Professional Documents
Culture Documents
WJM 6 143
Uploaded by
luluksOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
WJM 6 143
Uploaded by
luluksCopyright:
Available Formats
WJM World Journal of
Methodology
Submit a Manuscript: http://www.wjgnet.com/esps/ World J Methodol 2016 June 26; 6(2): 143-153
Help Desk: http://www.wjgnet.com/esps/helpdesk.aspx ISSN 2222-0682 (online)
DOI: 10.5662/wjm.v6.i2.143 © 2016 Baishideng Publishing Group Inc. All rights reserved.
MINIREVIEWS
Methodology in improving antibiotic implementation
policies
Onur Özgenç
Onur Özgenç, Department of Infectious Diseases and Clinical over the world. They are the only drugs which do not
Microbiology, Dokuz Eylul University Hospital, Karsiyaka, intentionally affect the patient. They affect the patho
35350 Izmir, Turkey gens which invade the host. The emergence and spread
of antibiotic-resistant pathogens are accelerated by
Author contributions: Özgenç O solely contributed to this heavy antibiotic usage. The effective antimicrobial
manuscript. stewardship and infection control program have been
shown to limit the emergence of antimicrobial-resistant
Conflict-of-interest statement: The author declares that there is
bacteria. In this respect, education for antibiotic
no conflict of interest related to the manuscript.
prescribing could be designed by going through the
Open-Access: This article is an open-access article which was steps of scientific methodology. A defined leadership and
selected by an in-house editor and fully peer-reviewed by external a coordinated multidisciplinary approach are necessary
reviewers. It is distributed in accordance with the Creative for optimizing the indication, selection, dosing, route of
Commons Attribution Non Commercial (CC BY-NC 4.0) license, administration, and duration of antimicrobial therapy. In
which permits others to distribute, remix, adapt, build upon this scenarios, knowledge is also as important as experience
work non-commercially, and license their derivative works on for critical decision making as is designated. In this
different terms, provided the original work is properly cited and setting, the prevalence and resistance mechanisms of
the use is non-commercial. See: http://creativecommons.org/ antimicrobials, and their interactions with other drugs
licenses/by-nc/4.0/ need to be observed. In this respect, infectious disease
service should play an important role in improving
Correspondence to: Onur Özgenç, MD, Professor of antimicrobial use by giving advice on the appropriate
Medicine, Department of Infectious Diseases and Clinical
use of antimicrobial agents, and implementing evidence-
Microbiology, Dokuz Eylul University Hospital, Cemal Gursel
based guidelines.
Cad 368, Karsiyaka, 35350 Izmir,
Turkey. ozgenc.onur@gmail.com
Telephone: +90-532-4153169 Key words: Antibiotics; Infection; Antibiotic resistance;
Fax: +90-232-4645050 Therapy; Medical informatic applications
Received: July 25, 2015 © The Author(s) 2016. Published by Baishideng Publishing
Peer-review started: July 27, 2015 Group Inc. All rights reserved.
First decision: September 30, 2015
Revised: February 12, 2016 Core tip: Treatment of infections has become pro
Accepted: March 17, 2016 blematic because of increasing global antimicrobial
Article in press: March 18, 2016 resistance. One of the major reasons of this is antibiotic
Published online: June 26, 2016 misuse and over use. In order to make antibiotic therapy
more effective, some guidelines are used. Although
guidelines lead to improvements in clinical practice,
no guideline can be sufficiently specific that can be
Abstract applied to all clinical situations. For improving antibiotic
implementation strategies, not only consensus-based but
The basic requirements of antibiotic prescribing are com
also evidence-based scientific methods are needed. This
ponents of methodology; knowledge, logical reasoning,
review highlights the knowledge and experimentation
and analysis. Antimicrobial drugs are valuable but of expert physicians under the supervision of antibiotic
limited resources, different from other drugs and they stewardship.
are among the most commonly prescribed drugs all
WJM|www.wjgnet.com 143 June 26, 2016|Volume 6|Issue 2|
Özgenç O. Improving antibiotic implementation policies
Özgenç O. Methodology in improving antibiotic implementation WHY ARE ANTIMICROBIAL AGENTS
policies. World J Methodol 2016; 6(2): 143-153 Available from:
URL: http://www.wjgnet.com/2222-0682/full/v6/i2/143.htm DIFFERENT FROM OTHER DRUGS?
DOI: http://dx.doi.org/10.5662/wjm.v6.i2.143 Antimicrobial drugs are valuable but limited resources,
and they are different from other drugs. Why are anti
[8]
biotics different from other drugs? The three factors
which differ antimicrobials from other drugs, compose
INTRODUCTION the important components of antimicrobial therapy :
[9]
The implementation of antibiotics in cancer chem First, antibiotics are among the most prescribed
otherapy and organ transplant patients, make the drugs all over the world. Antimicrobials account more
[4]
than of 30% of hospital pharmacy budgets . In
serious lethal complications of diseases likely treatable.
developing countries one third of the budget reserved for
Therefore parallel to medical advances, practice of [10]
health care is also spent for antibiotics . Therefore the
medicine have changed greatly through antibiotic usage.
cost effectiveness of antimicrobial treatment of bacterial
The early initiation of antibiotics to treat infections reduce [11]
[1] infections is important . The excessive consumption
morbidity . However, 20%-50% of the prescribed
and prescription of antibiotics ended up with high costs;
antibiotics in hospitals are either unnecessary or
[1-3] so the “the Ministry of Health in Turkey” restricted the
inappropriate . Unnecessary antibiotic using patients
prescription of excessively used expensive antibiotics
are candidates for serious adverse effects even without [10]
nationwide . With this new policy the responsibility of
any effective clinical cure. The misuse of antibiotics
the prescription of antimicrobials is given to the infectious
also contributes to the growing problem of antibiotic
disease (ID) specialist physicians. Nevertheless, the
resistance. In the twenty-first century, because antibiotic
comparative cost of antibiotics is only one of the factors
resistance has become a serious issue for patient safety,
in determining the physicians’ antibiotic choice, and it
improving the use of antibiotics is an important public [11]
[1,4,5] should never be the most important factor .
health problem .
Second, antimicrobials are the only drugs which do
Therefore, antibiotic prescribing should be based on
not intentionally affect the patient; this feature differs
a prudent, well-thought, and rational process. The basic
antibiotics from other drugs. Antibiotics can affect both
requirement for this is knowledge, logical reasoning [8,9]
the pathogen and the colonizing flora . Antimicrobial
and analysis. Meanwhile, the system of rules and pro
therapy is based on the characteristics of a patient
cedures for interventions to improve antibiotic use is
and a drug, as well on the characteristics of the micro
constantly being updated as scientists and physicians [8]
organisms . This complex relationship between the
look for new and better ways of making observations, patient, antimicrobial, and microorganism is defined as
[6]
analysis and synthesis . For implementation strategies [8]
the cornerstones of a triangle , as shown in Figure 1.
we may need evidence-based methodology. Thus, the In this concept host presents the antimicrobial agent to
below stated steps of a scientific method can be app the pathogen
[9,12]
.
[7]
lied for improving antibiotic implementation policies : The selection of an antibiotic for the appropriate
(1) Asking a question; (2) Carrying out background empirical antimicrobial therapy has become increasingly
research; (3) Constructing a hypothesis; (4) Testing the difficult. Physician has to know many different aspects
hypothesis through an experiment; (5) Analyzing data of IDs; such as immunological and genetic host factors,
and drawing a conclusion; and (6) Communicating the microbial virulence, pharmacokinetics (PKs) and phar
results. [8]
macodynamics (PDs) of drugs . PKs describes the
action of drugs in tissues and body fluids over a period of
time, including the processes of absorption, distribution,
A PRAGMATIC APPROACH TO THE [13]
and excretion . PDs studies the relationship between
METHODOLOGY OF ANTIBIOTIC the biochemical and physiological interactions of drugs
on the body or on microorganisms. Physiological effects
IMPLEMENTATION POLICIES
are associated with primary and underlying disorders,
In 2015 Center’s for Disease Control and Prevention aging, interactions with other drugs, etc. Meanwhile, the
(CDC) published a report about core elements of hospital time course and the concentration of the therapeutic
[1]
antibiotic stewardship programs . According to CDC agent at the infection site, and its adverse effects have to
“there is no single template to optimize antibiotic usage”. [13]
be concerned . PDs, with PKs, explains the relationship
The medical decision is complex and the antibiotic between the dose and response. The postantibiotic
implementation policies should be flexible. Therefore, and bactericidal action of antimicrobials related to
there is need for defined leadership and coordinated drug’s PD effects, have to be known for optimal dose
[1]
multidisciplinary approach . Although the relevant gui regimens. In addition, the optimal dose and dosing
delines for antibiotic usage and expert opinions steer intervals have also to be determined according to the
and shape the author’s vision for judicious antibiotic minimal inhibitory concentrations (MICs) and minimal
use in writing this review, the methodology used in this bactericidal concentrations of the antimicrobials against
[13]
manuscript highlights the author’s own ideas. microorganism groups .
WJM|www.wjgnet.com 144 June 26, 2016|Volume 6|Issue 2|
Özgenç O. Improving antibiotic implementation policies
Host It is known that changing the attitude of the pro
fessional who is prescribing an antibiotic, is not easy.
So, to aide the physicians attitude for antibiotic usage,
early antimicrobial stewardship interventions have
[3,16]
been practiced at the postgraduate level . The IDs
Society of America (IDSA) has defined the antimicrobial
Pathogen Antimicrobial stewardship. With this, IDSA stated that for maximum
clinical cure, the indication, selection, dosing, route of
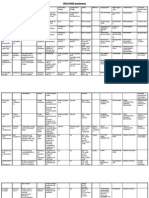
Figure 1 The relationship between the patient, antimicrobial and administration and duration of antimicrobial therapy
microorganism. have to be optimized. In addition while selecting anti
microbials, it should be taken into account that they
Some drugs, such as the β -lactams, exert their will produce no damage; including toxicity, selection of
maximal effect when antibiotic load exceed the MIC of pathogenic organisms, such as Clostridium difficile, and
[4,5,8,16]
the microorganism for a certain period of time between emergence of resistance . To avoide resistance
doses. Such agents are known as “time-dependent” selecting pressure, the antibiotics have to be given for
antibiotics and they are also recognized with the the shortest possible duration, in adequate doses, and
[8]
PD indices as “time above MIC”
[4,14]
. For time-depen with the least broad-spectrum .
dent antibiotics during the dosing interval, the serum The systematic ways of doing, teaching, and stu
drug concentrations should achieve at least 40% to dying antibiotic implementation strategies constitute
50% of the MIC of the causative pathogen . These
[13] the main issue of this manuscript. In other words the
studies support the concept of administering β-lactam question of what could be the system of methods and
antibiotics at shorter intervals, prolonging the infusion principles used in improving antibiotic implementation
time, or even administering by continuous infusion for practices, should be answered. James Bach states
serious systemic infections
[4,14]
. Beta-lactam antibiotics that “there is no consensus about what practices are
show an inoculum effect. When the bacterial density the best, unless consensus means; people I respect
is low, the concentration of the required β -lactam also say they like it. There are practices that are more
[13]
could be low, and vice versa . The aminoglycosides likely to be considered good and useful than others,
and fluoroquinolones, on the other hand, exhibit within a certain community”. But… so what? “Good
“concentration-dependent” killing. For these and similar practice is not a matter of popularity. It’s a matter of
agents, the PD indices are determined as “peak/MIC” skill and context” (James Bach; founder and operator of
(peak serum concentrations divided by the MIC) and exploratory software company Satisfice, Inc.).
as “24-h area under curve/MIC”. These ratios show
that giving the fluoroquinolones and aminoglycosides INFECTIONS AND ANTI-INFECTIVE
by once daily dose are encouraging from a PD point of
view
[4,14]
. Thus the high peak levels obtained after short THERAPY
infusion dosing or high exposures during 24 h, cause The IDSA and the Society for Healthcare Epidemiology
[4,14]
the most rapid killing of the infecting pathogen . In of America (SHEA) published Guidelines for Antimicrobial
most clinical settings, administering aminoglycosides [4]
Stewardship Programs in 2007 . These guidelines
as a total single daily dose are recommended and have do not pose as a substitute for clinical judgement
[4,16]
.
become the standard of application. On the other hand, In selecting the appropriate antimicrobial agent for
the glycopeptides exhibit time-dependent killing. They therapy of an infection, some important factors should
also show slow bactericidal activity and a short post- [14]
be kept in mind . First, the identification and the
[13]
antibiotic effect in vitro . Studies of PK and PD account source of infecting organism must be known or, at the
[4]
for the basis of dose optimization . very least, it must be possible to arrive at a statistically
Third, the overuse of antibiotics in human health care reasonable guess as to its identity on the basis of
[14]
and animal feeds, the increased use of invasive devices clinical information . Also, the environment where the
and procedures, and invalid infection control practices infecting organism is contracted (community or hospital)
have resulted in antibiotic resistance. The resistance should be questioned. Second, information about
is acquired by mutational change or by transfer and the susceptibility of the infecting organism, or likely
[14]
acquisition of resistance-encoding genetic material in susceptibility, must be as accurate as possible . Finally,
[15]
health care settings . So, multidrug resistant bacteria is a series of factors specific to the patient who is being
the major cause of failure of the treatment of IDs which treated must be considered to arrive at the optimal
[15] [14]
the clinician has to deal with . The overuse of other choice of antimicrobial agent .
drugs does not introduce any negative effect to other Today most antibiotic treatment is empirical. In 2012
[17]
medications as antimicrobials do. Therefore, to limit the as stated by Livermore , “in general most diagnostic
transmission of emerging multidrug-resistant organisms, microbiology laboratory practice moves at the speed it
implementation of regional antibiotic usage data has to did in Fleming’s time: 1 d from specimen to culture and
[5]
be developed . another from culture to identification and susceptibility
WJM|www.wjgnet.com 145 June 26, 2016|Volume 6|Issue 2|
Özgenç O. Improving antibiotic implementation policies
data”. In practice, for critically ill patient empirical
ANTIMICROBIAL STEWARDSHIP
therapy is started as early as possible when evidence
[18]
of infection is observed . The antibiotic guidelines PROGRAM
combined with the physician’s experience shape the Antibiotic implementation policies should be flexible .
[1]
[18]
therapeutic choices for empirical antimicrobial usage . Meanwhile, the success depends on a defined leadership
Meanwhile, several methods for the rapid identifica and a coordinated multidisciplinary approach . For
[1]
tion of pathogenic bacteria are available in clinical optimum decision making in prescribing antibiotics,
specimens. A Gram stain-preparation is perhaps the physicians have to have sufficient knowledge of IDs,
simplest and least expensive method to determine the infecting pathogens, and antimicrobials. So the dire
presence of bacterial and some fungal pathogens. Final ctor of the program should be ID specialist, or ID
and definitive identification of pathogenic organisms specialist should co-direct the program with a clinical
still often require a culture technique. It is extremely
pharmacist. Thus, the key members of an antimicrobial
important that appropriate specimens be obtained [4,5]
stewardship team is constituted . For antimicrobial
for culture before beginning antimicrobial therapy, to
resistance surveillance a clinical microbiologist, and for
test the susceptibility of agents that may be used in
[14] the computer support an information system specialist
therapy . Once anti-infective therapy starts, cultures [4,5]
are also needed . The IDs physician or a clinical
often become sterile, even though viable organisms
pharmacist with IDs training has to have interactions
remain in the host. So samples taken before starting
with the prescriber physicians. They should perform a
antimicrobic therapy is important for the identification
prospective audit and a feedback system, serving to
and antimicrobial susceptibility of the organisms causing [4,5]
[14] reduce the inappropriate use of antimicrobials .
an infection . If fast usage of molecular microbiology
What could be done for to avoid antimicrobial
techniques to identify pathogens and fast detection of
resistance? Many investigators in nowadays try to figure
their resistances in primary clinical specimens could be
out inappropriate antibiotic use and they use this figure
achieved, the individual patient may benefit from early [4,5]
[17] as a surrogate marker . For effective antimicrobial
use of the most powerful antimicrobial .
stewardship many interventions are recommended
For optimal therapy, a number of host factors that
such as; formulary restriction and preauthorization,
may influence the efficacy and toxicity of antimicrobial [4,5]
antimicrobial order forms, antimicrobial cycling .
agents should be considered. The age of the patient,
However, the formulary restriction should be dynamic.
the presence of genetic and metabolic abnormali
The recommendation rules of the routine uses of these
ties, pregnancy, renal and hepatic function all have
basic implementation procedures are not based on
significant effect on the toxicity of a given antimicrobial
[14,19,20] sufficient data. Therefore, to increase the acceptance
agent . Another consideration in selection of an
of stewardship strategies, continuous education pro
appropriate antimicrobial is the site of infection. The [4,5,8]
grams have to be considered . In addition, local
concentration of the antibiotic at the site of infection
microbiology laboratories’ antibiotic sensitivity results
should be ≥ the MIC of the infecting organism for the
antimicrobial therapy to be effective
[14,19,20]
. and resistance patterns, and infection control programs
For judgement of the effectiveness of therapy, should be taken into account to improve antimicrobial
[4,5]
clinical improvement is the best directory; although it utilization .
[21]
is not always easy to observe objectively . As stated
[21]
by Paterson et al , “culture results are sometimes Interaction between inappropriate antibiotic use and
negative, yet an infection is clinically present, or antimicrobial resistance
culture results are positive, but indicate the presence Although, antibiotic resistance is caused by mutations
of colonization rather than true infection”. In such in bacteria’s genes, inappropriate use of antibiotics
situations, switching an antimicrobial agent has to be accelerates the emergence of antibiotic-resistant
[15]
questioned in detail; “Don’t change a winning team” .
[21] bacteria . However, antibiotics kill susceptible bacteria
Besides, for serious infections such as endocarditis but resistant bacteria can overgo to grow and multiply.
long-trerm therapy is needed, so for monitoring clinical The people who have not taken antibiotics are also
improvement physician has to observe the patient for a under risk of getting infected with antibiotic resistant
longer period of time. Another point is that fever should bacteria strains. In this respect, there seems to be
not always be the only factor to judge the success of a complex relationship between antibiotic use and
[15,22]
antimicrobial therapy. Altough a febrile patient under antimicrobial resistance . The relationship is affected
antimicrobial therapy could be related to treatment by antimicrobial PDs, mutant selection windows (MSWs),
[15,22]
failure, there are also other factors which have to be the mutational or acquired resistance .
considered; such as, drug fever, abscess formation, or The MSW is a novel in vitro concept. It is defined
[14]
other infection with an opportunistic pathogen . Some as “the zone between MIC and mutant prevention
[23]
surgical interventions in such occasions, like abscess concentration” . In other words, it means “the ability
[23]
formation drainage, could be as important as anti- of antibiotics to prevent the emergence of mutant” .
infective therapy and should be considered by the ID Becauce antibiotic susceptibilities of different bacteria
[19]
specialist and by the surgean . strains may differ, they might have different selective
WJM|www.wjgnet.com 146 June 26, 2016|Volume 6|Issue 2|
Özgenç O. Improving antibiotic implementation policies
, [8]
windows, depending on the MIC of a given antibiotic. being shaped” as stated by Pulcini et al .
When resistance to antibiotics has reached high levels, For improving antibiotic usage educational programs
[24] [1]
it is difficult to prevent new mutants . should be based on the needs of the hospitals . The
Another interaction between antibiotic usage and effective element in one hospital may not be effective
[25] [8]
antimicrobial resistance can be MIC creep . To explain in another . To optimize antibiotic selection and
this phenomenon for at least last 20 years, vancomycin duration, there are written national guidelines. These
has been used as the cornerstone for the treatment of guidelines cover systemic infections such as respiratory
[25]
methicillin-resistant Staphylococcus aureus (MRSA) . tract, urinary tract, intra-abdominal, skin and soft
In healthcare settings, very small percent of S. aureus tissue infections, and as well, documentations for
[1]
isolates (< 1%) select resistance to vancomycin. There surgical prophylaxis . The Cleveland Clinic published
are also very rare vancomycin-resistant S. aureus and a guideline booklet (2012-2013) for antimicrobial
[26]
vancomycin intermediate-resistant S. aureus strains. usage . The information given in the introduction
“Vancomycin MIC creep” is the rising of vancomycin section of that booklet was striking; in that the authors
MICs among vancomycin susceptible S. aureus (van underlined that the materials were subject to change
comycin MIC ≥ 2 μg/mL). Vancomycin MIC creep and appropriate medical judgements were necessary
[5,26]
is seen in patients with recent vancomycin use. This relative to individual patient’s needs . Meanwhile
situation causes difficulty in the treatment of complicated to improve antibiotic usage, Fishman in CDC’s safe
staphylococcal infections like bacteremia, pneumonia, Healthcare Blog proposed some simple steps that
[25] [16]
etc . Various poor clinical outcomes and increased could be overviewed for antimicrobial therapy :
costs of hospitalization have shown to be associated (1) “Never treat viral syndromes such as acute bron
with infections caused by S. aureus isolates with higher chitis with antibiotics, even when patients demand
[25]
vancomycin MICs . therapy; (2) Use fluoroquinolones cautiously. Not only
Although, for successful empirical therapy broad- fluoroquinolone resistance is rising at an alarming rate,
spectrum coverage is necessary, excessive aggressive but this group of drugs causes resistance to many other
therapy may cause the emergence of antibiotic antibiotics and is associated with the new more virulent
[21]
resistance . After getting antibiotic sensitivity results, strain of C. difficile; (3) Antibiotics used for surgical
the sectrum of therapy should be narrowed. The value prophylaxis should rarely be given for more than 24 h;
of such streamlining and de-escalation therapy, have to post-operative doses are not required in many cases;
[21]
be evaluated fully by the IDs physicians . (4) Refine your antibiotic choice once culture data is
available and always use the drug with the narrowest
Formats of educational curricula spectrum; and (5) Double coverage is rarely necessary
For antibiotic prescribing behavior of hospital programs, once antimicrobial susceptibilities are known”.
[8]
education is an essential element . According to Pulcini Empirical therapy is being started at the first visit
[8]
et al “targeted antibiotic sessions in the format of of the patient. Soon after the hospitalization of the
problem-based learning are absolutely necessary. It patient some additional laboratory data are also avail
is important to identify the topics or concepts that able. Bacterial culture and susceptibility test results
benefit from a disease- (e.g., acute bronchitis) or are achieved in 48 h. So, all clinicians should review
problem- (e.g., antimicrobial resistance) oriented, their initial antibiotic choises after sufficient laboratory
[1]
rather than a pathogen- (e.g., MRSA) oriented, or a data are in hand . According to CDC (2015) for the
drug- (e.g., antibiotic classes) oriented approach”. In management of antimicrobial therapy, below key
[1]
the United Kingdom, for the same purpose a website questions have to be answered : (1) “Does this patient
is performed as “the Prudent Antibiotic User” (PAUSE, have an infection that will respond to antibiotics? (2) If
www.pause-online.org.uk). It is aimed to be used in the so, is the patient on the right antibiotic(s), dose, and
undergraduate medical curriculum. PAUSE has provided route of administration? (3) How long should the patient
standardized teaching aides for all educators of antibiotic receive the antibiotic(s)? and (4) Can a more targeted
[8]
prescribing that have based on cases . Meanwhile, “the antibiotic be used to treat the infection (de-escalate)”?
European Society of Clinical Microbiology and IDs study At the beginning of therapy, broad-spectrum anti
group for Antibiotic Policies” (available at www.escmid. biotics which are effective to the most likely pathogens
org/esgap) has performed postgraduate education are started. The de-escalation means; knowing and
courses; “Antimicrobial Stewardship: Measuring, au collecting bacterial culture results of the organisms
diting and improving”, held bi-annually before “the for later microbiological judgement while targeting
European Conference on Clinical Microbiology and IDs”, streamlining to a more narrow-spectrum antimicrobial
[8]
internationally . It is pointed out that antimicrobial regimen 2-3 d later. This intervention is performed by
stewardship programs have mainly been implemented the means of clinical status and culture results of the
[27]
at the postgraduate level. Instead, it seems antimicrobial patient . Thus, by definite or pre-emptive approaches
stewardship is likely to be more successful if started to the pathogen, a decrease in antimicrobial resistance
earlier with undergraduate programs, “at the time when pressure and antibiotic costs could be achieved by de-
[27]
knowledge, attitude, and behavior of professionals are escalation strategies .
WJM|www.wjgnet.com 147 June 26, 2016|Volume 6|Issue 2|
Özgenç O. Improving antibiotic implementation policies
Guidelines for antimicrobial usage
[34]
shunt infections is accepted as the best choice .
The guidelines for antimicrobial usage aim to encourage Besides, some medications penetrate tissues better
prudent prescribing of antimicrobials for empirical treat than others. For example, if the primary focus of
ment of infections, and thereby improve the results Pseudomonas meningitis treated with meropenem is
of treatment, reduce drug related toxicities, and limit mastoiditis, it is advised to combine meropenem with
[28,29]
the emergence of resistant strains . They contain an aminoglycoside antibiotic which penetrates to the
advice on the appropriate initial management of com skeletal system better.
mon conditions and include route of administration,
dose, and duration of treatment. Where a dose range Microbiology laboratory: For the identification of
is recommended, the patient’s status should be microorganisms and for the determination of bacterial
considered to define the need for using higher doses susceptibilities, the clinical microbiology laboratory
in more severe infections and considering lower doses plays an important role. For qualitative susceptibility
for certain patients’ groups such as the elderly, those testing principles, national and international guidelines
with a low body mass index, and those with liver and are used. Using disk-diffusion (Kirby-Bauer) techniques
[28,29]
kidney failures . Recommendations for antibiotics in by measuring zone diameters, or by calculating MICs,
medical prophylaxis are also given. Surgical prophylaxis ESBLs can be detected. For inducible clindamycin
[28,29]
documents are available separately . resistance of S. aureus D test is also performed with
[4]
disk-diffusion method . The detection of such para
Essentials of antimicrobial use guidelines meters regarding resistance leads to the selection of
Dose optimization: Optimal dosing of antimicrobials appropriate antimicrobials.
depends on patient’s age, renal function, weight, etc.,
and causative organism. Site of infections (endocarditis, Duration of therapy: To control the bacterial infection
meningitis, osteomyelitis, etc.), and PK and PD and prevent relapse, the duration of antibiotic therapy
parameters are also have to be taken in account. is to be sufficient. When optimizing therapy for an
Continuous infusion of β-lactams, once-daily dosing infection, one should consider the person’s immune
of aminoglycosides, and increased dosing of fluo status, the infecting agent and the focus of infection.
roquinolones for Streptococcus pneumoniae and for In most clinical scenarios, because the recommended
Pseudomonas aeruginosa in nosocomial pneumonia are duration of therapy depanding on the clinical situation
[35]
good examples depending on PK and PD parameters
[4,30]
. is flexible, it is usually based on expert opinions .
To base the clinical decision on laboratory data, some
Parenteral to oral conversion: To reduce the length biomarkers such as C-reactive protein or procalcitonin
[35]
of hospitalization and to lower the costs of antibiotics, (PCT) have been increasingly studied . Today, PCT is
switching from intravenous (IV) to oral (PO) therapy is the only biomarker which has been generally accepted
recommended when patients become stable. Generally to help the decision-making in discontinuing antibiotic
Ⅳ forms of antimicrobials are more bioavailable and therapy in sepsis and pneumonia of adults. In clinical
st nd
have greater effects, meanwhile some oral forms of practice the advised use of PCT levels are the 1 day, 2
rd
antibiotics provide high serum levels as comparable or 3 days, and every 48 h of antibiotic commencement
[36]
as parenteral forms
[31,32]
. Some antibiotics don’t have until antibiotic discontinuation . Meanwhile, the use of
an oral form, in such situations an oral antibiotic from procalcitonin levels has not been excessively studied in
a different class with similar spectrum of activity is all infection types. Besides, the high cost in determining
[35]
[33]
adviced . procalcitonin level can limit its use .
Longer antibiotic therapy encourages the develop
Combination therapy: Combination therapy is unne ment or acquisition of antibiotic-resistant organisms.
cessary when the pathogen and the susceptibility are Ventilator-associated pneumonia has traditionally
known. Combination therapy is recommended for the been treated for a long course (14-21-d). However,
prevention of resistance. When an organism load is prolonged antibiotic therapy has caused the emergence
heavy and when there is a high probability of mutational of multidrug-resistant strains. It is also associated with
resistance during therapy, combination of antimicro high toxicity and high costs. In patient groups who are
bials are to be considered. Good examples which are receiving antibiotics for shorter periods of time (8 d)
supporting the combined anti-infective therapy are antibiotic resistance is less common. The studies support
[4]
tuberculosis or HIV infection . Other indication of that if the choise for initial antibiotic therapy is prudent,
combined antibiotic therapy is enterococcal endocarditis. 8-d duration of therapy for ventilator-associated
Combination drug therapy in some situations may pneumonia may be appropriate, and the clinical course
[37]
prevent or delay the emergence of resistance during seems to be favorable after stopping antibiotics .
[14]
exposures within the MSW .
Rifampin has good CSF penetration but selects Emerging developments in antibiotic stewardship
resistant mutants when used alone, so its combined use In antibiotic stewardship programs the commonly used
with other antimicrobials is recommended. Rifampin diagnostic test is PCT. There are also novel tests which
with vancomycin combination in staphylococcal CSF are not used frequently, such as fluorescence in situ
WJM|www.wjgnet.com 148 June 26, 2016|Volume 6|Issue 2|
Özgenç O. Improving antibiotic implementation policies
hybridization and matrix-assisted laser desorption/ announced within 48 h, so that the clinician can change
[1] [38]
ionization time of flight mass spectrometric analysis . the antibiotic with the susceptible one . According
[38]
Recently, measuring antibiotic use as either days to Leibovici et al , “the thought that a healthy and
of therapy, or defined daily dose (DDD) is becoming active 83-year-old man will need hemodialysis because
favorable. With the use of DDD hospitals may have of a drug that you have prescribed is frightening; so
the opportunity to compare their antimicrobial consum the physician decide to order a second generation
[1,4]
ptions with that of other similar hospitals . cephalosporin. Still, the clinician are not altogether
satisfied with the fact that he has reduced the antibiotic
coverage by 7%-15% because of his concern about the
DECISION MAKING IN CLINICAL high costs and fear of side effects associated with other
PRACTICE [38]
antibiotics . He wishes that the balance of benefits and
detriments of antibiotic drugs could have been weighed
Study (clinical practice)[2]
at leisure somewhere else and that you had evidence
The Center of Disease Control (CDC) evaluated hospi [38]
based guidelines to help him make a choice” .
talized patients with the aim of improving inpatient
Two days after admission, the E. coli isolate iden
antibiotic prescribing. They used a national administrative
tified from urine sample of the patient is informed as
database, “MarketScan Hospital Drug Database”, and
[2] susceptible to second generation cephalosporins and
CDC’s “Emerging Infections Program” for the study .
the patient is doing well as expected with the result. “But
First, judicious antibiotic usage was described. Second,
still the physician wonders whether prescribing a drug
the principles of improving antibiotic prescribing data
that affords less than the maximum coverage is the
were illustrated in selected clinical cases. Third, when [38]
right thing to do”, as Leibovici et al emphasize. The
antibiotic usage had been improved, the decrease in
Clostridium difficile infections were estimated. The authors also highlight that, “this may well slow down
results of the study had been reported to the “National the development of resistance and give future patients
Healthcare Safety Network” with the findings of using (to whom you have a duty too) a better chance for
[2]
selected antibiotics in variable lengths of time . an uneventful recovery but your main duty is to your
[38]
present patient . How do you balance the two duties?
The important decision in antibiotic treatment turns out
Scenario (decision making-1)[38] [38]
to be a choice between present and future patients” .
An 83-year-old man with fever (38.7 ℃), dysuria, and
As antibiotic resistance increases, chosing prudent
chills is admitted to the ward. The patient’s medical
antibiotics for the empirical treatment of serious
history and clinical examination findings are recorded. [39]
infections become even more difficult . As stated by
On the basis of symptoms and signs of the patient, [39]
the urine examination is found to be necessary. After Retamar et al “in such situations, physicians face a
observing urine microscopy, the physician has to decide dilemma: To provide a very-broad-spectrum empirical
starting IV antibiotic treatment with the diagnosis of coverage, accepting that on many occasions it will be
severe urinary tract infection .
[38] excessive and might contribute to further resistance
The most common pathogens of urinary tract infe selection, or to use a narrower-spectrum empirical
ction are reviewed as Escherichia coli (E. coli) (60%), regimen, accepting that it may not cover the causative
Proteus mirabilis (10%), and Klebsiella pneumoniae pathogen and might require correction once the
(10%) in people of that age. It is known that the susceptibility results are known”.
microbiology laboratory of the hospital reports the
susceptibility of common pathogens yearly. From those Scenario (decision making-2)
datas the physician can estimate that the sensitivity of A 52-year-old male was admitted to the emergency
the mostly used antibiotics will be as follows: Imipenem room at the fifth day of right inguinal hernia operation.
100% third generation cephalosporins 95%, gentamicin He had 39.2 ℃ fever, erythematous rash on the
92%, second generation cephalosporins 75%, and right lower extremity and systemic signs of toxicity
[38]
ampicillin 40% . The clinician wants to choose the (tachycardia and hypotension). The surgeon learned
antibiotic which is supposed to be matching with the that the patient became erythematous at the site of
in vitro susceptibility of the pathogen, to give the the surgical wound the third day. He examined the
patient the best chance of recovery. However, you have patient; opened the incision and observed the wound as
been told by the head of the administration that third deceptively benign in appearance and obtained culture
generation cephalosporins and imipenem are expensive, specimen from the wound. The ID specialist diagnosed
and they should rather not be the first choice if patient’s the patient as septic shock and moved the patient to
[38]
clinical status is affordable . With gentamicin treatment the intensive care unit (Özgenç O; unpublished data).
nephrotoxicity and ototoxicity develop in the ratio of In patients with clean extra-abdominal operations,
10%. In addition, there can be more severe side effects, surgical site infections (SSIs) are generally seen in
and because of the patient’s advanced age, the risk the ratio of 2%-5%. This ratio can reach up to 20% in
[28]
of nephrotoxicity can be high. On the other hand, the abdominal surgery . Surgical complications associated
in vitro susceptibility pattern of the pathogen will be with infection at the site of incision generally are not
WJM|www.wjgnet.com 149 June 26, 2016|Volume 6|Issue 2|
Özgenç O. Improving antibiotic implementation policies
visible till two weeks. Some small portion can be With Gram-negative pathogens the resistance
[17]
apparent in five days after the operation. Late infections rate is twice that of Gram-positive bacteria . The
are less probable but 30 d period of following-up of spread of extended spectrum β-lactamases (ESBLs)
[40]
infectious complications are recommended . in Enterobacteriaceae have resulted cephalosporin
[43]
In this situation, how could the surgeon evaluate resistance to go up . In severe infections with ESBL-
the patient? (1) Not all postoperative fevers are related positive bacteria cephalosporins have not shown good
to SSIs and there could also be non-infectious erythe clinical outcomes. Moreover, in the last decade there
matous signs around the surgical incision; (2) Soft- have rosen a problem with the striking emerging of
tissue infection within the 48-72 h after an operation is CTX-M ESBLs. Although TEM and SHV ESBLs have
not common and an infection can rarely cause fever; associated with Klebsiella spp., CTX-M types confine to
and (3) In this respect, could the surgeon exclude the E. coli. The CTX-M ESBLs have both spread amongst
possibility of SSI for this case? The answer is no. After hospital and community patients. They are mostly
two days the microbiology laboratory reported that isolated from elderly patients and from patients who
[17]
S. aureus has grown from the culture of the above have hospital contacts .
mentioned patient’s wound specimen. The most CTX-M positive E. coli is resistant not
Early post-SSIs are due to Streptococcus pyogenes only to cephalosporins, but also to quinolones and
[40]
or Clostridium species . When high fever is measured trimethoprim-sulfamethoxazole which are commonly
or systemic signs of infection are observed in few used antimicrobials for the treatment of urinary tract
[44]
days after surgery, direct examination of the wound infections . Instead, susceptibility rates indicate that
[40]
is necessary . Toxic shock syndrome is another rare fosfomycin and nitrofurantoin can be considered as
[40]
cause of early SSI due to staphylococci . In such important oral treatment options for the treatment of
[44]
cases the wound misleads to benign appearance, uncomplicated urinary tract infections . By the way,
although there is serious infection beneath the incision there is concern about the rise of rapid and disturbing
site. Erythroderma may be seen early in the course spread of ESBLs, Amp C enzymes, and quinolone
of the infection. Fever, hypotension, hepatic and renal resistance against Enterobacteriaceae. Carbapenem
impairment, and sometimes diarrhea may also be the resistance, caused by Klebsiella pneumoniae carbapene
early findings. Before beginning antistaphylococcal mases, metallo-β-lactamases, and OXA-48 is decreasing
[17,42]
therapy, the incision should be opened and specimen reliance on carbapenems . Last, the gonococcus
[40]
for culture should be obtained . is also developing resistance to most antibiotics (fluo
This presented scenario highlights that knowledge roquinolones and cefixime) wich can easly be used
[17]
is as important as experience. The physician has to orally .
know all the clinical aspects of surgical manipulations In the last decades third-generation cephalosporins
which may lead to early or late SSIs, or to some other and fluoroquinolones were used alone for urinary
complications. “The devil is hidden in the individual infections in many hospitals. This phenomenon has
[41]
details” as stated by Fishman . These hidden details also resulted in selection of resistant mutants such as
[17]
could be lightened by the experienced and well- C. difficile . Thus, the use of β-lactamase inhibitor
informed ID specialists. combinations has been increased; principally piperacillin/
[17]
tazobactam and amoxicillin/clavulanic acid 3-4 fold .
Piperacillin/tazobactam shows less selective pressure
OVERWHELMING ANTIBIOTIC than cephalosporins for C. difficile, and also produces
RESISTANCE - KNOWLEDGE AND less selective pressure for vancomycin-resistant
enterococci, and for some ESBL-producers, than cephalo
EXPERIMENTATION sporins do .
[17]
“The Antibiotic Resistance Monitoring and Reference On the other hand, another important antimicro
Laboratory” have shown that during the last decades, bial resistance mechanism is the expression of
[45]
resistance to antibiotics have shifted from Gram- chromosomally encoded multidrug efflux pumps .
positive to Gram-negative bacteria. With the develop During fluoroquinolone monotherapy of P. aeruginosa
ment of new antimicrobials and with strict infection infections, these efflux producing mutants can be
control policies, resistance to MRSA has fell down. selected and especially if the given drug dosages are
New antibiotics; daptomycin, linezolid, and tigecycline, not adequate, fluoroquinolones can select multidrug-
[42]
active against MRSA have been discovered . After resistant organisms. Therefore, in the treatment of
the development of conjugate vaccine, the resistance serious infections among hospital patients, the usage of
[46]
problem to pneumococci has seemed to be declined. fluoroqinolones can be limited .
The problem with enterococci is greater. In serious For the treatment of serious infections by ESBL-
manifestations with enterococci such as in endocarditis, producer microorganisms, carbapenems remain as
[42]
high-level aminoglycoside resistance is great concern almost only active drug choise . Because of the fact
since bactericidal activity is needed. In this situation, the that cephalosporin resistance in Enterobacteriaceae has
[43]
clinician refers to daptomycin’s bactericidal effect with its risen, carbapenem use has increased . This increased
[42]
high activity . use of carbapenems has resulted in carbapenemase
WJM|www.wjgnet.com 150 June 26, 2016|Volume 6|Issue 2|
Özgenç O. Improving antibiotic implementation policies
enzymes selection which are much more commoner duration. These antibiotic implementation principles
in non-fermenters than in the Enterobacteriaceae. The early in the ID course, play the key role in initial app
[19,51]
carbapenemases are mostly produced by Acinetobacter ropriate antibiotic prescribing . By the way, initial
baumannii and Pseudomonas aeruginosa, due to OXA appropriate antibiotic treatment has been shown to
carbapenemases and to chrosomal mutations in the reduce mortality, length of stay in intensive care unit
[42]
non-fermenters, respectively . Meanwhile, against and hospital. Early correct antibiotic choses have also
[19,51]
carbapenemase-producers, colistin, tigecycline, and served to the reduction in antimicrobial costs .
fosfomycin are the treatment options with some In this respect, it is underlined that ID service being
[17]
adverse effects such as toxicity and resistance . an expert in the field, plays an important role in
To delay antibiotic resistance, heterogenous use of improving antimicrobial usage, by giving advice on the
different antimicrobial classes within a period, can be judicious use of antimicrobial agents and by developing
preferred. Prescribing antibiotics from different groups evidence-based guidelines under the light of antibiotic
[50,52]
in equal proportions are shown to be effective for implementation policies . The ID specialist in his
preventing the dissemination of multi-drug resistant tough way can adopt antibiotic resistance as a “chronic
[47,48] [53]
pathogens . disease”, instead of trying to overwhelm it .
Antibiotic resistance has become a major public
[42]
health priority . In this respect, Australian Govern
ment has announced “the first National Antimicrobial
REFERENCES
Resistance Strategy for the years of 2015-2019”, for 1 Center’s for Disease Control and Prevention (CDC). Core
[49] elements of hospital antibiotic stewardship programs. 2015.
“antibiotic misuse and resistance” (AMR) . Because
Available from: URL: http://www.cdc.gov/getsmart/healthcare/
the prevalence of AMR is increasing all over the world, implementation/core-elements.html
there is a great concern that we will be out of treatable 2 Fridkin S, Baggs J, Fagan R, Magill S, Pollack LA, Malpiedi P,
antibiotics. The World Health Organization and other Slayton R, Khader K, Rubin MA, Jones M, Samore MH, Dumyati
authorities are aware of the fact that pharmaceutical G, Dodds-Ashley E, Meek J, Yousey-Hindes K, Jernigan J, Shehab
N, Herrera R, McDonald CL, Schneider A, Srinivasan A. Vital signs:
industry is far beyond the increasing resistance pace of improving antibiotic use among hospitalized patients. MMWR Morb
microorganisms for to develop new anti-infective drugs Mortal Wkly Rep 2014; 63: 194-200 [PMID: 24598596]
[49]
against them . So, the physicians should achieve 3 Fishman N. Antimicrobial stewardship. Am J Med 2006; 119:
wide knowledge and experience regarding multidrug- S53-61; discussion S62-S70 [PMID: 16735152 DOI: 10.1016/
resistant bacteria, to prevent the failure of treatment of j.amjmed.2006.04.004]
4 Dellit TH, Owens RC, McGowan JE, Gerding DN, Weinstein RA,
IDs both in the hospital and in the community. Burke JP, Huskins WC, Paterson DL, Fishman NO, Carpenter CF,
Brennan PJ, Billeter M, Hooton TM. Infectious Diseases Society of
America and the Society for Healthcare Epidemiology of America
IMPORTANCE OF ANTIMICROBIAL guidelines for developing an institutional program to enhance
antimicrobial stewardship. Clin Infect Dis 2007; 44: 159-177 [PMID:
SURVEILLANCE PROGRAMS 17173212 DOI: 10.1086/510393]
Antimicrobial surveillance programs (SENTRY, MYSTIC, 5 Society for Healthcare Epidemiology of America; Infectious
Diseases Society of America; Pediatric Infectious Diseases Society.
European Antimicrobial Resistance Surveillance System,
Policy statement on antimicrobial stewardship by the Society for
etc.) have become necessary for to control antimicrobial Healthcare Epidemiology of America (SHEA), the Infectious
resistance and to guide appropriate clinical decisions for Diseases Society of America (IDSA), and the Pediatric Infectious
[50]
anti-infective therapy . From antimicrobial surveillance Diseases Society (PIDS). Infect Control Hosp Epidemiol 2012; 33:
studies there can be obtained many information serving 322-327 [PMID: 22418625 DOI: 10.1086/665010]
6 Research Methods II: Multivariate Analysis. Chapter 1 The scientific
for antimicrobial resistance data. These programs
method. Continuing Medical Education. Oxford University Press:
detect emerging and changing resistance problems Journal of Tropical Pediatrics. Available from: URL: http://www.
and patterns, as well guide appropriate antimicrobial oxfordjournals.org/our_journals/tropej/online/ce_ch1.pdf
therapy, based on antibiotic susceptibility data. These 7 Sciencebuddies. Steps of the Scientific Method. Available from:
findings and results will help to the progress of the URL: http://www.sciencebuddies.org/science-fair-projects/project_s
[50] cientific_method.shtml
development of new antibiotic compounds .
8 Pulcini C, Gyssens IC. How to educate prescribers in antimicrobial
stewardship practices. Virulence 2013; 4: 192-202 [PMID: 23361336
DOI: 10.4161/viru.23706]
CONCLUSION 9 Özgenç O. The role of infectious disease specialist in antimicrobial
In summary, selection of the appropriate antimicrobial therapy. Turkish J Infect 2007; 21: 157-163
10 Ozgenç O, Genç VE, Ari AA, El Sibel S, Ozunlu H, Akgul
depends on understanding of the likely pathogens
A, Demirturk N, Cetin CB, Sungur M, Coşkuner SA, Avci M,
and local susceptibility patterns. In choosing the right Ergonul O. Evaluation of the therapeutic use of antibiotics in
antibiotics, the properties of the antimicrobials; such as Aegean Region hospitals of Turkey: a multicentric study. Indian
PK and PD profiles, activity and potency, tolerability and J Med Microbiol 2011; 29: 124-129 [PMID: 21654105 DOI:
[51]
safety, are all important factors . For the treatment 10.4103/0255-0857.81788]
11 Simoens S. Factors affecting the cost effectiveness of antibiotics.
of serious infections, the prudent antibiotic with the Chemother Res Pract 2011; 2011: 249867 [PMID: 22312550 DOI:
narrowest spectrum should be started early with 10.1155/249867]
the right dose, and should be given for an adequate 12 Gould IM. Antibiotic resistance: the perfect storm. Int J Antimicrob
WJM|www.wjgnet.com 151 June 26, 2016|Volume 6|Issue 2|
Özgenç O. Improving antibiotic implementation policies
Agents 2009; 34 Suppl 3: S2-S5 [PMID: 19596110 DOI: 10.1016/ strategy for meropenem. J Clin Pharmacol 2003; 43: 1116-1123
S0924-8579(09)70549-7] [PMID: 14517194 DOI: 10.1177/0091270003257225]
13 Levison ME, Levison JH. Pharmacokinetics and pharmacodynamics 31 Scheinfeld NS, Chandrasekar PH, Levy CS. Intravenous-to-Oral
of antibacterial agents. Infect Dis Clin North Am 2009; 23: 791-815, Switch Therapy. 2015. Available from: URL: http://emedicine.
vii [PMID: 19909885 DOI: 10.1016/j.idc.2009.06.008] medscape.com/article/237521-overview
14 Eliopoulos GM, Moellering RC. Principles of anti-infective therapy. 32 Cyriac JM, James E. Switch over from intravenous to oral therapy:
In: Bennett JE, Dolin R, Blaser MJ. Mandell, Douglas, and Bennett’s A concise overview. J Pharmacol Pharmacother 2014; 5: 83-87
Principles and Practice of Infectious Diseases. 8th ed. Canada: [PMID: 24799810 DOI: 10.4103/0976-500X.130042]
Elsevier Saunders, 2014: 224-234 33 Wetzstein GA. Intravenous to oral (iv: po) anti-infective conversion
15 Dzidic S, Bedeković V. Horizontal gene transfer-emerging multidrug therapy. Cancer Control 2000; 7: 170-176 [PMID: 10783821]
resistance in hospital bacteria. Acta Pharmacol Sin 2003; 24: 34 Tunkel AR, Hartman BJ, Kaplan SL, Kaufman BA, Roos KL,
519-526 [PMID: 12791177] Scheld WM, Whitley RJ. Practice guidelines for the management of
16 Fishman N. Appropriate antibiotic use. CDC’s Safe Healthcare bacterial meningitis. Clin Infect Dis 2004; 39: 1267-1284 [PMID:
Blog: Categories Antibiotic use, Healthcare-associated infections. 15494903 DOI: 10.1086/425368]
2010. Available from: URL: http://blogs.cdc.gov/safehealth 35 Hayashi Y, Paterson DL. Strategies for reduction in duration of
care/2010/06/08/critical-strategies-for-proper-antibiotic-use/ antibiotic use in hospitalized patients. Clin Infect Dis 2011; 52:
17 Livermore DM. Fourteen years in resistance. Int J Antimicrob 1232-1240 [PMID: 21507920 DOI: 10.1093/cid/cir063]
Agents 2012; 39: 283-294 [PMID: 22386741 DOI: 10.1016/j.ijantim 36 Quenot JP, Luyt CE, Roche N, Chalumeau M, Charles PE,
icag.2011.12.012] Claessens YE, Lasocki S, Bedos JP, Péan Y, Philippart F, Ruiz S,
18 Makmor-Bakry M, Mustafa S, Omar MS. Antimicrobial therapy in Gras-Leguen C, Dupuy AM, Pugin J, Stahl JP, Misset B, Gauzit R,
critically ill patients with nosocomial infections. Inter Pharm Pharm Brun-Buisson C. Role of biomarkers in the management of antibiotic
Sci 2011; 3: 340-342 therapy: an expert panel review II: clinical use of biomarkers for
19 Leekha S, Terrell CL, Edson RS. General principles of antimicrobial initiation or discontinuation of antibiotic therapy. Ann Intensive Care
therapy. Mayo Clin Proc 2011; 86: 156-167 [PMID: 21282489 DOI: 2013; 3: 21 [PMID: 23830525 DOI: 10.1186/2110-5820-3-21]
10.4065/mcp.2010.0639] 37 Chastre J, Wolff M, Fagon JY, Chevret S, Thomas F, Wermert
20 Gyssens IC. Antibiotic policy. Int J Antimicrob Agents 2011; 38 D, Clementi E, Gonzalez J, Jusserand D, Asfar P, Perrin D, Fieux
Suppl: 11-20 [PMID: 22018989 DOI: 10.1016/j.ijantimicag.2011.09. F, Aubas S. Comparison of 8 vs 15 days of antibiotic therapy for
002] ventilator-associated pneumonia in adults: a randomized trial.
21 Paterson DL, Rice LB. Empirical antibiotic choice for the seriously JAMA 2003; 290: 2588-2598 [PMID: 14625336 DOI: 10.1001/
ill patient: are minimization of selection of resistant organisms and jama.290.19.2588]
maximization of individual outcome mutually exclusive? Clin Infect 38 Leibovici L, Shraga I, Andreassen S. How do you choose antibiotic
Dis 2003; 36: 1006-1012 [PMID: 12684913 DOI: 10.1086/374243] treatment? BMJ 1999; 318: 1614-1616 [PMID: 10364128 DOI:
22 Cantón R, Morosini MI. Emergence and spread of antibiotic 10.1136/bmj.318.7198.1614]
resistance following exposure to antibiotics. FEMS Microbiol Rev 39 Retamar P, Portillo MM, López-Prieto MD, Rodríguez-López F, de
2011; 35: 977-991 [PMID: 21722146 DOI: 10.1111/j.1574-6976.201 Cueto M, García MV, Gómez MJ, Del Arco A, Muñoz A, Sánchez-
1.00295.x] Porto A, Torres-Tortosa M, Martín-Aspas A, Arroyo A, García-
23 Croisier D, Etienne M, Bergoin E, Charles PE, Lequeu C, Piroth Figueras C, Acosta F, Corzo JE, León-Ruiz L, Escobar-Lara T,
L, Portier H, Chavanet P. Mutant selection window in levofloxacin Rodríguez-Baño J. Impact of inadequate empirical therapy on the
and moxifloxacin treatments of experimental pneumococcal mortality of patients with bloodstream infections: a propensity score-
pneumonia in a rabbit model of human therapy. Antimicrob Agents based analysis. Antimicrob Agents Chemother 2012; 56: 472-478
Chemother 2004; 48: 1699-1707 [PMID: 15105123 DOI: 10.1128/ [PMID: 22005999 DOI: 10.1128/AAC.00462-11]
AAC.48.5.1699-1707.2004] 40 Stevens DL, Bisno AL, Chambers HF, Everett ED, Dellinger P,
24 García-León G, Sánchez MB, Martínez JL. The Inactivation Goldstein EJ, Gorbach SL, Hirschmann JV, Kaplan EL, Montoya JG,
of intrinsic antibiotic resistance determinants widens the mutant Wade JC. Practice guidelines for the diagnosis and management of
selection window for quinolones in Stenotrophomonas maltophilia. skin and soft-tissue infections. Clin Infect Dis 2005; 41: 1373-1406
Antimicrob Agents Chemother 2012; 56: 6397-6399 [PMID: [PMID: 16231249 DOI: 10.1086/497143]
23006759 DOI: 10.1128/AAC.01558-12] 41 Fishman N, Rybak MJ, Rice LB, Moellering RC, Tenover FC,
25 Dhand A, Sakoulas G. Reduced vancomycin susceptibility Paterson DL, McGowan JE. Roundtable discussion. Am J Med 2006;
among clinical Staphylococcus aureus isolates (‘the MIC Creep’): 119 (6A): S62-S70
implications for therapy. F1000 Med Rep 2012; 4: 4 [PMID: 42 Livermore DM. Has the era of untreatable infections arrived? J
22312414 DOI: 10.3410/M4-4] Antimicrob Chemother 2009; 64 Suppl 1: i29-i36 [PMID: 19675016
26 Cleveland Clinic. Guidelines for antimicrobial usage 2012-2013. DOI: 10.1093/jac/dkp255]
West Islip, NY: Professional Communications, 2012. Available 43 Hawkey PM, Livermore DM. Carbapenem antibiotics for serious
from: URL: https://www.clevelandclinicmeded.com/medicalpubs/ infections. BMJ 2012; 344: e3236 [PMID: 22654063 DOI: 10.1136/
antimicrobial-guidelines/pdf/Antimicrobial-2013.pdf bmj.e3236]
27 Kaye KS. Antimicrobial de-escalation strategies in hospitalized 44 Auer S, Wojna A, Hell M. Oral treatment options for ambulatory
patients with pneumonia, intra-abdominal infections, and bacteremia. patients with urinary tract infections caused by extended-spectrum-
J Hosp Med 2012; 7 Suppl 1: S13-S21 [PMID: 23677630 DOI: beta-lactamase-producing Escherichia coli. Antimicrob Agents
10.1002/jhm.983] Chemother 2010; 54: 4006-4008 [PMID: 20585127 DOI: 10.1128/
28 Bratzler DW, Dellinger EP, Olsen KM, Perl TM, Auwaerter AAC.01760-09]
PG, Bolon MK, Fish DN, Napolitano LM, Sawyer RG, Slain 45 Sun J, Deng Z, Yan A. Bacterial multidrug efflux pumps:
D, Steinberg JP, Weinstein RA. Clinical practice guidelines for mechanisms, physiology and pharmacological exploitations.
antimicrobial prophylaxis in surgery. Am J Health Syst Pharm 2013; Biochem Biophys Res Commun 2014; 453: 254-267 [PMID:
70: 195-283 [PMID: 23327981 DOI: 10.2146/ajhp120568] 24878531 DOI: 10.1016/j.bbrc.2014.05.090]
29 NHS Lothian-University Hospitals Division. Antimicrobials 46 Aeschlimann JR. The role of multidrug efflux pumps in the
prescribing guidelines in adults. 2015. Available from: URL: http:// antibiotic resistance of Pseudomonas aeruginosa and other gram-
www.nhslothian.scot.nhs.uk/AntimicrobialPrescribingGuidelines/ negative bacteria. Insights from the Society of Infectious Diseases
Documents/UHDAntimicrobialPrescribingGuidelines.pdf Pharmacists. Pharmacotherapy 2003; 23: 916-924 [PMID:
30 Kuti JL, Dandekar PK, Nightingale CH, Nicolau DP. Use of Monte 12885104 DOI: 10.1592/phco.23.7.916.32722]
Carlo simulation to design an optimized pharmacodynamic dosing 47 Sandiumenge A, Diaz E, Rodriguez A, Vidaur L, Canadell L, Olona
WJM|www.wjgnet.com 152 June 26, 2016|Volume 6|Issue 2|
Özgenç O. Improving antibiotic implementation policies
M, Rue M, Rello J. Impact of diversity of antibiotic use on the 50 Masterton R. The importance and future of antimicrobial
development of antimicrobial resistance. J Antimicrob Chemother surveillance studies. Clin Infect Dis 2008; 47 Suppl 1: S21-S31
2006; 57: 1197-1204 [PMID: 16565158 DOI: 10.1093/jac/dkl097] [PMID: 18713046 DOI: 10.1086/590063]
48 Piper GL, Kaplan LJ. Antibiotic heterogeneity optimizes 51 Masterton R, Drusano G, Paterson DL, Park G. Appropriate
antimicrobial prescription and enables resistant pathogen control antimicrobial treatment in nosocomial infections-the clinical
in the intensive care unit. Surg Infect (Larchmt) 2012; 13: 194-202 challenges. J Hosp Infect 2003; 55 Suppl 1: 1-12 [PMID: 14623198]
[PMID: 22913313 DOI: 10.1089/sur.2012.121] 52 Al-Tawfiq JA. The pattern and impact of infectious diseases
49 Department of Health (Australia). Antimicrobial resistance consultation on antimicrobial prescription. J Glob Infect Dis 2013; 5:
(AMR). National Antimicrobial Resistance Strategy (2015-2019). 45-48 [PMID: 23853430 DOI: 10.4103/0974-777X.112266]
[updated 2016 Mar 8]. Available from: URL: http://www.health.gov. 53 Livermore DM. Minimising antibiotic resistance. Lancet Infect Dis
au/internet/main/publishing.nsf/Content/ohp-amr.htm 2005; 5: 450-459 [PMID: 15978531]
P- Reviewer: El-Karaksy HM
S- Editor: Ji FF L- Editor: A E- Editor: Jiao XK
WJM|www.wjgnet.com 153 June 26, 2016|Volume 6|Issue 2|
Published by Baishideng Publishing Group Inc
8226 Regency Drive, Pleasanton, CA 94588, USA
Telephone: +1-925-223-8242
Fax: +1-925-223-8243
E-mail: bpgoffice@wjgnet.com
Help Desk: http://www.wjgnet.com/esps/helpdesk.aspx
http://www.wjgnet.com
© 2016 Baishideng Publishing Group Inc. All rights reserved.
You might also like
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Nematodes and Cestodes OutlineDocument6 pagesNematodes and Cestodes OutlineFarlogy80% (5)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Dermatology BookDocument479 pagesDermatology BookBharath Magesh100% (2)
- Diabetes and Ocular Disease Past, Present, and Future TherapiesDocument534 pagesDiabetes and Ocular Disease Past, Present, and Future TherapiesHealthCare100% (2)
- Infectious-Disease Tables PDFDocument81 pagesInfectious-Disease Tables PDFMiguel CuevasNo ratings yet
- Pidsr PDFDocument192 pagesPidsr PDFSef MartinezNo ratings yet
- Food and Industrial MicrobiologyDocument196 pagesFood and Industrial Microbiologyisabeljanuario67% (3)
- Curse of The PharaohsDocument30 pagesCurse of The Pharaohsstarling0102No ratings yet
- Nursing Quiz LeptospirosisDocument3 pagesNursing Quiz LeptospirosisChieChay Dub100% (2)
- Perioperative Fluid Management: Zubin M. Bamboat, M.D. and Liliana Bordeianou, M.DDocument6 pagesPerioperative Fluid Management: Zubin M. Bamboat, M.D. and Liliana Bordeianou, M.DluluksNo ratings yet
- HHS Public Access: Resuscitation FluidsDocument12 pagesHHS Public Access: Resuscitation FluidsluluksNo ratings yet
- CD 000567Document189 pagesCD 000567luluksNo ratings yet
- Bab 4. Jaringan EpitelDocument23 pagesBab 4. Jaringan EpitelluluksNo ratings yet
- English Non-Modul Check List Oral PresentationDocument2 pagesEnglish Non-Modul Check List Oral PresentationluluksNo ratings yet
- Molecules: Antibiotic Discovery: Combatting Bacterial Resistance in Cells and in Biofilm CommunitiesDocument13 pagesMolecules: Antibiotic Discovery: Combatting Bacterial Resistance in Cells and in Biofilm CommunitiesluluksNo ratings yet
- Investigation of Oxidative Stress Status in Metabolic Syndrome Patients Using Lipid Peroxidation BiomarkersDocument9 pagesInvestigation of Oxidative Stress Status in Metabolic Syndrome Patients Using Lipid Peroxidation BiomarkersluluksNo ratings yet
- Curriculum Vitae Indonesia International (Bio) Medical Students' Congress (INAMSC) 2018Document2 pagesCurriculum Vitae Indonesia International (Bio) Medical Students' Congress (INAMSC) 2018luluksNo ratings yet
- Kuliah DVTDocument29 pagesKuliah DVTluluksNo ratings yet
- Journal Analysis "Pico & Consort Checklist Methode": Luluk SilviaDocument31 pagesJournal Analysis "Pico & Consort Checklist Methode": Luluk SilvialuluksNo ratings yet
- Vol 26 1 2018 15Document10 pagesVol 26 1 2018 15sind badNo ratings yet
- MDH BrochureDocument2 pagesMDH Brochurerahms79No ratings yet
- Unidirctional Anti Covid-19 Gate Using Motion SensorDocument45 pagesUnidirctional Anti Covid-19 Gate Using Motion SensorMuhammad SalmanNo ratings yet
- Drug Impacts DA - Michigan7 2013Document301 pagesDrug Impacts DA - Michigan7 2013lbrahin1No ratings yet
- Welcome To The: One Health Hackathon!Document11 pagesWelcome To The: One Health Hackathon!SimbuNo ratings yet
- A Case of Pleural Effusion With Cardiomegaly Cured With HomoeopathyDocument9 pagesA Case of Pleural Effusion With Cardiomegaly Cured With HomoeopathyDr. Rajneesh Kumar Sharma MD Hom100% (1)
- Health Promotion and PreventionDocument1 pageHealth Promotion and PreventionBeverly PagcaliwaganNo ratings yet
- VPH 83.43 Rev.1Document60 pagesVPH 83.43 Rev.1jubatus.libroNo ratings yet
- Argoli - On DecumbitureDocument3 pagesArgoli - On Decumbituremurx2No ratings yet
- Laws On Notifiable DiseaseDocument43 pagesLaws On Notifiable DiseaseKenji ToleroNo ratings yet
- Union County State of Emergency DeclarationDocument1 pageUnion County State of Emergency DeclarationAnonymous jeL70dsNo ratings yet
- Jurnal Internasional Tentang ScabiesDocument9 pagesJurnal Internasional Tentang ScabiesGalyNo ratings yet
- Compliance of Lung 2003Document13 pagesCompliance of Lung 2003Narendra Bhattarai100% (1)
- Endotoxins: Myoglobin, Hemoglobin Exotoxin: Drugs Ethylene Glycol Contrast Medium Snakebite Nephropathy InfectionDocument34 pagesEndotoxins: Myoglobin, Hemoglobin Exotoxin: Drugs Ethylene Glycol Contrast Medium Snakebite Nephropathy InfectionpeekhakhaNo ratings yet
- Edema in ChildDocument16 pagesEdema in ChildKesava DassNo ratings yet
- Profiting From Pain Business and The U.S. Opioid EpidemicDocument3 pagesProfiting From Pain Business and The U.S. Opioid EpidemicSammy ChegeNo ratings yet
- The Effects of Ethical Differences To The Efficacy of The Government in Resolving The Current PandemicDocument9 pagesThe Effects of Ethical Differences To The Efficacy of The Government in Resolving The Current PandemicMark James GuerzonNo ratings yet
- Hyg Env Part 1.loDocument184 pagesHyg Env Part 1.loJayvee MendozaNo ratings yet
- Agent Subjects: Hallucinogenic TotallyDocument6 pagesAgent Subjects: Hallucinogenic Totallydreid19877453No ratings yet
- Malaria Drugs 210Document66 pagesMalaria Drugs 210fombayNo ratings yet
- Bacterial Zoonosis: Departemen Mikrobiologi FK USU MedanDocument59 pagesBacterial Zoonosis: Departemen Mikrobiologi FK USU MedanRima Christa Ulin SitepuNo ratings yet
- 03 Tourism and Infectous DiseaseDocument18 pages03 Tourism and Infectous DiseaseNur Afifah ShahrizalNo ratings yet