Professional Documents
Culture Documents
Suicide Epilepsy Cohort
Uploaded by
Diana SelaruCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Suicide Epilepsy Cohort
Uploaded by
Diana SelaruCopyright:
Available Formats
The n e w e ng l a n d j o u r na l of m e dic i n e
original article
Suicide-Related Events in Patients Treated
with Antiepileptic Drugs
Alejandro Arana, M.D., Charles E. Wentworth, M.S., José L. Ayuso-Mateos, M.D.,
and Felix M. Arellano, M.D.
A bs t r ac t
Background
From Risk MR Pharmacovigilance Services, A previous meta-analysis of data from clinical trials showed an association between
Zaragoza (A.A., F.M.A.); the Department antiepileptic drugs and suicidality (suicidal ideation, behavior, or both). We used
of Psychiatry, Hospital Universitario de la
Princesa, Universidad Autónoma de Ma- observational data to examine the association between the use or nonuse of anti-
drid, and Centro de Investigación Bio- epileptic drugs and suicide-related events (attempted suicides and completed sui-
médica en Red de Salud Mental, Instituto cides) in patients with epilepsy, depression, or bipolar disorder.
de Salud Carlos III, Madrid (J.L.A.-M.) —
all in Spain; and RiskMR, Bridgewater, NJ
(C.E.W., F.M.A.). Address reprint requests Methods
to Dr. Arana at Risk MR Pharmacovigi- We used data collected as part of the clinical care of patients who were representa-
lance Services, Jerónimo Zurita 14, 1-D,
50001 Zaragoza, Spain, or at arana.riskmr@ tive of the general population in the United Kingdom to identify patients with epi-
gmail.com. lepsy, depression, or bipolar disorder and to determine whether they received anti-
epileptic drugs. We estimated the incidence rate of suicide-related events and used
N Engl J Med 2010;363:542-51.
Copyright © 2010 Massachusetts Medical Society. logistic regression to compute odds ratios, controlling for confounding factors.
Results
In a cohort of 5,130,795 patients, the incidence of suicide-related events per 100,000
person-years was 15.0 (95% confidence interval [CI], 14.6 to 15.5) among patients
without epilepsy, depression, bipolar disorder, or antiepileptic-drug treatment, 38.2
(95% CI, 26.3 to 53.7) among patients with epilepsy who did not receive antiepileptic
drugs, and 48.2 (95% CI, 39.4 to 58.5) among patients with epilepsy who received
antiepileptic drugs. In adjusted analyses, the use of antiepileptic drugs was not as-
sociated with an increased risk of suicide-related events among patients with epi-
lepsy (odds ratio, 0.59; 95% CI, 0.35 to 0.98) or bipolar disorder (1.13; 95% CI, 0.35
to 3.61) but was significantly associated with an increased risk among patients with
depression (1.65; 95% CI, 1.24 to 2.19) and those who did not have epilepsy, depres-
sion, or bipolar disorder (2.57; 95% CI, 1.78 to 3.71).
Conclusions
The current use of antiepileptic drugs was not associated with an increased risk of
suicide-related events among patients with epilepsy, but it was associated with an
increased risk of such events among patients with depression and among those who
did not have epilepsy, depression, or bipolar disorder.
542 n engl j med 363;6 nejm.org august 5, 2010
The New England Journal of Medicine
Downloaded from nejm.org on April 20, 2016. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
Suicide-Related Events and Antiepileptic Drugs
S
uicide is the 13th leading cause of the manuscript. All authors reviewed the manu-
death worldwide,1 and attempted suicide is script and decided before the study began to sub-
a major cause of injury.2 Psychiatric disor- mit the manuscript for publication.
ders (especially affective conditions) increase the
risk of suicide.3-5 Epilepsy increases both the risk Source Population and Data
of suicide among patients with psychiatric disor- We performed the study using The Health Im-
ders6 and the risk of the development of psychi- provement Network (THIN) database, which is rep-
atric illness.7 The early onset of epilepsy, female resentative of the general population in the Unit-
sex, psychiatric illness, temporal-lobe epilepsy, ed Kingdom12 and includes more than 6.7 million
and inadequate neurologic follow-up are risk fac- patients. THIN data are entered at general prac-
tors for suicide among patients with epilepsy.6,8 titioners’ offices and are based on the daily rec
Depression is common in patients with severe ord keeping of these practices. The data provide
epilepsy,8 but the severity of epilepsy does not anonymous demographic, medical, and prescrip-
necessarily correlate with the risk of suicide.5 tion information on individual patients, and they
The risk of suicide increases soon after the onset provide a longitudinal medical record for each
of epilepsy5 and then decreases gradually. Patients patient.13
with long-standing epilepsy or dysphoric condi-
tions appear to have an increased risk of suicide Study Population
soon after gaining control of their seizures.9 Patients were eligible for inclusion in the study
In January 2008, the Food and Drug Admin- population if they were enrolled in a clinical prac-
istration (FDA) issued a safety warning on the tice for at least 6 months during the study period
risk of suicidality associated with antiepileptic (from July 1, 1988, through March 31, 2008). A
drugs.10 The warning summarized the results of a history of a suicide attempt is the major risk fac-
meta-analysis of placebo-controlled clinical trials tor for a subsequent suicide attempt.14 Thus, we
of 11 antiepileptic drugs; this meta-analysis showed excluded patients with a family history of suicide
a risk of the development of suicidality (primar- and a personal history of one or more suicide at-
ily suicidal behavior or ideation) that was twice tempts.
as high among patients who received antiepilep- The study had two components. In the descrip-
tic drugs as among patients who received pla- tive analysis, we estimated the crude incidence
cebo. The risk increased soon after the initiation rate of suicide-related events among patients with
of treatment, persisted through week 24, and was epilepsy, depression, or bipolar disorder, with or
elevated regardless of the type of antiepileptic without the use of antiepileptic drugs. We then
drugs received and the indication for their use. performed a case−control analysis to examine
The assessment of suicidality in the clinical the association between the use or nonuse of
trials that were included in the meta-analysis antiepileptic drugs and suicide-related events.
was subject to several limitations such as the
lack of systematic or standardized language to Definition of the Cohorts
define suicidal ideation and behavior across In the descriptive analysis, we defined the refer-
clinical trials.11 We examined the association be- ence group as patients who did not have epilepsy,
tween antiepileptic drugs and suicide-related depression, or bipolar disorder and did not re-
events (defined as suicide attempts and completed ceive antiepileptic drugs. The other cohorts are
suicides), using data collected as part of clinical listed in Table 1.
practice in the United Kingdom.
Cohort Follow-up
Me thods Patients were assigned to cohorts according to
the presence of an event that defined a given co-
Study Design and Oversight hort. The index date was the date when the last
The study was designed by the investigators in Read code15 that would include a patient in a co-
Spain. The data were collected by the second au- hort was recorded. Patients were followed until
thor, and the analyses were performed by the death, loss to follow-up, or the end of the study
first and second authors. The last author wrote period, whichever came first.
n engl j med 363;6 nejm.org august 5, 2010 543
The New England Journal of Medicine
Downloaded from nejm.org on April 20, 2016. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
tempts) for validation to determine the positive
Table 1. Study Cohorts.
predictive value of the diagnoses used. The vali-
Patients who did not have epilepsy, depression, or bipolar disorder but who dation process included a questionnaire sent to
received antiepileptic drugs the general practitioner, as well as a review of the
Patients with epilepsy who did not receive antiepileptic drugs patient’s medical records and death certificate
Patients with epilepsy who received antiepileptic drugs when available (see the Supplementary Appendix,
Patients with depression who did not receive antiepileptic drugs available with the full text of this article at NEJM
Patients with depression who received antiepileptic drugs .org). The questionnaires and records were re-
viewed by one of the investigators, who was un-
Patients with bipolar disorder who did not receive antiepileptic drugs
aware of the patients’ exposure to antiepileptic
Patients with bipolar disorder who received antiepileptic drugs
drugs. The positive predictive value was 97% for
Patients with epilepsy and depression who did not receive antiepileptic drugs suicide-related events and 87% for completed
Patients with epilepsy and depression who received antiepileptic drugs suicide. This method of validating cases based
Patients with epilepsy and bipolar disorder who did not receive antiepileptic drugs on THIN data has been successfully used in other
Patients with epilepsy and bipolar disorder who received antiepileptic drugs studies.16
Selection of Controls
Exposure to Medications For the case−control component of the study, we
The antiepileptic drugs of interest were those randomly selected five controls from the cohort
drugs identified in the FDA’s meta-analysis which for each case patient, matched according to age
were available in the United Kingdom: carbamaz at the index date (±5 years), sex, and clinical prac-
epine, gabapentin, lamotrigine, levetiracetam, tice. Using risk-set control sampling, we defined
oxcarbazepine, pregabalin, tiagabine, topiramate, the date of the end of the follow-up period for the
valproate, and zonisamide (felbamate was not in- controls as the date when the case patient received
cluded because it was not marketed in the United a diagnosis. There were no unmatched case pa-
Kingdom). Current use was defined as the inter- tients. For the analysis of the use or nonuse of
val between the date of the prescription of an antiepileptic drugs within each category of ill-
antiepileptic drug and 75 days after that date. ness, another set of controls, matched according
After that interval, as long as no other antiepilep- to age, sex, clinical practice, and psychiatric or
tic drug was prescribed, the patient was consid- neurologic condition, was selected. A total of 103
ered to be a previous user. Patients without codes case patients did not match any controls.
for antiepileptic drugs were classified as nonusers.
Statistical Analysis
Case Identification and Characterization We described the characteristics of the various
Cases of suicide-related events were based on cohorts using frequency tables. We calculated
codes for suicide, attempted suicide, and inten-the incidence rates and 95% confidence intervals
tional self-inflicted injuries plus suicide. A com-
for suicide-related events in each of the cohorts
pleted suicide was defined as a code for suicidal-
with the use of a Poisson regression model.
ity followed by a code for death in the following The relationship between the use or nonuse
month and a final date of any administrative of antiepileptic drugs and suicide-related events
activity in the database or disenrollment within(expressed as odds ratios and 95% confidence
6 months after the suicidality code. If the disen-
intervals) was assessed with the use of a fixed-
rollment date occurred more than 6 months after effects conditional logistic-regression model. In
a suicidality code, we reviewed the patient’s pro-
addition to matching for age, sex, clinical prac-
file. Patients with a last medical or other health-
tice, and condition when applicable, we controlled
related code that was recorded within 1 month for potential confounders (Table 2) with the use
after the suicide date were also considered to of a backward-elimination process by stepwise
have completed suicide. deletion of the confounder that made the small-
est change in the exposure−effect estimate on
Case Validation deletion, provided that the effect of the con-
We selected a random sample of 218 cases of founder was 10% or less of the estimated effect.
suicide-related events (86 suicides and 132 at- Any confounder with an effect of more than 10%
544 n engl j med 363;6 nejm.org august 5, 2010
The New England Journal of Medicine
Downloaded from nejm.org on April 20, 2016. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
Suicide-Related Events and Antiepileptic Drugs
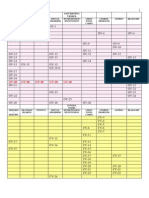
Table 2. Demographic Characteristics and Risk Factors for Suicide-Related Events, According to Use or Nonuse
of Antiepileptic Drugs.*
No Epilepsy, Depression,
Bipolar Disorder, or Use Antiepileptic Epilepsy and Use
of Antiepileptic Drugs Drugs Only Epilepsy Only of Antiepileptic Drugs
Variable (N = 4,514,366)† (N = 77,319) (N = 16,120) (N = 39,325)
Male sex — no. (%) 2,273,135 (50.4) 34,978 (45.2) 8,565 (53.1) 20,868 (53.1)
Age — no. (%)
<20 yr 1,413,006 (31.3) 3,975 (5.1) 3,715 (23.0) 7,935 (20.2)
20–34 yr 1,204,371 (26.7) 7,506 (9.7) 4,786 (29.7) 8,815 (22.4)
>34–64 yr 1,326,817 (29.4) 34,689 (44.9) 5,564 (34.5) 14,031 (35.7)
>64 yr 500,482 (11.1) 30,848 (39.9) 1,762 (10.9) 8,008 (20.4)
Data missing 69,690 (1.5) 301 (0.4) 293 (1.8) 536 (1.4)
Mean age — yr 32.0±23.1 56.5±20.6 35.3±20.9 41.3±23.5
Duration of time in study — yr 6.2±5.3 3.9±3.9 5.4±4.9 5.4±4.7
Drug use in previous yr — no. (%)
Antipsychotic agent 53,894 (1.2) 7,910 (10.2) 488 (3.0) 2,588 (6.6)
Antidepressant agent 103,343 (2.3) 23,034 (29.8) 810 (5.0) 3,002 (7.6)
Lithium 1,146 (<0.1) 402 (0.5) 6 (<0.1) 38 (0.1)
History — no. (%)
Drug abuse 1,232 (<0.1) 80 (0.1) 15 (0.1) 25 (0.1)
Diagnosis of mental disorder 171,846 (3.8) 13,845 (17.9) 1,794 (11.1) 4,174 (10.6)
Alcohol abuse 26,189 (0.6) 2,106 (2.7) 620 (3.8) 1,199 (3.0)
Chronic disease score‡
Mean score 0.45±0.97 3.26±1.96 0.68±1.20 2.09±1.51
Score — no. (%)
0 3,443,036 (76.3) 1,776 (2.3) 10,801 (67.0) 973 (2.5)
1 509,052 (11.3) 16,023 (20.7) 2,236 (13.9) 18,973 (48.2)
2 329,417 (7.3) 12,478 (16.1) 1,650 (10.2) 7,111 (18.1)
3 137,521 (3.0) 14,830 (19.2) 788 (4.9) 5,644 (14.4)
4 59,001 (1.3) 12,887 (16.7) 375 (2.3) 3,468 (8.8)
5 36,339 (0.8) 19,325 (25.0) 270 (1.7) 3,156 (8.0)
* Plus−minus values are means ±SD.
† This was the reference category.
‡ Chronic disease scores can range from 0 to 5, with higher scores indicating a higher frequency of chronic disease.
on the estimate was kept in the model. To con- follow-up. Table 2, and Table 1 in the Supplemen-
trol for the severity of chronic disease, we included
tary Appendix, show the demographic character-
a modified version of the chronic disease score istics of the patients. Overall, 48.6% of the pa-
in the model.17,18 All analyses were conducted tients were male, and the mean (±SD) age was
with the use of SAS software, version 9.1 (SAS 33.7±23.1 years. The mean follow-up time for all
Institute) and Stata software, version 7.0 (Stata). the cohorts was 6.2±5.2 years. A total of 66,925
patients had epilepsy; 16,120 of these patients
R e sult s did not have a diagnosis of depression or bipolar
disorder and did not receive antiepileptic drugs.
Characteristics of the Patients A total of 435,790 patients with depression only
The cohorts included a total of 5,130,795 pa- and 3814 with bipolar disorder only did not re-
tients, with a total of 31,527,585 patient-years of ceive antiepileptic drugs. A total of 77,319 pa-
n engl j med 363;6 nejm.org august 5, 2010 545
The New England Journal of Medicine
Downloaded from nejm.org on April 20, 2016. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
Table 3. Incidence of Suicide-Related Events, According to Cohorts and Use or Nonuse of Antiepileptic Drugs.
Patients with First
Suicide-Related Crude Incidence Rate
Cohort All Patients Event Person-Yr (95% Confidence Interval)
no. of events/
no. of patients 100,000 person-yr
No epilepsy, depression, or bipolar disorder
No use of antiepileptic drugs (reference group) 4,514,366 4239 28,170,361 15.05 (14.60−15.51)
Any use of antiepileptic drugs 77,319 120 304,807 39.37 (32.64−47.08)
Epilepsy only (no depression or bipolar disorder)
No use of antiepileptic drugs 16,120 33 86,333 38.22 (26.31−53.68)
Any use of antiepileptic drugs 39,325 103 213,507 48.24 (39.38−58.51)
Depression only (no epilepsy or bipolar disorder)
No use of antiepileptic drugs 435,790 3271 2,534,502 129.06 (124.70−133.60)
Any use of antiepileptic drugs 30,772 232 130,854 177.30 (155.21−201.64)
Bipolar disorder (no epilepsy)
No use of antiepileptic drugs 3,814 48 22,324 215.02 (158.54−285.08)
Any use of antiepileptic drugs 1,809 40 9,065 441.26 (315.24−600.87)
Epilepsy and depression (no bipolar disorder)
No use of antiepileptic drugs 3,392 28 16,353 171.22 (113.78−247.47)
Any use of antiepileptic drugs 7,870 96 38,452 249.66 (202.23−304.88)
Epilepsy and bipolar disorder
No use of antiepileptic drugs 47 0 210 0
Any use of antiepileptic drugs 171 2 819 244.24 (29.58−882.28)
All patients 5,130,795 8212 31,527,585 26.05 (25.49−26.62)
tients received antiepileptic drugs but did not Supplementary Appendix. The incidence rate of
have epilepsy, depression, or bipolar disorder. The suicide-related events among patients who did
indications for the use of antiepileptic drugs in not have epilepsy, depression, or bipolar disorder
these patients were not known, although pain was 57.9 (95% CI, 42.8 to 76.5) per 100,000 per-
and pain-related diagnoses (e.g., herpes zoster) son-years for current users of antiepileptic drugs
were documented in the records of 18.7% of these and 32.3 (95% CI, 25.2 to 40.7) per 100,000 per-
patients in the 30 days before prescription of the son-years for previous users of antiepileptic drugs
antiepileptic drugs. (Table 4 in the Supplementary Appendix). Among
patients with depression alone, the incidence rate
Incidence of Attempted and Completed of suicide-related events was 129.1 (95% CI, 124.7
Suicides to 133.6) per 100,000 person-years for those who
A total of 8212 patients attempted suicide, includ- were not currently receiving antiepileptic drugs
ing 464 patients who completed suicide. The in- and 177.3 (95% CI, 155.2 to 201.6) per 100,000
cidence rate of suicide-related events among pa- person-years for those who were receiving anti-
tients without epilepsy, depression, or bipolar epileptic drugs. Among patients with bipolar dis-
disorder who did not receive antiepileptic drugs order alone, the incidence rate of suicide-related
(the reference group) was 15.0 (95% confidence events was 215.0 (95% CI, 158.5 to 285.1) per
interval [CI], 14.6 to 15.5) per 100,000 person- 100,000 person-years for those who were not re-
years (Table 3). Details of the incidence of suicide ceiving antiepileptic drugs and 441.3 (95% CI,
according to the patient’s psychiatric or neuro- 315.2 to 600.9) per 100,000 person-years for those
logic condition are available in Table 2 in the who were receiving antiepileptic drugs. Among
546 n engl j med 363;6 nejm.org august 5, 2010
The New England Journal of Medicine
Downloaded from nejm.org on April 20, 2016. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
Suicide-Related Events and Antiepileptic Drugs
patients with epilepsy alone, the incidence of
suicide-related events was 38.2 (95% CI, 26.3 to 1.00
53.7) per 100,000 person-years for those who
Probability of No Suicide-Related Events
were not receiving antiepileptic drugs and 48.2 0.99
(95% CI, 39.4 to 58.5) per 100,000 person-years
for those who were receiving such treatment. Fig-
0.98
ure 1 shows the probability of no suicide-related Reference group
events over time in the various cohorts. The un- Epilepsy alone
derlying illness was more strongly associated 0.97 Epilepsy and antiepileptic drugs
with suicide-related events than was the use or Antiepileptic drugs
Depression alone
nonuse of antiepileptic drugs. 0.96
Depression and antiepileptic drugs
Bipolar disorder and antiepileptic drugs
Case–Control Analysis 0.95 Bipolar disorder alone
The results of the case−control analysis were ad- 0.00
0 10 20
justed for age; duration of illness; status with
respect to previous use of antiepileptic drugs, Years since Treatment Initiation
lithium, antipsychotic drugs, or antidepressants;
presence or absence of a history of alcohol abuse Figure 1. Kaplan−Meier Estimates of the Probability of No Suicide-Related
Events over Time, According to Cohort.
or a mental disorder; and chronic disease score.
With adjustment for these factors, epilepsy and
depression were associated with a 50% increase
in the risk of suicide-related events; the risk as- those who were receiving such treatment (odds
sociated with bipolar disorder was higher (Table ratio, 2.06; 95% CI, 1.36 to 3.11) and among
5 in the Supplementary Appendix). The risk of patients with bipolar disorder who were not re-
suicide-related events was increased with a history ceiving antiepileptic drugs (odds ratio, 2.44; 95%
of alcohol abuse (odds ratio, 6.45; 95% CI, 5.68 to CI, 1.48 to 4.03) and among those who were (odds
7.32), a mental disorder (odds ratio, 2.75; 95% CI, ratio, 3.77; 1.24 to 11.43) (Table 4 and Fig. 2). As
2.54 to 2.98), lithium use (odds ratio, 2.48; 95% compared with patients with bipolar disorder
CI, 1.76 to 3.49), antipsychotic-drug use (odds ra- who received neither lithium nor antiepileptic
tio, 1.64; 95% CI, 1.51 to 1.77), and antidepres- drugs, the odds ratio for suicide-related events
sant-drug use (odds ratio, 3.69; 95% CI, 3.42 to was 0.56 (95% CI, 0.11 to 1.71) among patients
3.99). Chronic diseases were clearly associated with with bipolar disorder who received antiepileptic
suicide-related events, with a 20% increase in risk drugs and lithium and 0.74 (95% CI, 0.45 to 1.19)
per unit of increase in the chronic disease score. among those who received lithium alone.
The current use of antiepileptic drugs in pa- In a series of separate case−control analyses,
tients without epilepsy, depression, or bipolar we observed no significant increase in the risk
disorder was associated with an increased risk of of suicide-related events among current users of
suicide-related events (odds ratio, 2.57; 95% CI, antiepileptic drugs as compared with nonusers
1.78 to 3.71). The risk of suicide-related events in the subgroup of patients with epilepsy alone
was elevated both among patients with epilepsy (odds ratio, 0.59; 95% CI, 0.35 to 0.98), the sub-
who received antiepileptic drugs and among group of patients with bipolar disorder alone
those who did not; among patients with epilepsy (odds ratio, 1.13; 95% CI, 0.35 to 3.61), or the
and no coexisting depression or bipolar disorder subgroup of patients with epilepsy and depres-
who did not receive antiepileptic drugs, the odds sion (odds ratio, 1.24; 95% CI, 0.56 to 2.72).
ratio was 3.34 (95% CI, 2.34 to 4.78), and among Among patients with depression alone, the use
patients with epilepsy who received antiepileptic of antiepileptic drugs was significantly associ-
drugs, the odds ratio was 2.31 (95% CI, 1.77 to ated with an increased risk of suicide-related
3.02). Similarly, the risk of suicide-related events events (odds ratio, 1.65; 95% CI, 1.24 to 2.19)
was increased among patients with depression (Table 5). The effects of the use of various anti-
who were not receiving antiepileptic drugs (odds epileptic drugs are shown in Table 6 in the
ratio, 1.58; 95% CI, 1.43 to 1.74) and among Supplementary Appendix.
n engl j med 363;6 nejm.org august 5, 2010 547
The New England Journal of Medicine
Downloaded from nejm.org on April 20, 2016. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
Table 4. Combined Effect of Use of Antiepileptic Drugs and Various Conditions on the Risk of Suicide-Related Events,
Adjusted for Covariates.*
Case
Cohort Patients Controls Odds Ratio (95% CI)
number
No epilepsy, depression, or bipolar disorder
No use of antiepileptic drugs (reference group) 5,948 45,620 1.00
Current use of antiepileptic drugs 76 84 2.57 (1.78−3.71)
Epilepsy only (no depression or bipolar disorder)
No use of antiepileptic drugs 64 168 3.34 (2.34−4.78)
Current use of antiepileptic drugs 134 380 2.31 (1.77−3.02)
Depression only (no epilepsy or bipolar disorder)
No use of antiepileptic drugs 3,475 4,448 1.58 (1.43−1.74)
Current use of antiepileptic drugs 239 159 2.06 (1.36−3.11)
Bipolar disorder only (no epilepsy)
No use of antiepileptic drugs 60 42 2.44 (1.48−4.03)
Current use of antiepileptic drugs 40 7 3.77 (1.24−11.43)
Epilepsy and depression (no bipolar disorder)
No use of antiepileptic drugs 33 37 1.60 (0.91−2.81)
Current use of antiepileptic drugs 93 59 2.82 (1.71−4.67)
Epilepsy and bipolar disorder
No use of antiepileptic drugs 0 1 0
Current use of antiepileptic drugs 2 0 Infinite
* Odds ratios were derived from one conditional logistic-regression model with matching according to age (±5 years),
sex, and clinical practice. Odds ratios were adjusted for age, duration of disease, previous use of antiepileptic drugs,
lithium, antipsychotic drugs, or antidepressants; presence or absence of a history of alcohol abuse or a mental disor-
der; and chronic disease score.
Discussion antiepileptic drugs (Table 2); we controlled for
these factors in the case−control analysis.
Our analyses of observational data collected as The risk of suicide-related events was in-
part of clinical practice in the United Kingdom creased among patients who received antiepilep-
confirmed the previously reported increased risk tic drugs for indications other than epilepsy,
of suicide-related events associated with epilepsy, bipolar disorder, or depression (odds ratio, 2.57;
depression, and bipolar disorder.19 Our findings 95% CI, 1.78 to 3.71). It is not possible to be
suggest that treatment with antiepileptic drugs certain about the indications for the use of anti-
does not confer an additional risk of suicide- epileptic drugs in these patients, but it is likely
related events among patients with epilepsy. that for some patients the indications were pain-
The crude incidence of suicide-related events related (e.g., herpes zoster). Pain, especially chron-
among patients with epilepsy who did not receive ic pain, has been associated with an increased
antiepileptic drugs was 38.2 per 100,000 person- risk of suicide.20 In patients with depression, the
years, and the incidence was slightly higher risk was also higher among current users of anti-
(48.2 per 100,000 person-years) among patients epileptic drugs than among nonusers. Although
with epilepsy who received antiepileptic drugs. a causal role of antiepileptic drugs is possible, it
The most likely explanation for the difference is also possible that the use of antiepileptic
between the unadjusted and adjusted findings is drugs in these patients is a marker of severe
that patients who received antiepileptic drugs depression or the presence of another condition
were older and had more coexisting conditions that may be associated with an increased risk of
and risk factors than those who did not receive suicide-related events.21
548 n engl j med 363;6 nejm.org august 5, 2010
The New England Journal of Medicine
Downloaded from nejm.org on April 20, 2016. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
Suicide-Related Events and Antiepileptic Drugs
A study has suggested that the risk of suicide
associated with bipolar disorder is lower during 100.0
No use of antiepileptic drugs Current use of antiepileptic drugs
treatment with lithium than with other treat-
ments.22 This finding was also observed in our
study; however, the number of patients who re- 10.0
ceived lithium was too low (29 patients overall)
Odds Ratio
to draw firm conclusions. Among patients with
bipolar disorder in our study, the odds ratio for
1.0
suicide-related events was 0.56 (95% CI, 0.11 to
1.71) among those who received antiepileptic
drugs and lithium and 0.74 (95% CI, 0.45 to 1.19)
among those who received lithium alone, as 0.1
No Disorder Epilepsy Depression Bipolar Disorder
compared with patients who received neither
lithium nor antiepileptic drugs. However, the
number of case patients who received lithium Figure 2. Effect of Current Antiepileptic-Drug Use on the Risk of Suicide-
Related Events.
was low (29 overall).
The risk is shown according to disease status (epilepsy, depression, bipolar
In general, our results do not confirm the disorder, or none of these conditions). The bars indicate 95% confidence
findings previously reported by the FDA.10 The intervals.
FDA study was a meta-analysis of data from
placebo-controlled clinical trials of the use of
antiepileptic drugs across a number of indica- of treatment and epidemiologic studies have a
tions for up to 24 weeks. Among the 142 cases long follow-up, the incidence of these early-occur-
of suicide-related events included in the meta- ring suicides becomes diluted in epidemiologic
analysis, 4 (2.8%) were completed suicides and studies as compared with clinical trials.
38 (26.8%) were suicide attempts. Our study fo- The incidence rate of completed suicide in our
cused on these “harder” end points that are of population was 1.5 per 100,000 patient-years. In
greatest clinical concern and involved a longer 2007, the incidence rate was 16.8 per 100,000
follow-up (mean, 6.2 years). Unlike the FDA meta- among men and 5.0 per 100,000 among women
analysis, our results suggest that in patients in the United Kingdom.27 Potential explanations
with epilepsy, the use of antiepileptic drugs is for the lower incidence of suicide in our cohort
not associated with an increased risk of suicide include the fact that we calculated the incidence
attempts or completed suicide. Our results were rate of suicide after excluding from the sample
similar for patients with bipolar disorder: we did patients with a family history of suicide or a per-
not detect a significant effect of antiepileptic sonal history of suicide attempts and the fact
drugs on suicide-related events among patients that suicide has been shown to be underreported
with this condition, which is associated with a in THIN.28 Underreporting would not have a
high risk of suicide,23 although our results had major effect on the associations observed in our
wide confidence intervals. We could not rule out case−control analyses unless it affected some
a large association, since the upper bound of the cohorts more than others. The high positive pre-
95% confidence interval for the odds ratio ex- dictive value for the diagnosis of suicide-related
ceeded 3, but we also could not rule out a “pro- events in the case validation supports the valid-
tective” effect, since the lower confidence limit ity of our study.
was 0.35. Our findings in bipolar disorder were An increased risk of suicide-related events
consistent with those of other studies.24 Differ- among patients receiving specific antiepileptic
ences between the results of a meta-analysis drugs as compared with patients receiving topi-
conducted by the FDA and epidemiologic studies ramate for any indication has recently been re-
of suicidality have also been reported with regard ported.29 This study addressed a different ques-
to antidepressants.25 Reasons for these differ- tion and used substantially different methods.
ences include ascertainment bias11 and the in- For a patient who is being treated with antiepi-
creased frequency of suicide in the first month leptic drugs, the risk of suicide results from the
after initiation of antidepressant treatment.26 combination of the risk associated with the ill-
Since most clinical trials have a short duration ness prompting the use of these drugs and the
n engl j med 363;6 nejm.org august 5, 2010 549
The New England Journal of Medicine
Downloaded from nejm.org on April 20, 2016. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
Table 5. Association between Current Use of Antiepileptic Drugs and Suicide-Related Events in Each of the Cohorts,
Adjusted for Covariates.*
Case
Cohort Patients Controls Odds Ratio (95% CI) P Value
number
Epilepsy only (no depression or bipolar disorder)
No use of antiepileptic drugs 64 282 1.00
Current use of antiepileptic drugs 104 399 0.59 (0.35−0.98) 0.04
Depression only (no epilepsy or bipolar disorder)
No use of antiepileptic drugs 3475 17,747 1.00
Current use of antiepileptic drugs 99 157 1.65 (1.24−2.19) 0.001
Bipolar disorder only (no epilepsy)
No use of antiepileptic drugs 60 65 1.00
Current use of antiepileptic drugs 17 14 1.13 (0.35−3.61) 0.84
Epilepsy and depression (no bipolar disorder)
No use of antiepileptic drugs 33 64 1.00
Current use of antiepileptic drugs 61 85 1.24 (0.56−2.72) 0.60
Epilepsy and bipolar disorder
No use of antiepileptic drugs 0 0 1.00
Current use of antiepileptic drugs 1 0 Infinite (0.00) Infinite
* Odds ratios were derived from conditional logistic-regression models matched according to diagnostic category, age
(±5 years), sex, and clinical practice. Odds ratios were adjusted for age; duration of disease; previous use of antiepilep-
tic drugs, lithium, antipsychotic drugs, or antidepressants; presence or absence of a history of alcohol abuse or a men-
tal disorder; and chronic disease score. A total of 103 case patients did not match any controls.
risk associated with the drugs themselves. Our that patients with pain, which is associated with
results, stratified according to the indication for an increased risk of suicide, received antiepilep-
drug use, suggest that illness carries more im- tic drugs. The way we built our cohorts, with no
portance than the use of antiepileptic drugs. The overlap of subjects between cohorts, may have
results of our analysis of individual antiepileptic led to immortal time bias. This bias was avoided
drugs were imprecise, with wide confidence in- in the case−control analysis.
tervals, but they point to differences in risk as- In conclusion, our findings do not provide
sociated with antiepileptic drugs used for vari- support for an association between antiepileptic
ous indications. drugs and suicide-related events among patients
To minimize confounding, we excluded from receiving antiepileptic drugs for epilepsy. How-
the analysis those patients with a history of sui- ever, we did observe an association between the
cide-related events, so it is theoretically possible current use of antiepileptic drugs and suicide-
that our results cannot be extrapolated to this related events among patients with depression
high-risk population. Although we tried to limit and among patients who did not have epilepsy,
confounding, some of the results may be partially depression, or bipolar disorder.
attributable to confounding by indication.30 For Disclosure forms provided by the authors are available with
example, the increased risk observed among the full text of this article at NEJM.org.
We thank Delories Dunn, Dr. Janet Price, and Dr. Randal Mar-
patients with pain may be due to an effect of shall for their suggestions for revisions of an earlier version of
antiepileptic drugs or may simply reflect the fact the manuscript.
References
1. DeLeo D, Bertolote J, Lester D. Self- neva: World Health Organization, 2002: 2. Moscicki EK. Epidemiology of suicid-
directed violence. In: Krug EG, Dahlberg 183-212. (Accessed July 9, 2010, at http:// al behavior. In: Silverman MM, Maris RW,
LL, Mercy JA, Zwi AB, Lozano R, eds. www.who.int/violence_injury_prevention/ eds. Suicide prevention: toward the year
World report on violence and health. Ge- violence/world_report/en/index.html.) 2000. New York: Guilford, 1985:22-35.
550 n engl j med 363;6 nejm.org august 5, 2010
The New England Journal of Medicine
Downloaded from nejm.org on April 20, 2016. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
Suicide-Related Events and Antiepileptic Drugs
3. Idem. Epidemiology of completed and 12. Hippisley-Cox J, Coupland CA, Vino disorder: an overview. Harv Rev Psychia-
attempted suicide: toward a framework gradova Y, Robson J, Brindle P. The per- try 2009;17:231-41.
for prevention. Clin Neurosci Res 2001;1: formance of the QRISK cardiovascular 22. Goodwin FK, Fireman B, Simon GE,
310-23. risk prediction algorithm in an external Hunkeler EM, Lee J, Revicki D. Suicide
4. Mortensen PB, Agerbo E, Erikson T, UK sample of patients from General Prac- risk in bipolar disorder during treatment
Qin P, Westergaard-Nielsen N. Psychiatric tice: a validation study. Heart 2008;94: with lithium and divalproex. JAMA 2003;
illness and risk factors for suicide in Den- 34-9. 290:1467-73.
mark. Lancet 2000;355:9-12. 13. The Health Improvement Network 23. Kessler RC, Chiu WT, Demler O, Wal-
5. Nilsson L, Ahlbom A, Fahraman BY, Web site. (Accessed July 9, 2010, at http:// ters EE. Prevalence, severity, and comor-
Asberg M, Tomson T. Risk factors for sui- www.thin-uk.com.) bidity of 12-month DSM-IV disorders in
cide in epilepsy: a case control study. Epi- 14. American Foundation for Suicide Pre- the National Comorbidity Survey Replica-
lepsia 2002;43:644-51. vention. Risk factors for suicide. (Accessed tion (NCS-R). Arch Gen Psychiatry 2005;
6. Christensen J, Vestergaard M, Morten July 9, 2010, at http://www.afsp.org/index 62:617-27.
sen PB, Sidenius P, Agerbo E. Epilepsy and .cfm?page_id=05147440-E24E-E376- 24. Gibbons RD, Hur K, Brown CH, Mann
risk of suicide: a population-based case- BDF4BF8BA6444E76.) JJ. Relationship between antiepileptic
control study. Lancet Neurol 2007;6:693-8. 15. NHS Centre for Coding and Classifi- drugs and suicide attempts in patients
7. Qin P, Xu H, Laursen TM, Vestergaard cation. The Read codes, version 3. London: with bipolar disorder. Arch Gen Psychia-
M, Mortensen PB. Risk for schizophrenia Stationery Office, 1996. try 2009;66:1354-60.
and schizophrenia-like psychosis among 16. Arellano FM, Arana A, Wentworth 25. Gibbons RD, Brown CH, Hur K, Mar-
patients with epilepsy: population based CE, Fernandez-Vidaurre C, Schlienger RG, cus SM, Bhaumik DK, Mann JJ. Relation-
cohort study. BMJ 2005;331:23. Conde E. Lymphoma among patients with ship between antidepressants and suicide
8. Hesdorffer DC, Hauser WA, Olafsson atopic dermatitis and/or treated with top- attempts: an analysis of the Veterans
E, Ludvigsson P, Kjartansson O. Depres- ical immunosupressants in the United Health Administration data sets. Am J
sion and suicide attempt as risk factors Kingdom. J Allergy Clin Immunol 2009; Psychiatry 2007;164:1044-9.
for incident unprovoked seizures. Ann 123:1111-6. 26. Jick H, Kaye JA, Jick SS. Antidepres-
Neurol 2006;59:35-41. 17. Von Korff M, Wagner EH, Saunders K. sants and the risk of suicidal behaviors.
9. Blumer D, Montouris G, Davies K, A chronic disease score from automated JAMA 2004;292:338-43.
Wyler A, Phillips B, Hermann B. Suicide in pharmacy data. J Clin Epidemiol 1992;45: 27. Suicides: UK suicide rates continue to
epilepsy: psychopathology, pathogenesis 197-203. fall. Newport, United Kingdom: Office
and prevention. Epilepsy Behav 2002;3: 18. Arellano FM, Yood MU, Wentworth for National Statistics, January 2009. (Ac-
232-41. CE, et al. Use of cyclo-oxygenase 2 inhibi- cessed July 9, 2010, at http://www.statistics
10. Katz R. Briefing document for the July tors (COX-2) and prescription non-steroi- .gov.uk/pdfdir/sui0109.pdf.)
10, 2008 advisory committee meeting to dal anti-inflammatory drugs (NSAIDs) in 28. Hall G. Validation of death and sui-
discuss antiepileptic drugs (AEDs) and UK and USA populations. Pharmacoepi- cide recording on the THIN UK primary
suicidality. Memorandum. (Accessed July 9, demiol Drug Safe 2006;15:861-72. care database. Pharmacoepidemiol Drug
2010, at http://www.fda.gov/ohrms/dockets/ 19. Harris EC, Barraclough B. Suicide as Safe 2009;18:120-31.
ac/08/briefing/2008-4372b1-01-FDA-Katz an outcome for mental disorders: a meta- 29. Patorno E, Bohn RL, Wahl PM, et al.
.pdf.) analysis. Br J Psychiatry 1997;170:205-28. Anticonvulsant medications and the risk
11. Posner K, Oquendo MA, Gould M, 20. Braden JB, Sullivan MD. Suicidal of suicide, attempted suicide, or violent
Stanley B, Davies M. Columbia Classifi- thoughts and behavior among adults with death. JAMA 2010;303:1401-9.
cation Algorithm of Suicide Assessment self-reported pain conditions in the Na- 30. Bell GS, Mula M, Sander JW. Suicidal-
(C-CASA): classification of suicidal events tional Comorbidity Survey Replication. ity in people taking antiepileptic drugs:
in the FDA’s pediatric suicidal risk analy- J Pain 2008;9:1106-15. what is the evidence? CNS Drugs 2009;23:
sis of antidepressants. Am J Psychiatry 21. Vigo DV, Baldessarini RJ. Anticonvul- 281-92.
2007;164:1035-43. sants in the treatment of major depressive Copyright © 2010 Massachusetts Medical Society.
n engl j med 363;6 nejm.org august 5, 2010 551
The New England Journal of Medicine
Downloaded from nejm.org on April 20, 2016. For personal use only. No other uses without permission.
Copyright © 2010 Massachusetts Medical Society. All rights reserved.
You might also like
- Antipsychotic Drug Use and The Risk of SeizuresDocument13 pagesAntipsychotic Drug Use and The Risk of SeizuresAttaufiq IrawanNo ratings yet
- Suicide Attempts in Hospital-Treated Epilepsy Patients: Radmila Buljan and Ana Marija ŠantićDocument6 pagesSuicide Attempts in Hospital-Treated Epilepsy Patients: Radmila Buljan and Ana Marija Šantićprodaja47No ratings yet
- Epilepsy, Suicidality, and Psychiatric Disorders: A Bidirectional AssociationDocument8 pagesEpilepsy, Suicidality, and Psychiatric Disorders: A Bidirectional AssociationDaiana PiacenzaNo ratings yet
- 7217 Nihms690005Document17 pages7217 Nihms690005meiutaNo ratings yet
- Fazel 2014 CORRECTE PDFDocument11 pagesFazel 2014 CORRECTE PDFMargaNo ratings yet
- Anticonvulsant Medications and The Risk of Suicide, Attempted Suicide, or Violent DeathDocument9 pagesAnticonvulsant Medications and The Risk of Suicide, Attempted Suicide, or Violent DeathMarcelo MonteiroNo ratings yet
- Pi Is 2215036614702573Document3 pagesPi Is 2215036614702573RealAelixirNo ratings yet
- Suicide Risk Assessment and Prevention. Challenges and OpportunitiesDocument12 pagesSuicide Risk Assessment and Prevention. Challenges and OpportunitiesMaira Espinoza LabraNo ratings yet
- Cassidy Suicidality Schizophrenia 2018Document11 pagesCassidy Suicidality Schizophrenia 2018Juan InsignaresNo ratings yet
- Psychotic Disorders Induced by Antiepileptic Drugs in People With EpilepsyDocument11 pagesPsychotic Disorders Induced by Antiepileptic Drugs in People With EpilepsydupuytrenNo ratings yet
- Violence and Homicidal Behaviors in Psychiatric DisordersDocument21 pagesViolence and Homicidal Behaviors in Psychiatric DisordersMarcelo ColodetiNo ratings yet
- Jurnal JiwaDocument4 pagesJurnal JiwaNaomiFettyNo ratings yet
- Intencion SuicidaDocument8 pagesIntencion SuicidaOsman CastroNo ratings yet
- 9.the Role of Inflammation in Suicidal BehaviourDocument12 pages9.the Role of Inflammation in Suicidal BehaviourWendy QuintanaNo ratings yet
- Emailing Yoa20484 - 82 - 91Document10 pagesEmailing Yoa20484 - 82 - 91DEEPA NAIRNo ratings yet
- Schizophrenia, Substance Abuse, and Violent Crime: Original ContributionDocument8 pagesSchizophrenia, Substance Abuse, and Violent Crime: Original ContributionMargaNo ratings yet
- 20 Year Follow Up Study of Physical Morbidity and Mortality in Relationship To Antipsychotic Treatment in A Nationwide Cohort of 62,250 Patients With Schizophrenia (FIN20)Document8 pages20 Year Follow Up Study of Physical Morbidity and Mortality in Relationship To Antipsychotic Treatment in A Nationwide Cohort of 62,250 Patients With Schizophrenia (FIN20)Alondra CastilloNo ratings yet
- HHS Public Access: Association of Antipsychotic Use With Mortality Risk in Patients With Parkinson DiseaseDocument17 pagesHHS Public Access: Association of Antipsychotic Use With Mortality Risk in Patients With Parkinson DiseasekasandraharahapNo ratings yet
- Estrategias de Prevención de Suicidio JAMADocument11 pagesEstrategias de Prevención de Suicidio JAMAapi-26621755No ratings yet
- An Evidence-Based Approach To Evaluating and Managing Suicidal EmergenciesDocument22 pagesAn Evidence-Based Approach To Evaluating and Managing Suicidal EmergencieslorainecumplidoNo ratings yet
- Popovic Et Al-2014-Acta Psychiatrica ScandinavicaDocument9 pagesPopovic Et Al-2014-Acta Psychiatrica ScandinavicaCarolina MuñozNo ratings yet
- Pi Is 1059131106001208Document5 pagesPi Is 1059131106001208Murli manoher chaudharyNo ratings yet
- Treatment of Anxiety Disorders by Psychiatrists From The American Psychiatric Practice Research NetworkDocument6 pagesTreatment of Anxiety Disorders by Psychiatrists From The American Psychiatric Practice Research NetworkStephNo ratings yet
- Suicidio. Conceptos ActualesDocument9 pagesSuicidio. Conceptos Actualesdaniela Hernandez LopezNo ratings yet
- Realworld Effectiveness of Pharmacological Treatments For Bipolar Disorder Registerbased National Cohort StudyDocument9 pagesRealworld Effectiveness of Pharmacological Treatments For Bipolar Disorder Registerbased National Cohort StudyJose BusaidNo ratings yet
- Komorbid 1Document15 pagesKomorbid 1ErioRakiharaNo ratings yet
- NewTreatmentsAgitationReview CITROME PsychQuarterly2004Document18 pagesNewTreatmentsAgitationReview CITROME PsychQuarterly2004Leslie CitromeNo ratings yet
- The FDA Warning On Antidepressants and Suicidality - Why The Controversy?Document5 pagesThe FDA Warning On Antidepressants and Suicidality - Why The Controversy?Etika Tunjung KencanaNo ratings yet
- Depressive Symptoms and AIDS-Related Mortality Among A Multisite Cohort of HIV-Positive WomenDocument8 pagesDepressive Symptoms and AIDS-Related Mortality Among A Multisite Cohort of HIV-Positive WomenArya Ady NugrohoNo ratings yet
- Risk Factors For Fatal and Nonfatal Repetition of Suicide Attempts: A Literature ReviewDocument12 pagesRisk Factors For Fatal and Nonfatal Repetition of Suicide Attempts: A Literature ReviewMuhammad AdithiaNo ratings yet
- NIH Public Access: Suicidal Thoughts and Behavior With Antidepressant TreatmentDocument15 pagesNIH Public Access: Suicidal Thoughts and Behavior With Antidepressant Treatmenttugba1234No ratings yet
- Caso Clinico NeuroDocument9 pagesCaso Clinico NeuroCinthia ChalacoNo ratings yet
- General Approach To Drug Poisoning in AdultsDocument14 pagesGeneral Approach To Drug Poisoning in AdultsAnonymous cHPg1bKrotNo ratings yet
- Jurnal PsikiatriDocument6 pagesJurnal PsikiatriAkka RakaNo ratings yet
- Captura de Pantalla 2024-01-23 A La(s) 11.26.43Document9 pagesCaptura de Pantalla 2024-01-23 A La(s) 11.26.43Dany MorBenNo ratings yet
- ASCP Corner Increased Risk of Cerebrovascular Adverse Events and Death in Elderly Demented PatienDocument1 pageASCP Corner Increased Risk of Cerebrovascular Adverse Events and Death in Elderly Demented PatienSantosh KumarNo ratings yet
- Tide Malm 2014Document9 pagesTide Malm 2014opanocayNo ratings yet
- Suicide Prevention in Psychiatric PatientsDocument11 pagesSuicide Prevention in Psychiatric PatientsDaniela DiazNo ratings yet
- Antipsychotic Medication Induced Movement Disorders: The Case of Amanuel Specialized Mental Hospital, Addis Ababa, EthiopiaDocument7 pagesAntipsychotic Medication Induced Movement Disorders: The Case of Amanuel Specialized Mental Hospital, Addis Ababa, Ethiopiael egendNo ratings yet
- Risk of SuicideDocument2 pagesRisk of SuicideKaram Ali ShahNo ratings yet
- Minociclina - Depresión en Vih, 2016Document7 pagesMinociclina - Depresión en Vih, 2016Merari Lugo OcañaNo ratings yet
- Is Low Total Cholesterol Levels Associated With Suicide Attempt in Depressive Patients?Document8 pagesIs Low Total Cholesterol Levels Associated With Suicide Attempt in Depressive Patients?Amal MessaoudNo ratings yet
- Prevention of Inpatient Suicides An Attempt To Portray An ApproachDocument11 pagesPrevention of Inpatient Suicides An Attempt To Portray An Approachgion.nandNo ratings yet
- Quin Et Al (2011) - Allergy Is Associated With Suicide Completion With A Possible Mediating Role of Mood Disorder - A Population-Based StudyDocument12 pagesQuin Et Al (2011) - Allergy Is Associated With Suicide Completion With A Possible Mediating Role of Mood Disorder - A Population-Based StudymaelisonNo ratings yet
- Swinkels PscychopathologieDocument16 pagesSwinkels PscychopathologiesezalwickNo ratings yet
- Practical Suicide-Risk Management For The Busy Primary Care PhysicianDocument9 pagesPractical Suicide-Risk Management For The Busy Primary Care PhysicianvathisNo ratings yet
- Use of Antidepressants To Treat Depression in Bipolar Disorder.Document5 pagesUse of Antidepressants To Treat Depression in Bipolar Disorder.teddypolNo ratings yet
- The Association Between Anomalous Self-E PDFDocument5 pagesThe Association Between Anomalous Self-E PDFferny zabatierraNo ratings yet
- Rodriguez Cabezas2018Document13 pagesRodriguez Cabezas2018Ioana CristinaNo ratings yet
- Risk Factors For Complications of Drug-Induced Seizures: Toxicology InvestigationDocument8 pagesRisk Factors For Complications of Drug-Induced Seizures: Toxicology InvestigationdayankramadhanyNo ratings yet
- Medications and Falls in Older People: Geriatric TherapeuticsDocument4 pagesMedications and Falls in Older People: Geriatric TherapeuticsMamenn DicinieNo ratings yet
- Antipsychotics and Suicide: Antipsicóticos y SuicidioDocument10 pagesAntipsychotics and Suicide: Antipsicóticos y SuicidioCamilo ArizaNo ratings yet
- Lalanne 2016Document4 pagesLalanne 2016Claudia HusinNo ratings yet
- Antidepressants Versus Interpersonal Psychotherapy in Treating Depression in HIV-positive PatientsDocument6 pagesAntidepressants Versus Interpersonal Psychotherapy in Treating Depression in HIV-positive PatientsMittaningtyasNo ratings yet
- Psychotic Symptoms and Population Risk For Suicide Attempt A Prospective Cohort StudyDocument9 pagesPsychotic Symptoms and Population Risk For Suicide Attempt A Prospective Cohort StudyGiselle Andrea Naranjo VillateNo ratings yet
- Yoa05015 931 938Document8 pagesYoa05015 931 938GauravNo ratings yet
- Original Paper: Factors That Impact Caregivers of Patients With SchizophreniaDocument10 pagesOriginal Paper: Factors That Impact Caregivers of Patients With SchizophreniaMichaelus1No ratings yet
- General Hospital Psychiatry: Mijung Park, PH.D., M.P.H., R.N., Wayne J. Katon, M.D., Fredric M. Wolf, PH.D., M.EdDocument9 pagesGeneral Hospital Psychiatry: Mijung Park, PH.D., M.P.H., R.N., Wayne J. Katon, M.D., Fredric M. Wolf, PH.D., M.EdOz ziqNo ratings yet
- Association of Depression With Viral Load, CD8 T Lymphocytes, and Natural Killer Cells in Women With HIV InfectionDocument8 pagesAssociation of Depression With Viral Load, CD8 T Lymphocytes, and Natural Killer Cells in Women With HIV InfectionSharon AdeleNo ratings yet
- Epilepsia - 2017 - Scheffer - ILAE Classification of The Epilepsies Position Paper of The ILAE Commission ForDocument10 pagesEpilepsia - 2017 - Scheffer - ILAE Classification of The Epilepsies Position Paper of The ILAE Commission ForCarlos Peña PaterninaNo ratings yet
- Seziures: Status Epilepticus Status EpilepticusDocument2 pagesSeziures: Status Epilepticus Status EpilepticusEna PaparićNo ratings yet
- Physical Disabilities Health ImpairmentsDocument15 pagesPhysical Disabilities Health ImpairmentsGeronimo Mark JosephNo ratings yet
- Health - 19-02-06 MEDICAL CANNABIS PDFDocument104 pagesHealth - 19-02-06 MEDICAL CANNABIS PDFJamielyn DilidiliNo ratings yet
- Sleepwalking PDFDocument9 pagesSleepwalking PDFPD11No ratings yet
- Epilepsy Lesson PlanDocument14 pagesEpilepsy Lesson PlanShree Kalidass100% (4)
- 4x4 - Hummer - UK Manual - PCDocument24 pages4x4 - Hummer - UK Manual - PCHan SoloNo ratings yet
- Thief 2 The Metal Age ManualDocument33 pagesThief 2 The Metal Age ManualMordenGreyNo ratings yet
- FPGA Implementation of Second-Order Difference Plot For Epileptic Seizure Detection in EEG SignalsDocument5 pagesFPGA Implementation of Second-Order Difference Plot For Epileptic Seizure Detection in EEG SignalsshalvinNo ratings yet
- Health Teaching Plan: EffectsDocument2 pagesHealth Teaching Plan: EffectsRheal P EsmailNo ratings yet
- IMPORTANT: The Original of This Form Is To Be Kept by The Seafarer. A Copy Must Be Kept by The ClinicDocument2 pagesIMPORTANT: The Original of This Form Is To Be Kept by The Seafarer. A Copy Must Be Kept by The ClinicTigreal MLNo ratings yet
- Juvenile Myoclonic Epilepsy: Under-Appreciated and Under-DiagnosedDocument3 pagesJuvenile Myoclonic Epilepsy: Under-Appreciated and Under-Diagnosedaniket mittalNo ratings yet
- Internal Medicine II GRDocument86 pagesInternal Medicine II GRAhmad SobihNo ratings yet
- Functional Neurological Disorders: It Is All in The Head: Linda ThomsonDocument12 pagesFunctional Neurological Disorders: It Is All in The Head: Linda ThomsonKit GuintoNo ratings yet
- Setup and Installation: Stuart Little 2 Stuart Little 2Document10 pagesSetup and Installation: Stuart Little 2 Stuart Little 2Prabesh KcNo ratings yet
- Neurointernet Moccia 2018Document8 pagesNeurointernet Moccia 2018deepam kapoorNo ratings yet
- Childhood Epilepsy: An Update On Diagnosis and Management: January 2015Document18 pagesChildhood Epilepsy: An Update On Diagnosis and Management: January 2015Berto PengNo ratings yet
- Ketogenic Diet and Metabolic Therapies Expanded Roles in Health and Disease 2Nd Edition Susan A Masino Editor Full ChapterDocument68 pagesKetogenic Diet and Metabolic Therapies Expanded Roles in Health and Disease 2Nd Edition Susan A Masino Editor Full Chapterglenn.hamilton954100% (4)
- Cost of Illness of Epilepsy and Associated Factors in PatientsDocument10 pagesCost of Illness of Epilepsy and Associated Factors in PatientsMezgebu Yitayal MengistuNo ratings yet
- Patients Dental Health FormDocument2 pagesPatients Dental Health Formthadopestsi100% (1)
- Supreme Court Judgement On Pension To Ex. Armyman Retired On Health GroundsDocument22 pagesSupreme Court Judgement On Pension To Ex. Armyman Retired On Health GroundsLatest Laws TeamNo ratings yet
- TBL 12 - Organic Mental DisorderDocument43 pagesTBL 12 - Organic Mental DisorderTanyap LimleeNo ratings yet
- Acupoint ConnectionsDocument9 pagesAcupoint ConnectionsFabioVetNo ratings yet
- Assessment of PsychosisDocument73 pagesAssessment of Psychosismanuel ricardo barojas alvarezNo ratings yet
- Beleza 2015Document8 pagesBeleza 2015Gerardo Lerma BurciagaNo ratings yet
- Impact of Levetiracetam and Valproic Monotherapy in Quality of Life in Patients With EpilepsyDocument2 pagesImpact of Levetiracetam and Valproic Monotherapy in Quality of Life in Patients With Epilepsyakshay dahiweleNo ratings yet
- Daftar Buku NeuroDocument4 pagesDaftar Buku NeuroDedi SutiaNo ratings yet
- Use of Electroencephalography (EEG) in The Management of Seizure DisordersDocument62 pagesUse of Electroencephalography (EEG) in The Management of Seizure DisordersSai ManojNo ratings yet
- Epilepsia Amjmed 2021Document8 pagesEpilepsia Amjmed 2021Juan Diego JImenez AlvizoNo ratings yet
- Al-Rokh's Pacemaker of PacesDocument312 pagesAl-Rokh's Pacemaker of PacesM H Safayet80% (5)