 1-A and reduction guiding reduction of the ra- cannot be maintained in a reduced state
1-B). A line called the radiocapitellar line diocapitellar joint. As early as 2 weeks by closed means. Specific indications
or, eponymously, the Storen line is after injury, attempts at closed reduction include loss of function, progressive
drawn from the center of the radial neck, may be met with failure11. However, in deformity, decreased range of motion,
through the radial head and capitel- the subacute setting, for patients pre- and increased pain in the affected
lum44. If the radiocapitellar joint is senting up to 4 weeks after their initial elbow24,30,48-50. Several authors have
congruent, the radiocapitellar line injury, closed reduction may be suc- suggested operative intervention as soon
should bisect the capitellum in all cessful in maintaining stable reduction as the missed lesion has been identified,
degrees of flexion and extension of the of the radiocapitellar joint7. No defini- as the duration of neglect has corre-
elbow15. Elbow radiographs should also tive interval from initial injury to treat- sponded with worse outcomes23,39.
be assessed for radial-head hypertrophy ment has been established beyond which Contraindications to operative reduc-
with loss of its convex articular surface, an attempt at closed reduction has been tion have been described on the basis of
as well as dysplastic flattening of the deemed futile; however, most authors the duration of radial-head dislocation
capitellar articular surface. Radial-head describe a .4-week delay in treatment and patient age at the time of surgical
hypertrophy is assessed via the head- as representing a chronic Monteggia intervention. The most commonly cited
neck ratio on a lateral radiograph of the lesion that is no longer amenable to criteria for surgical intervention are a
elbow. The diameter of the radial head is closed reduction21,27,28,33,45,46. Opera- duration of radial-head dislocation of
measured at the widest portion of the tive treatment has become the gold ,3 years and patient age of ,12
metaphysis adjacent to the physis, and standard for the management of these years12,51. Nakamura et al. evaluated 22
the diameter of the radial neck is mea- injuries; myriad techniques and opin- patients undergoing open reduction of
sured at the narrowest portion of the ions exist in the current literature with the radial head with ulnar correction
neck, just proximal to the bicipital regard to how to best approach the osteotomy and annular ligament recon-
tuberosity. Radial-head hypertrophy is chronic missed Monteggia injury. We struction with a mean follow-up of 7
present if the head-neck ratio is .1.539. provide a review of this literature below. years. Interestingly, those patients who
Radiographs of the forearm should were $12 years old at the time of the
be obtained to assess for plastic deformity Nonoperative Treatment surgical procedure and also had a delay of
of the ulna. On a true lateral radiograph of Recent literature has described a limited treatment of $3 years had an 88% rate
the elbow, the posterior border of the ulnar role for nonoperative management in of radial-head subluxation or osteoar-
diaphysis should be a straight line. In Lin- the setting of chronic Monteggia lesions. thritic changes12. Conversely, reduction
coln and Mubarak’s method (the ulnar A review of the literature provides his- of the radial head was maintained, and
bow sign), they drew a line tangential to the torical context for the evolution of and osteoarthritic changes were absent at the
posterior border of the ulna in both healthy rationale for modern surgical manage- time of the final follow-up in all patients
controls and patients with known radial- ment. There is often a delay in the pre- who were within ,3 years of the injury
head dislocation (Figs. 1-C and 1-D). They sentation of symptoms, which or who were ,12 years of age at the time
then measured the maximum perpendic- previously led some authors to believe of the surgical procedure12.
ular distance of this line from the ulnar that chronic radial-head dislocation was In further support of these criteria,
shaft and determined that this distance largely asymptomatic. Blount advised radial-head dislocation of $3 years has
4 JUNE 2018 · VOLUME 6, ISSUE 6 · e2
Missed Pediatr ic Monteg gia Fractures |
been shown to predict more pro- dislocated radius, and annular ligament wire and allowed active range of motion.
nounced dysplastic changes of the radial reconstruction using a turned-down In their series of 8 patients, 7 underwent
head52. However, in the absence of central slip of triceps tendon passed cir- radiocapitellar pinning, and the
dysplastic changes, several authors have cumferentially around the neck of the 1 patient who underwent annular liga-
demonstrated good results following radius and inserted into a drill-hole in ment reconstruction without pinning
reduction up to 10 years after the initial the lateral part of the ulna. Patients were demonstrated residual radial-head sub-
injury7,21,30,33,45,53. Horii et al. dem- subsequently splinted in full extension luxation at the 7-year follow-up.
onstrated that it was possible to obtain and supination for 6 weeks, with active Therefore, the authors concluded
good reduction in patients 18 to 20 years range of motion as tolerated to follow. In that radiocapitellar pinning was neces-
of age; however, they noted that the his original series of 6 patients, he sary to maintain reduction. This
interval from the time of the injury to the described good results using this proce- became a popular modification as
time of the surgical procedure was 2 to 7 dure, with the exception of 1 recurrent authors believed that transarticular
months in these patients. They con- dislocation in a patient in whom the immobilization of the radiocapitellar
cluded that the radial head can be suc- triceps tendon was of poor quality for joint maintained reduction and
cessfully reduced regardless of age if reconstruction54. Many authors have protected the healing annular ligament
treated within a year after the initial advocated for annular ligament recon- reconstruction3,29. Letts et al. further
injury51. Thus, it might be suggested struction as a necessary component of modified this technique, advocating
that these numbers be used as guidelines surgical treatment of missed Monteggia against the transradiocapitellar pin over
rather than strict criteria and that all lesions3,5,21,29,37,40,54,55; however, the concern for intra-articular pin breakage,
patients should be carefully evaluated for methods of reconstruction have varied, and recommending pinning the proxi-
dysplastic changes to the radial head with authors describing procedures uti- mal part of the radius to the ulna37.
prior to attempted surgical reduction of lizing a slip of triceps tendon5,21,29,40,54, Radiocapitellar pinning remains con-
the radiocapitellar joint. a free fascial loop3,55, a free palmaris troversial, with authors reporting good
Many surgical techniques have tendon loop40, and a slip of forearm outcomes both with and without trans-
been developed to address this complex fascia37. Seel and Peterson recognized fixing the capitellum and radial head.
clinical problem, yet there remains no that the original Bell Tawse procedure However, this strategy provides an
consensus gold-standard treatment at and many of its described variations option for increasing stability of the
this time. Further, treatment of these produced a posterolaterally directed reduced radiocapitellar joint in particu-
injuries can vary in difficulty depending reducing force on the radial head. larly unstable dislocations9,23,31.
on the chronicity of the injury and may Although they noted that this may be
necessitate adjunct procedures to assist appropriate for anteromedial disloca- Ulnar Osteotomy
in maintaining reduction of the radio- tions, it may malreduce other injuries Lloyd-Roberts and Bucknill recognized
capitellar joint. Broadly, treatment (e.g., anterolateral, lateral, and posterior early in the evolution of the treatment of
strategies have aimed to reduce the radial-head dislocations). To address missed Monteggia lesions that, despite
radial-head dislocation through recon- this, they developed a 2-drill-hole adequate debridement of interposed
struction of the ligamentous stabilizers annular ligament reconstruction tech- capsuloligamentous tissue from the ra-
of the radiocapitellar joint and/or via nique that allows the reconstructed diocapitellar joint, some radial-head
correction of the associated ulnar annular ligament to function in its ana- dislocations required ulnar osteotomy to
deformity. Therefore, orthopaedic sur- tomic role as a U-bolt, producing a more achieve full reduction40. Kalamchi was
geons treating these patients should be centrally directed reducing force33. All the first to discuss ulnar osteotomy as a
aware of the reconstructive options options appear to function similarly, primary means for obtaining radial-head
available for addressing the radial-head with authors reporting good results in all reduction in the English-language liter-
dislocation and have a guided strategy to case series regardless of the chosen ature. He recognized that residual ulnar
address the ulnar deformity. reconstructive method. deformity may splint the radial head in
an unreduced position via the interos-
Annular Ligament Reconstruction Radiocapitellar Pinning seous membrane and that subsequent
(without Osteotomy) Lloyd-Roberts and Bucknill modified correction of the ulnar deformity would
Open treatment of chronically dis- the Bell Tawse procedure by securing allow for reduction of the radial head. In
located Monteggia lesions was first their radiocapitellar joint reduction with his study of 2 patients, he performed an
described by Bell Tawse in 196554. His a Kirschner wire passed through the ulnar osteotomy through a 1-cm inci-
procedure entailed a posterolateral capitellum and proximal part of the sion using multiple passes of a Kirschner
approach to the elbow with excision of radius with the elbow in flexion40. They wire to maintain the structural integrity
interposed capsular material from the subsequently splinted patients for 6 of the surrounding periosteum. He then
radiocapitellar joint, reduction of the weeks, at which point they removed the performed open reduction of the radial
JUNE 2018 · VOLUME 6, ISSUE 6 · e2 5
| Missed Pediat r ic Monteg g ia Fractures
Fig. 2
Figs. 2-A through 2-D Annular ligament button-hole and proximal ulnar osteotomy through the Kocher approach. (Reproduced, with permission,
from San Diego Pediatric Orthopedics [SD PedsOrtho].) Fig. 2-A Intraoperative image highlighting an intact annular ligament under the Freer Elevator
(Sklar) (black arrow), which demonstrates a button-hole phenomenon. The radial head was dislocated anteriorly and medial to the annular ligament. The
annular ligament was vented to facilitate reduction of the radial head. However, given the chronicity of the injury, the annular ligament was taken down
and was repaired at the end of the case. Figs. 2-B, 2-C, and 2-D Intraoperative images, highlighting the exposure of the proximal part of the ulna (Fig. 2-B)
followed by a crescentic osteotomy (white arrow) of the proximal part of the ulna (Fig. 2-C), and a corresponding radiographic image with the white arrow
highlighting the ulnar osteotomy site (Fig. 2-D).
head with slight overcorrection of the both the proximal part of the ulna and required a mean time of 3.5 months in the
ulnar deformity, repairing the remnant the radiocapitellar joint through a single external fixator frame. They obtained
annular ligament around the proximal incision. excellent clinical outcomes in all 4
part of the radius. Both patients dem- Methods for concentric reduction patients in their series. However, the
onstrated maintenance of the radio- of the radiocapitellar joint vary. Some most commonly employed technique for
capitellar joint reduction at the 1-year authors have contended that open radiocapitellar joint reduction is open
follow-up and good range of motion at reduction of the radial head is reduction, with many authors finding it
the 5-year follow-up56. unnecessary16,18,19,22,24. Lädermann necessary to excise interposed capsu-
Numerous case series have subse- et al. obtained closed reduction of the loligamentous tissue to obtain concentric
quently reported on ulnar osteotomy in radiocapitellar joint via ulnar osteotomy reduction of the radiocapitellar
the treatment of missed Monteggia with lengthening and correction of the joint7,9,12,20,21,23,25,27,28,30-32,53,56.
lesions, and surgical techniques have ulnar angular deformity through the Opinions on the necessity and
varied to some degree between nearly osteotomy site in 6 patients. All patients method of stabilizing the reduced radial
every case series. This is largely attrib- demonstrated normal range of motion head vary among authors who agree that
utable to the rarity of this injury. and had excellent clinical outcomes open reduction of the radiocapitellar
Described approaches include a postoperatively16. Bor et al. described joint is required. Some authors have
single-incision technique9,12,16,18,19,21- closed reduction of the radiocapitellar contended that the ulnar osteotomy
25,28,30-32,53
and a dual-incision joint using an Ilizarov technique to facilitates stability of the radial-head
technique 20,24,56. Most authors gradually lengthen and correct the reduction through the interosseous
have advocated a single-incision angular deformity of the ulna through membrane and advocate against extensive
technique through either a Boyd the ulnar osteotomy site via callotasis19. annular ligament reconstruction23,27,31,53,
approach9,21,23,26,27,57 or a Kocher They obtained serial radiographs at the and others have advocated for repair20,23,56
approach11,16,24 (Figs. 2-A through clinical follow-up, adjusting the angle or reconstruction7,12,18,21,27,28,30,32 of
2-D). These approaches are favored and distraction through the osteotomy the annular ligament to increase the sta-
because they afford the surgeon the as necessary to obtain concentric radio- bility of the joint. Described options for
ability to perform procedures directed at capitellar joint reduction. Reduction annular ligament reconstruction include
6 JUNE 2018 · VOLUME 6, ISSUE 6 · e2
Missed Pediatr ic Monteg gia Fractures |
techniques utilizing triceps tendon or that even with osteotomy and anatomic
fascia7,9,11,17,21,30,32,34, forearm extensor correction of the ulna, excess scar tissue or
fascia12,25-28, free palmaris longus ten- callus at the fracture site may act as a ful-
don12, and absorbable suture18. Delpont crum to the radius during pronation and
et al. provided the only direct comparison that this may be a cause for recurrent
of ulnar osteotomy with annular ligament anterior radial-head dislocation, or, in the
reconstruction to ulnar osteotomy with- setting of a firmly stabilized radial head
out annular ligament reconstruction9. In (e.g., following annular ligament recon-
this multicenter study, the surgeon’s struction), this may result in a mechanical
standard practice dictated if annular lig- block to pronation. Further, they recom-
ament reconstruction was undertaken. mended overcorrection at the ulnar
They reviewed 28 cases in which all osteotomy as this further tensions the
patients underwent overcorrection oste- interosseous membrane against forces that
otomy, with 12 patients undergoing would lead to recurrent radial-head dis-
annular ligament reconstruction in asso- location32. All case series from the last
ciation with open reduction of the ra- decade recommend a protocol of ulnar
diocapitellar joint, and 16 patients osteotomy with the degree of angular
undergoing open reduction of the radio- correction through the osteotomy to be
capitellar joint alone. They showed no determined by the position that allows for
significant difference in clinical func- a stable reduction of the radial head in all Fig. 3
tional outcomes between groups. Annu- combinations of flexion, extension, pro- Figs. 3-A and 3-B Reduction of the radial
lar ligament reconstruction did not nation, and supination. Invariably, these head and ulnar osteotomy fixation. (Re-
produced, with permission, from San Diego
guarantee radial-head stability, with 2 studies demonstrate overcorrection of the Pediatric Orthopedics [SD PedsOrtho].)
patients in the annular ligament recon- ulnar deformity9,12,16,19,23,27,31. Anteroposterior (Fig. 3-A) and lateral
struction group demonstrating recur- The location of ulnar osteotomy (Fig. 3-B) radiographs demonstrating
reduction of the radial head after proximal
rence of dislocation. They concluded that has been described at the center of ulnar osteotomy and subsequent fixation
annular ligament reconstruction is not rotation of angulation (CORA; often using a 2.7-mm limited contact
beneficial in conjunction with ulnar diaphyseal)16,26,28,30,32,56, and at the prox- dynamic compression plate bent with
apex-dorsal angulation to correct the ulnar
osteotomy in chronic Monteggia lesions imal part of the metaphysis9,12,16,17,19,21-27. deformity.
and that, although ulnar osteotomy with Lädermann et al. performed osteotomies
or without annular ligament reconstruc- at both the CORA and the proximal part Fixation constructs for the ulnar
tion consistently produced functional of the metaphysis16. One patient who osteotomy have varied from reports of
improvement in the setting of Bado type-I underwent osteotomy at the CORA no fixation at all56, relying on the peri-
lesions, it may be less effective in treat- went on to nonunion requiring revision osteum for stability, to fixation with an
ment of Bado type-III lesions. and bone-grafting. The authors con- elastic nail16, Kirschner wire7,11,23,28,32,33,
The degree of angular correction cluded that proximal osteotomy is a better plate and screws9,11,12,16,17,20,21,23,25-
27,30,32,34,53
through the ulnar osteotomy has been option because of the better metaphyseal , and, more recently, external
described as corrective (i.e., restoration blood supply precluding an increased risk fixation18,19,22,24,27,31. Proponents of
of the posterior cortical line)28,32, over- of nonunion, and the shorter proximal leaving the osteotomy unfixed have
corrective (i.e., reversing the original bone segment allowing for finer adjust- argued that this approach allows for natural
deformity)16,21,22,27,32,53,56, and ment of the ulnar angulation. Horii et al. remodeling of the ulna over time58. How-
allowing for stable radial-head reduc- additionally recommended that more ever, this approach necessitates prolonged
tion to guide the degree of angular proximal osteotomy also maintains the immobilization, which has been cited as a
correction9,12,19,23,24,30,31. Inoue and stouter distal fibers of the interosseous cause for elbow contracture and limited
Shionoya performed the only retro- membrane intact to the distal portion of range of motion following radial-head
spective review directly comparing the ulna, better translating ulnar correc- reduction8,34,46. Kirschner wire and elastic
patients undergoing corrective ulnar tion to the intact radius51. None of the nail fixation provide more stability than
osteotomy with patients undergoing literature is sufficient to demonstrate an periosteum alone; these constructs only
overcorrection ulnar osteotomy in the effect on union rate and maintenance of provide relative stability, which may be
treatment of Bado type-I injuries. They radial-head reduction; however, the most inadequate for maintenance of angular
demonstrated a significant increase (p # obvious benefit of an ulnar metaphyseal correction of the ulna, leading to recurrent
0.01) in patient functional outcomes in osteotomy is that the radiocapitellar joint radial-head dislocation51. Rigid fixation of
the overcorrection group, particularly in may be addressed directly through the the osteotomy site with a plate-and-screw
pronosupination. They hypothesized same incision. construct provides absolute stability
JUNE 2018 · VOLUME 6, ISSUE 6 · e2 7
| Missed Pediat r ic Monteg g ia Fractures
TABLE II Demographic Data of Outcome Studies for Missed Pediatric Monteggia Fractures*
No. of Age at Time of Interval from Injury
Study Patients Sex† Surgery‡ (yr) to Treatment‡ Bado Classification†
54
Bell Tawse (1965) 7 M (2), F (5) 7.1 (4.5 to 10) 14.1 mo (1 to 34 mo) I (7)
Lloyd-Roberts40 (1977) 8 NR 5.5 (3 to 8) 17.8 mo (4 to 36 mo) I (5), II (1),
uncategorized radial-
head dislocation (2)
Hurst29 (1983) 1 M (1) 12 2 yr I (1)
Fowles3 (1983) 5 M (2), F (3) 7.2 (3 to 9) 9.1 mo (1.5 to 24 mo) I (5)
Kalamchi56 (1986) 2 F (2) 5 (2.5 to 7.5) 5 mo (3.5 to 6.5 mo) I (2)
Hirayama53 (1987) 9 M (5), F (4) NR (2 to 12) NR (2 to 36 mo) I (5), III (4)
21
Stoll (1992) 8 NR 8.5 (4.3 to 15.5) 3.3 yr (1 to 9.5 yr) I (6), II (1), unknown (1)
Oner49 (1993) 7 M (1), F (6) 5.7 (4 to 9) 8.75 mo (1.25 to 16 mo) I (5), III (2)
Best30 (1994) 6 NR 9.8 (2.75 to 12) 27.4 mo (7 to 67 mo) I (6)
Tajima20 (1995) 23 NR NR NR I (10), II (2), III (9), IV (2)
Rodgers11 (1996) 7 M (3), F (4) 6.75 (1 to 12) 13.7 mo (1 to 39 mo) I (6), IV (1)
Devnani46 (1997) 3 M (2), F (1) 4.4 (2 to 5.66) 7.33 wk (6 to 8 wk) I (3)
Cappellino34 (1998) 3 F (3) 4 (1.4 to 6) 10 wk (NR) I (3)
Inoue32 (1998) 12 M (7), F (5) 7 (3 to 11) 16 mo (2 to 60 mo) I (12)
Seel33 (1999) 7 F (7) 5.8 (3.25 to 9) 30 mo (3 to 84 mo) NR
De Boeck35 (2000) 4 M (3), F (1) 7.1 (4 to 8.5) 10.5 mo (5 to 21 mo) I (4)
Exner22 (2001) 2 M (1), F (1) 7.13 (2.25 to 12) 2.6 yr (0.25 to 5 yr) I (2)
Horii51 (2002) 22 M (9), F (13) 10.1 (4 to 20) 10 mo (2 to 62 mo) NR
Kim39 (2002) 12 NR 7.4 (3 to 11) 30.3 mo (3 to 144 mo) I (11), II (1)
25
Degreef (2004) 6 M (4), F (2) 5 (2 to 6) 17 wk (5 to 59 wk) I (6)
David-West7 (2005) 8 M (5), F (3) 6.3 (4 to 8) 33.5 wk (2 to 192 wk) I (8)
Hasler24 (2005) 15 M (6), F (9) 9.5 (5 to 15) 22 mo (2 to 84 mo) I (15)
Hui28 (2005) 15 M (10), F (5) 8.25 (3 to 16) 3 mo (1.5 to 24 mo) I (14), III (1)
Koslowsky18 (2006) 3 F (3) 6.33 (6 to 7) 4 mo (1 to 7 mo) I (1), II (1), IV (1)
Wang26 (2006) 13 M (11), F (2) 8.3 (4 to 13) 7.8 yr (1 to 16.9 yr) I (13)
Belangero59 (2007) 8 M (2), F (6) 5.2 (2.7 to 10) 9.5 mo (1 to 18 mo) I (8)
Lädermann16 (2007) 6 M (3), F (3) 6.5 (4 to 8) 17 mo (1 to 49 mo) I (5), II (1)
Nakamura12 (2009) 22 M (14), F (8) 10 (4 to 16) NR I (19), III (1), IV (2)
23
Rahbek (2011) 16 M (11), F (5) 7.5 (3 to 13) 21 mo (1 to 83 mo) I (16)
Stitgen17 (2012) 1 M (1) 2.66 7 yr I (1)
Song27 (2012) 10 M (8), F (2) 7.5 (6 to 10) 1.7 yr (0.1 to 5 yr) I (6), III (4)
Lu31 (2013) 33 M (23), F (10) 7 (3 to 13) 15 mo (1.5 to 84 mo) NR
9
Delpont (2014) 28 M (12), F (16) 7 (4 to 12) 9.5 mo (3 to 44 mo) I (25), III (3)
Bor19 (2015) 4 M (2), F (2) 9.75 (9 to 11) 24 mo (3 to 54 mo) I (4)
*NR 5 not reported. †The number of patients is given in parentheses. ‡The values are given as the mean, with or without the range in parentheses.
allowing for early postoperative range of data in the literature with regard to the treatment or longer12,23,26,27. Across
motion, minimizing contracture51 (Figs. surgical treatment of chronic Monteggia these 4 studies, the majority of patients
3-A and 3-B). lesions, and comparisons across studies achieved good to excellent outcomes,
are made difficult by heterogeneity in with a mean redislocation rate of 6.6%.
Outcomes outcome measures. Most case series have Nakamura et al. reported on long-
Tables II, III, and IV show a thorough provided only short-term outcome data, term outcomes of open reduction of
summary of the literature and outcomes. with only 4 case series reporting final the radial head in combination with
There is a paucity of long-term outcome results at a mean time of 7 years after posterior-bending elongation ulnar
8 JUNE 2018 · VOLUME 6, ISSUE 6 · e2
Missed Pediatr ic Monteg gia Fractures |
TABLE III Surgical Information for Outcome Studies for Missed Pediatric Monteggia Fractures*
Approach for Ulnar Type of Ulnar Annular Ligament
Radial-Head Osteotomy Osteotomy Transradiocapitellar Reconstruction
Study Operative Treatment† Reduction Site† Fixation† Wire† Graft†
54
Bell Tawse Open reduction of radial head and Boyd NA NA No Triceps (6)
(1965) annular ligament reconstruction (6);
attempted closed reduction (1)
Lloyd- Open reduction of radial head and Boyd NA Plate and screws Yes (7) Palmaris (2),
Roberts40 annular ligament reconstruction (5); (1) triceps (6)
(1977) ulnar osteotomy, open reduction of
radial head, and annular ligament
reconstruction (1)
Hurst29 (1983) Open reduction of radial head and Boyd None NA Yes (6) Triceps (1)
annular ligament reconstruction (1)
Fowles3 (1983) Ulnar osteotomy (1); ulnar NR NR Plate and screws Yes (5) Remnant annular
osteotomy and annular ligament (2) ligament (4)
reconstruction (1); annular ligament
reconstruction (3)
Kalamchi56 Ulnar osteotomy and annular Kocher Site of original Molded cast (no No Remnant annular
(1986) ligament reconstruction (2) fracture (2) internal fixation) ligament (2)
Hirayama53 Ulnar osteotomy (9) Boyd Proximal part of Plate and screws No NA
(1987) metaphysis (9) (9)
Stoll21 (1992) Closed reduction (1); open Boyd Proximal part of Plate and screws Yes (3) Triceps tendon (5)
reduction of radial head, ulnar metaphysis (5) (5)
osteotomy, radial osteotomy, and
late radial-head excision (1); open
reduction of radial head and
annular ligament reconstruction (1);
radial-head excision (1); open
reduction of radial head, ulnar
osteotomy, and annular ligament
reconstruction (4)
Oner49 (1993) Open reduction of radial head and Boyd NA NA Yes (7) Triceps tendon (7)
annular ligament reconstruction (7)
Best30 (1994) Ulnar osteotomy and open Kocher CORA (7) None (5), plate Yes (7) Triceps tendon
reduction of radial head (1); ulnar and screws (2) (5), remnant
osteotomy, open reduction of radial annular ligament
head, and annular ligament (1)
reconstruction (6; note: 1 repeat
operation for late loss of reduction)
Tajima20 (1995) Isolated ulnar osteotomy (13); NR NR NR No NA
isolated radial shaft osteotomy (3);
combined radial and ulnar
osteotomies (2); radial-head
resection (5)
Rodgers11 Closed reduction of radial head and Kocher NR Kirschner wire (1), Yes (1) Triceps, ulnar
(1996) ulnar osteotomy (1); open reduction plate and screws periosteum,
of radial head and annular ligament (2), Rush rod (1), repair
reconstruction (2); open reduction and none (1)
of radial head, annular ligament
reconstruction, and ulnar
osteotomy (4)
Devnani46 Ulnar osteotomy and open Anterolateral Site of original 1.6-mm Kirschner Yes (3) NA
(1997) reduction of radial head (2); open fracture (2) wire
reduction of radial head (1)
Cappellino34 Open reduction of radial head and Boyd NR Plate and screws Yes (2) Triceps (3)
(1998) annular ligament reconstruction (2); (1)
open reduction of radial head,
annular ligament reconstruction,
ulnar osteotomy (1)
Inoue32 (1998) Ulnar osteotomy and open Posterolateral CORA (12) Plate and screws Yes (8) Triceps fascia (4)
reduction of radial head (8); ulnar (NR); Kirschner
osteotomy, open reduction of radial wires (NR);
head, annular ligament combination plate
reconstruction (4) and screws or
Kirschnerwires(NR)
continued
JUNE 2018 · VOLUME 6, ISSUE 6 · e2 9
| Missed Pediat r ic Monteg g ia Fractures
TABLE III (continued )
Approach for Ulnar Type of Ulnar Annular Ligament
Radial-Head Osteotomy Osteotomy Transradiocapitellar Reconstruction
Study Operative Treatment† Reduction Site† Fixation† Wire† Graft†
33
Seel (1999) Open reduction of radial head, Kocher NR Steinmann pin (1) Yes (4) Remnant annular
annular ligament reconstruction, ligament (5),
ulnar osteotomy (1); open reduction triceps (2)
of radial head and annular ligament
reconstruction (6)
De Boeck35 Open reduction of radial head Kocher NA NA Yes (4) NA
(2000)
Exner22 (2001) Ulnar osteotomy and external NA Proximal part of External fixation No NA
fixation (2) metaphysis (2) (2)
Horii51 (2002) Ulnar osteotomy (10); ulnar Kocher Proximal part of Plate and screws No Triceps fascia (11)
osteotomy and annular ligament metaphysis (NR);
reconstruction (6); ulnar osteotomy, (NR), ulnar shaft intramedullary
radial osteotomy, and annular (NR) Kirschner wire
ligament reconstruction (2); annular (NR)
ligament reconstruction (3); and
radial osteotomy (1)
Kim39 (2002) Open reduction of radial head and Posterior CORA (6) Plate and screws Yes (4) Triceps (11)
annular ligament reconstruction (2); (6)
ulnar osteotomy, open reduction of
radial head, and annular ligament
reconstruction (6); ulnar osteotomy,
radial shortening osteotomy, open
reduction of radial head, and
annular ligament reconstruction (1);
open reduction of radial head,
annular ligament reconstruction,
radial osteotomy, radial-head
arthroplasty, proximal radioulnar
joint notchplasty (2); open
reduction of radial head, annular
ligament reconstruction, radial
osteotomy (1)
Degreef25 Ulnar osteotomy and open Kaplan Proximal part of Plate and screws Yes (6) Forearm fascia (1),
(2004) reduction of radial head (4); ulnar metaphysis (6) (6) remnant annular
osteotomy, open reduction of radial ligament (1)
head, annular ligament
reconstruction (2)
David-West7 Ulnar osteotomy, open reduction of Boyd NR Intramedullary Yes (6) Triceps (6)
(2005) radial head, annular ligament Kirschner wire (6)
reconstruction (6); and closed
reduction (2)
Hasler24 (2005) Ulnar osteotomy, open reduction of Kocher Proximal part of External fixation No NA
radial head, and external fixation metaphysis (15) (15)
(NR); ulnar osteotomy, closed
reduction of radial head, and
external fixation (NR)
Hui28 (2005) Ulnar osteotomy, open reduction Modified Boyd Diaphyseal (12) Kirschner wires No Forearm fascia
of radial head, annular ligament (12) (15)
reconstruction (11); open
reduction of radial head and
annular ligament reconstruction
(3); ulnar osteotomy, radial
osteotomy, open reduction of
radial head, annular ligament
reconstruction (1)
Koslowsky18 Ulnar osteotomy, closed reduction NR NR External fixation Yes (1) Absorbable
(2006) of radial head, and external fixation (3) suture (2)
(1); ulnar osteotomy, open
reduction of radial head, annular
ligament reconstruction, and
external fixation (2)
Wang26 (2006) Ulnar osteotomy, open reduction of Boyd CORA (11), Plate and screws No Forearm fascia
radial head, annular ligament proximal part of (13) (13)
reconstruction (13) metaphysis (2)
continued
10 JUNE 2018 · VOLUME 6, ISSUE 6 · e2
Missed Pediatr ic Monteg gia Fractures |
TABLE III (continued )
Approach for Ulnar Type of Ulnar Annular Ligament
Radial-Head Osteotomy Osteotomy Transradiocapitellar Reconstruction
Study Operative Treatment† Reduction Site† Fixation† Wire† Graft†
59
Belangero Ulnar osteotomy and open Boyd (2), Proximal part of Plate and screws Yes (8) NA
(2007) reduction of radial head (8) Kocher (6) metaphysis (8) (8)
Lädermann16 Ulnar osteotomy (6) NA Proximal part of Plate and screws No NA
(2007) metaphysis (4), (5), and elastic nail
CORA (2) (1)
Nakamura12 Ulnar osteotomy, open reduction of Kocher Proximal part of Plate and screws No Forearm fascia
(2009) radial head, and annular ligament metaphysis (22) (22) (NR); remnant
reconstruction (22) annular ligament
augmented with
palmaris longus
(NR)
Rahbek23 Ulnar osteotomy, open reduction of Boyd Proximal part of Steinmann pin (9), Yes (7; if deemed Remnant annular
(2011) radial head, and annular ligament metaphysis (16) and plate and unstable ligament (10)
reconstruction (16) screws (7) intraoperatively)
Stitgen17 (2012) Ulnar osteotomy, open reduction of NR Proximal part of Plate and screws No Triceps (1)
radial head, and annular ligament metaphysis (1) (1)
reconstruction (1)
Song27 (2012) Ulnar osteotomy and closed Boyd Proximal part of Plate and screws No Forearm fascia (2)
reduction of radial head (8); ulnar metaphysis (10) (6),
osteotomy, open reduction of radial intramedullary
head, annular ligament nail (2), external
reconstruction (2) fixation (1), and
cast (1)
Lu31 (2013) Ulnar osteotomy, open reduction of Henry Proximal part of External fixation Yes (1) Remnant annular
radial head, external fixation (NR); metaphysis (33) (33) ligament (NR)
ulnar osteotomy, open reduction of
radial head, external fixation,
annular ligament reconstruction
(NR)
Delpont9 Ulnar osteotomy and open Boyd Proximal part of Plate and screws Yes (5) Triceps (12)
(2014) reduction of radial head (16); ulnar metaphysis (28) (28)
osteotomy, open reduction of radial
head, annular ligament
reconstruction (12)
Bor19 (2015) Ulnar osteotomy and external NA Proximal part of External fixation No NA
fixation metaphysis (4) (4)
*NA 5 not applicable, NR 5 not reported, and CORA 5 center of rotation of angulation. †The values in parentheses are given as the number of patients.
osteotomy and annular ligament recon- produce good long-term clinical and demonstrated a negative correlation
struction in 22 children with a mean final radiographic outcomes in patients who between patient age and interval from
follow-up of 7 years12. The mean Mayo underwent the surgical procedure at the injury to open reduction with radio-
Elbow Performance Index (MEPI) and age of ,12 years or within 3 years from graphic outcomes. In their series, annular
motion improved at the time of the final the date of the injury12. ligament reconstruction and trans-
follow-up. Radiographic outcomes were Rahbek et al. reported on long-term radiocapitellar Kirschner wire fixation did
good (maintained radial-head reduction, outcomes of open reduction of the radial not affect radiographic outcomes or
no osteoarthritic changes) in 15 patients head with posterior-bending elongation patient pain scores when compared with
and fair (radial-head subluxation or oste- ulnar osteotomy in 16 children performed procedures in which they were not per-
oarthritic changes) in 7 patients. Notably, by 1 of 2 surgeons at a mean final follow- formed. They did not recommend for or
all patients who underwent the surgical up of 8 years. Cases varied in terms of against annular ligament reconstruction as
procedure at the age of ,12 years or who annular ligament reconstruction com- their study was likely underpowered to
had an interval from the date of the injury pared with annular ligament resection as detect an effect on outcomes. However,
to the date of the surgical procedure of well as plate compared with Steinmann they emphasized that it is possible to
,3 years had good radiographic and pin fixation of the ulnar osteotomy. Ra- achieve a radial-head reduction that is
clinical outcomes. Thus, the authors diocapitellar pinning was also utilized if dynamically stable and provides good
concluded that open reduction for missed there was residual radial-head instability radiographic and clinical outcomes at a
Monteggia lesions could be expected to following ulnar osteotomy. They also long-term follow-up through posterior-
JUNE 2018 · VOLUME 6, ISSUE 6 · e2 11
| Missed Pediat r ic Monteg g ia Fractures
TABLE IV Outcomes for Missed Pediatric Monteggia Fracture Studies*
Flexion and Extension at Final Pronation and Supination at
Study Follow-up† Follow-up† (deg) Final Follow-up† (deg) Complications‡
54
Bell Tawse (1965) 2.1 yr (1 to 5.5 yr) NR (100 to “full”) and NR (240 to “full”) NR (“Loss of pronation” to “full”) Recurrent radial-head
and NR (“full”) dislocation (1)
Lloyd-Roberts40 (1977) 5.39 yr (0.5 to 18 yr) NR (100 to “full”) and NR (220 to “full”) NR (45 to “full”) and NR (45 to Radial-head subluxation (2)
“full”)
Hurst29 (1983) NR NR NR NR
Fowles3 (1983) 4.6 yr (1 to 8 yr) 157 (125 to 180) and 26 (225 to 0) 76 (60 to 90) and 88 (80 and 90) Loss of rotation (3); residual
valgus carrying angle (2);
radiocapitellar dysplasia (2);
radial-head subluxation (1)
Kalamchi56 (1986) 3 yr (1 to 5 yr) “Full” and “full” 60 and 90 None
Hirayama53 (1987) 3 yr (1.5 to 7 yr) NR NR Loss of pronation (4); persistent
radial nerve palsy (2); plate
fracture (2)
Stoll21 (1992) 3.25 yr (0.5 to 8 yr) 142.1 (130 to 155) and 8.1 (0 to 15) 56.9 (45 to 80) and 51.9 (0 to 80) Loss of radial-head reduction (1;
initially treated without
transcapitellar Kirschner wire
and converted to Kirschner
wire); loss of radial-head
reduction with pain and cubitus
valgus necessitating radial-
head resection (1)
Oner49 (1993) 3.3 yr (1 to 7 yr) NR NR Radioulnar synostosis (1);
radial-neck notching (2); radial-
head subluxation (2)
Best30 (1994) 21.8 mo (11 to 53 mo) “Full” and 21.2 (25 to “full”) 81.7 (60 to 90) and 83.3 (70 to Residual varus (1); loss of radial-
90) head reduction necessitating
reoperation (1)
Tajima20 (1995) NA NR NR Proximal radial migration with
subsequent positive ulnar
variance distally following
radial-head resection (5)
Rodgers11 (1996) 4.5 yr (2 to 11.25 yr) NR 49 (5 to 85) and 64 (35 to 90) Ulnar nerve palsy (2); loss of
fixation of ulnar osteotomy (2);
nonunion of ulnar osteotomy (1);
loss of radial-head reduction (3)
Devnani46 (1997) 3.66 yr (1 to 5 yr) 127.5 (125 to 130) and 25 (220 to 10) 16.66 (10 to 20) and “full” Loss of pronation (3)
Cappellino34 (1998) 25.7 (12 to 44) NR NR None
Inoue32 (1998) 5 yr (1 to 12 yr) 138 (130 to 150) and 20.5 (25 to 0) 55 (30 to 90) and 73 (30 to 100) Persistent radial-head
dislocation (3); unstable valgus
deformity of the elbow (1);
radiohumeral osteoarthritis
Seel33 (1999) 47.7 mo (12 to 96 mo) 132.7 (95 to 145) and 211 (240 to 0) 63.6 (5 to 90) and 81.4 (60 to 90) Recurrent radial-head
subluxation (2)
De Boeck35 (2000) 4.3 (2 to 8.6) 131.25 (120 to 140) and 26.25 (210 to 0) 77.5 (70 to 90) and 85 (80 to 90) None
Exner22 (2001) 5 yr (1 to 9 yr) 142.5 (140 to 145) and 10 (NR) 80 and 90 None
Horii51 (2002) 3 yr (0.66 to 12 yr) 134.2 (NR) and 3 (NR) 56.5 (NR) and 76.5 (NR) Radial-head subluxation (4),
radial-head redislocation (7;
prior to changing to ulnar
angulation osteotomy)
Kim39 (2002) 43.5 mo (12 to 105 mo) Mean flexion-extension arc, 125.0 (NR) 57.9 (45 to 75) and 74.6 (40 to Loss of pronation (7); loss of
85) pronation, supination, flexion,
and extension (1); radial-neck
notching (3); heterotopic
ossification (2); superficial
infection (1); radioulnar
synostosis (1)
Degreef25 (2004) 18 mo (4 to 36 mo) “Full” and “full” “Full” and “full” None
David-West7 (2005) 2.5 yr (1 to 5 yr) 108.8 (100 to 120) and 3.1 (0 to 10) 43.1 (30 to 60) and 61.3 (30 to Loss of radial-head reduction (2;
85) initially treated without
transcapitellar Kirschner wire
and converted to Kirschner wire)
continued
12 JUNE 2018 · VOLUME 6, ISSUE 6 · e2
Missed Pediatr ic Monteg gia Fractures |
TABLE IV (continued )
Flexion and Extension at Final Pronation and Supination at
Study Follow-up† Follow-up† (deg) Final Follow-up† (deg) Complications‡
24
Hasler (2005) 20 mo (6 to 60 mo) 136 (110 to 150) and 0 (220 to 10) 75.4 (40 to 90) and 80 (20 to 90) Delayed union of ulnar
osteotomy (2); superficial pin-
track infections (2)
Hui28 (2005) 4.25 yr (1 to 6 yr) 138.7 (90 to 150) and 2 (0 to 10) 76 (30 to 90) and 84 (60 to 90) Delayed union of ulnar
osteotomy (1); transient radial
nerve palsy (1), redislocation (1);
persistent radiocapitellar
subluxation (1)
Koslowsky18 (2006) 27.33 (26 to 30) 136.7 (130 to 140) and 16.7 (10 to 20) 90 and 90 None
Wang26 (2006) 7.8 yr (1 to 16.9 yr) 133 (110 to 145) and 1 (0 to 10) 67 (30 to 90) and 79 (30 to 90) Delayed union of ulnar
osteotomy (1); transient
posterior interosseous nerve
palsy (1); redislocation (1)
Belangero59 (2007) 4.5 (2 to 12) 135 and 0 76.25 (60 to 90) and 88.75 (80 to None
90)
Lädermann16 (2007) 3 yr (1.5 to 4.3 yr) 132.5 (120 to 140) and 4.2 (0 to 15) 85 (70 to 90) and 90 Nonunion (1)
Nakamura12 (2009) 7 yr (2 to 17 yr) 137.5 (130 to 145) and 2.3 (220 to 20) 66.8 (40 to 90) and 89.5 (70 to Delayed union ulnar osteotomy
95) (2); elbow contracture requiring
soft-tissue release (2)
Rahbek23 (2011) 8 yr (3 to 17 yr) NR NR Arthrosis or radial-head
subluxation (4); late dislocated
radial head (2)
Stitgen17 (2012) 5 mo “Full” and “full” 10 and “full” None
Song27 (2012) 10 yr (3 to 20 yr) NR NR Redislocation (3)
Lu31 (2013) 38 mo (12 to 86 mo) 130 (115 to 140) and 5 (5 to 10) 80 (70 to 90) and 80 (65 to 90) Redislocation (3; within 1 week),
delayed union ulnar osteotomy
(2; treatment with iliac crest
bone graft)
Delpont9 (2014) 6 yr (2 to 34 yr) 127 (110 to 140) and 24 (225 to 0) 66 (0 to 90) and 77 (20 to 90) Recurrent dislocation of the
radial head despite annular
ligament reconstruction (2);
osteoarthritis (3; 2 with
radiocapitellar pin); recurrent
subluxation of radial head (5;
every radiocapitellar pin)
Bor19 (2015) 3.75 yr (2 to 6 yr) 150 and 0 90 and 85 (70 to 90) Pin-track infection (1)
*NR 5 not recorded. †The values are given as the mean, with or without the range in parentheses. The values in parentheses are the number of patients.
bending elongation osteotomy of the ulna with osteotomy and correction of the Wang and Chang reported on a
alone. Finally, they did not demonstrate ulnar deformity alone. Three patients case series of 13 children treated with a
an effect of transradiocapitellar fixation who did not undergo annular ligament uniform surgical protocol26. Their
with a Kirschner wire on radiographic or reconstruction needed a revision pro- described technique used a single inci-
clinical outcomes, but recommended cedure for early redislocation of the sion via the Boyd approach with
against it if a stable radial-head reduction radial head and underwent revision of debridement of the remnant annular
could be obtained without it23. the ulnar osteotomy without annular ligament, osteotomy and correction of
Song et al. reported on outcomes in ligament reconstruction because the the ulnar deformity as dictated by
10 patients undergoing ulnar osteotomy original deformity was undercorrected. reduction of the radiocapitellar joint
with correction of ulnar deformity with a One patient had persistent radial-head with plate and screw fixation, and
mean final follow-up of 10 years27. Nine dislocation because of an uncorrected annular ligament reconstruction using a
patients reported excellent functional proximal radial deformity not appreci- strip of forearm fascia. The mean final
outcomes, and 1 patient reported a good ated at initial treatment. Similar to follow-up was 7.8 years. Restoration of a
functional outcome. All osteotomies Rahbek et al.23, these authors con- normal flexion-extension arc was noted
healed at 6 weeks without the use of cluded that annular ligament recon- to be more predictable than restoration
bone-grafting. Two patients underwent struction is not a necessary component of full pronosupination. One patient
annular ligament reconstruction and of maintaining a reduced and stable with a fair outcome and inadequate
the remaining 8 patients were treated radiocapitellar joint. motion had a redislocation that was
JUNE 2018 · VOLUME 6, ISSUE 6 · e2 13
| Missed Pediat r ic Monteg g ia Fractures
TABLE V Preferred Treatment Algorithm for Missed Pediatric Monteggia Injuries
Approach Single-incision, lateral approach through Kocher interval or Boyd approach
Ulnar osteotomy Crescentic osteotomy (to increase surface area for union) with angular correction of the ulnar deformity without
ulnar lengthening. Fixed in place with plate-and-screw fixation.
Radial-head reduction Initially attempt to reduce radial head into intact annular ligament. If this is unsuccessful, pie-crust annular ligament
and attempt second reduction. If this remains unsuccessful, incise annular ligament and repair around radial neck
following reduction.
Assessment of Fluoroscopic examination of radiocapitellar joint through full elbow range of motion. If radiocapitellar joint noted to
radiocapitellar stability be unstable, reassess adequacy of corrective ulnar osteotomy. If further ulnar deformity correction does not yield a
stable radiocapitellar joint, consider reinforcement of annular ligament repair with triceps fascia.
Postoperative Univalved long arm cast with overwrap at 1 week postoperatively. Long arm cast maintained for 6 weeks
management postoperatively, at which point the cast is removed and range of motion is initiated. Progressive increase in weight-
bearing and active range of motion as dictated by clinical and radiographic assessment of osteotomy healing, with
expected full activity without restrictions at 4 to 6 months postoperatively.
attributed to undercorrection of the radiocapitellar articulation and annu- whom the native annular ligament is
ulnar deformity. This patient under- lar ligament reconstruction along with inadequate or in whom reduction of the
went revision ulnar osteotomy and supplemental radiocapitellar pinning radiocapitellar joint necessitates debride-
demonstrated a reduced radiocapitellar directed at increasing the stability of ment of the interposed annular ligament.
joint at the time of the final follow-up. this relationship. Most of the modern The summary of a preferred technique for
One patient with an excellent outcome literature has transitioned to a focus on management of these injuries is included
had a delayed union of the ulna that the correction of the ulnar deformity, as in Table V. Further prospective study is
authors attributed to a 2-mm gap in the the ulnar deformity has been demon- necessary to determine optimal treatment
osteotomy site following plate-and- strated to splint the radial head in a of these injuries, with recognition that the
screw fixation and recommended bone- dislocated position through the inter- rarity of this injury presents a great chal-
grafting for gapping of $2 mm. The osseous membrane. Various tech- lenge to high-quality study design.
authors concluded that their proposed niques for osteotomy and fixation are
technique provided excellent functional described, and it is our belief that a James Hubbard, MD1,2,
outcomes and range of motion at the crescentic osteotomy of the ulna Aakash Chauhan, MD, MBA1,
long-term follow-up and that forearm without lengthening minimizes the Ryan Fitzgerald, MD3,
Reid Abrams, MD1,
fascia was a suitable alternative annular risk of osteotomy nonunion. The Scott Mubarak, MD2,
ligament reconstruction graft26. degree of ulnar correction is dictated by Mark Sangimino, MD4
the stability of the radiocapitellar joint
1Division of Hand, Upper Extremity, and
Conclusions on intraoperative fluoroscopic exami-
Pediatric Monteggia injuries represent nation through a full range of motion at Microvascular Surgery, Department of
Orthopaedic Surgery, University of
a rare upper-extremity fracture pat- the elbow. Correction of the deformity California, San Diego (UCSD), San Diego,
tern, and they may be easily missed. is increased until the radiocapitellar California
After as little as 2 weeks, a neglected joint is found to be stable in all posi-
2Department of Pediatric Orthopaedic
Monteggia injury can present a serious tions of flexion, extension, and pro-
Surgery, Rady Children’s Hospital, San
clinical challenge, often necessitating nosupination. Various supplemental
Diego, California
operative intervention. Closed treat- techniques directed at increasing the
ment and “skillful neglect,” as stability of the radiocapitellar joint are 3Department of Pediatric Orthopaedic
described by Blount47, represent the described and may be used at the discre- Surgery, Riley Children’s Hospital,
earliest management strategy for these tion of the treating surgeon as dictated by Indianapolis, Indiana
injuries; however, this has largely fallen the perceived stability of the radio- 4Division of Pediatric Orthopaedic
out of favor as many authors have rec- capitellar joint following ulnar osteotomy Surgery, Department of Orthopaedic
ognized that surgical radiocapitellar and indirect reduction. Our preferred Surgery, Allegheny General Hospital,
reduction is possible and provides good method of secondary stabilization is Pittsburgh, Pennsylvania
functional outcomes prior to onset of reduction of the radial head into the
chronic pathologic remodeling of the native annular ligament as this ligament is E-mail address for A. Chauhan: achau-
han1000@gmail.com
radial head and capitellum. Histori- often intact following radial-head dislo-
cally, operative techniques have cation in the pediatric population. ORCID iD for A. Chauhan: 0000-0002-
focused on direct reduction of the Reconstruction is reserved for patients in 1195-2491
14 JUNE 2018 · VOLUME 6, ISSUE 6 · e2
Missed Pediatr ic Monteg gia Fractures |
References 18. Koslowsky TC, Mader K, Wulke AP, acquired dislocation of the radial head. J
Gausepohl T, Pennig D. Operative treatment of Pediatr Orthop. 1998 May-Jun;18(3):410-4.
1. Ring D, Waters PM. Operative fixation of chronic Monteggia lesion in younger children: a
Monteggia fractures in children. J Bone Joint 35. De Boeck H. Treatment of chronic isolated
report of three cases. J Shoulder Elbow Surg. radial head dislocation in children. Clin Orthop
Surg Br. 1996 Sep;78(5):734-9. 2006 Jan-Feb;15(1):119-21. Relat Res. 2000 Nov;380:215-9.
2. Landin LA. Fracture patterns in children. 19. Bor N, Rubin G, Rozen N, Herzenberg JE.
Analysis of 8,682 fractures with special reference 36. Tompkins DG. The anterior Monteggia
Chronic anterior Monteggia lesions in children: fracture: observations on etiology and
to incidence, etiology and secular changes in a report of 4 cases treated with closed reduction
Swedish urban population 1950-1979. Acta treatment. J Bone Joint Surg Am. 1971 Sep;
by ulnar osteotomy and external fixation. J 53(6):1109-14.
Orthop Scand Suppl. 1983;202:1-109. Pediatr Orthop. 2015 Jan;35(1):7-10.
3. Fowles JV, Sliman N, Kassab MT. The 37. Letts M, Locht R, Wiens J. Monteggia
20. Tajima T, Yoshizu T. Treatment of long- fracture-dislocations in children. J Bone Joint
Monteggia lesion in children. Fracture of the
standing dislocation of the radial head in ne- Surg Br. 1985 Nov;67(5):724-7.
ulna and dislocation of the radial head. J Bone
glected Monteggia fractures. J Hand Surg Am.
Joint Surg Am. 1983 Dec;65(9):1276-82. 38. Lincoln TL, Mubarak SJ. “Isolated” traumatic
1995 May;20(3 Pt 2):S91-4.
4. Bado JL. The Monteggia lesion. Clin Orthop radial-head dislocation. J Pediatr Orthop. 1994
21. Stoll TM, Willis RB, Paterson DC. Treatment Jul-Aug;14(4):454-7.
Relat Res. 1967 Jan-Feb;50:71-86.
of the missed Monteggia fracture in the child. J
5. Dormans JP, Rang M. The problem of Bone Joint Surg Br. 1992 May;74(3):436-40. 39. Kim HT, Conjares JNV, Suh JT, Yoo CI.
Monteggia fracture-dislocations in children. Chronic radial head dislocation in children,
22. Exner GU. Missed chronic anterior part 1: pathologic changes preventing
Orthop Clin North Am. 1990 Apr;21(2):251-6.
Monteggia lesion. Closed reduction by gradual stable reduction and surgical correction.
6. Gleeson AP, Beattie TF. Monteggia fracture- lengthening and angulation of the ulna. J Bone
dislocation in children. J Accid Emerg Med. J Pediatr Orthop. 2002 Sep-Oct;22(5):
Joint Surg Br. 2001 May;83(4):547-50. 583-90.
1994 Sep;11(3):192-4.
23. Rahbek O, Deutch SR, Kold S, Søjbjerg JO, 40. Lloyd-Roberts GC, Bucknill TM. Anterior
7. David-West KS, Wilson NIL, Sherlock DA, Møller-Madsen B. Long-term outcome after
Bennet GC. Missed Monteggia injuries. Injury. dislocation of the radial head in children:
ulnar osteotomy for missed Monteggia fracture aetiology, natural history and
2005 Oct;36(10):1206-9. Epub 2005 Mar 28. dislocation in children. J Child Orthop. 2011 management. J Bone Joint Surg Br. 1977
8. Freedman L, Luk K, Leong JC. Radial head Dec;5(6):449-57. Epub 2011 Oct 16. Nov;59-B(4):402-7.
reduction after a missed Monteggia fracture: 24. Hasler CC, Von Laer L, Hell AK. Open
brief report. J Bone Joint Surg Br. 1988 Nov; 41. Garg R, Fung BKK, Chow SP, Ip WY. Surgical
reduction, ulnar osteotomy and external
70(5):846-7. management of radial head dislocation in
fixation for chronic anterior dislocation of the
quadriplegic cerebral palsy — a 5 year follow-
9. Delpont M, Jouve JL, Sales de Gauzy J, head of the radius. J Bone Joint Surg Br. 2005
up. J Hand Surg Eur Vol. 2007 Dec;32(6):725-6.
Louahem D, Vialle R, Bollini G, Accadbled F, Jan;87(1):88-94.
Epub 2007 Aug 2.
Cottalorda J. Proximal ulnar osteotomy in the 25. Degreef I, De Smet L. Missed radial head
treatment of neglected childhood Monteggia 42. Morrey BF, An KN. Articular and
dislocations in children associated with ulnar
lesion. Orthop Traumatol Surg Res. 2014 Nov; ligamentous contributions to the stability of the
deformation: treatment by open reduction and
100(7):803-7. Epub 2014 Oct 7. elbow joint. Am J Sports Med. 1983 Sep-Oct;
ulnar osteotomy. J Orthop Trauma. 2004 Jul;
11(5):315-9.
10. Holst-Nielsen F, Jensen V. Tardy posterior 18(6):375-8.
interosseous nerve palsy as a result of an 43. Chen WS. Late neuropathy in chronic
26. Wang MN, Chang WN. Chronic
unreduced radial head dislocation in dislocation of the radial head. Report of two
posttraumatic anterior dislocation of the radial
Monteggia fractures: a report of two cases. J cases. Acta Orthop Scand. 1992 Jun;63(3):
head in children: thirteen cases treated by open
Hand Surg Am. 1984 Jul;9(4):572-5. 343-4.
reduction, ulnar osteotomy, and annular
11. Rodgers WB, Waters PM, Hall JE. Chronic ligament reconstruction through a Boyd 44. Storen G. Traumatic dislocation of the radial
Monteggia lesions in children. Complications incision. J Orthop Trauma. 2006 Jan;20(1):1-5. head as an isolated lesion in children; report of
and results of reconstruction. J Bone Joint Surg one case with special regard to roentgen
27. Song KS, Ramnani K, Bae KC, Cho CH, Lee KJ,
Am. 1996 Sep;78(9):1322-9. diagnosis. Acta Chir Scand. 1959 Jan 31;116(2):
Son ES. Indirect reduction of the radial head in
144-7.
12. Nakamura K, Hirachi K, Uchiyama S, children with chronic Monteggia lesions. J
Takahara M, Minami A, Imaeda T, Kato H. Long- Orthop Trauma. 2012 Oct;26(10):597-601. 45. Gyr BM, Stevens PM, Smith JT. Chronic
term clinical and radiographic outcomes after Monteggia fractures in children: outcome after
28. Hui JHP, Sulaiman AR, Lee HC, Lam KS, Lee
open reduction for missed Monteggia fracture- treatment with the Bell-Tawse procedure. J
EH. Open reduction and annular ligament
dislocations in children. J Bone Joint Surg Am. Pediatr Orthop B. 2004 Nov;13(6):402-6.
reconstruction with fascia of the forearm in
2009 Jun;91(6):1394-404. chronic Monteggia lesions in children. J Pediatr 46. Devnani AS. Missed Monteggia fracture
13. Tubbs RS, O’Neil JT Jr, Key CD, Zarzour JG, Orthop. 2005 Jul-Aug;25(4):501-6. dislocation in children. Injury. 1997 Mar;28(2):
Fulghum SB, Kim EJ, Lyerly MJ, Shoja MM, 131-3.
29. Hurst LC, Dubrow EN. Surgical treatment of
George Salter E, Jerry Oakes W. The oblique symptomatic chronic radial head dislocation: a 47. Blount WP. Fractures in children. Baltimore:
cord of the forearm in man. Clin Anat. 2007 May; Williams & Wilkins; 1954.
neglected Monteggia fracture. J Pediatr
20(4):411-5. Orthop. 1983 May;3(2):227-30. 48. Papandrea R, Waters PM. Posttraumatic
14. Captier G, Canovas F, Mercier N, Thomas E, reconstruction of the elbow in the pediatric
30. Best TN. Management of old unreduced
Bonnel F. Biometry of the radial head: patient. Clin Orthop Relat Res. 2000 Jan;370:
Monteggia fracture dislocations of the elbow in
biomechanical implications in pronation and 115-26.
children. J Pediatr Orthop. 1994 Mar-Apr;14(2):
supination. Surg Radiol Anat. 2002 Dec;24(5):
193-9. 49. Oner FC, Diepstraten AF. Treatment of
295-301. Epub 2002 Nov 1.
31. Lu X, Kun Wang Y, Zhang J, Zhu Z, Guo Y, Lu chronic post-traumatic dislocation of the radial
15. Shah AS, Waters PM. Monteggia fracture-
M. Management of missed Monteggia fractures head in children. J Bone Joint Surg Br. 1993 Jul;
dislocation in children. In: Flynn JM, Skaggs
with ulnar osteotomy, open reduction, and 75(4):577-81.
DL, Waters PM, editors. Rockwood and
dual-socket external fixation. J Pediatr Orthop. 50. Bhaskar A. Missed Monteggia fracture in
Wilkins’ fractures in children. 8th ed.
2013 Jun;33(4):398-402. children: is annular ligament reconstruction
Philadelphia: Wolters Kluwer Health; 2014.
p 527-63. 32. Inoue G, Shionoya K. Corrective ulnar always required? Indian J Orthop. 2009 Oct;
osteotomy for malunited anterior Monteggia 43(4):389-95.
16. L ädermann A, Ceroni D, Lef èvre Y,
lesions in children. 12 patients followed for 1-12 51. Horii E, Nakamura R, Koh S, Inagaki H, Yajima
De Rosa V, De Coulon G, Kaelin A. Surgical
years. Acta Orthop Scand. 1998 Feb;69(1):73-6. H, Nakao E. Surgical treatment for chronic radial
treatment of missed Monteggia lesions in
children. J Child Orthop. 2007 Oct;1(4): 33. Seel MJ, Peterson HA. Management of head dislocation. J Bone Joint Surg Am. 2002
237-42. Epub 2007 Aug 29. chronic posttraumatic radial head Jul;84(7):1183-8.
17. Stitgen A, McCarthy JJ, Nemeth BA, Garrels dislocation in children. J Pediatr Orthop. 52. Oka K, Murase T, Moritomo H, Sugamoto K,
K, Noonan KJ. Ulnar fracture with late radial 1999 May-Jun;19(3):306-12. Yoshikawa H. Morphologic evaluation of
head dislocation: delayed Monteggia fracture. 34. Cappellino A, Wolfe SW, Marsh JS. Use of chronic radial head dislocation: three-
Orthopedics. 2012 Mar 7;35(3):e434-7. a modified Bell Tawse procedure for chronic dimensional and quantitative analyses. Clin
JUNE 2018 · VOLUME 6, ISSUE 6 · e2 15
| Missed Pediat r ic Monteg g ia Fractures
Orthop Relat Res. 2010 Sep;468(9):2410-8. Epub 55. Aufranc OE, Jones WN, Bierbaum BE. Late one incision. Surg Gynecol Obstet. 1940;71:
2010 Mar 4. traumatic dislocation of the radial head. JAMA. 86-8.
53. Hirayama T, Takemitsu Y, Yagihara K, Mikita A. 1969 Jun 30;208(13):2465-7. 58. Mehta SD. Flexion osteotomy of ulna for
Operation for chronic dislocation of the radial 56. Kalamchi A. Monteggia fracture- untreated Monteggia fracture in children. Ind J
head in children. Reduction by osteotomy of the dislocation in children. Late treatment in two Surg. 1985;47:15-9.
ulna. J Bone Joint Surg Br. 1987 Aug;69(4):639-42. cases. J Bone Joint Surg Am. 1986 Apr;68(4): 59. Belangero WD, Livani B, Zogaib RK.
54. Bell Tawse AJS. The treatment of malunited 615-9. Treatment of chronic radial head dislocations in
anterior Monteggia fractures in children. J Bone 57. Boyd HB. Surgical exposure of the ulna children. Int Orthop. 2007 Apr;31(2):151-4. Epub
Joint Surg Br. 1965 Nov;47(4):718-23. and proximal third of the radius through 2006 Jun 2.
16 JUNE 2018 · VOLUME 6, ISSUE 6 · e2
You might also like
- I. X-Ray Image: Hindfoot Fractures By: Jeremy Tan and Sarah HillDocument8 pagesI. X-Ray Image: Hindfoot Fractures By: Jeremy Tan and Sarah HillSheril MarekNo ratings yet
- Z Effect & Reverse Z Effect in PFNDocument7 pagesZ Effect & Reverse Z Effect in PFNNandan SurNo ratings yet
- Ankle Fractures: A Literature Review of Current Treatment MethodsDocument13 pagesAnkle Fractures: A Literature Review of Current Treatment Methodsadrian1989No ratings yet
- Management of Avn HipDocument13 pagesManagement of Avn Hipterencedsza100% (1)
- SUTGMultiLocJ9981A PDFDocument60 pagesSUTGMultiLocJ9981A PDFLouis MiuNo ratings yet
- Ligamentous Injuries About The Ankle and Subtalar Joints: Hans Zwipp, MD, PHD, Stefan Rammelt, MD, Rene Grass, MDDocument35 pagesLigamentous Injuries About The Ankle and Subtalar Joints: Hans Zwipp, MD, PHD, Stefan Rammelt, MD, Rene Grass, MDAnonymous kdBDppigENo ratings yet
- Fractures of The Humeral ShaftDocument25 pagesFractures of The Humeral ShaftMuhammad IqbalNo ratings yet
- External Fixator 110222141011 Phpapp01 131027142629 Phpapp01Document65 pagesExternal Fixator 110222141011 Phpapp01 131027142629 Phpapp01manjunathaNo ratings yet
- The Intramedullary Nail Is Commonly Used For LongDocument4 pagesThe Intramedullary Nail Is Commonly Used For LongUhuebor DavidNo ratings yet
- Pricippriles of Intramedullary NailingDocument57 pagesPricippriles of Intramedullary NailingAbdallah OmerNo ratings yet
- Acetabular and Hip FractureDocument133 pagesAcetabular and Hip FractureJuanita HenryNo ratings yet
- Avascular Necrosis of The Fibular SesamoidDocument7 pagesAvascular Necrosis of The Fibular SesamoidAlex Yvan Escobedo HinostrozaNo ratings yet
- Radiography of the Hip: Recognizing Disease PatternsDocument16 pagesRadiography of the Hip: Recognizing Disease PatternsVivi Evita DewiNo ratings yet
- Articular Fractures: PrinciplesDocument24 pagesArticular Fractures: Principlestom kurniawanNo ratings yet
- Arm:Leg Fracture PDFDocument11 pagesArm:Leg Fracture PDFHannaNo ratings yet
- Gamma3 Trochanteric Nail 180 TécCirurgDocument48 pagesGamma3 Trochanteric Nail 180 TécCirurgPetru GanganNo ratings yet
- Mosaicplasty 1030208g UsDocument12 pagesMosaicplasty 1030208g UsAnil SoodNo ratings yet
- The Ankle Joint: Articulating BonesDocument5 pagesThe Ankle Joint: Articulating BonesJoe SpencerNo ratings yet
- Large Fragment Locking Compression Plate (LCP) : Technique GuideDocument23 pagesLarge Fragment Locking Compression Plate (LCP) : Technique GuideLouis MiuNo ratings yet
- Ankle ComplexDocument95 pagesAnkle ComplexMangala Prema MohanarangamNo ratings yet
- Humeral Shaft Fractures: Nonoperative and Operative Treatment OptionsDocument82 pagesHumeral Shaft Fractures: Nonoperative and Operative Treatment OptionsYoga AninditaNo ratings yet
- Distal Humeral Fractures-Current Concepts PDFDocument11 pagesDistal Humeral Fractures-Current Concepts PDFRina AlvionitaNo ratings yet
- Trochanteric #Document20 pagesTrochanteric #Prakash AyyaduraiNo ratings yet
- Ankle Anatomy and Blood Supply of TalusDocument66 pagesAnkle Anatomy and Blood Supply of TalusShashank29 LakkalaNo ratings yet
- Wound Care Dressings and Their Uses: Carolyn Watts MSN, RN, CWON Vanderbilt University Medical Center Nashville, TNDocument34 pagesWound Care Dressings and Their Uses: Carolyn Watts MSN, RN, CWON Vanderbilt University Medical Center Nashville, TNSuciNo ratings yet
- Gamma NailDocument49 pagesGamma NailMihaela HerghelegiuNo ratings yet
- 2015 OS - Fanelli Surgery PowerpointDocument24 pages2015 OS - Fanelli Surgery PowerpointMamedNo ratings yet
- Jude's Quadriceps Plasty For Stiff KneeDocument6 pagesJude's Quadriceps Plasty For Stiff KneeRaviNo ratings yet
- Peripheral Nerve Disorders: Grades of Injury and Treatment OptionsDocument75 pagesPeripheral Nerve Disorders: Grades of Injury and Treatment OptionsAllahbesertkitaNo ratings yet
- Clavo para ClaviculaDocument12 pagesClavo para ClaviculaMartinLydenNo ratings yet
- Shoulder Arthroscopy Patient Education Packet RayappaDocument5 pagesShoulder Arthroscopy Patient Education Packet Rayappaapi-549337910No ratings yet
- Distal Femur Fractures Fixation by Locking Compression Plate-Assessment of Outcome by Rasmussens Functional Knee ScoreDocument7 pagesDistal Femur Fractures Fixation by Locking Compression Plate-Assessment of Outcome by Rasmussens Functional Knee ScoreIJAR JOURNALNo ratings yet
- Kamars RadiologyDocument135 pagesKamars RadiologyNayantara Nair100% (1)
- Polyaxial Locking System: Numelock IIDocument24 pagesPolyaxial Locking System: Numelock IIpecheniqNo ratings yet
- Journeyii CR 00344v1 UsDocument40 pagesJourneyii CR 00344v1 UsSufyanNo ratings yet
- Achilles Tendon RuptureDocument19 pagesAchilles Tendon Ruptureapi-509245925No ratings yet
- Management of FractureDocument20 pagesManagement of FractureHitesh RohitNo ratings yet
- MDN Femoral Retrograde Intramedullary Fixation Surgical Technique 97-2252-009-01 Rev2 09 2011 PDFDocument22 pagesMDN Femoral Retrograde Intramedullary Fixation Surgical Technique 97-2252-009-01 Rev2 09 2011 PDFcuki5No ratings yet
- Tibia Nailing System: T2 AlphaDocument52 pagesTibia Nailing System: T2 AlphaJoselo ChNo ratings yet
- Ministry of Defence Synopsis of Causation Pes PlanusDocument14 pagesMinistry of Defence Synopsis of Causation Pes PlanusSari HestiyariniNo ratings yet
- Distal End Humerus Fractures: BY:-Dr. Anshu Sharma Guide:-Dr.A.K. MathurDocument76 pagesDistal End Humerus Fractures: BY:-Dr. Anshu Sharma Guide:-Dr.A.K. MathurToàn Đặng Phan VĩnhNo ratings yet
- Statured Patients.: Surgical TechniqueDocument76 pagesStatured Patients.: Surgical TechniqueAdithya StephanaNo ratings yet
- AO Trauma Vol.2Document100 pagesAO Trauma Vol.2Cujba GheorgheNo ratings yet
- Diaphyseal fixation using long tapered stem femoral revision techniqueDocument19 pagesDiaphyseal fixation using long tapered stem femoral revision techniquePurushotham NalamatiNo ratings yet
- Triple ArthrodesisDocument10 pagesTriple ArthrodesisdrkbarryNo ratings yet
- S2 Tibial NailDocument32 pagesS2 Tibial NailAloexandru All IonNo ratings yet
- Fracture of The Talus and Calcaneus NickDocument43 pagesFracture of The Talus and Calcaneus NickTan Zhi HongNo ratings yet
- Introduction of MSK ImagingDocument63 pagesIntroduction of MSK ImagingyeabsraNo ratings yet
- Synthes Titanium Implant PlatesDocument36 pagesSynthes Titanium Implant PlatesMico StanojevicNo ratings yet
- Avascular NecrosisDocument58 pagesAvascular Necrosischatree100% (4)
- Diagnosis and Treatment of Acute Essex-Lopresti inDocument11 pagesDiagnosis and Treatment of Acute Essex-Lopresti inMỸ NGUYỄN CÔNGNo ratings yet
- Giant Cell TumorDocument22 pagesGiant Cell TumorMaxmillian Alexander KawilarangNo ratings yet
- 3 5mmClavHookPlateDocument11 pages3 5mmClavHookPlatethomsoon01No ratings yet
- Expert Tibia NailDocument32 pagesExpert Tibia NailStefan KambeyNo ratings yet
- DRUJinstabilityreview - PDF 034407Document15 pagesDRUJinstabilityreview - PDF 034407Oscar Cayetano Herrera RodríguezNo ratings yet
- ZOO3731 chptr.6-8Document55 pagesZOO3731 chptr.6-8Raylax2sik24No ratings yet
- Club Foot PDFDocument54 pagesClub Foot PDFBelle Sakunrat SarikitNo ratings yet
- Short Reconstruction NailDocument14 pagesShort Reconstruction NailSimona DraganNo ratings yet
- All Papers Topic WiseDocument55 pagesAll Papers Topic WiseZ TariqNo ratings yet
- var-wal-01_02-variax-t8-system-back-table-layout_finalDocument1 pagevar-wal-01_02-variax-t8-system-back-table-layout_finalEric RothNo ratings yet
- Idiopathic Congenital Talipes Equinovarus PDFDocument10 pagesIdiopathic Congenital Talipes Equinovarus PDFEric RothNo ratings yet
- s-0043-1774371Document14 pagess-0043-1774371Eric RothNo ratings yet
- Enfermedad de PerthesDocument11 pagesEnfermedad de PerthesDanilo SolarteNo ratings yet
- PDF ConsumersInHealthCareBurdenChoiceDocument34 pagesPDF ConsumersInHealthCareBurdenChoiceEric RothNo ratings yet
- Monteggia Fractures in Children and AdultsDocument10 pagesMonteggia Fractures in Children and AdultsEric RothNo ratings yet
- TX of Severe ClubfootDocument24 pagesTX of Severe ClubfootEric RothNo ratings yet
- JOT Talar Body FXDocument8 pagesJOT Talar Body FXEric RothNo ratings yet
- Pediatric Monteggia FracturesDocument6 pagesPediatric Monteggia FracturesEric RothNo ratings yet
- Wms GOLD 2017 Pocket Guide 1 PDFDocument42 pagesWms GOLD 2017 Pocket Guide 1 PDFL P PutriNo ratings yet
- Biology and Enhancement of Skeletal RepairDocument31 pagesBiology and Enhancement of Skeletal RepairEric RothNo ratings yet
- Tocolytics (Also Called Anti-Contraction Medications or Labor Represents) AreDocument2 pagesTocolytics (Also Called Anti-Contraction Medications or Labor Represents) AreEric RothNo ratings yet
- Cardiovascularsystemexamination 170514182612Document119 pagesCardiovascularsystemexamination 170514182612Eric RothNo ratings yet
- ASCCP CX Cancer Precursor Management Guidelines For LondonDocument47 pagesASCCP CX Cancer Precursor Management Guidelines For LondonEric RothNo ratings yet
- 2012 ASCCP Updated Guidelines PAPDocument27 pages2012 ASCCP Updated Guidelines PAPhayamasNo ratings yet
- Garfinkel Case at The University of MinnesotaDocument9 pagesGarfinkel Case at The University of MinnesotaMarkingsonCaseNo ratings yet
- MemoryDocument46 pagesMemoryMaha Al AmadNo ratings yet
- A New Drug-Shelf Arrangement For Reducing MedicatiDocument9 pagesA New Drug-Shelf Arrangement For Reducing MedicatiEmmanuel LawerNo ratings yet
- Drugs & PregnancyDocument385 pagesDrugs & Pregnancysanjeevani20100% (3)
- Respiratory Physiology AnswersDocument4 pagesRespiratory Physiology AnswersRamya100% (2)
- A Novel Visual Clue For The Diagnosis of Hypertrophic Lichen PlanusDocument1 pageA Novel Visual Clue For The Diagnosis of Hypertrophic Lichen Planus600WPMPONo ratings yet
- General Survey TECHNIQUE Actual Findings Normal Findings AnalysisDocument21 pagesGeneral Survey TECHNIQUE Actual Findings Normal Findings AnalysisJerry Joseph B. AbordoNo ratings yet
- Indian ListenerDocument103 pagesIndian ListenerTareq Aziz100% (1)
- Drug Study - MidazolamDocument2 pagesDrug Study - MidazolamKian HerreraNo ratings yet
- Example of SpeechDocument9 pagesExample of SpeechDanville CoquillaNo ratings yet
- DR, OR, WardDocument14 pagesDR, OR, WardjanNo ratings yet
- BellDocument8 pagesBellZu MieNo ratings yet
- Tracheostomy Care With ChecklistDocument5 pagesTracheostomy Care With ChecklistHollan GaliciaNo ratings yet
- Resume 101: Write A Resume That Gets You NoticedDocument16 pagesResume 101: Write A Resume That Gets You Noticedgqu3No ratings yet
- Act 342 Prevention and Control of Infectious Diseases Act 1988Document26 pagesAct 342 Prevention and Control of Infectious Diseases Act 1988Adam Haida & Co100% (1)
- Cardiovascular Nursing NotesDocument17 pagesCardiovascular Nursing NotesLucky GomezNo ratings yet
- Regulation5362014 Qa enDocument143 pagesRegulation5362014 Qa enmeiNo ratings yet
- KENCAP Changzhou 2013Document19 pagesKENCAP Changzhou 2013KencapchangzhouNo ratings yet
- Vocal Cord ParalysisDocument74 pagesVocal Cord ParalysisWaqas KhanNo ratings yet
- 3.mechanical VentilationDocument33 pages3.mechanical Ventilationisapatrick8126No ratings yet
- Dynamic Approach To Discounting Patient ShareDocument11 pagesDynamic Approach To Discounting Patient SharemaleticjNo ratings yet
- 1 PBDocument21 pages1 PBDewi Puspita SariNo ratings yet
- Effects of Boiling Time On Mineral and Vitamin C Content of Three Varieties of Hibiscus Sabdriffa Drink in NigeriaDocument6 pagesEffects of Boiling Time On Mineral and Vitamin C Content of Three Varieties of Hibiscus Sabdriffa Drink in NigeriariniyuliasamosirNo ratings yet
- Life Calling Map Fillable FormDocument2 pagesLife Calling Map Fillable Formapi-300853489No ratings yet
- 515Document972 pages515solecitodelmarazul100% (6)
- Balcom Rebecca Functional ResumeDocument2 pagesBalcom Rebecca Functional Resumeapi-360266135No ratings yet
- From Wikipedia, The Free EncyclopediaDocument12 pagesFrom Wikipedia, The Free EncyclopediaCharlie EspinoNo ratings yet
- Toxic Metabolic Encephalopathy John W. Melton, M.DDocument17 pagesToxic Metabolic Encephalopathy John W. Melton, M.DabdalkhalidNo ratings yet
- Healing Stories of People Final EditingDocument53 pagesHealing Stories of People Final Editinggabyk6867% (3)
- Pterygomandibular Space DepthDocument10 pagesPterygomandibular Space DepthBharathNo ratings yet