Professional Documents
Culture Documents
The Pelvis & Perineu M: Able of Ontents
Uploaded by
Waqar WikiOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The Pelvis & Perineu M: Able of Ontents
Uploaded by
Waqar WikiCopyright:
Available Formats
TH E PE LV I S & PE R IN EU M
T ABLE OF C ONTENTS
Muscles of the Pelvic Cavity .................................................................................. 2 Ureters ..................................................................................................................... 15
Walls of the Pelvis.................................................................................................... 3 Urethra ..................................................................................................................... 16
Sacral Plexus ............................................................................................................. 4 Vas Deferens........................................................................................................... 18
Coccygeal Plexus ...................................................................................................... 6 Seminal Vesicles ..................................................................................................... 18
Sympathetic Trunks ................................................................................................. 6 Ejaculatory Ducts................................................................................................... 19
Parietal Branches of the Internal Iliac Artery ...................................................... 7 Prostate Gland ........................................................................................................ 19
General Anatomy ..................................................................................................... 9 Arterial Supply to the Prostate ............................................................................. 20
Peritoneal Relations ................................................................................................. 9 Venous Drainaige from the Prostate .................................................................. 20
Relations of the Rectum ....................................................................................... 10 Innervation of the Prostate .................................................................................. 20
Arterial Supply to the Rectum ............................................................................. 10 Lymphatic Drainage of the Prostate ................................................................... 20
Venous Drainage from the Rectum .................................................................... 11 General Anatomy of the Anal Canal................................................................... 21
Innervation of the Rectum ................................................................................... 11 Arterial Supply to the Anal Canal ........................................................................ 22
Lymphatic Drainage of the Rectum.................................................................... 11 Venous Drainage from the Anal Canal .............................................................. 22
General Anatomy of the Bladder ........................................................................ 12 Innervation of the Anal Canal ............................................................................. 22
The Bladder Bed .................................................................................................... 13 Lymphatic Drainage of the Anal Canal .............................................................. 22
Structure of the Bladder ........................................................................................ 14 External Anal Sphincter ........................................................................................ 23
Arterial Supply to the Bladder ............................................................................. 14 Internal Anal Sphincter ......................................................................................... 23
Venous Drainage from the Bladder .................................................................... 14 Internal Pudendal Artery ...................................................................................... 23
Innervation of the Bladder ................................................................................... 15 Pudendal Nerve ...................................................................................................... 23
Lymphatic Drainage of the BLadder .................................................................. 15
C REATED BY M ICHAEL C HEERAN D AVID ON 12/05/1999 12:15:00 P AGE 1 OF 23
T HE P ELVI C C AVIT Y
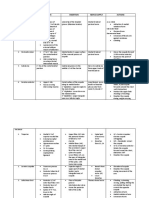
M U S C L E S OF T H E P E LV I C C AV I T Y
NAME. ORIGIN. INSERTION INNERVATION ACTION
1. Pelvic surfaces of Ileum and Passes through the Lesser Sciatic 1. Lateral rotation of thigh
Nerve to Obturator Internus
Obturator Internus Ischium Foramen to the Greater 2. Assists holding head of
(L5, S1, S2)
2. Obturator membrane Trochanter of Femur Femur in the Acetabulum
1. Pelvic surface of 2nd to 4th
1. Lateral rotation of thigh
Sacral segments
2. Abduction of thigh
Piriformis 2. Superior margin of Greater Greater Trochanter of Femur Ventral Rami of S1 & S2
3. Assists holding head of
Sciatic Notch
Femur in the Acetabulum
3. Sacrotuberous Ligament
1. Pass posteriorly to unite 1. Supports pelvic viscera
1. Pubic Symphysis with its partner 2. Resists inferior thrust of
Puborectalis
2. Superior Pubic Ramus 2. Perineal Body increased abdominal
(Pubovaginalis) pressure
1. Unite with its partner to 3. Raises pelvic floor
1. Superior Pubic Ramus 4. Support prostate or
form a raphé behind the Perineal branches of the S3 & S4
Pubococcygeus 2. Fascia of Obturator posterior wall of the vagina
Anorectal junction nerves (enter the muscle’s pelvic
Internus 5. Raises the anal canal over a
2. Anococcygeal Body surface)
descending mass of faeces,
Levator Ani
1. Tendinous arch of and increases anorectal
Obturator Internus 1. Coccyx
Iliococcygeus angle supports weight of
2. Pelvic aspect of Ischial 2. Anococcygeal Body
faeces and relieves external
Spine
anal sphincter
1. Assist Levator Ani in
1. Pelvic surface of Ischial
1. Lateral margin of Coccyx supporting pelvic viscera
Coccygeus Spine Branches of S4 & S5 nerves
2. S5 vertebra 2. Pull coccyx anteriorly
2. Sacrospinous Ligament
elevate pelvic floor
C REATED BY M ICHAEL C HEERAN D AVID ON 12/05/1999 12:15:00 P AGE 2 OF 23
WA L L S OF T H E P E LV I S
ANTERIOR WALL PELVIC FLOOR
Pubic Symphysis Funnel shaped Pelvic Diaphragm, composed of:
Bodies of Pubic Bones + Superior and Inferior Rami 2 Levator Ani muscles
Terminate laterally in the bodies and rami of the Ischium. 2 Coccygeus muscles – lying directly on the posterior border of the
Obturator Internus muscle, and its overlying fascia Levator Ani muscles continuous sheet of muscle.
Pelvic Diaphragm closes the Pelvic Outlet, except for an anterior
LATERAL WALLS deficiency:
Bounded by the anterior margin of the Puborectalis fibres of Levator
Obturator Internus covers most of these walls. Ani
Medial to this, are the Obturator nerves and vessels, and other Filled with loose fascia around the Prostate Gland (male), or Vagina
branches of the Internal Iliac Artery. (female).
Pelvic Fascia, near the pelvic brim The Urogenital Diaphragm and its superior fascia close anterior
deficiency.
POSTERIOR WALL
Pelvic Diaphragm separates the pelvic cavity from the perineum.
Sacrum There are a number of midline structures associated with the Pelvic
Adjacent parts of the Ilium bones Diaphragm:
Sacro-iliac joints + associated ligaments The rectum lies directly against the anterior aspect of the sacrum.
Piriformis muscles line the lateral portion of the posterior wall. At the level of the Pelvic Diaphragm, is the Anorectal Junction.
Medial to the piriformis, lie the sacral plexus and internal iliac vessels Behind the anorectal junction, lies the Anococcygeal Body.
forms a muscular bed for the sacral plexus. Fibrous tissue in front of the anorectal junction, forms the Perineal
Body.
C REATED BY M ICHAEL C HEERAN D AVID ON 12/05/1999 12:15:00 P AGE 3 OF 23
I NNERVATION AND B LOODY S UPPLY OF THE P ELVIC C AVITY
SACRAL PLEXUS
Ventral 1º Ramus of L4 – runs laterally into Psoas Major, from which it Branches of Ventral 1º Rami of S2 & S3, turn medially, and lie on the
sends a descending branch. anterior aspect of the sacrum.
Ventral 1º Ramus of L5 – arises from behind the Lumbosacral Form the Pelvic Splanchnic Nerves.
Intervertebral Disc. Cell bodies lie within Lateral Horns of Grey Matter of Spinal Cord.
Turns forwards and inferiorly. Compose the Sacral part of the Cranio-Sacral Parasympathetic
Lies in a small triangular recess: Outflow.
Lateral boundary = Psoas Major Ventral 1º Ramus of S4.
Medial boundary = the Lumbosacral Intervertebral Disc Emerges through the lowest Sacral Foramen, and enters the Pelvic
Inferior boundary = Ala of Sacrum. Cavity.
Passes down, anterior to the Ala of the Sacrum, and joined by the Lies on the surface of Coccygeus muscle.
descending branch of the Ventral 1º Ramus of L4. Ascending branch – joins the Sacral Plexus and eventually its fibres
This forms the Lumbosacral Trunk. form the Pudendal Nerve.
Lumbosacral Trunk lies anterior to the Sacroiliac joint, but behind the Descending branch – turns inferiorly to join the Coccygeal Plexus.
Common Iliac Vessels.
Runs down and across the anterior aspect of Piriformis.
Passes through the lower part of the Greater Sciatic Foramen.
Enters the tissue of the buttock.
Ventral 1º Rami of S1, S2 (½ inch diameter) & S3 (a little smaller).
Emerge through corresponding Sacral Foramina, and enter the
Pelvic Cavity.
All lie on Piriformis (a muscular bed for the Sacral Plexus).
Head to the lower border of the Greater Sciatic Foramen.
As they pass through, they join together to form the Sacral
Plexus.
Recombine to form efferent branches that emerge through the
foramen, and enter the tissue of the buttock.
C REATED BY M ICHAEL C HEERAN D AVID ON 12/05/1999 12:15:00 P AGE 4 OF 23
SCIATIC NERVE BRANCHES TO PIRIFORMIS (S1, S2)
Nerve to the lower limb, with a root value of L4-S3. BRANCHES TO LEVATOR ANI AND COCCYGEUS (S3-S5)
Largest nerve of the body (≈ 2 cm wide).
NERVE TO QUADRATUS FEMORIS (L4-S1)
Passes through Greater Sciatic Foramen, inferior to Piriformis, to enter
the Gluteal region. NERVE TO OBTURATOR INTERNUS (L5-S2)
PUDENDAL NERVE
OBTURATOR NERVE
Root value of S2-S4.
Accompanies the Internal Pudendal Artery. Arises from the Lumbar Plexus in the Abdomen.
Leaves the pelvis through the Greater Sciatic Foramen, between Enters the Pelvis Minor, and runs along the lateral wall of the Pelvis, in
Piriformis and Coccygeus muscles. the extra-peritoneal fat.
Hooks around the Sacrospinous Ligament, and enters the perineum Reaches the Obturator Foramen, where it divides into anterior and
through the Lesser Sciatic Foramen. posterior parts.
Supplies the External Anal Sphincter, and other muscles of the Leaves through the Obturator Canal, and supplies the Adductor muscles
perineum. of the thigh.
Sensory supply to the external genitalia.
Terminates as the Dorsal Nerve of the Penis/Clitoris.
SUPERIOR GLUTEAL NERVE
Leaves through the Greater Sciatic Foramen, above Piriformis.
Supplies Gluteus Medius, Gluteus Minimus, and the Tensor Fascia Latae
muscles.
C REATED BY M ICHAEL C HEERAN D AVID ON 12/05/1999 12:15:00 P AGE 5 OF 23
C O C C YG E A L P L E X U S S Y M PA T H E T I C T RU N K S
Formed by the: Tucked in behind the Abdominal Aorta and the Inferior Vena Cava.
Descending branch of the Ventral 1º Ramus of L4 Lie on the posterior abdominal wall.
Pass onto pelvic aspect of Coccygeus muscle. Passing caudally, they run behind the Common Iliac Vessels lie on the
Ventral 1º Ramus of L5 anterior aspect of the Sacrum.
Coccygeal Spinal Nerves. Sympathetic Trunks lie just medial to the Anterior Sacral Foramina.
Emerge from fibrous posterior wall of Sacral Canal. On reaching the anterior aspect of the Coccyx, they terminate.
Turn forward to enter the Pelvic Cavity, by piercing Coccygeus Unite to form a single terminal ganglion = Ganglion Impar.
muscle. White Rami Communicantes restricted to the Thoracolumbar
On the pelvic aspect of Coccygeus, these nerves are joined simply by 2 Sympathetic Outflow (T1-L2)
nerve loops Coccygeal Plexus. Grey Rami Communicantes connect to Ventral 1º Rami of
Efferent branches supply part of Coccygeus. corresponding spinal nerves.
Efferent Cutaneous branches pass back through Coccygeus, and supply Convey post-ganglionic sympathetic fibres to all the branches of the
an area of perineal skin just over the Coccyx. Sacral and Coccygeal Plexuses.
Distribute to Sweat Glands, Hair Follicles, and Blood Vessels.
Some branches of the segmental ganglia, turn medially, to form the:
Autonomic Plexus – sends visceral branches.
Left & Right Inferior Hypogastric Plexuses – innervate the pelvic
viscera.
C REATED BY M ICHAEL C HEERAN D AVID ON 12/05/1999 12:15:00 P AGE 6 OF 23
PA R I E TA L B R A N C H E S OF T H E I N T E R NA L I L I A C A RT E RY
The common iliac artery divides, anterior to the Sacro-Iliac Joints, at the level of the Lumbosacral Intervertebral Disc.
The Internal Iliac artery is 2.5 cm long.
It turns over the Pelvic Brim
Goes to the upper border of the Greater Sciatic Foramen.
There it breaks up into a sheaf of Parietal and Visceral branches.
OBTURATOR ARTERY INTERNAL PUDENDAL ARTERY
Arises close to where the umbilical artery arises (obliterated to form the Passes infero-laterally, over Piriformis muscle and the ventral 1º rami of
medial umbilical ligaments, which form medial umbilical folds in the the sacral plexus.
peritoneum). Passes between Piriformis and Coccygeus, to the inferior part of Greater
Runs antero-inferiorly on the obturator fascia, on the lateral wall of the Sciatic Foramen.
pelvis. Hooks around the Sacrospinous Ligament.
Runs between the obturator nerve and vein. Enters the perineum via the Lesser Sciatic Foramen.
Leaves through the Obturator Canal. Pass through the Pudendal Canal, in the lateral wall of the Ischioanal
Supplies muscles of the medial compartment of the thigh. Fossa.
Within the pelvis, it gives off muscular branches, and nutrient branches Just prior to the Pubic Symphysis, it divides into its terminal branches.
to the Ilium and Pubis. Deep arteries of the penis/clitoris.
The Obturator Artery may abnormally arise from the Inferior Epigastric Dorsal arteries of the penis/clitoris.
Artery (a branch of the External Iliac artery).
In this case, it simply turns inferiorly over the pelvic brim, and goes
straight to the Obturator Canal.
C REATED BY M ICHAEL C HEERAN D AVID ON 12/05/1999 12:15:00 P AGE 7 OF 23
INFERIOR GLUTEAL ARTERY LATERAL SACRAL ARTERIES
Runs over the ventral 1º rami of the sacral plexus. Superior and inferior vessels on each side.
Passes posteriorly between S2 & S3 ventral 1º rami. Arise from the posterior aspect of the Internal Iliac artery.
Leaves pelvis through the Greater Sciatic Foramen, inferior to Piriformis. Descend, anterior to the Ventral 1º Rami of the Sacral Nerves.
Supplies skin and muscles of the buttock and posterior thigh. Superior – disappears through the 1st ventral foramen.
Inferior – passes through the 2nd ventral foramen, sending branches to
SUPERIOR GLUTEAL ARTERY the 3rd & 4th ventral foramina.
Enter the sacral canal, and supply the Spinal Meninges, and the Roots of
Large artery; passes posteriorly between Lumbosacral Trunk and the the Sacral Nerves.
Ventral 1º Ramus of S1. Some branches of these pass from the sacral canal, through the dorsal
Leaves the pelvis through the superior part of the Greater Sciatic sacral foramina.
Foramen, above Piriformis. Supply the muscles and skin overlying the dorsum of the sacrum.
Supplies the Gluteal muscles of the buttock.
ILIOLUMBAR ARTERY
Arises from the posterior aspect of the Internal Iliac Artery
Runs supero-laterally to the Iliac Fossa.
Passes anterior to the Sacroiliac Joint, and posterior to the Psoas Major
muscle.
Separating the Obturator Nerve from the Lumbosacral Trunk.
Within the iliac fossa, it divides:
Iliac branch – supplies Iliacus muscle, and the Ilium.
Lumbar branch – supplies Psoas Major and Quadratus Lumborum
muscles.
C REATED BY M ICHAEL C HEERAN D AVID ON 12/05/1999 12:15:00 P AGE 8 OF 23
T HE R ECTUM
G E N E R A L A NA TOM Y P E R I TON E A L R E L A T I O N S
Fixed terminal part of the large intestine, continuous superiorly with the Superior 1/3 – peritoneum covers the anterior and lateral surfaces.
Sigmoid Colon. Lateral reflections of peritoneum form Para-Rectal Fossae on each
Begins anterior to S3, and is 12-15 cm long. side.
Terminates 3-4 cm antero-inferior to the tip of the coccyx. Permit the rectum to distend as it fills with faeces.
At the anorectal junction, there is a sharp angle maintained by the Middle 1/3 – peritoneum covers only the anterior surface of the rectum.
Puborectalis fibres of Levator Ani. Inferior 1/3 – has no peritoneal coverings.
These fibres draw the anorectal junction anteriorly, to increase
the angle. MALE
Prevents faeces from entering the anal canal and relieves the
pressure on the External Anal Sphincter. Peritoneum is reflected from the anterior surface of the middle 1/3 of the
The terminal part of the rectum has a dilation = Rectal Ampulla. rectum to the posterior wall of the bladder.
Distensible stores faeces, just before it is expelled during Forms the floor of the Rectovesical Pouch.
defecation. In male children, the peritoneum will extend down as far as the base of
This inferior portion of the rectum lies just posterior to the Prostate the prostate, since the bladder has not yet descended from the abdomen.
Gland (male), or the Vagina (female).
FEMALE
The termination of the rectum at the anorectal junction lies posterior to
the Perineal Body in both sexes. The peritoneum is reflected from the anterior surface of the middle 1/3
The rectum has 3 sharp flexures as it follows the sacrococcygeal curve of the rectum to the Posterior Fornix of the Vagina.
within the coronal plane, it is “S”-shaped. Forms the floor of the Recto-uterine Pouch (of Douglas).
It first bends to the right, then to the left, and then to the right as it
returns to the midline at the anorectal junction.
These flexures throw up folds of the mucous, submucous, and
circular muscle coats, at the concavities of the rectum.
These Transverse Rectal Folds partly occlude the lumen of the
rectum, and are maintained by prolongations of the Taeniae Coli.
Transverse Rectal Folds form a series of shelves within the rectal
lumen, which will support a column of faeces.
C REATED BY M ICHAEL C HEERAN D AVID ON 12/05/1999 12:15:00 P AGE 9 OF 23
RELATIONS OF THE REC TUM A RT E R I A L S U P P LY TO T H E R E C T U M
ANTERIOR Superior Rectal artery – continuation of the Inferior Mesenteric artery.
Supplies the terminal part of the sigmoid colon, and the superior part
Male of the rectum.
At the level of S3, behind the origin of the rectum, it divides into 2:
Fundus of the Urinary Bladder. These right and left branches cross the Left Common Iliac
Rectovesical Septum – 2 layers of peritoneum in the median plane, Vessels
separating the rectum from the urinary bladder. Descend into Pelvis Minor, via the Sigmoid Mesocolon.
Terminal parts of the Ureters Descend along each side of the rectum.
Vasa Deferentes Middle Rectal arteries – branches of the Internal Iliac arteries.
Seminal Vesicles Supply the middle and inferior parts of the rectum.
Prostate Gland Inferior Rectal arteries – branches of the Internal Pudendal artery (a parietal
branch of the Internal Iliac).
Female Supply the inferior part of the rectum.
Originate in the Ischioanal Fossae.
Vagina Small branches of the Median Sacral Artery supply the rectum posteriorly.
Recto-uterine Pouch – separates posterior fornix of vagina and the
cervix, from the rectum.
(Weak) Recto-uterine Septum – separates the vagina and rectum.
POSTERIOR
Inferior 3 Sacral Vertebrae (S2-S5) + loosely attached fascial sheath.
Coccyx
Anococcygeal Body
Median Sacral Vessels (terminal continuation of the abdominal aorta).
Branches of the Superior Rectal Artery
Inferior ends of the Sympathetic Trunks & Sacral Plexuses.
C REATED BY M ICHAEL C HEERAN D AVID ON 12/05/1999 12:15:00 P AGE 10 OF 23
V E N O U S D R A I NA G E F R OM T H E R E C T U M I N N E RVA T I ON O F T H E R E C T U M
Drained by the Superior Rectal Vein Inferior Mesenteric Vein. Middle Rectal Plexus is derived from the Inferior Hypogastric Plexus (a
Middle and Inferior Rectal Veins Internal Iliac Vein. sympathetic ganglion)
Rectal Venous Plexus: 4-8 nerves pass directly to the rectum – sympathetic,
Internal Rectal Venous Plexus – just deep to the epithelium of the parasympathetic and sensory supply.
rectum. Parasympathetic supply is derived from S2-S4.
Drains to the Superior Rectal Vein Join the Inferior Hypogastric Plexus, via the Pelvic Splanchnic
Communicates freely with the External Rectal Venous Plexus. Nerves.
External Rectal Venous Plexus – lies outside the muscle coats of the Sensory fibres follow the path of the Pelvic Splanchnic Nerves, and
rectum. respond to distension of the rectum.
Superior part drains to the Superior Rectal Vein too.
Middle part drains to the Middle Rectal Vein.
Inferior part drains to the Internal Pudendal Vein.
LY M P H A T I C D R A I NA G E O F T H E R E C T U M
Superior ½ - Superior Rectal vessels Para-rectal Lymph Nodes Inferior Mesenteric Lymph Nodes Aortic Lymph Nodes.
Inferior ½ - lymph vessels pass superiorly with the middle rectal arteries Internal Iliac Lymph Nodes.
C REATED BY M ICHAEL C HEERAN D AVID ON 12/05/1999 12:15:00 P AGE 11 OF 23
U RINARY O RGANS
G E N E R A L A NA TOM Y O F T H E B L A D D E R
Hollow muscular vesicle, for storing urine (up to 500 ml). Apex – the anterior end of the bladder, points anteriorly to the superior
Infants – the bladder lies in the abdomen, even when empty. edge of the pubic symphysis.
Enters the Pelvis Major at the age of 6. Infero-lateral Surfaces – direct relations with the fascia over Levator Ani
Not entirely within the Pelvis Major, until puberty. and Obturator Internus.
Adult – when empty, it lies almost entirely within the Pelvis Minor, Converges posteriorly with Fundus, to form the Neck of the
posterior and slightly superior to the pubic bones. Bladder.
Separated from the pubic bones by the Retro-pubic Space. This is where the lumen of the bladder opens into the prostatic
As it fills with urine, it distends into the Pelvis Major, and even up to urethra of the male.
the level of the Umbilicus. In the male, the Neck of the Bladder rests on the Prostate Gland.
Its shape, size and position vary with the amount of urine it contains, and Lie just anterior to the Perineal Body.
with age. From the neck of the bladder, the Median Umbilical Fold of peritoneum
The mucous membrane of the bladder is loosely attached to its muscular passes superiorly to the Umbilicus.
walls. This fold is raised by the Median Umbilical Ligament, that is the
Therefore thrown into numerous Rugae (folds). remnant of the embryonic Urachus.
Except for a small triangular area on the Fundus (base) of the
Bladder = Trigone.
Here the mucous membrane is smooth and firmly bound down
to the muscular wall.
From its lower end, the urethra leaves the bladder at the Internal
Urethral Orifice.
Posterior to this is a small elevation = Uvula Vesicae.
The middle lobe of the Prostate Gland produces it.
The cadaveric, empty bladder has 4 surfaces: superior surface, 2 antero-
inferior surfaces (that face anteriorly), and a Fundus (posterior surface).
Fundus – closely related to the anterior wall of the vagina (female), and
rectum (male).
C REATED BY M ICHAEL C HEERAN D AVID ON 12/05/1999 12:15:00 P AGE 12 OF 23
MALE
THE BLADDER BED
The peritoneum is reflected from the middle 3 of the rectum, onto the
1/
superior surface of the bladder. Shape of the bladder is largely determined by the structures related to it.
From the bladder it is then reflected onto the superior surfaces of Bladder is enveloped by loose connective tissue = Vesical Fascia.
the Vasa Deferentes and Seminal Vesicles. Within which is the Vesical Venous Plexus
The neck of the bladder is firmly fixes by Medial and Lateral The bladder bed is formed by the Pubic Bones, the Levator Ani muscles,
Puboprostatic Ligaments, on each side of the midline. and the Obturator Internus muscles.
The rest of the bladder is relatively free, within loose extra-peritoneal Posteriorly formed by the rectum.
fatty tissue. Female – fundus of the bladder is separated from the rectum, by the
As the bladder fills, it can easily expand superiorly into the extra- cervix and superior part of the vagina.
peritoneal fatty tissue of the anterior abdominal wall The neck of the bladder lies directly on the pelvic fascia, surrounding
This movement, thus strips the peritoneum from the Transversalis the short urethra.
Fascia of the abdominal wall. Male – fundus of the bladder is separated from the rectum, by the
ampullae of the Vasa Deferentes and Seminal Vesicles.
FEMALE
Its neck fuses with the Prostate Gland.
The peritoneum is reflected from the bladder near its posterior border,
onto the anterior wall of the uterus.
At the junction of its body, and cervix.
The vesico-uterine pouch extends between the bladder and the uterus.
C REATED BY M ICHAEL C HEERAN D AVID ON 12/05/1999 12:15:00 P AGE 13 OF 23
S T RU C T U R E O F T H E B L A D D E R A RT E R I A L S U P P LY TO T H E B L A D D E R
Wall of the bladder composed mainly of smooth muscle = Detrusor Superior Vesical arteries – branches of the Umbilical arteries (= branches
Muscle. of the Internal Iliac arteries).
External & Internal longitudinal layers Supply the antero-superior parts of the bladder.
Intermediate Circular layer. Males – the Inferior Vesical arteries (branches of the Internal Iliac
Towards the neck of the bladder, the circular fibres form the involuntary arteries), supply the Fundus of the Bladder.
Internal Sphincter Vesicae. Females – the Vaginal Arteries replace the Inferior Vesical arteries, and
Male – the muscle fibres from the neck of the bladder are supply the postero-inferior parts of the bladder.
continuous with the connective tissue stroma of the prostate. Obturator and Inferior Gluteal arteries also send branches to the bladder.
Female – muscle fibres of the neck of the bladder are continuous
with those in the wall of the urethra.
V E N OU S D R A I NA G E F R OM T H E B L A D D E R
Mucous membrane of the bladder is lined with transitional epithelium
can be stretched.
The Ureteric Orifices are located at the lateral angles of the Trigone. Correspond to the arteries, and are tributaries of the Internal Iliac Vein.
Ureters pass infero-medially through the bladder wall, to prevent Males – the Vesical and Prostatic Venous Plexuses envelop the base of
urine back-flow. the bladder, the prostate, the seminal vesicles, vasa deferentes, and the
Increased intra-vesical pressure will press the walls of the ureters terminal parts of the Ureters.
together. Male Vesical Venous Plexus Inferior Vesical Veins Internal
Urine cannot pass retrogradely and damage the kidneys. Iliac Veins.
Internal Urethral Orifice is at the inferior angle of the Trigone. Females – the Vesical Venous Plexus envelops the pelvic part of the
The small slit-like Ureteric Orifices are connected by a narrow Inter- urethra, and the neck of the bladder.
ureteric Ridge – forms the superior margin of the Trigone. The Female Vesical receives blood from the Dorsal Vein of the
Caused by the continuation of the internal longitudinal coat of the Clitoris, communicates with the Vaginal Venous Plexus.
right ureter meeting that of the left ureter.
The terminal portions of the ureter as they travel obliquely through the
fundus wall.
Cause a depression, lateral to each Ureteric Orifice = Ureteric Folds.
C REATED BY M ICHAEL C HEERAN D AVID ON 12/05/1999 12:15:00 P AGE 14 OF 23
I N N E RVA T I O N O F T H E B L A D D E R URETERS
Pelvic Splanchnic Nerves (S2-S4) – provide parasympathetic fibres. Thick-walled, expandable muscular ducts, with narrow lumina.
Motor to the Detrusor muscles. Each is continuous superiorly with the funnel-shaped Renal Pelvis.
Inhibitory to the Internal Vesical Sphincter. Emerges through the Hilum, and descends the medial margin of the
Stimulated by stretch. Kidney to the inferior pole – here begins the Ureter Proper.
Cause the bladder to contract, and the sphincter to relax. The abdominal part of each ureter is 12.5 cm long, and 5 mm wide.
Urine flows into the urethra. Adheres closely to the parietal peritoneum, lying retro-peritoneally.
Sympathetic fibres are derived from T11-L2. Descends vertically, anterior to Psoas Major Muscle.
Inhibitory to the Detrusor muscles. Both ureters cross the pelvic brim, and the External Iliac Artery – just
Constrict the sphincter. beyond the bifurcation of the Common Iliac Artery.
Innervation of the bladder is from the Vesical Nerve Plexus. The pelvic parts of the ureters run postero-inferiorly on the lateral wall of
Sympathetic, parasympathetic, and sensory. the pelvis.
Sensory fibres are visceral, and transmit pain. Run external to the parietal peritoneum, and anterior to the Internal
Continuous with the Inferior Hypogastric Plexus. Iliac Arteries.
Continue to a point about 1.5 cm superior to the Ischial Spines.
Then curves antero-medially, above the Levator Ani muscle,
LY M P H A T I C D R A I NA G E O F T H E B L A D D E R
adhering closely to the peritoneum.
Male – Vas Deferens passes between the Ureter and the Peritoneum.
Superior part of bladder External Iliac Lymph Nodes. The ureter lies lateral to the Vas, and enters the postero-superior
Inferior part of bladder Internal Iliac Lymph Nodes. angle of the Bladder, just superior to the Seminal Vesicles.
Neck region Common Iliac Lymph Nodes. Females – ureter descends on the lateral wall of the Pelvis Minor
(forming the posterior boundary of the Ovarian Fossa).
Passes medial to the origin of the Uterine Artery.
Continues to descend to the level of the Ischial Spine – here it is
crosses superiorly by the Uterine Artery.
Passes close to the lateral fornix of the Vagina, as it passes down the
posterior fixed margin of the Broad Ligament
Runs horizontally forward, to enter the postero-superior angle of the
Bladder.
C REATED BY M ICHAEL C HEERAN D AVID ON 12/05/1999 12:15:00 P AGE 15 OF 23
URETHRA
MALE URETHRA Membranous Urethra
Long muscular tube – 15-20 cm long. Lies in the Deep Perineal Space, which is enclosed by the superior and
Conveys urine from the bladder to the exterior, via the External Urethral inferior fascial layers of the Urogenital Diaphragm.
Orifice at the tip of the Glans Penis.
Also provides a route of exit for semen. Spongy Urethra
Prostatic Urethra Longest part of the male urethra (15-16 cm long).
Passes through the Bulb of the Penis, and the Corpus Spongiosum.
3 cm long, beginning at the Internal Urethral Orifice, at the apex of the Ends at the External Urethral Orifice – the narrowest part of the urethra.
Trigone of the Bladder. The lumen of the spongy urethra is ≈ 5mm in diameter.
Descends through the Prostate Gland, with a gentle anterior concavity. Expanded in the Bulb of the Penis, to form the Intrabulbar Fossa.
Terminates by piercing the Superior Fascia of the Urogenital Diaphragm. Also expanded in the Glans Penis, to form the Navicular Fossa.
Its lumen is narrower superiorly and inferiorly, than in the middle. Slender ducts of the Bulbourethral Glands open into the proximal part of
The prostatic urethra is the widest and most dilatable part of the entire the Spongy Urethra.
urethra, even though it is within the substance of the Prostate Gland. About 3 cm distal to the Perineal Membrane.
Urethral Crest – median longitudinal ridge on the external aspect of its On the dorsal surface of the Spongy Urethra, there are minute openings
posterior wall. of the mucous-secreting Urethral Glands.
This has a groove on each side = Prostatic Sinuses.
Into which open up most of the Prostatic Ductules.
Others open up into the sides of the Urethral Crest.
In the middle part of the Urethral Crest, is a rounded eminence =
Seminal Colliculus.
On which is a slit-like orifice, that leads to a vestigial cul-de-sac (≈ 5
mm long).
This is the Prostatic Utricle – on each side of its orifice, are the slit-
like apertures of the Ejaculatory Ducts.
C REATED BY M ICHAEL C HEERAN D AVID ON 12/05/1999 12:15:00 P AGE 16 OF 23
FEMALE URETHRA
Short muscular tube (≈ 4 cm long), lined by mucous membrane.
Superior ½ corresponds to the male prostatic urethra.
Inferior ½ is homologous with the male membranous urethra.
Female Urethra passes antero-inferiorly from the urinary bladder.
Posterior and inferior to the Pubic Symphysis.
The urethra lies anterior to the vagina.
Inferiorly, it is so closely related to the vagina, that it appears
embedded in it.
Together they pass through the Pelvic & Urogenital Diaphragms,
and the Perineal Membrane.
External Urethral Orifice is located within the Vestibule of the Vagina.
2-3 cm posterior to the Clitoris, but immediately anterior to the
Vagina.
Surrounded by the Sphincter Urethrae muscle.
Para-urethral Glands (homologous with the Prostate), open into the
urethra, via a duct on each side, near the external urethral orifice.
C REATED BY M ICHAEL C HEERAN D AVID ON 12/05/1999 12:15:00 P AGE 17 OF 23
M ALE P ELVI C V ISCERA
VA S D E F E R E N S SEMINAL VESICLES
Thick walled, muscular tube, ≈45 cm long. Thin-walled, pear-shaped structure, about 5 cm long.
A continuation of the Duct of the Epididymus. Actually consists of a coiled tube that is 10-15 cm long.
Begins in the tail of the Epididymus. Honeycombed mucous membrane.
Terminates by joining the duct of the Seminal Vesicle, to form the Each extends supero-laterally from the Ampulla of the Vas, above the
Ejaculatory Duct. Prostate.
Ascends in the Spermatic Cord. Do not store sperm.
Passes through the Inguinal Canal. Secrete a thick alkaline fluid, which mixes with the sperm in the
Crosses over the external iliac vessels. Ejaculatory Ducts.
Enters the Pelvis Minor. Provide 70% of the ejaculate volume, and is expelled during orgasm, as
Passes across the lateral wall of the pelvis. the seminal vesicles contract.
Lies external to (but adherent to) the Parietal Peritoneum. The superior end of each Seminal Vesicle, is covered with peritoneum.
Lies medial to the vessels and nerves there. Lies posterior to the Ureter.
No other structure intervenes between it and the peritoneum. Separated from the Rectum, by the peritoneum of the Rectovesical
Near the postero-lateral angle of the bladder, it meets the Ureter, as it Pouch.
descends towards the Bladder. The inferior end of each Seminal Vesicle, is more closely related to the
It crosses the ureter, and then turns inferiorly. Rectum.
Runs down between the ureter and peritoneum, until it reaches the Only separated by the Rectovesical Septum.
Fundus of the Bladder. The duct of the each Seminal Vesicle joins the Ampulla of each Vas
The Vas Deferens now enlarges to form the Ampulla of the Vas, as it Deferens, to form the Ejaculatory Duct.
passes posterior to the bladder.
Its wall becomes thinner, and its lumen widens.
The 2 Ampullae of the Vasa gradually approach each other, as they
descend.
The Ampullae of the Vasa descend medial to the Seminal Vesicle.
Finally, they narrow as they unite with the ducts of the Seminal Vesicles,
to form the Ejaculatory Ducts.
C REATED BY M ICHAEL C HEERAN D AVID ON 12/05/1999 12:15:00 P AGE 18 OF 23
E JA C U L A TO RY D U C T S P RO S TA T E G L A N D
Each is a slender tube formed by the union of the ducts of the Seminal Largest gland of the male reproductive system – partly glandular and
Vesicle and Vas Deferens. partly fibromuscular.
Posterior to the neck of the urinary bladder. The size of a walnut.
About 2.5 cm long. Surrounds the Prostatic Urethra.
Run close together, antero-inferiorly, through the posterior part of the Enveloped in a thin, dense fibrous capsule (true capsule).
Prostate Gland (in the median plane). This is then enveloped in a loose Prostatic Sheath (false capsule), derived
Now run along the sides of the Prostatic Utricle, traversing the from pelvic fascia.
substance of the Prostate Gland. Continuous inferiorly with the superior fascia of the Urogenital
Converge to open into the Seminal Colliculus of the posterior wall of Diaphragm.
the Prostatic Urethra. Posteriorly forms part of the Rectovesical Septum.
They do so via 2 slit-like apertures, on each side of the Orifice Separates the bladder, prostate, and seminal vesicles from the
for the Prostatic Utricle. rectum.
The prostatic venous plexus lies beneath the fibrous capsule and
prostatic sheath – within the pelvic fascia.
BASE
Closely related to the neck of the urinary bladder.
The prostatic urethra enters the middle of the base, near its anterior
border.
APEX
Directed inferiorly, and closely related with the superior fascia of the
Urogenital Diaphragm.
Apex rests on the Sphincter Urethrae muscle.
Embraced by the antero-medial free margin of the Levator Ani muscle.
C REATED BY M ICHAEL C HEERAN D AVID ON 12/05/1999 12:15:00 P AGE 19 OF 23
INFEROLATERAL SURFACES Prostatic Secretion – thin milky fluid.
Expelled into prostatic urethra by contraction of smooth muscle in
Meet the sides of the convex anterior surface. the Prostate.
Rest on the fascia covering Levator Ani muscles. Provides 20% of the volume of the ejaculate.
POSTERIOR SURFACE
A RT E R I A L S U P P LY TO T H E P R O S TA T E
Triangular – facing posteriorly, and slightly inferiorly.
Lies directly on the anterior wall of the Ampulla of the Rectum.
Palpable via a rectal examination. Inferior Vesical Artery
Shallow median groove, demarcating the Lateral Lobes. Middle Rectal Artery – both branches of the Internal Iliac Artery.
Often fused referred to as a single posterior lobe.
Superiorly, there are another shallow grooves, where the ejaculatory V E N OU S D R A I NA I G E F RO M T H E P R O S TA T E
ducts pierce the Prostate.
Indicates the Middle Lobe – the section of the Prostate between the
The veins of the Prostate form the Prostatic Venous Plexus, around its
Ejaculatory Ducts and the Prostatic Urethra.
sides and base.
Middle Lobe lies posterior to the lower end of the bladder,
Located between the fibrous capsule and the fascial sheath.
producing the Uvula Vesicae.
Communicates with the Vesical and Vertebral Venous Plexuses.
Middle Lobe is superiorly in contact with the inferior portion of the
Trigone of the Bladder. Drains to the Internal Iliac Vein.
The Prostatic Utricle is located within the Middle Lobe.
I N N E RVA T I ON O F T H E P RO S TA T E
ANTERIOR SURFACE
Transversely narrow and convex. Parasympathetic supply – Pelvic Splanchnic Nerves (S2-S4).
Extends from the apex to the base. Sympathetic supply – Inferior Hypogastric Plexus.
Prostatic Ductules (20-30) open chiefly into the prostatic sinuses, on
each side of the Urethral Crest on the posterior surface of the Prostatic LY M P H A T I C D R A I NA G E O F T H E P R OS TA T E
Urethra.
Because most of the glandular tissue lies postero-lateral to the
prostatic urethra. Lymph vessels terminate chiefly in the Internal Iliac & Sacral Lymph
Nodes.
Some vessels from the posterior surface of the Prostate, pass with the
lymph vessels of the bladder to the External Iliac Lymph Nodes.
C REATED BY M ICHAEL C HEERAN D AVID ON 12/05/1999 12:15:00 P AGE 20 OF 23
T HE A NAL C ANAL
G E N E R A L A NA TOM Y O F T H E A NA L C A N A L
Terminal and most inferior part of the GI-Tract – 4 cm long. INTERIOR OF THE ANAL CANAL
Begins at the Anorectal Junction, at the level of the “U”-shaped sling
formed by the Puborectalis fibres of Levator Ani. Superior ½ of the mucous membrane has a series of longitudinal Anal
Ends at the anus, the external outlet of the GI Tract. Columns.
When not defecating, the anus is contracted into an antero-posterior slit. Contain terminal branches of the Superior Rectal Artery.
Internal and external sphincters surround anal canal. This is the site of a portal-systemic anastomosis.
Also surrounded by the Levator Ani muscles. Anorectal Line – indicated by the superior ends of the anal columns.
Descends postero-inferiorly, between the Anococcygeal and Perineal Demarcates the anorectal junction.
Bodies. Anal Valves – join the inferior ends of the anal columns.
The Taeniae Coli of the anterior and posterior surfaces of the Rectum Semilunar folds of epithelium.
and Anal Canal become increasingly fibro-elastic. Superior to these are a number of Anal Sinuses.
Form the Conjoint Longitudinal Tendon. Exude mucus when compressed by faeces.
Spread out as a series of septa, into the Ischioanal Fossae on either Pectinate Line – formed by the inferior comb-shaped limit of the anal
side of the Anal Canal (beneath the pelvic diaphragm). valves.
Divide up the Ischioanal Fossae into lobules of supporting fatty Indicates the junction of the superior part of the anal canal (derived
tissue. from the embryonic hindgut), and the inferior part of the anal canal
These support the anal canal, but allow distension. (derived from the embryonic anal pit).
Individual lobules can be filled with blood and pus, and since Indicates the squamo-columnar epithelial junction.
innervated by branches of the Pudendal Nerve, result in Superior ½ = columnar epithelium.
excruciating pain. Lower ½ = stratified squamous epithelium.
In the lower part of the anal canal, the mucous membrane is
arranged in a cushion pattern (at 3 o’clock, 7 o’clock and 11 o’clock).
Highly vascular and spongy.
Provides a watertight enclosure, which assists in continence.
At the anus, the moist hairless mucosa of the anal canal, becomes dry
hairy skin.
C REATED BY M ICHAEL C HEERAN D AVID ON 12/05/1999 12:15:00 P AGE 21 OF 23
A RT E R I A L S U P P LY TO T H E A N A L C A NA L I N N E RVA T I O N O F T H E A NA L C A N A L
Superior to the Pectinate Line: Superior to the Pectinate Line:
Superior Rectal Artery (a continuation of the Inferior Mesenteric Derived from the Inferior Hypogastric Plexus (sympathetic).
artery). The sympathetic nerves run mainly along the Inferior Mesenteric and
Its terminal branches run distally through the mucosa of the Anal the Superior Rectal arteries.
Columns. The parasympathetic supply is via the Pelvic Splanchnic nerves (S2-
They form anastomotic loops in the Anal Valves. S4), which run to the Inferior Hypogastric Plexus.
Inferior to the Pectinate Line: Sensitive to stretch only.
Inferior Rectal Arteries supply this region as well as the surrounding Inferior to the Pectinate Line:
muscles and peri-anal skin. Derived from Inferior Rectal Nerves, branches of the Pudendal
The Middle Rectal Arteries assist by communicating between the Nerve.
Superior and Inferior Rectal arteries. Sensitive to pain, touch and temperature.
V E N O U S D R A I NA G E F R O M T H E A N A L C A NA L LY M P H A T I C D R A I NA G E O F T H E A N A L C A N A L
Superior to the Pectinate Line: Superior to the Pectinate Line:
Internal Rectal Venous Plexus Superior Rectal Vein Inferior Internal Iliac Lymph Nodes Common Iliac & Lumbar Lymph
Mesenteric Vein. Nodes.
Inferior to the Pectinate Line: Inferior to the Pectinate Line:
Internal Rectal Venous Plexus Inferior Rectal Veins (around the Horizontal group of Superficial Inguinal Lymph Nodes.
margin of the external anal sphincter) Internal Iliac Vein.
Middle Rectal Veins – drain the muscle wall of the Ampulla of the
Rectum and Anal Canal.
Communicates between the Superior and Inferior Rectal Veins.
A tributary of the Internal Iliac Vein.
C REATED BY M ICHAEL C HEERAN D AVID ON 12/05/1999 12:15:00 P AGE 22 OF 23
E X T E R NA L A N A L S P H I N C T E R I N T E R NA L A N A L S P H I N C T E R
Large voluntary sphincter – surrounds the inferior 2/3 of the anal canal. Involuntary sphincter, surrounding the upper 2/3 of the anal canal.
Forms a broad band (2-3 cm wide) on each side of the anal canal. An inferior extension of the circular muscle of the rectum.
Consists of 3 parts: Subcutaneous, Superficial and Deep. Controlled by the Autonomic Nervous System:
Many branches of the Inferior Rectal nerve and artery, runs between the Sympathetic – closed.
superficial and deep parts. Parasympathetic – open (Pelvic Splanchnic Nerves).
Fibres of the external anal sphincter run from the Perineal Body to the Stimulated by the pressure of faeces in the Ampulla of the Rectum.
Anococcygeal Body and Coccyx.
Fibres blend superiorly with the Puborectalis fibres of Levator Ani.
I N T E R NA L P U D E N DA L A R T E RY
The fibres also overlap superiorly, with those of the internal anal
sphincter.
Subcutaneous Part – lies most inferiorly. Main arterial supply to perineal structures – lies in Pudendal Canal.
Slender, and surrounds the anus. Branches:
Annular fibres have no bony attachment. Inferior Rectal artery
Superficial Part – elliptical in shape. Posterior Scrotal/Labial arteries
Fibres extend from the tip of the Coccyx & Anococcygeal Body, Artery to the Bulb
around the anus, to the Perineal Body. Deep artery of the Penis/Clitoris
Moors the anus in the median plane. Dorsal artery of the Penis/Clitoris.
Deep Part – thick annular band, surrounding the anus like a collar.
Arise from the Perineal Body.
P U D E N DA L N E RV E
Some fibres cross to join the opposite Superficial Transverse
Perineal Muscle.
Superior fibres merge with the Puborectalis fibres of Levator Ani. Major nerve of the Perineum – also lies in the Pudendal Canal.
Together form the Chief Muscle of Continence. Branches:
Innervation – Inferior Rectal Nerve + Perineal Branch of S4. Inferior Rectal nerve
Actions – assists in closing anus and anal canal. Posterior Scrotal/Labial nerve
The deep part assists the Puborectalis fibres draw the anal canal Perineal Nerve
anteriorly increasing Anorectal Angle. Dorsal Nerve of the Penis/Clitoris.
C REATED BY M ICHAEL C HEERAN D AVID ON 12/05/1999 12:15:00 P AGE 23 OF 23
You might also like
- Oia Keisha PDFDocument7 pagesOia Keisha PDFJAN CAMILLE LENONNo ratings yet
- Pelvic WallDocument30 pagesPelvic Walllasheenmohamed46No ratings yet
- Muscles of The Head Origin Insertion ActionDocument4 pagesMuscles of The Head Origin Insertion Actionanon ymousNo ratings yet
- Anatomy Lecture Chapter 12 Vertebral Coulmn and Back v2Document3 pagesAnatomy Lecture Chapter 12 Vertebral Coulmn and Back v2Neil Vincent De AsisNo ratings yet
- The Inner Ear: Including Otoneurology, Otosurgery, and Problems in Modern WarfareFrom EverandThe Inner Ear: Including Otoneurology, Otosurgery, and Problems in Modern WarfareNo ratings yet
- I. Introduction To The Upper ExtremityDocument10 pagesI. Introduction To The Upper ExtremityKailash KhatriNo ratings yet
- Upper Extremity (Anatomy)Document17 pagesUpper Extremity (Anatomy)Margareth Christine CusoNo ratings yet
- 4 - Anatomy of PelvisDocument10 pages4 - Anatomy of PelvisJISHNU TKNo ratings yet
- EVAL OF FEMALE PELVIS TRANS Dr. ReylesDocument5 pagesEVAL OF FEMALE PELVIS TRANS Dr. ReylesRea Dominique CabanillaNo ratings yet
- Anatomy - Upper LimbDocument9 pagesAnatomy - Upper LimbjainilNo ratings yet
- Muscular SystemDocument8 pagesMuscular Systemnaofumixeia24No ratings yet
- Rabbit (Oryctolagus Cuniculus) Muscular System: I. Dermal/IntegumentaryDocument9 pagesRabbit (Oryctolagus Cuniculus) Muscular System: I. Dermal/IntegumentaryAnnray Justine T. GlipaNo ratings yet
- (ANAT) P.08 Anatomy of The Eyeball Extra-Ocular Muscles, Eyelid and Lacrimal ApparatusDocument14 pages(ANAT) P.08 Anatomy of The Eyeball Extra-Ocular Muscles, Eyelid and Lacrimal ApparatusArthur NerickNo ratings yet
- I. Facial MusclesDocument5 pagesI. Facial MusclesAnya RamosNo ratings yet
- The Skull and Vicsceral Skeleton PDFDocument13 pagesThe Skull and Vicsceral Skeleton PDFAmberValentineNo ratings yet
- Complab Exercise 2 SharkDocument9 pagesComplab Exercise 2 SharkstephaniealmendralNo ratings yet
- Gross Anatomy of The Forearm: A CAL Package Designed By-Pratik SinhaDocument24 pagesGross Anatomy of The Forearm: A CAL Package Designed By-Pratik Sinhaapi-19916399No ratings yet
- Anatomy of The Musculoskeletal System: AppendagesDocument16 pagesAnatomy of The Musculoskeletal System: AppendagesRyzeNo ratings yet
- 6288787c5b072 Bio2206l Exercise 7a Muscles of The Head Neck and ShouldersDocument6 pages6288787c5b072 Bio2206l Exercise 7a Muscles of The Head Neck and ShouldersKimNo ratings yet
- Cat SkeletonDocument10 pagesCat SkeletonJefferson TanNo ratings yet
- LAB Shoulder Region & Superficial BackDocument11 pagesLAB Shoulder Region & Superficial BacknanaNo ratings yet
- Abdominal Wall, Omentum, Mesentery and RetroperitoneumDocument8 pagesAbdominal Wall, Omentum, Mesentery and RetroperitoneumRae Marie AquinoNo ratings yet
- 2-Pelvic Walls, Joints, Vessels & NervesDocument32 pages2-Pelvic Walls, Joints, Vessels & NervesAbdul Rafay ShaikhNo ratings yet
- Pelvic Walls, Joints, Vessels & Nerves, Pelvic Organs PPT FinalDocument106 pagesPelvic Walls, Joints, Vessels & Nerves, Pelvic Organs PPT Finalntege stuart100% (1)
- TA Lab 3 Bone - Cooperative Learning - Version2Document7 pagesTA Lab 3 Bone - Cooperative Learning - Version2Hajira NusretNo ratings yet
- Cat Muscles - Origin, Insertion, ActionDocument5 pagesCat Muscles - Origin, Insertion, ActionHarvey Domingo93% (29)
- 11.pelvic Walls, Joints, Vessels & NervesDocument36 pages11.pelvic Walls, Joints, Vessels & NervespashaNo ratings yet
- Gross Anatomy of The Appendix, Colon, Rectum, and AnusDocument8 pagesGross Anatomy of The Appendix, Colon, Rectum, and Anusbo gum parkNo ratings yet
- Syllabus Laboratory Anatomy Gastrointestinal System: A SequenceDocument17 pagesSyllabus Laboratory Anatomy Gastrointestinal System: A Sequenceamelia rahayuNo ratings yet
- Pelvic Neurovasculature Practice QuizDocument4 pagesPelvic Neurovasculature Practice QuizMr .Hacker xDNo ratings yet
- Aiims Nov 2010 Review by Tanmay MehtaDocument56 pagesAiims Nov 2010 Review by Tanmay MehtaGIST (Gujarat Institute of Science & Technology)No ratings yet
- Female Pelvic Floor Anatomy: The Pelvic Floor, Supporting Structures, and Pelvic OrgansDocument9 pagesFemale Pelvic Floor Anatomy: The Pelvic Floor, Supporting Structures, and Pelvic OrgansJimmy JimmyNo ratings yet
- Reviewer Extrinsic Muscle of The ForelimbDocument2 pagesReviewer Extrinsic Muscle of The ForelimbJM&MC TV ninjaNo ratings yet
- 0.5x ANATOMY LOWER LIMBSDocument24 pages0.5x ANATOMY LOWER LIMBSArijeet77No ratings yet
- Muscle, Origin, InsertionDocument9 pagesMuscle, Origin, Insertionshananana1616No ratings yet
- Cmca MidtermsDocument6 pagesCmca Midtermsmcriscruzada12No ratings yet
- Joints in The Upper Limb Cheat Sheet: by ViaDocument1 pageJoints in The Upper Limb Cheat Sheet: by ViaBELİS YILMAZNo ratings yet
- Pectoral Region and AxillaDocument25 pagesPectoral Region and AxillaSelva pandi100% (1)
- Asset - 8288 - Anatomy of The Canine Forelimb PDFDocument35 pagesAsset - 8288 - Anatomy of The Canine Forelimb PDFBianca ElenaNo ratings yet
- LAB Gluteal Region & Posterior ThighDocument8 pagesLAB Gluteal Region & Posterior ThighnanaNo ratings yet
- Pelvic Peritoneum and Abdominopelvic StaticsDocument27 pagesPelvic Peritoneum and Abdominopelvic StaticsScribdTranslationsNo ratings yet
- Elbow Forearm Lab 2021Document13 pagesElbow Forearm Lab 2021Matthew GuiseNo ratings yet
- 16 Upper Extremity (FINAL)Document30 pages16 Upper Extremity (FINAL)kath-kath100% (1)
- Labs 1 and 2: Muscular System Cat Dissection: Photo Atlas, Chapter 19 Human Muscles: Unit 7, Muscle Tissue and Muscular SystemDocument10 pagesLabs 1 and 2: Muscular System Cat Dissection: Photo Atlas, Chapter 19 Human Muscles: Unit 7, Muscle Tissue and Muscular SystemFranco AlminoNo ratings yet
- 07 Pelvis, Perineum, ReproductiveDocument35 pages07 Pelvis, Perineum, ReproductiveShaira Aquino VerzosaNo ratings yet
- Anatomy NotesDocument3 pagesAnatomy NotesKaren Kaye Canlas100% (3)
- LAB Antero-Medial Thigh & HipDocument10 pagesLAB Antero-Medial Thigh & HipnanaNo ratings yet
- ANATOMY Trans PELVIS POST ABDOMINAL WALL PERINEUMDocument8 pagesANATOMY Trans PELVIS POST ABDOMINAL WALL PERINEUMSan LapuhapuNo ratings yet
- Williams Study Guide Maternal AnatomyDocument5 pagesWilliams Study Guide Maternal AnatomyCarl Vin Pasion100% (1)
- Baquero Act 6 Anaphy DONEDocument11 pagesBaquero Act 6 Anaphy DONEKent TutorNo ratings yet
- The Girdles Sternum and Paired AppendagesDocument9 pagesThe Girdles Sternum and Paired AppendagesAmberValentineNo ratings yet
- St. Luke's College of Medicine - William H. Quasha Memorial: AnatomyDocument4 pagesSt. Luke's College of Medicine - William H. Quasha Memorial: AnatomyMavic VillanuevaNo ratings yet
- Anatomy - B. Rabischong - GRDocument20 pagesAnatomy - B. Rabischong - GRAnonymous UHnQSkxLBDNo ratings yet
- Oia Rabbit PDFDocument13 pagesOia Rabbit PDFJhoanna Rein DuzonNo ratings yet
- Unit 2 Skeletal Muscles Part 3Document3 pagesUnit 2 Skeletal Muscles Part 3Sharva BhasinNo ratings yet
- Lab SHT Act-1 - Santos - Yzai (DMD 2y2-2)Document9 pagesLab SHT Act-1 - Santos - Yzai (DMD 2y2-2)Miguel Yancy AverillaNo ratings yet
- Female Reproductive SystemDocument4 pagesFemale Reproductive SystemHollan GaliciaNo ratings yet
- Factors Influencing Permanent Teeth Eruption. Part One - General FactorsDocument6 pagesFactors Influencing Permanent Teeth Eruption. Part One - General FactorsestherNo ratings yet
- Excretory System (Excercise)Document17 pagesExcretory System (Excercise)Shadab HanafiNo ratings yet
- Exm 2011-07-25 Final Anatomy Practice MCQ Questions 2Document26 pagesExm 2011-07-25 Final Anatomy Practice MCQ Questions 2Lucas TobingNo ratings yet
- Https://d1c0fc7ib89kee - Cloudfront.net/uploads/attachment/file//reproduction Exam QuestionDocument8 pagesHttps://d1c0fc7ib89kee - Cloudfront.net/uploads/attachment/file//reproduction Exam QuestionAmaya AliNo ratings yet
- Functia Integrativa A Creierului PDFDocument14 pagesFunctia Integrativa A Creierului PDFalinalexandru007No ratings yet
- WEEK 1 - Chapter 16 - Lymphatic System and ImmunityDocument59 pagesWEEK 1 - Chapter 16 - Lymphatic System and ImmunityOliver Namyalo100% (1)
- Comparative Anatomy of Female Reproductive System in Domestic AnimalsDocument34 pagesComparative Anatomy of Female Reproductive System in Domestic Animalsد. حيدر الرماحيNo ratings yet
- Stretching: Mechanisms and Benefits For Sport Performance and Injury PreventionDocument19 pagesStretching: Mechanisms and Benefits For Sport Performance and Injury PreventionGeorge M. PamborisNo ratings yet
- Kelly9e Ch03 Male Sexual-Anatomy and PhysiologyDocument19 pagesKelly9e Ch03 Male Sexual-Anatomy and Physiologysauloalberto6254No ratings yet
- BCH 376 (Urinalysis Lecture Notes)Document7 pagesBCH 376 (Urinalysis Lecture Notes)biddyusmc100% (1)
- TMP F781Document29 pagesTMP F781FrontiersNo ratings yet
- A Clinical Case Report/ Oral Diagnosis On Lichenoid ReactionDocument7 pagesA Clinical Case Report/ Oral Diagnosis On Lichenoid ReactionJu WenNo ratings yet
- Normal Menstrual CycleDocument28 pagesNormal Menstrual CycleCristóbal ConchaNo ratings yet
- Special Senses Part 1 (Taste & Smell)Document18 pagesSpecial Senses Part 1 (Taste & Smell)rizwanbas100% (1)
- MK Hematology-LeukemiasDocument35 pagesMK Hematology-LeukemiasMoses Jr KazevuNo ratings yet
- Principles of Motor DevelopmentDocument15 pagesPrinciples of Motor DevelopmentRina Siason AbaNo ratings yet
- 2 - Puberty-GirlsDocument40 pages2 - Puberty-Girlsapi-241585431No ratings yet
- PsiconeuroinmunologíaDocument10 pagesPsiconeuroinmunologíaLuis Alfredo Rosales GuerreroNo ratings yet
- 5 - Circulation GraysDocument33 pages5 - Circulation GraysdrmanojkulNo ratings yet
- Combining Form SummaryDocument24 pagesCombining Form Summaryapi-57828209No ratings yet
- HORMON REPRODUKSI DAN SIKLUS HAID Prof. Dr. Dr. Nusratuddin Abdullah, SP - OG (K) MARSDocument21 pagesHORMON REPRODUKSI DAN SIKLUS HAID Prof. Dr. Dr. Nusratuddin Abdullah, SP - OG (K) MARStenri olaNo ratings yet
- Excretory System of ChickenDocument3 pagesExcretory System of ChickenAjikNo ratings yet
- Aesthetic Management of Immediate Anterior Tooth Replacement With Ovate Pontic: A Case Report PDFDocument5 pagesAesthetic Management of Immediate Anterior Tooth Replacement With Ovate Pontic: A Case Report PDFAnita PrastiwiNo ratings yet
- Pre-Assessment: Odd Organ OutDocument45 pagesPre-Assessment: Odd Organ OutMelody Miras MacabontocNo ratings yet
- HymenectomyDocument5 pagesHymenectomyShamaine limNo ratings yet
- Blood Transfusion: DR Vishwabharathi TDocument28 pagesBlood Transfusion: DR Vishwabharathi TSuma0% (1)
- LiverDocument35 pagesLiverJustin Harris100% (2)
- Nursing Head-to-Toe Assessment Cheat Sheet - Nurseslabs PDFDocument7 pagesNursing Head-to-Toe Assessment Cheat Sheet - Nurseslabs PDFNyeweh Sia Yomba67% (15)
- AnaPhy - Digestive SystemDocument5 pagesAnaPhy - Digestive SystemJan Mark SotoNo ratings yet
- Love Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)From EverandLove Life: How to Raise Your Standards, Find Your Person, and Live Happily (No Matter What)Rating: 3 out of 5 stars3/5 (1)
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (404)
- By the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsFrom EverandBy the Time You Read This: The Space between Cheslie's Smile and Mental Illness—Her Story in Her Own WordsNo ratings yet
- The Age of Magical Overthinking: Notes on Modern IrrationalityFrom EverandThe Age of Magical Overthinking: Notes on Modern IrrationalityRating: 4 out of 5 stars4/5 (32)
- Summary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisFrom EverandSummary: Outlive: The Science and Art of Longevity by Peter Attia MD, With Bill Gifford: Key Takeaways, Summary & AnalysisRating: 4.5 out of 5 stars4.5/5 (42)
- ADHD is Awesome: A Guide to (Mostly) Thriving with ADHDFrom EverandADHD is Awesome: A Guide to (Mostly) Thriving with ADHDRating: 5 out of 5 stars5/5 (3)
- Think This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeFrom EverandThink This, Not That: 12 Mindshifts to Breakthrough Limiting Beliefs and Become Who You Were Born to BeRating: 2 out of 5 stars2/5 (1)
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 4.5 out of 5 stars4.5/5 (82)
- Cult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryFrom EverandCult, A Love Story: Ten Years Inside a Canadian Cult and the Subsequent Long Road of RecoveryRating: 4 out of 5 stars4/5 (46)
- The Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaFrom EverandThe Body Keeps the Score by Bessel Van der Kolk, M.D. - Book Summary: Brain, Mind, and Body in the Healing of TraumaRating: 4.5 out of 5 stars4.5/5 (266)
- The Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsFrom EverandThe Ritual Effect: From Habit to Ritual, Harness the Surprising Power of Everyday ActionsRating: 4 out of 5 stars4/5 (4)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)
- Manipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesFrom EverandManipulation: The Ultimate Guide To Influence People with Persuasion, Mind Control and NLP With Highly Effective Manipulation TechniquesRating: 4.5 out of 5 stars4.5/5 (1412)
- Raising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsFrom EverandRaising Mentally Strong Kids: How to Combine the Power of Neuroscience with Love and Logic to Grow Confident, Kind, Responsible, and Resilient Children and Young AdultsRating: 5 out of 5 stars5/5 (1)
- Dark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.From EverandDark Psychology & Manipulation: Discover How To Analyze People and Master Human Behaviour Using Emotional Influence Techniques, Body Language Secrets, Covert NLP, Speed Reading, and Hypnosis.Rating: 4.5 out of 5 stars4.5/5 (110)
- Why We Die: The New Science of Aging and the Quest for ImmortalityFrom EverandWhy We Die: The New Science of Aging and the Quest for ImmortalityRating: 4 out of 5 stars4/5 (5)
- Raising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsFrom EverandRaising Good Humans: A Mindful Guide to Breaking the Cycle of Reactive Parenting and Raising Kind, Confident KidsRating: 4.5 out of 5 stars4.5/5 (170)
- Summary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisFrom EverandSummary: Limitless: Upgrade Your Brain, Learn Anything Faster, and Unlock Your Exceptional Life By Jim Kwik: Key Takeaways, Summary and AnalysisRating: 5 out of 5 stars5/5 (8)
- When the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisFrom EverandWhen the Body Says No by Gabor Maté: Key Takeaways, Summary & AnalysisRating: 3.5 out of 5 stars3.5/5 (2)
- Mindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessFrom EverandMindset by Carol S. Dweck - Book Summary: The New Psychology of SuccessRating: 4.5 out of 5 stars4.5/5 (328)
- Troubled: A Memoir of Foster Care, Family, and Social ClassFrom EverandTroubled: A Memoir of Foster Care, Family, and Social ClassRating: 4.5 out of 5 stars4.5/5 (27)
- Dark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingFrom EverandDark Psychology: Learn To Influence Anyone Using Mind Control, Manipulation And Deception With Secret Techniques Of Dark Persuasion, Undetected Mind Control, Mind Games, Hypnotism And BrainwashingRating: 4 out of 5 stars4/5 (1138)
- The Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeFrom EverandThe Courage Habit: How to Accept Your Fears, Release the Past, and Live Your Courageous LifeRating: 4.5 out of 5 stars4.5/5 (254)