Professional Documents
Culture Documents
Rhinitis Guidelines: Classification and Differential Diagnosis
Uploaded by
EricaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Rhinitis Guidelines: Classification and Differential Diagnosis
Uploaded by
EricaCopyright:
Available Formats
Hull & East Riding Prescribing Committee
Rhinitis Guidelines
Classification and Differential Diagnosis
1. Rhinitis is defined as having two of the listed symptoms for ≥1 hour/day for ≥2 weeks
a. blockage
b. running (including postnasal drip)
c. sneezing (including nasal itch)
2. Classification of rhinitis
Allergic Infective Other As part of systemic disorder
Seasonal Acute Idiopathic Primary defect in mucus
Perennial Chronic NARES (non-allergic rhinitis cystic fibrosis
Occupational with eosinophilia) Young's syndrome
Drug induced: Primary ciliary dyskinesia
beta-blockers (Kartagener's syndrome)
oral contraceptives Immunological
aspirin systemic lupus
NSAIDS erythematosus
local decongestants rheumatoid arthritis
Autonomic (responds to AIDS
anticholinergics) Antibody deficiency
Atrophic Granulomatous disease
Neoplastic Wegener's
sarcoidosis
Hormonal
hypothyroidism
pregnancy
“old man's drip”
Severity Mild
normal sleep and
no impairment of daily activities, sport, leisure and
no impairment of work and school and
no troublesome symptoms
Moderate-Severe
abnormal sleep or
impairment of daily activities, sport, leisure or
impaired work and school or
troublesome symptoms
Nasal problems are often multi-factorial and this needs to be taken into account when using the
above classification or considering treatment.
Prescribing Guideline for Rhinitis
Date approved HERPC: July 2017 Review: July 2020 Page 1 of 5
Diagnosis
1. Take a history
2. Nasal examination
a. external and internal appearance
b. secretions (clear, discoloured or blood stained)
c. airflow
d. palpation
3. Consider:
a. specific IgE
b. other blood tests, e.g. FBC, thyroid function
Treatment (see Figure 1)
1. Education
a. provide advice on allergen avoidance and drug therapy, including safety and side
effects
b. poor compliance or poor technique in the use of nasal sprays and drops will result in
treatment failure, therefore appropriate training is imperative
2. Antihistamines (AH)
a. available as oral (OAH) or intranasal (INAH) preparations
b. first-line therapy for mild allergic rhinitis
c. addition to intranasal steroids for moderate/severe allergic rhinitis uncontrolled on
topical intranasal steroids (INS) alone
d. OAH – effective predominantly on “wet” symptoms such as itch, sneeze and
rhinorrhoea; regular therapy is more effective than ‘as-needed’ use. Hull and East
Riding Joint Formulary: First line choice – Cetirizine; Second line choices – Loratadine
or Fexofenadine
e. INAH (Azelastine) – useful as rescue therapy due to fast onset of action within 15
minute
3. Topical intranasal corticosteroids (INS)
a. first-line therapy for moderate to severe allergic rhinitis persistent symptoms. Hull
and East Riding Joint Formulary: First line choice – Beclometasone nasal spray;
Second line choices - Budesonide nasal spray or Mometasone nasal spray or
Fluticasone nasal spray
b. addition to OAH or INAH in uncontrolled mild allergic rhinitis
c. topical steroid drops should be used initially in nasal polyposis and severe
obstruction. These are for short term use only.
d. systemic absorption negligible with Mometasone and Fluticasone, modest for the
remainder and high for Betamethasone nasal drops and Fluticasone nasal drops
which are for short term use only
4. Systemic corticosteroids:
Prescribing Guideline for Rhinitis
Date approved HERPC: July 2017 Review: July 2020 Page 2 of 5
a. rarely indicated in the management of rhinitis, except for
i. severe nasal obstruction
ii. short-term Prednisolone (0.5 mg/kg for 5 to 10 days) rescue medication for
uncontrolled symptoms on conventional pharmacotherapy
iii. important social or work-related events, e.g. examinations, weddings
b. oral corticosteroids should be used briefly and always in combination with a topical
nasal corticosteroid
c. Injectable corticosteroids are not recommended as the risk-benefit profile is poor
5. Anti-leukotrienes (LTRA)
a. Montelukast is licensed in the UK for those with seasonal allergic rhinitis who also
have concomitant asthma since the age of 6 months
6. Topical anti-cholinergic (e.g. Ipratropium bromide)
a. watery rhinorrhoea in allergic rhinitis despite compliance with INS or INS with OAH
or INAH
b. autonomic rhinitis when the dominant symptom is profuse watery rhinorrhoea in
response to irritant triggers or changes in temperature
7. Chromones (e.g. Sodium cromoglicate)
a. children and adults with mild symptoms only and sporadic problems in season or on
limited allergen exposure
b. Cromoglicate and Nedocromil eye drops are useful in allergic conjunctivitis as
topical therapy
8. Allergen immunotherapy (desensitisation)
a. for pollen-allergic patients who fail to respond sufficiently to maximum conventional
treatment (combination of INS and OAH or INAH)
NB. Treatment failure should always provoke a review of compliance.
Rhinitis in pregnancy and during breastfeeding
rhinitis affects at least 20% of pregnancies and can start during any gestational week
regular nasal douching may be helpful
most medications cross the placenta and should only be prescribed when the apparent
benefit is greater than the risk to the foetus
it is a good practice to start treatment with ‘tried and tested’ drugs
intranasal Beclomethasone, Fluticasone and Budesonide appear to have good safety
records as they are widely used in pregnant asthmatic women
intanasal and ocular Cromoglicate may be helpful
oral Chlorphenamine, Loratidine or Cetirizine may be added cautiously if additional
treatment is needed but decongestants should be avoided
Prescribing Guideline for Rhinitis
Date approved HERPC: July 2017 Review: July 2020 Page 3 of 5
Referral (see Figure 1)
1. ENT referral
a. unilateral nasal problems
b. nasal perforations, ulceration or collapse
c. blood-stained discharge
d. crusting high in the nasal cavity
e. periorbital cellulitis (refer urgently)
2. Allergy referral
a. inadequate control of symptoms
b. allergen/trigger identification
c. to consider desensitisation
d. recurrent nasal polyps
e. recurrent infective rhinitis and sinusitis requiring antibiotics to exclude allergy or
immunodeficiency
f. multisystem allergy (e.g. rhinitis with asthma, eczema or food allergy)
g. occupational rhinitis
References
1. e-Guidelines: Rhinitis management guidelines (registration and log in required)
https://www.guidelines.co.uk/bsaci/rhinitis
2. Management of allergic and non-allergic rhinitis: BSACI guidelines (2008)
http://onlinelibrary.wiley.com/doi/10.1111/j.1365-2222.2007.02888.x/pdf
APPROVAL PROCESS
Written by: Mr Jassar, ENT Consultant, HEY
Consultation process: Dr P Gordins, Consultant Immunologist; Dr B Fernandes, Consultant
Allergist HEY
Approved by: Medicines Management Interface Group (Dec 16)
Ratified by: HERPC July 2017
Review date: July 2020
Prescribing Guideline for Rhinitis
Date approved HERPC: July 2017 Review: July 2020 Page 4 of 5
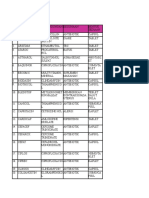
Figure 1. Management or rhinitis
Prescribing Guideline for Rhinitis
Date approved HERPC: July 2017 Review: July 2020 Page 5 of 5
You might also like
- Sample Community Pharmacy Intern Training PlanDocument20 pagesSample Community Pharmacy Intern Training PlanAmatou ASSAMII EL HADRAOUINo ratings yet
- Pharma MnemonicsDocument27 pagesPharma MnemonicsPraveen KumarNo ratings yet
- Drug ClearanceDocument65 pagesDrug ClearanceSyed Umair100% (1)
- Potential Hazards of Drugs For General PublicDocument14 pagesPotential Hazards of Drugs For General Publicnarutouzamaki59% (17)
- Allergic RhinitisDocument55 pagesAllergic RhinitisZZNo ratings yet
- Allergic PDFDocument17 pagesAllergic PDFSiska HarapanNo ratings yet
- Jurding Sabrina Tasya W - 30101800159 (Allergic Rhinitis)Document34 pagesJurding Sabrina Tasya W - 30101800159 (Allergic Rhinitis)NAUFAL ADI PAMUNGKASNo ratings yet
- Allergic RhinitisDocument53 pagesAllergic RhinitisYousfNo ratings yet
- Upper Respiratory Disorders: ObjectivesDocument16 pagesUpper Respiratory Disorders: ObjectivesJennie QuachNo ratings yet
- Acfrogcmuqv1z T0qaucxvbfwtfin2xu Xkrzp4ddeso7qwbd Fha38sq6mihfw2aozwxn5r0mxgmgmkvemhr46tntlwea3quddq9w2pmvyn6by5wqcyi7ge8gmmnzlzhis 1dzejbeghuvr9bapDocument7 pagesAcfrogcmuqv1z T0qaucxvbfwtfin2xu Xkrzp4ddeso7qwbd Fha38sq6mihfw2aozwxn5r0mxgmgmkvemhr46tntlwea3quddq9w2pmvyn6by5wqcyi7ge8gmmnzlzhis 1dzejbeghuvr9bapFareed KhanNo ratings yet
- p13 RhinitisDocument4 pagesp13 RhinitisJery VanegasNo ratings yet
- Diagnosis and Treatment of Allergic RhinitisDocument11 pagesDiagnosis and Treatment of Allergic RhinitisJustineValJadeLacabaNo ratings yet
- Managementofrhinitis: Guidelines, Evidence Basis, Andsystematic Clinicalapproachfor WhatwedoDocument16 pagesManagementofrhinitis: Guidelines, Evidence Basis, Andsystematic Clinicalapproachfor WhatwedoIndra ApriantoNo ratings yet
- Allergic Rhinitis: PathophysiologyDocument28 pagesAllergic Rhinitis: Pathophysiologysneh1509No ratings yet
- Allergic Rhinitis: University of Michigan Guidelines For Health System Clinical CareDocument12 pagesAllergic Rhinitis: University of Michigan Guidelines For Health System Clinical Carerko_akibNo ratings yet
- Allergic Rhinitis FinalDocument9 pagesAllergic Rhinitis FinalDrAyushi Aggarwal AshiNo ratings yet
- Treatment of Allergic RhinitisDocument21 pagesTreatment of Allergic RhinitisLee Ji MinNo ratings yet
- Allergic Rhinitis - University of MichiganDocument12 pagesAllergic Rhinitis - University of MichiganarsyiadlinaNo ratings yet
- Rhinitis Allergic: Elma Wiliandini G4A020043Document10 pagesRhinitis Allergic: Elma Wiliandini G4A020043elma wiliandiniNo ratings yet
- Rhinitis: The Pharmacist's RoleDocument6 pagesRhinitis: The Pharmacist's RoleOkmaronab FebrizaNo ratings yet
- ODT LevocetirizinDocument6 pagesODT LevocetirizinThanh Huy LeNo ratings yet
- Antihistamine BlockersDocument12 pagesAntihistamine Blockersyra capiliNo ratings yet
- Allergic Rhinitis in ChildhoodDocument67 pagesAllergic Rhinitis in Childhoodmp1a1234No ratings yet
- Non-Allergic RhinitisDocument9 pagesNon-Allergic RhinitisDeden SiswantoNo ratings yet
- Side Effects of Retinoid Therapy On The Quality of Vision: DOI: 10.1515/acph-2016-0039Document8 pagesSide Effects of Retinoid Therapy On The Quality of Vision: DOI: 10.1515/acph-2016-0039Ulul AzmiNo ratings yet
- CPC Module 3 Sinusitis and PneumoniaDocument12 pagesCPC Module 3 Sinusitis and PneumoniahevinpatelNo ratings yet
- Acute Respiratory Tract Infections in ChildrenDocument31 pagesAcute Respiratory Tract Infections in ChildrenNaushad AlamNo ratings yet
- CH 014 Allergic RhinitisDocument8 pagesCH 014 Allergic Rhinitishai1No ratings yet
- Bp1 Sgd1: TopicsDocument7 pagesBp1 Sgd1: TopicsAlan Joseph BaldovinoNo ratings yet
- Aria - in - The - Pharmacy 2002Document15 pagesAria - in - The - Pharmacy 2002emmanuellagrace06No ratings yet
- Urticaria, Angioedema, and Anaphylaxis AGO 2020Document12 pagesUrticaria, Angioedema, and Anaphylaxis AGO 2020Elizabeth HendersonNo ratings yet
- Journal Reading Allergic RhinitisDocument39 pagesJournal Reading Allergic RhinitisBimaKharismaNo ratings yet
- Fun and Colorful Parts of The Nose Science PresentationDocument27 pagesFun and Colorful Parts of The Nose Science PresentationZZNo ratings yet
- Anti Allergic DrugsDocument18 pagesAnti Allergic Drugsaamer niaziNo ratings yet
- Top 10 Perlas Clã Nicas en Acne Dermatologic Clinics 2015Document11 pagesTop 10 Perlas Clã Nicas en Acne Dermatologic Clinics 2015Yulay HBNo ratings yet
- Allergic RhinitisDocument3 pagesAllergic Rhinitisapi-3822433No ratings yet
- Urticaria AnaphylaxisDocument12 pagesUrticaria AnaphylaxismanchalunaNo ratings yet
- Tratamiento de Emg de AnafilaxiaDocument8 pagesTratamiento de Emg de AnafilaxiaGuissela Montoya LopezNo ratings yet
- Allergic RhinitisDocument24 pagesAllergic RhinitisENTERTAINMENT WORLDNo ratings yet
- Comparison of Fluticasone Furoate and Cetirizine Vs Fluticasone Furoate and Montelukast in Allergic RhinitisDocument8 pagesComparison of Fluticasone Furoate and Cetirizine Vs Fluticasone Furoate and Montelukast in Allergic RhinitisFuad hadyanNo ratings yet
- Allergic 2Document5 pagesAllergic 2EiynaMaulydhaNo ratings yet
- VerdeDocument24 pagesVerdeRaluca Andreea AxinteNo ratings yet
- Journal Reading - Allergic Rhinitis - Safira AmaliaDocument34 pagesJournal Reading - Allergic Rhinitis - Safira AmaliasafiraNo ratings yet
- International Journal of Pharma and Bio Sciences: Corresponding AuthorDocument6 pagesInternational Journal of Pharma and Bio Sciences: Corresponding AuthorDavid Restu Prasetia ManikNo ratings yet
- Allergic RhinitisDocument30 pagesAllergic RhinitisNoor Al AhmadNo ratings yet
- Lo 4 Sk1 Rhinitis AlergiDocument4 pagesLo 4 Sk1 Rhinitis AlergiFullyNo ratings yet
- Acute Allergic RhinitisDocument6 pagesAcute Allergic RhinitiskrisnawatiNo ratings yet
- FTX Infeksi JamurDocument64 pagesFTX Infeksi JamurNafisah SofiaNo ratings yet
- Vasomotor Rinitis Ncbi PDFDocument8 pagesVasomotor Rinitis Ncbi PDFrahmat khairulNo ratings yet
- Allergic RhinitisDocument8 pagesAllergic RhinitisJuanNo ratings yet
- Rinitis Alergi Only DR - SPH 2Document34 pagesRinitis Alergi Only DR - SPH 2ezradamanikNo ratings yet
- Angioedema Pics 2012 0425 BDocument86 pagesAngioedema Pics 2012 0425 BSuhada AkmalNo ratings yet
- O H C Hiv-I P: RAL Ealth Omplicationsinthe Nfected AtientDocument14 pagesO H C Hiv-I P: RAL Ealth Omplicationsinthe Nfected AtientTemesgen EndalewNo ratings yet
- Common Antacid Medication-Ranitidine Causing A Rare Serious Adverse EffectDocument3 pagesCommon Antacid Medication-Ranitidine Causing A Rare Serious Adverse EffectL ANo ratings yet
- Antihistamines Case StudyDocument5 pagesAntihistamines Case StudySpaynkterNo ratings yet
- Pharmacotherapy Allergic RhinitisDocument32 pagesPharmacotherapy Allergic RhinitisJambo BuneNo ratings yet
- CetirizineDocument2 pagesCetirizineDanielle Marie SamblacenoNo ratings yet
- CPG On Allergic Rhinitis 2Document8 pagesCPG On Allergic Rhinitis 2mkct111No ratings yet
- Allergic Rhinitis: Yucheng YangDocument22 pagesAllergic Rhinitis: Yucheng YangNidya PutrijNo ratings yet
- Allergology InternationalDocument15 pagesAllergology InternationalAndarvinka EvandraNo ratings yet
- RhinosinusitisDocument45 pagesRhinosinusitisMuhammad Ade RahmanNo ratings yet
- Allergic RhinitisDocument22 pagesAllergic RhinitissuciNo ratings yet
- Drug StudyDocument5 pagesDrug StudyJohn Cyprian AbeloNo ratings yet
- Fast Facts: Respiratory Allergies: Understand aeroallergens, improve treatment responseFrom EverandFast Facts: Respiratory Allergies: Understand aeroallergens, improve treatment responseNo ratings yet
- Aadal 2016Document8 pagesAadal 2016EricaNo ratings yet
- Madrid ReportDocument58 pagesMadrid ReportEricaNo ratings yet
- 4 Principles of Fracture Fixation - HandoutDocument12 pages4 Principles of Fracture Fixation - HandoutMuhammad Yasir Ahmad Muslim100% (1)
- Poster HTSDocument2 pagesPoster HTSEricaNo ratings yet
- Ni Hms 449614Document6 pagesNi Hms 449614EricaNo ratings yet
- PCH 10335Document3 pagesPCH 10335EricaNo ratings yet
- First Page PDFDocument1 pageFirst Page PDFEricaNo ratings yet
- Ni Hms 449614Document6 pagesNi Hms 449614EricaNo ratings yet
- 2015 01 17 Homework KeyDocument3 pages2015 01 17 Homework KeyEricaNo ratings yet
- Lirik Lagu Dandelion PromiseDocument3 pagesLirik Lagu Dandelion PromiseEricaNo ratings yet
- PDF Module 9 Antihyperlipidemic DrugsDocument6 pagesPDF Module 9 Antihyperlipidemic DrugsAJ VitangculNo ratings yet
- CRRT Antibiotic DosingDocument8 pagesCRRT Antibiotic DosingFranz Josef TariganNo ratings yet
- BioassayDocument38 pagesBioassayMuhammad Masoom AkhtarNo ratings yet
- Nama ObatDocument49 pagesNama ObatDwianti Lestari IINo ratings yet
- Treatment of Migraine Attacks and Prevention of MiDocument40 pagesTreatment of Migraine Attacks and Prevention of MiHemi Amalia AmirullahNo ratings yet
- Vims-Vas Biyong 1-12-2022Document122 pagesVims-Vas Biyong 1-12-2022Julia JacoboNo ratings yet
- 2018 DPRI Booklet Nov-19-18Document34 pages2018 DPRI Booklet Nov-19-18Michelle Anne Ramirez GalangaNo ratings yet
- Allergic RhinitisDocument8 pagesAllergic RhinitisJuanNo ratings yet
- Calcium GluconateDocument1 pageCalcium GluconateMary Reigns BuhatNo ratings yet
- TDM Dan Rancangan Aturan DosisDocument37 pagesTDM Dan Rancangan Aturan Dosisadelin ransunNo ratings yet
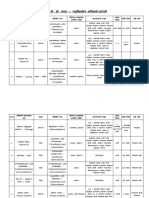
- डॉक्टर कदम पशुवैद्यकीय अधिकारी सांगली PDFDocument9 pagesडॉक्टर कदम पशुवैद्यकीय अधिकारी सांगली PDFSandy ManchareNo ratings yet
- ABL BrochureDocument8 pagesABL BrochureSairam EdupugantiNo ratings yet
- Regulatory Affairs Training - Mod 3Document95 pagesRegulatory Affairs Training - Mod 3Sunil Kumar100% (1)
- Daftar Obat High AlertDocument2 pagesDaftar Obat High Alertayu aNo ratings yet
- Opioid Lawsuit Carr v. Manufacturers and DistributorsDocument114 pagesOpioid Lawsuit Carr v. Manufacturers and DistributorsepraetorianNo ratings yet
- Drug StudyDocument32 pagesDrug StudyPrincess Gutierrez RositaNo ratings yet
- Ampule Box WipDocument1 pageAmpule Box WipCaryl Franchette SamsonNo ratings yet
- DRUG STUDY - AnticonvulsantsDocument1 pageDRUG STUDY - AnticonvulsantsZam PamateNo ratings yet
- May 07 Hippos InfoDocument9 pagesMay 07 Hippos InfonovitalumintusariNo ratings yet
- Detail Sertifikat TKDN Obat ObatanDocument116 pagesDetail Sertifikat TKDN Obat Obatannakes puskesmas Kecamatan Cempaka PutihNo ratings yet
- LGC AXIO PT Application Form Booklet Clinical 2022 SterlingDocument36 pagesLGC AXIO PT Application Form Booklet Clinical 2022 SterlingAsraf HashmiNo ratings yet
- Nclex PharmaDocument22 pagesNclex Pharmakennedy14344No ratings yet
- All Caps Formulary 09-03-2012-2003formatDocument806 pagesAll Caps Formulary 09-03-2012-2003formatasgbalajiNo ratings yet
- Price List Ogb KF 2021Document25 pagesPrice List Ogb KF 2021rianNo ratings yet
- Antpyretic-Analgesic and Antinlammatory DrugsDocument38 pagesAntpyretic-Analgesic and Antinlammatory DrugskasondaNo ratings yet
- 06 Kinetics of Elimination-1Document12 pages06 Kinetics of Elimination-1Rohit SahNo ratings yet