Professional Documents
Culture Documents
A
Uploaded by
Latifatul QolbyOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
A
Uploaded by
Latifatul QolbyCopyright:
Available Formats
Pneumonia is the third most common cause of death worldwide1 and remains responsible for
approximately 50% of all episodes of sepsis and septic shock. Both community-acquired bacterial
pneumonia (CABP) and hospitalacquired bacterial pneumonia (HABP) are associated with increased
morbidity, mortality, hospital length of stay, and health care costs. Furthermore, patients with ventilator-
acquired bacterial pneumonia (VABP) have longer mean hospital and intensive care unit (ICU) stays,
more mechanical ventilation days, and higher mortality than ICU non-VABP patients. In 2013,
pneumonia was among the 10 most economically charged diseases to the US health care systems, with an
aggregate cost of approximately $9.5 billion.
Despite advances in antimicrobial therapy and improvement in the clinical management of pneumonia,
treatment failure rates for HABP and CABP remain high at 30.0% to 62.0% and 2.4% to 31.0%,
respectively. Although many factors contribute to treatment failures, several of these factors concern the
provision of antibacterial therapy. Foremost, an antibiotic must be selected to which the suspected
causative organism is susceptible. However, the emergence of multidrug resistant (MDR) or extensive-
drug resistant (XDR) pathogens makes this a challenge, both in ensuring adequate likelihood of efficacy
and in preventing the inappropriate use of broadspectrum antibacterials. Indeed, drug resistance is
particularly important, given that the ESKAPE pathogens (Enterococcus faecium, Staphylococcus aureus,
Klebsiella pneumoniae, Acinetobacter baumannii, Pseudomonas aeruginosa, and Enterobacter species)
represent more than 80% of HABP. In addition to selecting the right drug, the right dose must be used.
Many antibacterials lack labeled indications for the treatment of pneumonia. Labeled doses for other
indications may yield insufficient concentrations in lung tissues or fail to account for variation among
patients, such as those with critical illness, obesity, augmented renal clearance, or those receiving organ
replacement therapies, such as hemodialysis or extracorporeal membrane oxygenation.
Optimal antibacterial treatment, which includes the correct selection of 1 or more antibiotics, dosing,
route of administration, and appropriate duration of therapy, significantly improves outcomes of patients
with pneumonia. Certainly, the ideal approach should maximize the likelihood of a satisfactory
microbiological response as well as minimize the exposure-related toxicity and the emergence and spread
of bacterial resistance. In this context, intelligent dosing decisions should be driven by the principles of
pharmacokinetics (PK) and pharmacodynamics (PD).
Although a significant portion of PK/PD studies are performed to identify optimal doses for use in
clinical trials, these methods can also be used in a patient-specific fashion to guide dosing. The latest
Infectious Diseases Society of America/American Thoracic Society (IDSA/ATS) guidelines for the
treatment of HABP/VABP weakly recommend PK/PD-driven dosing strategies. Although the downsides
of this approach are scant, involving cost and personnel burden, limited clinical evidence exists
supporting the practice, garnering the weak recommendation. Under these circumstances, the extent to
which patient-specific adjustment of antibacterial regimens based on PK/PD data should be used and its
potential impact on major outcomes are still under debate.
In the era of multidrug resistance, the optimization of antibiotic efficacy is a priority. Although several
promising new antibiotics are in development, some may lack the clear guidance of a labeled indication,
and others will be routinely used in poorly studied subpopulations. For patient-specific treatment
decisions, an understanding of PK/PD is indispensable. This article reviews the principle considerations
of PK and PD for the treatment of pneumonia, and highlights potential approaches to optimization and
future areas of investigation.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Perhitungan 1Document6 pagesPerhitungan 1Latifatul QolbyNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Assesment Terapi Oleh FarmasisDocument20 pagesAssesment Terapi Oleh FarmasisLatifatul QolbyNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- List of Common Medical AbbreviationsDocument2 pagesList of Common Medical AbbreviationsLatifatul QolbyNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- WHENDocument2 pagesWHENLatifatul QolbyNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- 1 2Document1 page1 2Latifatul QolbyNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Contoh Obat Ponstan Dengan Zat Aktif Asam MefenamatDocument3 pagesContoh Obat Ponstan Dengan Zat Aktif Asam MefenamatLatifatul QolbyNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Contoh Obat Ponstan Dengan Zat Aktif Asam MefenamatDocument3 pagesContoh Obat Ponstan Dengan Zat Aktif Asam MefenamatLatifatul QolbyNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Pet - WikipediaDocument12 pagesPet - Wikipediabdalcin5512No ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Board Review Endocrinology A. ApiradeeDocument47 pagesBoard Review Endocrinology A. ApiradeePiyasak NaumnaNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- Circulatory System Packet BDocument5 pagesCirculatory System Packet BLouise SalvadorNo ratings yet
- Chapter 5Document16 pagesChapter 5Ankit GuptaNo ratings yet
- Very Easy Toeic Units 7 - 12 (Q1)Document39 pagesVery Easy Toeic Units 7 - 12 (Q1)Minh KhaiNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Moral Character ViolationsDocument2 pagesMoral Character ViolationsAnne SchindlerNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Lesson 1 CA 3Document13 pagesLesson 1 CA 3myndleNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hydrogeological Characterization of Karst Areas in NW VietnamDocument152 pagesHydrogeological Characterization of Karst Areas in NW VietnamCae Martins100% (1)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Fluid Mechanics Sessional: Dhaka University of Engineering & Technology, GazipurDocument17 pagesFluid Mechanics Sessional: Dhaka University of Engineering & Technology, GazipurMd saydul islamNo ratings yet
- Calm Your Aggressive DogDocument58 pagesCalm Your Aggressive DogASd33475% (4)
- Health 6 Q 4 WK 6 Module 6 Version 4Document16 pagesHealth 6 Q 4 WK 6 Module 6 Version 4Kassandra BayogosNo ratings yet
- Nutrition During PregnancyDocument8 pagesNutrition During PregnancyHalliahNo ratings yet
- Alternate Mekton Zeta Weapon CreationDocument7 pagesAlternate Mekton Zeta Weapon CreationJavi BuenoNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- CHAPTER3 Foundations of Individual BehaviorDocument32 pagesCHAPTER3 Foundations of Individual BehaviorLynoj AbangNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Cfm56-3 Engine Regulation by CFMDocument43 pagesCfm56-3 Engine Regulation by CFMnono92100% (5)
- Case Studies On Industrial Accidents - 2Document84 pagesCase Studies On Industrial Accidents - 2Parth N Bhatt100% (2)
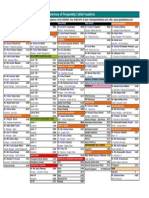
- Directory of Frequently Called Numbers: Maj. Sheikh RahmanDocument1 pageDirectory of Frequently Called Numbers: Maj. Sheikh RahmanEdward Ebb BonnoNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Akshaya Trust NgoDocument24 pagesAkshaya Trust NgodushyantNo ratings yet
- TS4-F - Fire SafetyDocument2 pagesTS4-F - Fire SafetyDominic SantiagoNo ratings yet
- ASR1201D ASR1201D-D: Slim Water-Proof RFID ReaderDocument1 pageASR1201D ASR1201D-D: Slim Water-Proof RFID ReaderCatalin BailescuNo ratings yet
- Design and Built-A4Document2 pagesDesign and Built-A4farahazuraNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Grade Eleven Test 2019 Social StudiesDocument6 pagesGrade Eleven Test 2019 Social StudiesClair VickerieNo ratings yet
- Proper Operating Room Decorum: Lee, Sullie Marix P. Maderal, Ma. Hannah Isabelle JDocument15 pagesProper Operating Room Decorum: Lee, Sullie Marix P. Maderal, Ma. Hannah Isabelle Jjoannamhay ceraldeNo ratings yet
- Mabuhay Wedding Package2006Document3 pagesMabuhay Wedding Package2006Darwin Dionisio ClementeNo ratings yet
- 07 Chapter2Document16 pages07 Chapter2Jigar JaniNo ratings yet
- WSAWLD002Document29 pagesWSAWLD002Nc BeanNo ratings yet
- The Girls Center: 2023 Workout CalendarDocument17 pagesThe Girls Center: 2023 Workout Calendark4270621No ratings yet
- InjectorDocument23 pagesInjectorBac Nguyen100% (1)
- Guide Propedevt Stomat 2c EngDocument256 pagesGuide Propedevt Stomat 2c EngJhoel Jhonatan Torres MuñozNo ratings yet
- Quiz EmbryologyDocument41 pagesQuiz EmbryologyMedShare90% (67)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)