Professional Documents
Culture Documents
Microglossia in A Newborn: A Case Report and Review of The Literature
Uploaded by
Sela Putriana0 ratings0% found this document useful (0 votes)
10 views1 pagejurnal
Original Title
fd3b16c88091ee529dad07b411237d6f646a
Copyright
© © All Rights Reserved
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Documentjurnal
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
10 views1 pageMicroglossia in A Newborn: A Case Report and Review of The Literature
Uploaded by
Sela Putrianajurnal
Copyright:
© All Rights Reserved
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 1
Microglossia in a Newborn: A Case Report and Review of the Literature
Stanley Voigt, B.A., Aric Park, M.D., Mark A. Vecchiotti, M.D.
Tufts Medical Center, Boston, Massachusetts
INTRODUCTION A conclusive etiology for microglossia remains at this time unknown
however several theories have been postulated. Certain drugs used during
Microglossia is a very rare condition with approximately 50 cases
pregnancy such as diazepam, chlorpromazine, meclizine and tigan have been
reported in literature to date. Frequently, this disorder presents in thought to possibly contribute to the condition. Another proposed risk factor
association with limb abnormalities and is grouped as a hypoglossia- is hyperthermia in utero especially in association with Moebius syndrome.
hypodactilia syndrome. In 1718, de Jussieu was the first to describe the There is no substantial evidence for heredity or sexual preference in the
condition. He reported on a 15-year old with what he termed ‘congenital development of microglossia[1,3]. Interference of the stapedial blood
lingual hypoplasia’. In 1932 the literature up to that date was review by supply has been postulated by some as a potential cause leading to
Rosenthal and he also documented the first report of the hypoglossia- malformation of the 2nd branchial arch [6]. Congenital anomalies associated
hypodactilia syndrome. Subsequent reports have been released which Figure 1: Embryology of the tongue. Note the anterior two thirds are with some cases of microglossia or aglossia are: Hanhart Syndrome, Charles
confirming a relationship between hypoglossia and hypodactilia [1,3]. created by the combination of the tuberculum impar and the lateral lingual M. syndrome, Robin sequence & Moebius syndrome [3]. Several cases of
In this poster we discuss a case of isolated microglossia, its workup, and swellings. The posterior tongue develops from the third arch mesoderm and microglossia have also been associated with situs inversus and dextrocardia
develops from the hypobranchial eminence. Hamilton et al, 1968
management. [6].
On physical exam, various oral anomalies may be present in association with
microglossia or aglossia. These patients tend to have a narrowing of the face
CASE PRESENTATION referred by many as “bird-like” along with retrognathia, a high palatal vault
and an excessive overbite [2]. Cleft palate has also been reported in a small
Patient AR was born to a 21 year old G1P1 female via Cesarean section
subset of cases. Intraoral bands may be present between the mandible and
secondary to fetal distress and polyhydramnios at 40 4/7 weeks at an maxilla involving soft tissue or bone. These attachments may require
outside hospital. Otolaryngology consultation was performed to surgery due to limitation of oral excursion or feeding. Uvular enlargement is
evaluate the patient’s craniofacial abnormalities. Weight at birth was present in many cases of hypoglossia. A consistent finding later during
3770 grams and Apgars were 4,7, and 8 at 1,5, and 10 minutes development are dental anomalies, notably absence of both the molars and
respectively. The pregnancy was otherwise uneventful. He was incisors leading to malocclusion. The muscles of the floor of the mouth,
transferred to Tufts Medical Center for further workup of his particularly the mylohyoid, tend to hypertrophy over time and aid with
Figure 2: Sagittal CT of Soft Tissue Neck with Contrast. Note the minimal
microglossia and retrognathia at day of life 1. Initially he was kept movement of food. Thus, problems with nutrition tend to subside as the
development of the anterior 2/3s of the tongue as shown by the green arrow.
n.p.o. and received tube feeds via a nasogastric tube until his swallowing child ages. Taste sensation is usually intact and it is interesting to note that
function could be fully assessed. On physical exam he was noted to some neonates present with enhanced taste perception [5].
have marked retrognathia and a high arched palate, without associated Several developmental issues need to be followed as the patient matures.
limb abnormalities (figure 2). His tongue deflected posteriorly with a The tongue is involved in speech, mastication, swallowing, and dental
small anterior two-thirds of the tongue but normal appearing posterior development [3]. These issues have to be addressed through infancy and
tongue. The posterior third of the tongue effaced the valleculae and childhood. The treatment team should involve a nutrition, psychology,
epiglottis. On imaging he was noted to have a sabertooth appearance to speech & hearing, general dentistry, and orthodontics if necessary [5].
his trachea along with evidence of supraglottic malacia on laryngoscopy Follow up should continue through adolescence to correct possible speech
(figure 3). After evaluation by the feeding and swallowing team, he was impediments, deal with self-esteem issues from her facial appearance and
dentistry to address occlusal issues.
made n.p.o. due to risk for aspiration, which is a common finding in the
small number of documented microglossia cases. After a modified
barium swallow study and functional endoscopic evaluation of swallow Figure 3. Physical exam findings in oral cavity. Note REFERENCES
which confirmed aspiration, he underwent placement of a gastrostomy the vestigial anterior 2/3 of tongue bud present. 1. R.J. Gorlin, N.M. Cohen, L.S. Leven. Syndromes of the Head and Neck. Oxford University
Press, New York, 1990, pp. 666-670.
tube for feeding on DOL 24.
DISCUSSION
2. J.B. Roth, A. Sommer, C. Strafford. Microglossia – Micrognathia: A case report and a survey
He was discharged home on DOL 31 on G tube feeds in good condition of 30 others on record. Clinical Pediatrics. 11 (1972) 357-359.
with close follow up every 1 to 2 months. Genetic workup did not Development of the tongue begins at the fourth week of
3. M.A. Thorp, P.J. de Waal, C.A.J. Prescott. Extreme Microglossia. International Journal of
Pediatric Otorhinolaryngology. (2003) 67, 473-477.
reveal any syndromic causes of his craniofacial abnormalities. At five gestation when a swelling termed the tuberculum impar is 4. P. Wadhwani, S. Mohammad, R Sahu. Oromandibular limb hypogenesis syndrome, type IIA,
months of age, he passed a subsequent modified barium swallow and formed at the fusion site of the 1st and 2nd pharyngeal hypoglossia-hypodactylia: a case report. J Oral Pathol Med. (2007) 36: 555-557.
was allowed to start soft solids with supplemental G tube feeds. His 5. F. Salles et al. Complete and Isolated Congenital Aglossia: case report and treatment of
arches. Between the 4th-8th weeks, the anterior 2/3rds of sequelae using rapid prototyping models. Oral Surg Oral Med Oral Pathol Oral Radiol
parents have been referred to audiology for sign language classes as his the tongue develop by the fusion of the lateral lingual Endod. 2008; 105:e41-e47.
future expressive language may be delayed due to his microglossia. swellings and tuberculum impar (figure 1). The posterior 6. H.K.K. Tan, J.D. Smith, D.Y.T. Goh. Case Report: Unfused hypoplastic tongue in a newborn.
Finally a craniofacial consultation was performed to discuss potential International Journal of Pediatric Otorhinolaryngology. 49 (1999) 53-61.
third of the tongue develops from the hypobranchial 7. W. J. Hamilton, ]. D. Boyd, & H. W. Mossman, Human Embryology, Williams & Wilkins, 3rd
intervention for his mild micrognathia. eminence [6]. ed., 1962, p. 288.
You might also like
- (2010) Handbook Strategy As PracticeDocument367 pages(2010) Handbook Strategy As PracticeViniciusNo ratings yet
- School Learning and Development Plan For Head TeachersDocument3 pagesSchool Learning and Development Plan For Head TeachersLiza Bacudo100% (1)
- Project Management British English TeacherDocument4 pagesProject Management British English TeacherАнастасия МицковскаяNo ratings yet
- Exam Paper DiscussionDocument5 pagesExam Paper DiscussionilyanasuhailaabdollaNo ratings yet
- A Practical Guide To Behavioral Research Tools and Techniques - Capítulo 01 PDFDocument9 pagesA Practical Guide To Behavioral Research Tools and Techniques - Capítulo 01 PDFdani_g_1987No ratings yet
- 1 s2.0 S0738081X14002375 MainDocument13 pages1 s2.0 S0738081X14002375 Mainmarisa araujoNo ratings yet
- Achondroplasia: September 2012Document7 pagesAchondroplasia: September 2012ancillaagrayn100% (1)
- Arthrogryposis (Multiple Congenital Contractures) - Diagnostic Approach To Etiology, Classification, Genetics, and General PrinciplesDocument9 pagesArthrogryposis (Multiple Congenital Contractures) - Diagnostic Approach To Etiology, Classification, Genetics, and General PrinciplesKiara VásquezNo ratings yet
- 2479 ArticleDocument5 pages2479 Articleclbenitez52No ratings yet
- Medip, IJCP-1422 CDocument3 pagesMedip, IJCP-1422 CdsagemaverickNo ratings yet
- The Physiology of Intrapartum Fetal Compromise at TermDocument10 pagesThe Physiology of Intrapartum Fetal Compromise at TermseopyNo ratings yet
- Gastroschisis Omphalocele PDFDocument5 pagesGastroschisis Omphalocele PDFFariz Eka SetiawanNo ratings yet
- Glandula Salivar HeterotopicaDocument2 pagesGlandula Salivar HeterotopicaJuan Esteban RamirezNo ratings yet
- Case Report Persistent Buccopharyngeal Membrane: Report of A Case and Review of The LiteratureDocument4 pagesCase Report Persistent Buccopharyngeal Membrane: Report of A Case and Review of The LiteratureLiviaNo ratings yet
- Pierre Robin SindromeDocument11 pagesPierre Robin SindromearturocarpesNo ratings yet
- Intussusception: Afua A.J. Hesse Francis A. Abantanga Kokila LakhooDocument8 pagesIntussusception: Afua A.J. Hesse Francis A. Abantanga Kokila LakhooFATIN NAJIHAHNo ratings yet
- Craniofacialanomalies: Laszlo Nagy,, Joshua C. DemkeDocument26 pagesCraniofacialanomalies: Laszlo Nagy,, Joshua C. DemkeariskaNo ratings yet
- Hypertrophic Pyloric Stenosis in The Adult: Johannesburg AetiologyDocument3 pagesHypertrophic Pyloric Stenosis in The Adult: Johannesburg AetiologyzapomannNo ratings yet
- Hirschsprung - Megacólon CongênitoDocument17 pagesHirschsprung - Megacólon CongênitoBarbara NevesNo ratings yet
- Hercules Baby - A Rare Case Presentation of Congenital MyopathyDocument4 pagesHercules Baby - A Rare Case Presentation of Congenital MyopathyInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- 235 FullDocument5 pages235 FullAdillaSPNo ratings yet
- Tsaousoglou P 2016 Diagnosis and Treatment of Ankyloglossia a Narrative Review and a Report of Three CasesDocument13 pagesTsaousoglou P 2016 Diagnosis and Treatment of Ankyloglossia a Narrative Review and a Report of Three CasesNhung Võ Thị MỹNo ratings yet
- Craniofacial Syndromes.33Document26 pagesCraniofacial Syndromes.33andrew kilshawNo ratings yet
- Rare Case of Sirenomelia Congenital AnomalyDocument3 pagesRare Case of Sirenomelia Congenital Anomalymahesh shindeNo ratings yet
- Phimosis 5 PDFDocument4 pagesPhimosis 5 PDFNurul YaqinNo ratings yet
- Physiotherapy Treatment of Endemic Cretinism in New Guinea HighlandsDocument4 pagesPhysiotherapy Treatment of Endemic Cretinism in New Guinea Highlandsadilla kusumaNo ratings yet
- Voss 2018Document6 pagesVoss 2018lupalladiniNo ratings yet
- Hirschsprung'S Disease: Peter MatteiDocument1 pageHirschsprung'S Disease: Peter MatteiJulia Wibawa HaryantoNo ratings yet
- Nihms 1657970Document20 pagesNihms 1657970mchojnacki81No ratings yet
- Achondroplasia Case Report: June 2015Document7 pagesAchondroplasia Case Report: June 2015Juodie Lee VaelNo ratings yet
- Pathologic and Physiologic PhimosisDocument7 pagesPathologic and Physiologic Phimosisdianita507No ratings yet
- 3.tahrir N. Aldelaimi Article Bony Syngnathia (Congenital Fusion of Maxilla and Mandible)Document3 pages3.tahrir N. Aldelaimi Article Bony Syngnathia (Congenital Fusion of Maxilla and Mandible)Mohammed AbdulhammedNo ratings yet
- In Brief: Inguinal HerniaDocument4 pagesIn Brief: Inguinal HerniaSaf DicamNo ratings yet
- Tongue: Tie and Frenotomy in The Breastfeeding NewbornDocument7 pagesTongue: Tie and Frenotomy in The Breastfeeding Newbornlaidasilva26No ratings yet
- December 2017 Ophthalmic PearlsDocument2 pagesDecember 2017 Ophthalmic PearlsMEDIWAY CLINICNo ratings yet
- p1319 PDFDocument4 pagesp1319 PDFSyairodhiNo ratings yet
- Case Report: Giant Cell Fibroma of Tongue: Understanding The Nature of An Unusual Histopathological EntityDocument5 pagesCase Report: Giant Cell Fibroma of Tongue: Understanding The Nature of An Unusual Histopathological EntityPrince AhmedNo ratings yet
- Diagnosis and Management of Pediatric DysphagiaDocument9 pagesDiagnosis and Management of Pediatric DysphagiaHERNAN DANIEL RODRIGUEZ HERRERANo ratings yet
- Stenosis PilorusDocument5 pagesStenosis PilorusNovita ApramadhaNo ratings yet
- IJPI_2(2)_61-63Document3 pagesIJPI_2(2)_61-63Tiara HapkaNo ratings yet
- Espina BífidaDocument18 pagesEspina BífidaDamary Cifuentes ReyesNo ratings yet
- Hirschsprung DiseaseDocument18 pagesHirschsprung DiseaseResianaPutriNo ratings yet
- Congenital Orthopedic DeformitiesDocument6 pagesCongenital Orthopedic Deformitiesmamang somayNo ratings yet
- 495 FullDocument2 pages495 Fulltigtigrai49No ratings yet
- PregnancyTumor GeneralDentistryDocument4 pagesPregnancyTumor GeneralDentistryNguyên TrầnNo ratings yet
- Review Article: Phimosis in ChildrenDocument7 pagesReview Article: Phimosis in ChildrenmerlinNo ratings yet
- Isrn Urology2012-707329 PDFDocument6 pagesIsrn Urology2012-707329 PDFNaomiRimaClaudyaNo ratings yet
- Interdisciplinary Neurosurgery: Jimmy Ntimbani, Adrian Kelly, Patrick Lekgwara TDocument4 pagesInterdisciplinary Neurosurgery: Jimmy Ntimbani, Adrian Kelly, Patrick Lekgwara TKunni MardhiyahNo ratings yet
- Thanatophoric Dysplasia: A Rare Entity: Oman Medical Journal May 2011Document3 pagesThanatophoric Dysplasia: A Rare Entity: Oman Medical Journal May 2011Atria DewiNo ratings yet
- Cleft Lip and Palate: Etiological Factors, A ReviewDocument8 pagesCleft Lip and Palate: Etiological Factors, A ReviewAbu-Hussein MuhamadNo ratings yet
- 2019 Zebras in Foreskin Dermatopathology (Natural Circumcision)Document6 pages2019 Zebras in Foreskin Dermatopathology (Natural Circumcision)msdsubNo ratings yet
- Syndromic Craniosynostosis 19pDocument6 pagesSyndromic Craniosynostosis 19pAnna Karolinne NascimentoNo ratings yet
- BurgDocument16 pagesBurgGrazyele SantanaNo ratings yet
- Clinical Anatomy 2019 Mills Defining The Anatomy of The Neonatal Lingual FrenulumDocument12 pagesClinical Anatomy 2019 Mills Defining The Anatomy of The Neonatal Lingual FrenulumDiana ChavezNo ratings yet
- Irvine 1996Document3 pagesIrvine 1996Ali AmokraneNo ratings yet
- Ejpd 2018 19 3 9Document3 pagesEjpd 2018 19 3 9Ismail YusufNo ratings yet
- Etiology of HypospadiaDocument10 pagesEtiology of HypospadiaJemy IkkiNo ratings yet
- Review of The Genetic Basis of Jaw Malformations: Mairaj K. Ahmed Xiaoqian Ye Peter J. TaubDocument11 pagesReview of The Genetic Basis of Jaw Malformations: Mairaj K. Ahmed Xiaoqian Ye Peter J. Taubchristian roblesNo ratings yet
- Management of The Difficult Pediatric AirwayDocument9 pagesManagement of The Difficult Pediatric AirwayinescubertaNo ratings yet
- A Case Series of Anterior and Posterior Tongue TiesDocument4 pagesA Case Series of Anterior and Posterior Tongue TiesTrung Sơn LêNo ratings yet
- A Rare Case of Fatal Bowel Obstruction Secondary To A Colonic BezoarDocument3 pagesA Rare Case of Fatal Bowel Obstruction Secondary To A Colonic BezoarLannydchandraNo ratings yet
- Penoscrotal Hypospadias: Sami Arap, Anuar Ibrahim MitreDocument11 pagesPenoscrotal Hypospadias: Sami Arap, Anuar Ibrahim MitreBambang HariyanaNo ratings yet
- Seminar: Christine Léauté-Labrèze, John I Harper, Peter H HoegerDocument10 pagesSeminar: Christine Léauté-Labrèze, John I Harper, Peter H HoegerMayaSuyataNo ratings yet
- Ajo 12169-1Document8 pagesAjo 12169-1Cinthya ayu MerithaNo ratings yet
- The Dental Pulp: Biology, Pathology, and Regenerative TherapiesFrom EverandThe Dental Pulp: Biology, Pathology, and Regenerative TherapiesNo ratings yet
- 1 s2.0 S0378874110006525 Main PDFDocument4 pages1 s2.0 S0378874110006525 Main PDFSela PutrianaNo ratings yet
- Nandita Shenoy, Junaid Ahmed, Arjun Kumar Tallada, Vidya Pai, Almas BinnalDocument6 pagesNandita Shenoy, Junaid Ahmed, Arjun Kumar Tallada, Vidya Pai, Almas BinnalSela PutrianaNo ratings yet
- Hypoglossia Type 1A - Report of A Case A... Dian Journal of Dental Research (IJDR)Document3 pagesHypoglossia Type 1A - Report of A Case A... Dian Journal of Dental Research (IJDR)Sela PutrianaNo ratings yet
- Jurnal Cheek 2Document3 pagesJurnal Cheek 2Sela PutrianaNo ratings yet
- Congenital Macroglossia: Clinical Features and Therapeutic Strategies in Pediatric PatientsDocument5 pagesCongenital Macroglossia: Clinical Features and Therapeutic Strategies in Pediatric PatientsSela PutrianaNo ratings yet
- Daftar Pustaka Farmako Prak IDocument1 pageDaftar Pustaka Farmako Prak ISela PutrianaNo ratings yet
- Failure AnesthesiaDocument6 pagesFailure AnesthesiaSela PutrianaNo ratings yet
- Jurnal AntibiotikDocument5 pagesJurnal AntibiotikSela PutrianaNo ratings yet
- Quantitative Examination Second Term 20212022 CompleteDocument15 pagesQuantitative Examination Second Term 20212022 CompleteOladele FamesoNo ratings yet
- Psychological Hardiness in Relation To Entrepreneurial Orientation Among Youth of PunjabDocument7 pagesPsychological Hardiness in Relation To Entrepreneurial Orientation Among Youth of PunjabPriyashree RoyNo ratings yet
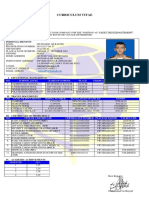
- Curriculum Vitae: To: Crewing Manager Subject: Deck Cadet Application Dear Sir or MadamDocument1 pageCurriculum Vitae: To: Crewing Manager Subject: Deck Cadet Application Dear Sir or MadamWiwit PrihatiniNo ratings yet
- Managing ServiceguardDocument534 pagesManaging ServiceguardSagar BachalNo ratings yet
- Science Society Education - Topical Issues and Development Prospects - 5 7.07.20Document341 pagesScience Society Education - Topical Issues and Development Prospects - 5 7.07.20OS IONo ratings yet
- Pur CommunicationDocument20 pagesPur CommunicationDarlNo ratings yet
- Somaiya Vidyavihar UniversityDocument2 pagesSomaiya Vidyavihar UniversitySumit BhongNo ratings yet
- Pancasila Character EducationDocument6 pagesPancasila Character EducationDaniel Prayoga D100% (1)
- Cold Calling 26 AugDocument4 pagesCold Calling 26 AugGajveer SinghNo ratings yet
- The Vicious CycleDocument3 pagesThe Vicious CycleSimona IlieNo ratings yet
- Standard Form of Quadratic EquationDocument2 pagesStandard Form of Quadratic EquationTheKnow04No ratings yet
- Linking The Van Hiele Theory To Instruction 2015Document11 pagesLinking The Van Hiele Theory To Instruction 2015Oliver IpoNo ratings yet
- ECON2206 Course OutlineDocument12 pagesECON2206 Course OutlineChris Bury0% (1)
- Selection 6th 5 in 1 EM Term - 1Document64 pagesSelection 6th 5 in 1 EM Term - 1Jeeva BharathiNo ratings yet
- Day 1 Introduction, Project Environment & Role of Project Manager (1) - Read-Only (53) - Read-OnlyDocument33 pagesDay 1 Introduction, Project Environment & Role of Project Manager (1) - Read-Only (53) - Read-OnlySuraj ShresthaNo ratings yet
- 1890 Pgmedicalcqsecondphaseallotments201920Document60 pages1890 Pgmedicalcqsecondphaseallotments201920krishnaNo ratings yet
- Course Title: Teachers As Reflective - Course Code: PGDT 422 - Credit Hour: 2Document45 pagesCourse Title: Teachers As Reflective - Course Code: PGDT 422 - Credit Hour: 2yohanes100% (3)
- Junior HSE AssistantDocument2 pagesJunior HSE AssistantMuhammad AdnanNo ratings yet
- How To Qualify As A Lawyer in The Philippines: Back To List of CountriesDocument4 pagesHow To Qualify As A Lawyer in The Philippines: Back To List of CountriesJhei VictorianoNo ratings yet
- Bryson Yurkemik: Employment ObjectiveDocument2 pagesBryson Yurkemik: Employment Objectiveapi-345358688No ratings yet
- Method For Shifting Focus From Outcome To ProcessDocument2 pagesMethod For Shifting Focus From Outcome To ProcessEduard ShNo ratings yet
- Unit 1: Curriculum Essentials: Intended Learning OutcomesDocument8 pagesUnit 1: Curriculum Essentials: Intended Learning Outcomesjestony matilla100% (1)
- BJCP Study GuideDocument77 pagesBJCP Study GuideCarlos BarrientosNo ratings yet
- Sme Chapther Unsa: Plan Anual 2018Document6 pagesSme Chapther Unsa: Plan Anual 2018JuniorMendoza97No ratings yet
- Siti Asyifa Soraya Noordin - Artikel - Infomasi Karir - Sman1garut PDFDocument17 pagesSiti Asyifa Soraya Noordin - Artikel - Infomasi Karir - Sman1garut PDFSiti AsyifaNo ratings yet