Professional Documents
Culture Documents
Metabolic Changes Associated With Antipsychotic Use: Joseph A. Lieberman, III, M.D., M.P.H
Uploaded by
MerlintaOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Metabolic Changes Associated With Antipsychotic Use: Joseph A. Lieberman, III, M.D., M.P.H
Uploaded by
MerlintaCopyright:
Available Formats
Joseph A.
Lieberman, III
Metabolic Changes Associated With Antipsychotic Use
Joseph A. Lieberman, III, M.D., M.P.H.
In the United States, the risk of type 2 diabetes is currently growing to epidemic proportions, with
many physicians unaware that disorders such as schizophrenia and bipolar disorder naturally place
patients at an increased risk for diabetes. Another serious concern for physicians is the development of
metabolic syndrome, also known as syndrome X, in patients suffering from schizophrenia. Metabolic
syndrome often encompasses medical conditions such as weight gain, hypertriglyceridemia, and
increased insulin, glucose, and low-density lipoprotein cholesterol levels. Treatment with atypical
antipsychotics may increase the risk of metabolic syndrome and diabetes, and physicians need to be
proactive when treating patients with schizophrenia. Physicians should be aware that the treatment of
schizophrenia involves the right balance for the patient in terms of adverse effects versus benefit, and
failing to treat a patient’s mental illness because of potential medical problems may place the patient
at an increased risk for more serious problems.
(Prim Care Companion J Clin Psychiatry 2004;6[suppl 2]:8–13)
I n the United States, the risk of type 2 diabetes is
growing to epidemic proportions. Today, physicians
are more attuned to the risk of diabetes among patients,
Although it is thought that a patient’s genetic makeup
and environment may directly contribute to metabolic syn-
drome,2 it is unknown why some patients will develop
but many physicians are unaware that disorders such as metabolic syndrome while others will not. Insulin resis-
schizophrenia and bipolar disorder are associated with in- tance and obesity are considered to be integral elements in
creased risk of diabetes. The use of atypical antipsychotics the development of metabolic syndrome,2 but accumulat-
may also place patients at risk for a complicated disorder ing evidence suggests that simply varying degrees of insu-
known as metabolic syndrome. Physical changes such as lin resistance may be the common etiological factor for the
weight gain may be an indication of metabolic side effects individual components of metabolic syndrome.1
in patients treated with antipsychotics. Physicians treating While metabolic syndrome itself is a serious health risk
patients with psychiatric disorders need to be attuned to and medical complication, research3,4 suggests that meta-
physical changes that may be a sign of serious medical bolic syndrome may place patients at an increased risk for
conditions such as diabetes or metabolic syndrome. other serious medical diseases such as heart disease. In
one study by Isomaa and colleagues,4 the risk of cardio-
METABOLIC SYNDROME vascular disease associated with metabolic syndrome was
analyzed in 4483 subjects aged 35 to 70 years. The risk
The use of antipsychotics increases the risk not only of coronary heart disease and stroke was found to
of diabetes but also of metabolic syndrome, which is be tripled among subjects with metabolic syndrome
sometimes referred to as syndrome X. While a standard as compared with those who did not have metabolic
definition of metabolic syndrome does not exist, meta- syndrome (p < .001). Cardiovascular mortality was as-
bolic syndrome is generally thought to include weight sessed in a median follow-up of 6.9 years in 3606 of the
gain and hypertriglyceridemia along with increased participants and was found to be increased among partici-
insulin, glucose, and low-density lipoprotein cholesterol pants diagnosed with metabolic syndrome when compared
levels (Table 1).1 with participants who were not diagnosed with metabolic
syndrome (p < .001).
RISK FACTORS FOR METABOLIC SYNDROME
From Jefferson Medical College, Philadelphia, Pa.
This article was derived from the planning roundtable Abnormalities in glucose regulation were first reported
“Using Atypical Antipsychotics in Primary Care,” which was in patients with schizophrenia and bipolar disorder prior to
held June 2–4, 2002, in Washington, D.C., and supported by an
unrestricted educational grant from Janssen Pharmaceutica, the introduction of antipsychotic medication, with early
L.P. reports5,6 indicating a pattern of insulin resistance in un-
Corresponding author and reprints: Joseph A. Lieberman,
III, M.D., M.P.H., 2 Aston Circle, Hockessin, DE 19707–2500 treated patients. However, treatment with antipsychotic
(email: jlieberman@jalmd.com). medications is also associated with weight gain, impaired
8 Prim Care Companion J Clin Psychiatry 2004;6 (suppl 2)
Metabolic Changes Associated With Antipsychotic Use
Table 1. Features of Metabolic Syndromea Figure 1. Weight Gain as a Function of Druga
Impaired glucose regulation or diabetes
90 Clozapine
Insulin resistance
Olanzapine
Raised arterial pressure ≥ 160/90 mm Hg 80 Risperidone
Raised plasma triglyceride levels, raised LDL Sertindole
cholesterol level, and/or low HDL cholesterol level 70 Haloperidol
Percentage of Subjects
Central obesity and/or BMI > 30 kg/m2
Microalbuminuria 60
a
Data from Alberti and Zimmet.1 50
Abbreviations: BMI = body mass index, HDL = high density
lipoprotein, LDL = low-density lipoprotein. 40
30
glucose metabolism, exacerbation of existing type 1 and 20
type 2 diabetes, new onset of type 2 diabetes mellitus, and 10
diabetic ketoacidosis.7,8 The onset of one or all of these
0
side effects increases the probability of patients develop- No Change, < 10% ≥ 10%
ing metabolic syndrome; patients displaying these side ef- or Lost Weight Weight Gain Weight Gain
fects should be monitored carefully. Weight Gain From Baseline to Maximum Weight, %
a
Reprinted with permission from Wirshing et al.11
Weight Gain
Weight gain may be the most noticeable signal of meta-
bolic syndrome and is usually the most distressing issue
among patients. Physicians should view dramatic weight diagnosis, weight changes, duration of treatment, and inpa-
gain as a red flag for complicating medical issues. Even tient status. Participants were required to weigh themselves
without the development of diabetes or metabolic syn- and report weight at each visit (every 1 to 4 weeks). A fail-
drome, significant weight gain associated with antipsy- ure to maintain weight was defined as an increase of
chotic treatment may compromise a patient’s health by at least 10 lb [4.5 kg]. Participants who failed to maintain
contributing to comorbid conditions such as hypertension weight were first instructed to keep a detailed food diary,
and coronary artery disease.9 and those who subsequently were unable to maintain
Atypical antipsychotics have been frequently cited as weight were then referred to the “wellness clinic” in which
causing a higher increase in weight gain than conventional participants were involved in a more rigorous evaluation of
antipsychotics. In a randomized, 10-week, parallel-group, both dietary and exercise habits along with educational and
double-blind trial,10 the effects of the atypical agent cloza- exercise classes and group support meetings. Clozapine-
pine and the conventional agent haloperidol on weight and olanzapine-treated patients demonstrated the highest
gain were tested. Participants were stable outpatients who maximal weight gain and also gained weight over a greater
met the DSM-III-R criteria for chronic schizophrenia. period of time when compared with other treatments.
Nineteen patients who were prescribed clozapine and 20 Risperidone-treated patients were found to have an inter-
patients who were prescribed haloperidol were weighed mediate amount of weight gain, and sertindole-treated pa-
weekly, and their ideal weight was calculated, considering tients gained less weight than haloperidol-treated patients
gender and height. After 10 weeks, the clozapine group (Figure 1).
gained 7% over their baseline measurement (absolute
weight gain of 11.7 lb [5.3 kg]) while the haloperidol Hyperglycemia and Glucose Levels
group gained 1% over baseline (absolute weight gain, 1.5 Hyperglycemia and impaired glucose levels are
lb [0.68 kg]). often seen in patients suffering from diabetes or metabolic
The amount of drug-induced weight gain varies among syndrome. Atypical antipsychotics can increase the risk
atypical antipsychotics. In a retrospective analysis of 122 of hyperglycemia and impaired glucose levels and sub-
clinical records, Wirshing and colleagues11 studied the in- sequently increase the risk of metabolic syndrome. The
crease of weight during antipsychotic treatment with the development of hyperglycemia should be regarded as a
assistance of weight maintenance programs in patients serious medical condition since diabetic ketoacidosis—a
with a DSM-III-R diagnosis of schizophrenia. Male par- severe, potentially fatal medical disturbance—is character-
ticipants (N = 92) from 8 clinical drug trials that were con- ized by the presence of hyperglycemia.7
ducted over a 6-year period were included in the study. Individual cases12,13 have shown marked hyperglycemia
The clinical drug trials included in the analysis comprised in patients taking clozapine and olanzapine, although these
patients treated with haloperidol and the atypical agents cases are extreme. In one case,13 a 41-year-old black man
risperidone, clozapine, olanzapine, and sertindole. Medi- with a 23-year history of treatment-refractory schizophre-
cal charts were collected to review data on age, ethnicity, nia and no past history of diabetes or glucose intolerance
Prim Care Companion J Clin Psychiatry 2004;6 (suppl 2) 9
Joseph A. Lieberman, III
Figure 2. Plasma Glucose Values at Fasting and Postload Table 2. Risk Factors for Diabetes Mellitus in Patients With
Time Pointsa Mental Illnessa
200
Psychiatric diagnosis Schizophrenia or other neuropsychiatric
Control *
disorder
Plasma Glucose Level, Mean ± SE, mg/dL
Typical Antipsychotic
180 * Obesity (high BMI) Increasing BMI increases the risk: > 20%
Risperidone
Clozapine over desired weight or BMI > 27 kg/m2
160 Olanzapine Race/ethnicity Native Americans, Asian Indians,
* Australian Aborigines, Mexican
140
Americans, Hispanics, Polynesians and
120 Micronesians, and African Americans
100
* Hypertension Blood pressure above 140/90 mm Hg
Lipid level abnormalities Low HDL cholesterol or high triglyceride
80 levels (atypical antipsychotic agents
may contribute to this)
60 Family history First-degree relatives with diabetes
40 (genetic predisposition)
Diet Generally poor food choices
20 Inactivity Antipsychotic agents may cause
0
sedation/fatigue and reduce activity
0 15 45 75 Antipsychotic agents Low-potency conventional agents and
Time, min atypical agents
a
Data from Henderson.15
a
Reprinted with permission from Newcomer et al.14 Abbreviations: BMI = body mass index, HDL = high-density
*p < .05. lipoprotein.
was administered clozapine. Clozapine was slowly in- sured time points in comparison with untreated healthy
creased to 450 mg b.i.d. over 2 months. The patient was control subjects and patients receiving typical antipsy-
also taking ranitidine and benztropine. After 2 months, the chotics.14 Clozapine-treated patients had significant eleva-
patient had marked hyperglycemia and was given a regi- tions in fasting and 75-minute postload plasma glucose
men of insulin. Soon thereafter, clozapine treatment was levels. Risperidone-treated patients had elevations in fast-
tapered over a 1-week period and then discontinued. The ing and 75-minute postload levels, but only when com-
patient’s serum glucose levels were noted to be signifi- pared with healthy subjects. When risperidone was com-
cantly lower after the discontinuation of clozapine, which pared with typical antipsychotics, no significant difference
shortly resulted in a decrease and then discontinuation of in plasma glucose levels was seen. A significant difference
insulin treatment. was also not found between typical antipsychotic–treated
One study14 observed the changes in fasting plasma patients and healthy subjects (Figure 2).
glucose levels in 48 patients diagnosed with schizophrenia
and 31 healthy controls. Subjects were divided into 5 Diabetes and Diabetic Ketoacidosis
groups: participants treated with typical antipsychotics, Patients with mental illness are at an increased risk to
clozapine, olanzapine, or risperidone, and healthy sub- develop diabetes, regardless of antipsychotic use15; how-
jects. Groups were matched for body mass index (BMI), ever, a recent analysis16 of prescription claims for patients
age, and ethnicity. Participants were excluded if they suf- receiving diabetes-related medications and antipsychotic
fered from an Axis I disorder other than schizophrenia, medications suggests that patients with schizophrenia suf-
had a substance abuse problem occurring less than 6 fer from an increased rate of type 2 diabetes mellitus when
months before study entry, or had any of the following: compared with the general population. This increase was
medical conditions that could confound glucose regulation largely independent of which antipsychotic medication pa-
assessments including a history of diabetes; a recurring tients were prescribed.
cardiovascular or respiratory condition; epilepsy; endo- The onset of diabetes tends to occur within the first few
crine disease; current fever; dehydration; nausea; a body months of treatment with atypical antipsychotics. A recent
weight of less than 80% of ideal; pregnancy; high-dose es- meta-analysis17 of 45 published cases of new-onset diabe-
trogen therapy; narcotic, corticosteroid, or spironolactone tes and diabetic ketoacidosis over a 21-year period found
therapy; sedative hypnotic withdrawal; or any changes the highest increase of new diabetes cases (45%) within
in medication within the last 10 days. Modified oral glu- the first 1 to 3 months after the initiation of atypical anti-
cose tolerance tests were used with fasting baseline and psychotic treatment. Physicians need to closely monitor
multiple postload plasma samples for glucose, insulin, all patients when initiating an atypical antipsychotic treat-
c-peptide, glucagon, and cortisol. Postload samples were ment as well as continuously monitor patients who present
taken at 15, 45, and 75 minutes. 1 or more risk factors for diabetes (Table 2).
Olanzapine-treated patients had significant elevations Mukherjee and colleagues18 observed the prevalence of
in fasting and postload plasma glucose levels at all mea- diabetes in 95 residents aged 45 to 74 years in a long-term
10 Prim Care Companion J Clin Psychiatry 2004;6 (suppl 2)
Metabolic Changes Associated With Antipsychotic Use
Figure 3. Percentage of Patients With Schizophrenia in a specialty mental health outpatient clinic. For inclusion
Receiving Prescriptions for Atypical and Typical Neuroleptic in the study, participants had to have been prescribed either
Medication Who Also Had a Diagnosis of Diabetes Mellitusa a conventional antipsychotic or clozapine, risperidone,
Patients receiving typical neuroleptics (N = 15,984) quetiapine, or olanzapine at least 4 months prior to the
30 Patients receiving atypical neuroleptics (N = 22,648) study. The typical and atypical antipsychotic groups were
Schizophrenia Patients Diagnosed
further divided into 5 age groups: under 40 years, 40 to 49
25
With Diabetes Mellitus, %
d years, 50 to 59 years, 60 to 69 years, and over 70 years. Pa-
20 tients treated with atypical antipsychotics had a signifi-
c cantly higher rate of diagnosis of diabetes among the 3
15 younger age groups during treatment (Figure 3). For ex-
ample, the under-40 age group had an 8.7% rate of diabetes
10 b
when prescribed atypicals, compared with a 6.43% rate
5 with typical antipsychotics (p < .07). Also, the risk of being
diagnosed with diabetes was greater in all age groups of
0 patients treated with clozapine, olanzapine, and quetiapine
All Ages < 40 40–49 50–59 60–69 ≥ 70
than with typical agents or risperidone.
Age, y
a
Reprinted with permission from Sernyak et al.19 RISKS VERSUS BENEFITS
χ = 7.24, df = 1, p < .07.
b 2
χ = 9.81, df = 1, p = .002.
c 2 OF ANTIPSYCHOTIC TREATMENT
χ = 8.53, df = 1, p = .003.
d 2
Despite the risk of potentially serious medical condi-
tions, clinicians need to treat the mental disorder. The treat-
care facility who met the DSM-III-R criteria for schizo- ment of schizophrenia involves the right balance for the pa-
phrenia. Inclusion criteria included no history of alcohol tient in terms of adverse effects versus benefit. Failing to
or drug use within the last year or endocrine disorders treat a patient because of the risk of or complications from
other than diabetes. Subjects were excluded if they had an diabetes places the patient at a higher risk for more serious
onset of psychosis after age 40 years, a history of severe problems. Studies15,18 have demonstrated that even un-
head injury preceding psychosis, a history of seizure disor- treated patients suffering from schizophrenia are at an in-
der, any other neurologic disorder, or severe cognitive im- creased risk of developing medical conditions associated
pairment. Eight of the participants had not been prescribed with metabolic syndrome.
an antipsychotic treatment for at least 1 year and 87 had The quality of life associated with schizophrenia ranks
been treated continuously for at least 2 years. Diagnosis among the worst of any chronic medical illness, and treat-
of diabetes was based on a review of patients’ medical ment with atypical antipsychotics may improve the quality
records and criteria set forth by the World Health of life for many patients.20 The greatest advantage of atypi-
Organization. All patients diagnosed with diabetes had a cal antipsychotics is their ability to improve cognition,
record of fasting plasma glucose levels greater than 140 since impaired cognition is now considered to be a funda-
mg/dL on at least 2 occasions. mental feature of schizophrenia.20 Atypical antipsychotics
The overall prevalence of diabetes was 15.8%, and have been shown to significantly improve many aspects of
a significant difference was not found between age and cognitive function,21 including executive function, verbal
gender and the prevalence of diabetes. However, untreated fluency, attention, and memory and learning impairment.22
patients were reported to have a higher prevalence of Atypical antipsychotics have also been shown to be effec-
diabetes than treated patients. tive in treating depression, as both a monotherapy and an
Although Mukherjee and colleagues studied older adjunct to antidepressant therapy.23–25
adults, other studies19 suggest that type 2 diabetes develops It is arguable that the benefits of antipsychotic treatment
more frequently among younger schizophrenic patients outweigh the risks. However, physicians must weigh the
treated with atypical antipsychotics. However, research risks and benefits for each patient before beginning an anti-
has yet to determine whether reported cases of early-onset psychotic treatment. The patient and physician must work
type 2 diabetes are caused by the presence of atypical anti- together to outline potential risk factors and to carefully
psychotic treatment or merely a quickening of the natural monitor risks during treatment.
development of the disease in these patients.19
Sernyak et al.19 observed the development of types 1 MONITORING AND MANAGING
and 2 diabetes among 38,632 participants treated with METABOLIC SYNDROME
atypical and typical antipsychotics. Participants were re-
quired to have received either a primary or secondary When treating an at-risk patient, physicians need to be
diagnosis of schizophrenia from at least 2 outpatient visits especially vigilant in monitoring antipsychotic medication.
Prim Care Companion J Clin Psychiatry 2004;6 (suppl 2) 11
Joseph A. Lieberman, III
Table 3. Monitoring Tips for Metabolic Syndromea Table 4. Management Tips for Antipsychotic Treatmenta
Weigh patients and track BMI at each visit Refer patients with abnormal glucose or lipid levels for medical
Take a history and record whether known risk factors are present or consultation
absent at baseline and monitor at regular intervals Encourage weight loss. Even a modest weight loss can have health
Get a baseline fasting glucose level and lipid profile for psychiatric benefits
patients who have a BMI ≥ 27 kg/m2 and who are treated with Be alert to the possibility of diabetic ketoacidosis, especially in
psychotropic drugs, then track glucose and lipid levels at regular diabetic patients newly begun on atypical antipsychotics
intervals, especially if further weight gain occurs Leverage your therapeutic rapport to establish moderate exercise and
Monitor glucose levels frequently, including shortly after beginning a discourage smoking whenever possible
new antipsychotic agent and when treating a diabetic patient Consider discontinuing the antipsychotic, because it may resolve
a
Data from Stahl.26 hyperglycemia and diabetes in some cases
a
Abbreviation: BMI = body mass index. Data from Stahl.26
Simple monitoring and management tips can aid physi- CONCLUSION
cians in handling potential medical complications (Tables
3 and 4). While the onset of weight gain, hyperglycemia, in-
At least 10 million Americans at high risk for type creased glucose levels, or diabetes may be signs or symp-
2 diabetes can sharply lower their chances of getting the toms of antipsychotic-induced metabolic syndrome, phy-
disease with diet and exercise.27 With the increased sicians should nevertheless continue to treat a patient’s
emergence of diabetes and metabolic syndrome, clinicians mental disorder. Careful monitoring of at-risk patients
should consider screening for hyperlipidemia or hypergly- may aid in the prevention of metabolic syndrome as well
cemia annually and prior to starting or changing an anti- as the management of any potential symptoms should they
psychotic treatment.7 Physicians should also consider occur. With patients suffering from schizophrenia at an
treatments for lipid dysfunction and weight gain if they already increased risk for diabetes, the advantages and
emerge during antipsychotic treatment. disadvantages of any antipsychotic treatment must be
Although a dose-response relationship for weight gain weighed before initiating treatment in a patient.
has not been established, the development of hyperglyce-
mia after the initiation of or increase in antipsychotic dose Drug names: benztropine (Cogentin and others), clozapine (Clozaril
and others), haloperidol (Haldol and others), olanzapine (Zyprexa),
could signal a problem. Likewise, physicians who have quetiapine (Seroquel), ranitidine (Zantac and others), risperidone
been worried about metabolic issues with a patient on anti- (Risperdal), spironolactone (Aldactone and others).
psychotic treatment should increase monitoring when rais-
Disclosure of off-label usage: The author of this article has determined
ing the dose. that, to the best of his knowledge, sertindole is not approved for use in
Weight gain is often the most visible side effect of anti- the United States.
psychotic treatment and therefore can often be the easiest
to manage. Physicians should not only weigh patients REFERENCES
at regular visits but also pay attention to an increase in
1. Alberti K, Zimmet P. Definition, diagnosis, and classification of diabetes
weight and be proactive in advising patients. Most patients mellitus and its complications, pt 1: diagnosis and classification of diabe-
treated with antipsychotics are at risk to gain 5 lb [2.25 kg] tes mellitus provisional report of a WHO consultation. Diabet Med
to 7 lb [3.15 kg]. This weight, while perhaps cosmetically 1998;15:539–553
2. Liese A, Mayer-Davis E, Haffner S. Development of the multiple meta-
undesirable, is much easier to manage and less of a health bolic syndrome: an epidemiologic perspective. Epidemiol Rev
risk than 30 lb [13.5 kg] or 40 lb [18 kg]. What physicians 1998;20:157–172
do not want to see is dramatic weight gain, such as 30 to 3. American Heart Association. Syndrome X or metabolic syndrome. Avail-
able at: http://www.americanheart.org/presenter.jhtml?identifier=534.
40 lb. Weight gain poses serious health risks and can be a Accessed July 29, 2003
distressing issue for the patient. Physicians should educate 4. Isomaa B, Almgren P, Tuomi T, et al. Cardiovascular morbidity and mor-
patients and their families that weight gain is possible and tality associated with the metabolic syndrome. Diabetes Care
2001;24:683–689
to be on the lookout for it. 5. Meduna L, Gerty F, Urse V. Biochemical disturbances in mental disor-
Physicians can advise patients to monitor weight by ders. Arch Neurol Psychiatry 1942;47:38–52
watching how their clothes fit, especially around the waist. 6. Raphael T, Parsons I. Blood sugar studies in dementia praecox and manic
depressive insanity. Arch Neurol Psychiatry 1921;5:687–709
Physicians might remind patients to try leaving food on 7. Haupt D, Newcomer J. Hyperglycemia and antipsychotic medications.
their plate or climbing the stairs instead of taking the el- J Clin Psychiatry 2001;62 (suppl 27):15–26
evator. With extremely impaired patients or those who al- 8. Allison DB, Mentore JL, Heo M, et al. Antipsychotic-induced weight
gain: a comprehensive research synthesis. Am J Psychiatry
ready have substantial weight gain, suggesting a nutri- 1999;156:1686–1696
tional consultation may help. Steps to treating overweight 9. Must A, Spadano J, Coakley E, et al. The disease burden associated with
and obesity in the primary care setting include measuring overweight and obesity. JAMA 1999;282:1523–1529
10. Bustillo JR, Buchanan RW, Irish D, et al. Differential effect of clozapine
height and weight, measuring waist circumference, assess- on weight: a controlled study. Am J Psychiatry 1996;153:817–819
ing comorbidities, and placing a patient on a diet. 11. Wirshing DA, Wirshing WC, Kysar L, et al. Novel antipsychotics:
12 Prim Care Companion J Clin Psychiatry 2004;6 (suppl 2)
Metabolic Changes Associated With Antipsychotic Use
comparison of weight gain liabilities. J Clin Psychiatry 1999;60:358–363 risk versus benefits of atypical antipsychotics. J Clin Psychiatry 2001;
12. Ober SK, Hudak R, Rusterholtz A. Hyperglycemia and olanzapine 62(suppl 27):35–39
[letter]. Am J Psychiatry 1999;156:970 21. Keefe RS, Silva SG, Perkins DO, et al. Effects of atypical antipsychotic
13. Kamran A, Doraiswamy PM, Jane JL, et al. Severe hyperglycemia drugs on neurocognitive impairment in schizophrenia: a review and meta-
associated with high doses of clozapine [letter]. Am J Psychiatry analysis. Schizophr Bull 1999;25:201–222
1994;151:1395 22. Collaborative Working Group on Clinical Trial Evaluations. Evaluating
14. Newcomer JW, Haupt DW, Fucetola R, et al. Abnormalities in glucose the effects of antipsychotics on cognition in schizophrenia. J Clin
regulation during antipsychotic treatment of schizophrenia. Arch Gen Psychiatry 1998;59(suppl 12):35–40
Psychiatry 2002;59:337–345 23. Ranjan R, Meltzer HY. Acute and long-term effectiveness of clozapine
15. Henderson DC. Atypical antipsychotic–induced diabetes mellitus: in treatment-resistant psychotic depression. Biol Psychiatry 1996;40:
how strong is the evidence? CNS Drugs 2002;16:77–89 253–258
16. Kwong K, Cavazzoni P, Hornbuckle K, et al. Higher incidence of diabetes 24. Hillert A, Maier W, Wetzel H, et al. Risperidone in the treatment of disor-
mellitus during exposure to antipsychotics: findings from a retrospective ders with a combined psychotic and depressive syndrome: a functional
study in the US [abstract]. Presented at the 41st Annual cohort Meeting of approach. Pharmacopsychiatry 1992;25:213–217
the New Clinical Drug Evaluation Unit; May 28–31, 2001; Phoenix, Ariz 25. Tollefson GD, Sanger TM, Beasley CM, et al. Double-blind, controlled
17. Jin H, Meyer JM, Jeste DV. Phenomenology of and risk factors for new- comparison of the novel antipsychotic olanzapine versus haloperidol or
onset diabetes mellitus and diabetic ketoacidosis associated with atypical placebo on anxious and depressive symptoms accompanying schizophre-
antipsychotics: an analysis of 45 published cases. Ann Clin Psychiatry nia. Biol Psychiatry 1998;43:803–810
2002;14:59–64 26. Stahl S. The metabolic syndrome: psychopharmacologists should weigh
18. Mukherjee S, Decina P, Bocola V, et al. Diabetes mellitus in schizo- the evidence for weighing the patient [BRAINSTORMS]. J Clin Psychiatry
phrenic patients. Compr Psychiatry 1996;37:68–73 2002;63:1094–1095
19. Sernyak MJ, Leslie DL, Alarcon RD, et al. Association of diabetes melli- 27. National Institute of Diabetes & Digestive & Kidney Disease. Diet and
tus with use of atypical neuroleptics in the treatment of schizophrenia. exercise dramatically delay type 2 diabetes: diabetes medication metfor-
Am J Psychiatry 2002;159:561–566 min also effective. Available at: http://www.niddk.nih.gov/welcome/
20. Meltzer H. Putting metabolic side effects into perspective: releases/8_8_01.htm. Accessed Aug 20, 2003
Prim Care Companion J Clin Psychiatry 2004;6 (suppl 2) 13
You might also like
- Metabolic Syndrome Program: How to Lose Weight, Beat Heart Disease, Stop Insulin Resistance and MoreFrom EverandMetabolic Syndrome Program: How to Lose Weight, Beat Heart Disease, Stop Insulin Resistance and MoreRating: 4.5 out of 5 stars4.5/5 (2)
- Diet in Metabolic Effects and Health ImplicationsDocument2 pagesDiet in Metabolic Effects and Health Implicationslightning proNo ratings yet
- Metabolic Syndrome: Learning ObjectivesDocument20 pagesMetabolic Syndrome: Learning Objectivesddeeb420% (1)
- Caroline M. Apovian - Body Weight Considerations in The Management of Type 2 DiabetesDocument15 pagesCaroline M. Apovian - Body Weight Considerations in The Management of Type 2 DiabetesFarid RakhmanNo ratings yet
- Type 2 Diabetes MellitusDocument19 pagesType 2 Diabetes MellitusFelipe Senn Guerrero100% (2)
- Manu Et Al-2015-Acta Psychiatrica ScandinavicaDocument12 pagesManu Et Al-2015-Acta Psychiatrica ScandinavicamerianaNo ratings yet
- Jbcahs 4 39Document7 pagesJbcahs 4 39miranddaelvira02No ratings yet
- Metabolic Syndrome As A Predictor of Type 2 Diabetes, and Its Clinical Interpretations and UsefulnessDocument10 pagesMetabolic Syndrome As A Predictor of Type 2 Diabetes, and Its Clinical Interpretations and UsefulnessChiranjeeviNo ratings yet
- A Guide to Diabetes: Symptoms; Causes; Treatment; PreventionFrom EverandA Guide to Diabetes: Symptoms; Causes; Treatment; PreventionNo ratings yet
- Exercise and Type 2 DiabetesDocument15 pagesExercise and Type 2 Diabetespb.nakulaNo ratings yet
- Drug Induced DiabetesDocument12 pagesDrug Induced Diabetesfawaz jaffarNo ratings yet
- A Case Report On Dietary Management of A Patient With Type 2 Diabetes MellitusDocument4 pagesA Case Report On Dietary Management of A Patient With Type 2 Diabetes MellitusJasmin RanganiNo ratings yet
- DM FinaDocument3 pagesDM FinaChared LumbaNo ratings yet
- Diabetis ThesisDocument23 pagesDiabetis ThesisHannah CaldinoNo ratings yet
- Nej M CPC 049017Document10 pagesNej M CPC 049017Bibiana Chavarro PortilloNo ratings yet
- Community Rotation - Counseling CaseDocument24 pagesCommunity Rotation - Counseling Caseapi-635948254No ratings yet
- Non-Pharmacological Treatment Options inDocument9 pagesNon-Pharmacological Treatment Options inkemal ghazaliNo ratings yet
- DD Metabolic SyndromeDocument5 pagesDD Metabolic SyndromeEluNo ratings yet
- Insulike BrochureDocument24 pagesInsulike BrochureRakesh KumarNo ratings yet
- Metabolic Syndrome - Overview and Current GuidelinesDocument12 pagesMetabolic Syndrome - Overview and Current GuidelinessserggiosNo ratings yet
- 2004 Metabolic Risk During Antipsychotic TreatmentDocument11 pages2004 Metabolic Risk During Antipsychotic TreatmentDiego HormacheaNo ratings yet
- Hypoglycemia in Diabetes: Pathophysiology, Prevalence, and PreventionFrom EverandHypoglycemia in Diabetes: Pathophysiology, Prevalence, and PreventionNo ratings yet
- Unraveling The Mysteries of Syndrome X 2003Document2 pagesUnraveling The Mysteries of Syndrome X 2003Basilharbi HammadNo ratings yet
- Case StudyDocument19 pagesCase StudyKiscica82No ratings yet
- J Yogaratnam 2013 Asia Piola PDFDocument8 pagesJ Yogaratnam 2013 Asia Piola PDFCamila RosenNo ratings yet
- Metabolic SyndromDocument11 pagesMetabolic SyndromAshaNo ratings yet
- Paisey1998 PDFDocument7 pagesPaisey1998 PDFNelson MolinaNo ratings yet
- Remisión de Diabetes 2021Document8 pagesRemisión de Diabetes 2021Maria Alejandra Quispe FloresNo ratings yet
- Management of Blood GlucoseDocument8 pagesManagement of Blood GlucoseerwanNo ratings yet
- Gudoy, Charies Jamille 12-WeierstrassDocument4 pagesGudoy, Charies Jamille 12-WeierstrasschaNo ratings yet
- Article - Ghrelin and Leptin in Insulin Resistance (CHECKED)Document6 pagesArticle - Ghrelin and Leptin in Insulin Resistance (CHECKED)pixoguiasNo ratings yet
- (Simpo 2 Dr. Sally) - Sindrom MetabolikDocument57 pages(Simpo 2 Dr. Sally) - Sindrom MetabolikYosefin RatnaningtyasNo ratings yet
- Pregnancy at Risk Preexisting ConditionsDocument39 pagesPregnancy at Risk Preexisting ConditionsMatthew RyanNo ratings yet
- Type 2 Diabetes MellitusDocument24 pagesType 2 Diabetes Mellitusdr. M.F. Romdhoni100% (1)
- IN BRIEF More Than 90% of Patients With Diabetes Have Overweight orDocument7 pagesIN BRIEF More Than 90% of Patients With Diabetes Have Overweight ornellieauthorNo ratings yet
- Diabetic Ketoacidosis in Toddler With A Diaper RashDocument4 pagesDiabetic Ketoacidosis in Toddler With A Diaper RashKarl Angelo MontanoNo ratings yet
- Diabetes Mellitus and Multiple TherapeutDocument9 pagesDiabetes Mellitus and Multiple TherapeutMOHAMMAD OVAISNo ratings yet
- Diabetes and Hyperlipidemia: A Direct Quantitative AnalysisDocument6 pagesDiabetes and Hyperlipidemia: A Direct Quantitative AnalysisAnonymous Kc2tM8No ratings yet
- Alternative Therapies For DM 2Document14 pagesAlternative Therapies For DM 2Ferc27No ratings yet
- Running Head: Alternative Medicine Nursing 1Document26 pagesRunning Head: Alternative Medicine Nursing 1MuhammadBilalSaleemNo ratings yet
- Diabetes Fundies PaperDocument7 pagesDiabetes Fundies Paperapi-315435865No ratings yet
- Anorexia Nervosa in Adults and Adolescents - The Refeeding Syndrome - UpToDateDocument10 pagesAnorexia Nervosa in Adults and Adolescents - The Refeeding Syndrome - UpToDatethelesphol pascalNo ratings yet
- Seminar: Robert H Eckel, Scott M Grundy, Paul Z ZimmetDocument14 pagesSeminar: Robert H Eckel, Scott M Grundy, Paul Z ZimmetPaulo Victor Amorim MarquesNo ratings yet
- Diabetes Case StudyDocument3 pagesDiabetes Case Studydsaitta108No ratings yet
- Diabetes Mellitus - Type 2 DiabetesDocument11 pagesDiabetes Mellitus - Type 2 DiabetesHafiz IbrahimNo ratings yet
- Diabetes Mellitus of The Human Digestive SystemDocument7 pagesDiabetes Mellitus of The Human Digestive SystemCHRISTINE KARENDINo ratings yet
- DiabetesDocument352 pagesDiabetesbeltonNo ratings yet
- Diabetes Mellitus and SchizophreniaDocument1 pageDiabetes Mellitus and SchizophreniaEndah FitriNo ratings yet
- Lifestyle Modification in The Management of The MeDocument13 pagesLifestyle Modification in The Management of The MeBhupeshNo ratings yet
- Case Presentation EndocrineDocument42 pagesCase Presentation EndocrineLéojAfallaNo ratings yet
- Obesity, A Burning Problem: Dr. Arunima Chaudhuri, Dr. Amit Kumar BandopadhyayDocument5 pagesObesity, A Burning Problem: Dr. Arunima Chaudhuri, Dr. Amit Kumar BandopadhyayIOSR Journal of PharmacyNo ratings yet
- Lipodistrofia FamiliarDocument4 pagesLipodistrofia FamiliarKaren Magalí CruzNo ratings yet
- Lindgarde 2000Document10 pagesLindgarde 2000fachry albabNo ratings yet
- Nfs 774 Case StudyDocument37 pagesNfs 774 Case Studyapi-533845626No ratings yet
- 201008barclay PDFDocument6 pages201008barclay PDFLee Chee SengNo ratings yet
- DefinitionDocument6 pagesDefinitionChana 'eLecter' ChuLumNo ratings yet
- Sindrom MetabolikDocument9 pagesSindrom MetabolikUlquiorra SchifferNo ratings yet
- Assessment & Treatment of Diabetic Emergencies: Paramedic LevelDocument12 pagesAssessment & Treatment of Diabetic Emergencies: Paramedic LevelSarah-kate PatersonNo ratings yet
- Metabolic Syndrome and DiabetesDocument6 pagesMetabolic Syndrome and DiabetesKarla MonsalvoNo ratings yet
- Psych Pabaon Nov 2022 PnleDocument9 pagesPsych Pabaon Nov 2022 PnleDarwin DerracoNo ratings yet
- Annotated BibDocument3 pagesAnnotated Bibapi-489789428No ratings yet
- Prader Willi SyndromeDocument14 pagesPrader Willi Syndromeapi-471834071No ratings yet
- HarrisonDocument18 pagesHarrisonayuliadrNo ratings yet
- IAF MD 8 2011 Application of ISO 17011 in MDQMS (ISO 13485) Issue 1 2011Document17 pagesIAF MD 8 2011 Application of ISO 17011 in MDQMS (ISO 13485) Issue 1 2011carlosprieto36No ratings yet
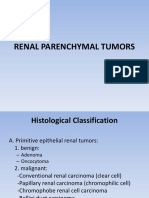
- Renal Parenchymal TumorsDocument45 pagesRenal Parenchymal TumorsDaniel100% (1)
- 06nov Dec Sf2Document14 pages06nov Dec Sf2freemedicNo ratings yet
- (Artigo) Groin Hernias in Adults Solomon. (2015)Document8 pages(Artigo) Groin Hernias in Adults Solomon. (2015)Beatriz BelottiNo ratings yet
- Lecture (2) - Pharmaceutical CareDocument38 pagesLecture (2) - Pharmaceutical CareRaju NiraulaNo ratings yet
- Pre Analytical Clot EdDocument12 pagesPre Analytical Clot EdAnonymous w4qodCJNo ratings yet
- Choosing An Enteral Feeding FormulaDocument44 pagesChoosing An Enteral Feeding FormulaMeta Hanindita NugrohoNo ratings yet
- TerminologyDocument11 pagesTerminologyMustafa SaßerNo ratings yet
- Cerebral EdemaDocument15 pagesCerebral EdemaMae FlagerNo ratings yet
- Practice Guidelines For Telemental HealthDocument51 pagesPractice Guidelines For Telemental HealthNataanatiNo ratings yet
- Pharmaceutics IntroductionDocument9 pagesPharmaceutics IntroductionVIJAY KUMAR TIRUKKACHINo ratings yet
- Drug Card ZantacDocument1 pageDrug Card ZantacAdrianne Bazo100% (1)
- Efektifitas Latihan Progressive Muscle Relaxation (PMR) Terhadap Mual Muntah Kemoterapi Pasien Kanker OvariumDocument8 pagesEfektifitas Latihan Progressive Muscle Relaxation (PMR) Terhadap Mual Muntah Kemoterapi Pasien Kanker OvariumMutmin AnsariNo ratings yet
- Case Studies of The EntrepreneursDocument14 pagesCase Studies of The EntrepreneursSneha DobariaNo ratings yet
- Drug DetoxcificationDocument23 pagesDrug DetoxcificationPUSAT LATIHAN AADKNo ratings yet
- Drug Therapy ProblemDocument19 pagesDrug Therapy ProblemAulia NorfiantikaNo ratings yet
- Metabolic Encephalopathies and Delirium: Panayiotis N. Varelas, MD, PHDDocument34 pagesMetabolic Encephalopathies and Delirium: Panayiotis N. Varelas, MD, PHDjorge_suoNo ratings yet
- 19 Nov Malam Qara Fatikha FixDocument9 pages19 Nov Malam Qara Fatikha FixatikahNo ratings yet
- TCCC Quick Reference Guide 2017Document54 pagesTCCC Quick Reference Guide 2017https://www.t-medical.orgNo ratings yet
- Pregnancy: Signs/Symptoms and Common Health ConcernsDocument5 pagesPregnancy: Signs/Symptoms and Common Health ConcernsTracy50% (2)
- Stroke StatisticsDocument13 pagesStroke StatisticsAldo EmeraldNo ratings yet
- PRESENTATION: Quality of Hospital Care in KP by Michael NiechzialDocument25 pagesPRESENTATION: Quality of Hospital Care in KP by Michael NiechzialADB Health Sector GroupNo ratings yet
- Reteplase (MIRel)Document23 pagesReteplase (MIRel)Jhoann JamanilaNo ratings yet
- 52 Healing HabitsDocument11 pages52 Healing Habitsjethro123_69No ratings yet
- Astringent Herbs Stambhana KarmaDocument4 pagesAstringent Herbs Stambhana Karmaqueencel100% (1)
- Assertiveness Training A Forgotten EvideDocument20 pagesAssertiveness Training A Forgotten EvideinicelliNo ratings yet