Professional Documents
Culture Documents
Giant Cell Fibroma of The Gingiva: A Case Report and Review of Literature
Uploaded by
AgieOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Giant Cell Fibroma of The Gingiva: A Case Report and Review of Literature
Uploaded by
AgieCopyright:
Available Formats
Giant Cell Fibroma of the Gingiva: A Case Report
and Review of
Literature
Introduction
Gingival enlargement and gingival overgrowth are common features of gingival diseases.
Weathers and Callihan were the first to describe giant cell fibroma (GCF) as a separate entity
among fibrous soft tissue lesions of the oral cavity, in the early 1970s.[1] They considered GCF
as a fibrous tumor with distinct diagnostic clinicopathological features. GCF represents
approximately 2%–5% of all oral fibrous proliferations. GCF was once hypothesized to have a
viral etiology; later, stimulus of unknown origin was believed to initiate the lesion.[2] GCF
lesion is usually seen in the young with some studies showing female preponderance.[3] Fifty
percent of all cases reported were found on the gingiva, mandibular gingiva being affected twice
more commonly than maxillary gingiva.[4,5] This case report describes a solitary fibrotic lesion
of the maxillary buccal gingiva and its surgical management.
Case Report
A 33-year-old man presented with a growth on the gums of his upper front teeth since childhood.
The growth had gradually progressed asymptomatically to the present size. The medical history
was unremarkable. Intraoral examination revealed a solitary, grayish-brown sessile overgrowth
on the labial surface of the marginal gingiva of maxillary left lateral incisor (22) measuring about
5 mm × 7 mm with no loss of attachment [Figure 1a]. The lesion was firm and fibrotic with a
rough, pebbly surface, and corrugated gingival margin. 22 occluded in crossbite with the fused
31 and 32 and exhibited wear facets suggestive of traumatic occlusion. Radiographic
examination did not reveal any associated bony changes [Figure 1b].
We made a provisional diagnosis of irritation fibroma and/or chronic inflammatory enlargement.
As the lesion was smaller in dimension and less hemorrhagic, surgical scalpel excision of the
entire lesion was planned. Scaling and root planning was done on the first visit. After 1 week,
internal bevel gingivectomy using no. 15 BP blade under local anesthesia was done, excising the
entire lesion and conforming to the gingival contour [Figure 2a]. The adjoining interdental
papilla was trimmed and curetted [Figure 2b]. The patient was prescribed analgesics, to be taken
if required. However, after histopathological examination, the lesion was diagnosed as GCF
based on light microscopy findings [Figure 3]. On review after 1 week, a stabilized gingival
contour with minimal signs of inflammation of adjoining papillae was observed [Figure 2c].
Diskusi
Fibrous hyperplasias are described as “reactive” rather than neoplastic proliferations of
fibroblastic tissue occurring as a result of chronic injury or irritation. They are most commonly
seen in the first three decades of life without any gender predilection. They present clinically as
an asymptomatic elevated small lesion. These lesions have a “bosselated” or “pebbly” surface.
They may be pedunculated or sessile and are found most commonly on the mandibular gingiva.
Infrequently, they also occur on the tongue, palate, and buccal mucosa. Unless traumatized while
brushing or chewing, they typically have the color of normal mucosa.
Histopathological examination of GCF shows characteristic multiple large stellate‑shaped and
sometimes multinucleated fibroblasts (giant cells) with large nuclei and thin elongated
cytoplasmic processes in a loosely arranged immature avascular fibrous connective tissue. These
pathognomonic cells often have a smudged appearance and are most abundant just under the
epithelium. Regezi et al. reported that the occurrence of stellate cells depends on the collagen
pattern in the lamina propria and that they were concentrated in sites where the submucosa
consisted largely of lamina propria.[6] Rare occurrence of this lesion in extraoral sites like in the
nose has been reported. However, the lesion was found to differ histologically by the presence of
large stellate fibroblasts and have a tendency to recur.[7] Among the various
immunohistochemical markers such as cytokeratin, neurofilament, HHF, CD68, HLA‑DR,
tryptase, leukocyte common antigen, S‑100, vimentin, and desmin, the giant fibroblasts showed
positivity to only vimentin suggesting a fibroblastic origin.[2] The negative reactivity of giant
cells for desmin eliminates the possibility of a myofibroblastic phenotype.[2,8] Immunostaining
with PCNA and Ki‑67 reveals negative reactivity with Ki‑67, whereas PCNA shows variable
expression, suggesting their formation from differentiated mononuclear cells.[9,10].
Until the early 1970s, GCF was considered to belong to a group of similar lesions referred to as
fibromas, fibrous hyperplasias, or fibroepithelial polyps. Although they may share common
characteristics, various studies on the clinical and histologic features have enabled the
classification of these lesions as a separate pathologic entity. The differential diagnosis includes
irritation fibroma, papilloma, pyogenic granuloma, ossifying fibroma, and peripheral giant cell
granuloma. The lesion with the most similarity to GCF is the irritation fibroma. It is usually seen
in individuals between the ages of 40 and 60 years, with a female predilection. Irritation fibroma
usually occurs along the line occlusal plane on the labial/buccal mucosa rather than
on the gingiva.[11] However, the provisional diagnosis was considered as the tooth was palatally
located compared to the adjacent teeth predisposing the marginal gingiva to constant irritation
during tooth brushing.
Chronic inflammatory gingival enlargement occurs as a discrete sessile or pedunculated slow-
growing and usually painless overgrowth. It has abundant inflammatory cells and fluid, vascular
engorgement, vascular neogenesis, and associated degenerative changes. Lesions that are
relatively firm, resilient, and pink have a higher fibrotic component with more of fibroblasts and
collagen fibers. In our case, characteristic giant stellate-shaped and spindle-shaped fibroblasts
with large nuclei and thin elongated cytoplasmic processes were seen.[12] Differential diagnosis
of papilloma may be considered because of the papillary surface of most of the squamous
papillomas. The lesion in this report presented only with a corrugated gingival margin.[11]
Pyogenic granulomas exclusively occur in areas of inflamed gingiva and are usually associated
with compromised oral hygiene and local factors.[13] They may be sessile or pedunculated with
surface ulcerations, and the color can range from a purplish-red hue to deep blue, depending on
the vascularity of the lesion and degree of venous stasis. They usually have a smooth surface,
bleed easily, and may later become hyperplastic and nodular. They may develop rapidly to reach
their full size. In the present case, the sessile lesion which had developed over a period of years,
clinically presented with a gritty surface texture with no signs of spontaneous bleeding.[13] Due
to the similarity in the hue, a differential diagnosis of ossifying fibroma may be considered.
However, the presence of islands of osteogenic cells within the ossifying fibroma differentiates it
from GCF. Unlike GCF, peripheral ossifying fibroma occurs more in females and it is more of a
gingival lesion as it is thought to arise from the periodontal ligament. The lesion in our patient
was much smaller in dimension when compared to ossifying fibroma.[11] Peripheral giant cell
granulomas are asymptomatic and hemorrhagic, rapidly growing lesions with a female
predilection while the lesion was a slow-growing one in our patient. The tissue surface appeared
near-normal with no signs of hemorrhage.[14].
GCF does not regress spontaneously because of the excessive collagenous tissue. GCF is best
treated by conservative surgical excision and does not usually recur after excision. Periodontal
root planing and curettage are also recommended while excising so as to remove any source of
irritation. Recurrence has been reported in a few instances following incomplete excision.[2]
Early recognition and complete excision are necessary to minimize repeated surgical
intervention.
Conclusion
All fibrous hyperplasias are relatively innocent lesions. However, histologic examination is
required in most cases to rule out a malignancy. These benign lesions may continue to grow
unless the source of irritation is removed. It is important to distinguish GCF from other
nonneoplastic lesions that could potentially affect developing structures or result in osteolytic
lesions. Early diagnosis and treatment of these lesions are necessary to avoid developing
unaesthetic soft tissue architecture and the need for extensive periodontal surgical management.
You might also like
- Salivary Gland Cancer: From Diagnosis to Tailored TreatmentFrom EverandSalivary Gland Cancer: From Diagnosis to Tailored TreatmentLisa LicitraNo ratings yet
- Exophytic Gingival LesionsDocument8 pagesExophytic Gingival LesionsAlexandra ElenaNo ratings yet
- Complications in UveitisFrom EverandComplications in UveitisFrancesco PichiNo ratings yet
- Clinically, These Lesions All Form Pinkish Nodules Unless The Surface Has Been InjuredDocument28 pagesClinically, These Lesions All Form Pinkish Nodules Unless The Surface Has Been Injuredreal_septiady_madrid3532No ratings yet
- Giant Cell Lesions of Oral CavityDocument4 pagesGiant Cell Lesions of Oral CavityPreetam PatnalaNo ratings yet
- Giant Cell Epulis: Report of 2 Cases.: Oral PathologyDocument11 pagesGiant Cell Epulis: Report of 2 Cases.: Oral PathologyVheen Dee DeeNo ratings yet
- Oral Pathology: Hyperplasia of Oral MucosaDocument7 pagesOral Pathology: Hyperplasia of Oral Mucosaعلي صادق جعفرNo ratings yet
- Large CystDocument4 pagesLarge CystKin DacikinukNo ratings yet
- Epulis Fibromatosa MedscapeDocument6 pagesEpulis Fibromatosa MedscapeSofiyahH.AbdulKarimNo ratings yet
- Temporal Bone GranulomaDocument5 pagesTemporal Bone GranulomaRabie MohamedNo ratings yet
- Cervicofacial LymphangiomasDocument11 pagesCervicofacial LymphangiomasCharmila Sari100% (1)
- Juvenile Nasopharyngeal Angiofibroma (JNA)Document19 pagesJuvenile Nasopharyngeal Angiofibroma (JNA)YogiHadityaNo ratings yet
- 12-Giant Cell LesionDocument78 pages12-Giant Cell Lesionفراس الموسويNo ratings yet
- Clinical: Peripheral Ossifying Fibroma: A Case ReportDocument4 pagesClinical: Peripheral Ossifying Fibroma: A Case Reportsagarjangam123No ratings yet
- Friedberg 1940Document14 pagesFriedberg 1940YPramudiyaNo ratings yet
- Cystic HygromaDocument5 pagesCystic HygromaAde Triansyah EmsilNo ratings yet
- Peripheral Giant Cell Granuloma - A Review and Case Report Jurnal 3Document6 pagesPeripheral Giant Cell Granuloma - A Review and Case Report Jurnal 3Trisna Budi UtamiNo ratings yet
- Tumors of Oral CavityDocument57 pagesTumors of Oral CavityRobins DhakalNo ratings yet
- Unusual Large and Abiding Fibroepithelial Polyp in Oral Cavity: A Case ReportDocument4 pagesUnusual Large and Abiding Fibroepithelial Polyp in Oral Cavity: A Case ReportmuharrimahNo ratings yet
- Central Giant Cell Granuloma A Case ReportDocument5 pagesCentral Giant Cell Granuloma A Case ReportYara Arafat NueratNo ratings yet
- 1 - Natural History of Periodontal DiseaseDocument42 pages1 - Natural History of Periodontal DiseasejazzNo ratings yet
- Keywords: Peripheral Giant Cell Granuloma/giant Cell Epulis, Jaw, ReactiveDocument4 pagesKeywords: Peripheral Giant Cell Granuloma/giant Cell Epulis, Jaw, ReactiveYeni PuspitasariNo ratings yet
- Superficial Acral Fibromyxoma SAF A Case ReportDocument4 pagesSuperficial Acral Fibromyxoma SAF A Case ReportAthenaeum Scientific PublishersNo ratings yet
- Oral Pathology Lec - 1Document11 pagesOral Pathology Lec - 1مصطفى محمدNo ratings yet
- Jejunal Invagination in An Adult Caused by Inflammatory Fibroid Polyp: A Case ReportDocument3 pagesJejunal Invagination in An Adult Caused by Inflammatory Fibroid Polyp: A Case ReportAde CandraNo ratings yet
- Articulo CientíficoDocument11 pagesArticulo CientíficoCarolina SalazarNo ratings yet
- JPNR - S04 - 233Document6 pagesJPNR - S04 - 233Ferisa paraswatiNo ratings yet
- Peripheral Cemento-Ossifying Fibroma - A Case Report With A Glimpse On The Differential DiagnosisDocument5 pagesPeripheral Cemento-Ossifying Fibroma - A Case Report With A Glimpse On The Differential DiagnosisnjmdrNo ratings yet
- Palatal SwellingsDocument6 pagesPalatal Swellingsopi akbarNo ratings yet
- Common Conjunctival LesionsDocument4 pagesCommon Conjunctival LesionsSri AgustinaNo ratings yet
- Epulis GravidarumDocument4 pagesEpulis GravidarumRisdan Hardani TjlNo ratings yet
- 1.epulis Fissuratum: ClassificationDocument3 pages1.epulis Fissuratum: ClassificationArafat Masud NiloyNo ratings yet
- Cabt 12 I 3 P 330Document4 pagesCabt 12 I 3 P 330abeer alrofaeyNo ratings yet
- Pof CR4Document5 pagesPof CR4Swab IndonesiaNo ratings yet
- Necrotizing SialometaplasiaDocument33 pagesNecrotizing SialometaplasiaJessica GreenNo ratings yet
- 63 - CASE REPORT Epulis GranulomaDocument3 pages63 - CASE REPORT Epulis GranulomaRina NovitrianiNo ratings yet
- Case Report: A Rare Case of Cutaneous Desmoid-Type FibromatosisDocument5 pagesCase Report: A Rare Case of Cutaneous Desmoid-Type FibromatosisIJAR JOURNALNo ratings yet
- Recurrence Odontogenic Keratocyst of The Mandible Treated by Surgical Hemimandibulectomy: Case ReportDocument10 pagesRecurrence Odontogenic Keratocyst of The Mandible Treated by Surgical Hemimandibulectomy: Case Reportarbi123No ratings yet
- Gingival Squamous Cell Carcinoma: A Case Report: Dr. P.S.Rakhewar, Dr. Vrunda Kanjalkar, DR - Ruby SyedDocument3 pagesGingival Squamous Cell Carcinoma: A Case Report: Dr. P.S.Rakhewar, Dr. Vrunda Kanjalkar, DR - Ruby SyedGrecia SunurNo ratings yet
- Benign Extrapleural Solitary Fibrous Tumorofthe Headand NeckDocument7 pagesBenign Extrapleural Solitary Fibrous Tumorofthe Headand NeckCara Danielle PabellanoNo ratings yet
- Oral Squamous Papilloma in A Pediatric Patient A Case ReportDocument4 pagesOral Squamous Papilloma in A Pediatric Patient A Case Reportaulia lubisNo ratings yet
- Case Report: Giant Cell Fibroma of Tongue: Understanding The Nature of An Unusual Histopathological EntityDocument5 pagesCase Report: Giant Cell Fibroma of Tongue: Understanding The Nature of An Unusual Histopathological EntityPrince AhmedNo ratings yet
- Non-Odontogenic Benign and Malignant Tumours of Fibrous Tissue OriginDocument52 pagesNon-Odontogenic Benign and Malignant Tumours of Fibrous Tissue OriginRajat NangiaNo ratings yet
- Case Report Irritation Fibroma of PalateDocument4 pagesCase Report Irritation Fibroma of PalateTri Sakti Sunda RomdhoniNo ratings yet
- Dental Journal: Peripheral Ossifying Fibroma of The Anterior Maxillary GingivaDocument5 pagesDental Journal: Peripheral Ossifying Fibroma of The Anterior Maxillary Gingivaanugraha GanendraNo ratings yet
- A Central Giant Cell Granuloma in Anterior Mandible-A Case ReportDocument4 pagesA Central Giant Cell Granuloma in Anterior Mandible-A Case Reportsenja raharjaNo ratings yet
- Peripheral Giant Cell Granuloma - A Case ReportDocument4 pagesPeripheral Giant Cell Granuloma - A Case ReportAziz IkbalNo ratings yet
- Patología OralDocument11 pagesPatología OralLula Bá RdNo ratings yet
- (11-16) Aggresive Central Giant Cell Granuloma of The MaxillaDocument6 pages(11-16) Aggresive Central Giant Cell Granuloma of The Maxillagauri kokaneNo ratings yet
- Odontogenic CystsDocument63 pagesOdontogenic CystsshabeelpnNo ratings yet
- Lip Mucocele: A Case Report: DR - Rushi Kumar Patel, DR - Nishant Singh, DR - Aniket Singh Chauhan, DR - Vinay KumarDocument3 pagesLip Mucocele: A Case Report: DR - Rushi Kumar Patel, DR - Nishant Singh, DR - Aniket Singh Chauhan, DR - Vinay Kumaryuliatinnurhasanah100% (1)
- Marsupialization With Enucleation of Mandibular Lateral Periodontal CystDocument1 pageMarsupialization With Enucleation of Mandibular Lateral Periodontal CystSkyeNo ratings yet
- Granular Cell Tumor Presenting As A Tongue Nodule: Two Case ReportsDocument4 pagesGranular Cell Tumor Presenting As A Tongue Nodule: Two Case ReportsMargarita Mega PertiwiNo ratings yet
- Giant CellDocument5 pagesGiant CellTamimahNo ratings yet
- Case PresentationDocument46 pagesCase PresentationCareer Guide with Dr ShahzadNo ratings yet
- Gingival Epulis: Report of Two Cases.: Dr. Praful Choudhari, Dr. Praneeta KambleDocument5 pagesGingival Epulis: Report of Two Cases.: Dr. Praful Choudhari, Dr. Praneeta KambleAnandNo ratings yet
- 128 435 1 PBDocument3 pages128 435 1 PBTri Sakti Sunda RomdhoniNo ratings yet
- Peripheral Ameloblastic FibromaDocument3 pagesPeripheral Ameloblastic FibromadoktergigikoeNo ratings yet
- UntitledDocument7 pagesUntitledRika Sartyca IlhamNo ratings yet
- Data SCC From InternetDocument3 pagesData SCC From InternetristaniatauhidNo ratings yet
- NMBDocument3 pagesNMBAgieNo ratings yet
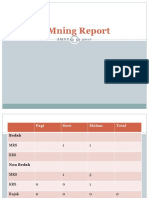
- Pagi Sore Malam Total: BedahDocument7 pagesPagi Sore Malam Total: BedahAgieNo ratings yet
- Lichen Simplex Chronicus Is Induced by Rubbing and Scratching Secondary To ItchDocument1 pageLichen Simplex Chronicus Is Induced by Rubbing and Scratching Secondary To ItchAgieNo ratings yet
- Pagi Sore Malam Total: BedahDocument7 pagesPagi Sore Malam Total: BedahAgieNo ratings yet
- Pagi Sore Malam Total: BedahDocument7 pagesPagi Sore Malam Total: BedahAgieNo ratings yet
- Pagi Sore Malam Total: BedahDocument7 pagesPagi Sore Malam Total: BedahAgieNo ratings yet
- Pagi Sore Malam Total: BedahDocument7 pagesPagi Sore Malam Total: BedahAgieNo ratings yet
- Pagi Sore Malam Total: BedahDocument7 pagesPagi Sore Malam Total: BedahAgieNo ratings yet
- MR 31 1Document10 pagesMR 31 1AgieNo ratings yet
- Pagi Sore Malam Total: BedahDocument7 pagesPagi Sore Malam Total: BedahAgieNo ratings yet
- Pagi Sore Malam Total: BedahDocument7 pagesPagi Sore Malam Total: BedahAgieNo ratings yet
- Pagi Sore Malam Total: BedahDocument7 pagesPagi Sore Malam Total: BedahAgieNo ratings yet
- Morning Report: Kamis, 31 Agustus 2017Document10 pagesMorning Report: Kamis, 31 Agustus 2017AgieNo ratings yet
- MR 31 1Document10 pagesMR 31 1AgieNo ratings yet
- MR 1lopDocument6 pagesMR 1lopAgieNo ratings yet
- MRMNBDocument6 pagesMRMNBAgieNo ratings yet
- MBDocument11 pagesMBAgieNo ratings yet
- MR 31 1Document10 pagesMR 31 1AgieNo ratings yet
- Morning Report: Kamis, 31 Agustus 2017Document10 pagesMorning Report: Kamis, 31 Agustus 2017AgieNo ratings yet
- Mmning Report: J M N T 1 2 1 2 2 0 1 7Document6 pagesMmning Report: J M N T 1 2 1 2 2 0 1 7AgieNo ratings yet
- Timing of Initiation of Antiretrovirals Among Patients With HIV Requiring Tuberculosis TreatmentDocument2 pagesTiming of Initiation of Antiretrovirals Among Patients With HIV Requiring Tuberculosis TreatmentAgieNo ratings yet
- MRED 17 s12Document6 pagesMRED 17 s12AgieNo ratings yet
- Morning Report: Jumat, 1 Desember 2017Document6 pagesMorning Report: Jumat, 1 Desember 2017AgieNo ratings yet
- MMDocument8 pagesMMAgieNo ratings yet
- MR 3 9 17Document8 pagesMR 3 9 17AgieNo ratings yet
- MR 17 Sept 17Document7 pagesMR 17 Sept 17AgieNo ratings yet
- MR 3 9 17Document8 pagesMR 3 9 17AgieNo ratings yet
- Morning Report: Minggu, 3 September 2017Document8 pagesMorning Report: Minggu, 3 September 2017AgieNo ratings yet
- Dengue FeverDocument1 pageDengue FeverAgieNo ratings yet
- Valleylab ForceTriad - User Manual PDFDocument100 pagesValleylab ForceTriad - User Manual PDFPaulina LekszyckaNo ratings yet
- Dinoprostone GelDocument7 pagesDinoprostone GelSahil AliNo ratings yet
- Episodic SOAP Note Template - RX PedsDocument11 pagesEpisodic SOAP Note Template - RX PedsBrianne Foster75% (4)
- Proteinuria and Chronic Kidney DiseaseDocument34 pagesProteinuria and Chronic Kidney DiseaseВалерий ГаврилуцаNo ratings yet
- Head InjuryDocument2 pagesHead InjuryHavez KleibNo ratings yet
- Is Consciousness FractalDocument10 pagesIs Consciousness FractalFederico Flores RichaudNo ratings yet
- Psych Units 11-13 Cheat SheetDocument1 pagePsych Units 11-13 Cheat SheetTalia ShumanNo ratings yet
- Adl IadlDocument20 pagesAdl IadlKrisna Eka Yudha100% (1)
- SJT Med SchoolDocument101 pagesSJT Med SchoolErine Novita BasukiNo ratings yet
- Intensive Nursing Practicum: Bachelor of Science in NursingDocument9 pagesIntensive Nursing Practicum: Bachelor of Science in NursingMichelle Gliselle Guinto MallareNo ratings yet
- Vascular EDSDocument5 pagesVascular EDSMelissa MartinNo ratings yet
- Super Recall EAQDocument63 pagesSuper Recall EAQlourdeslulylou100% (27)
- CAD/CAM Dentistry and Chairside Digital Impression Making: 4 CE CreditsDocument11 pagesCAD/CAM Dentistry and Chairside Digital Impression Making: 4 CE CreditsShraddha AgarwalNo ratings yet
- SurgerySuturePatternsT SissenerDocument5 pagesSurgerySuturePatternsT SissenerPitche Tomale100% (1)
- Alcon Cheatsheet PDFDocument1 pageAlcon Cheatsheet PDFSoham SahaNo ratings yet
- Correlation Between Healthcare Service Quality and HIV Testing Services Patient's Satisfaction in Kedungdoro Primary Health Care SurabayaDocument4 pagesCorrelation Between Healthcare Service Quality and HIV Testing Services Patient's Satisfaction in Kedungdoro Primary Health Care SurabayaAgung KatritamaNo ratings yet
- SOGC Clinical Guideline LiomyomaDocument22 pagesSOGC Clinical Guideline LiomyomaSarah MuharomahNo ratings yet
- Sulcus Vocalis Our Experience-DikonversiDocument5 pagesSulcus Vocalis Our Experience-DikonversiNuni SukindarNo ratings yet
- Smith Medical - H-1200 Fast Fluid WarmerDocument78 pagesSmith Medical - H-1200 Fast Fluid WarmerVictor ȘchiopuNo ratings yet
- MSN FP6216 ForsythKathryn Assessment4 2Document6 pagesMSN FP6216 ForsythKathryn Assessment4 2NbiNo ratings yet
- Oral Cancer 26.3.19Document23 pagesOral Cancer 26.3.19Pradeep100% (2)
- Va SwotDocument3 pagesVa Swotapi-280277788No ratings yet
- Drug Interactions Results - MICROMEDEX®Document3 pagesDrug Interactions Results - MICROMEDEX®Kike MenesesNo ratings yet
- Bilevel VentilationDocument18 pagesBilevel VentilationBonehead7No ratings yet
- Insulin Adjustment Workbook CompleteDocument53 pagesInsulin Adjustment Workbook CompleteDiabestes-stuff100% (1)
- Nursing Trends Paper: Nursing InformaticsDocument6 pagesNursing Trends Paper: Nursing Informaticscwarrington09No ratings yet
- Therapeutic CommunicationDocument82 pagesTherapeutic CommunicationYvette Vallejo100% (2)
- Basic Surgical Skills Indonesia 2016Document17 pagesBasic Surgical Skills Indonesia 2016'putu' AcaaRyaaNo ratings yet
- Bbraun DialyserDocument36 pagesBbraun Dialyserpankaj29sharmaNo ratings yet
- Skin Care PowerpointDocument52 pagesSkin Care Powerpointisapatrick812667% (3)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (28)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (2)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (81)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 3.5 out of 5 stars3.5/5 (3)
- Outlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisFrom EverandOutlive: The Science and Art of Longevity by Peter Attia: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (1)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (3)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- Sleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningFrom EverandSleep Stories for Adults: Overcome Insomnia and Find a Peaceful AwakeningRating: 4 out of 5 stars4/5 (3)
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)No ratings yet
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Gut: the new and revised Sunday Times bestsellerFrom EverandGut: the new and revised Sunday Times bestsellerRating: 4 out of 5 stars4/5 (392)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (44)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- The Marshmallow Test: Mastering Self-ControlFrom EverandThe Marshmallow Test: Mastering Self-ControlRating: 4.5 out of 5 stars4.5/5 (58)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingFrom EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingRating: 4 out of 5 stars4/5 (1138)
- Troubled: A Memoir of Foster Care, Family, and Social ClassFrom EverandTroubled: A Memoir of Foster Care, Family, and Social ClassRating: 4.5 out of 5 stars4.5/5 (26)