Professional Documents
Culture Documents
Handout
Uploaded by
Erica Dagdag0 ratings0% found this document useful (0 votes)
22 views2 pages,mk
Copyright
© © All Rights Reserved
Available Formats
DOCX, PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this Document,mk
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
22 views2 pagesHandout
Uploaded by
Erica Dagdag,mk
Copyright:
© All Rights Reserved
Available Formats
Download as DOCX, PDF, TXT or read online from Scribd
You are on page 1of 2
OVERVIEW Complications
occurs when fluid builds up in the air sacs in Pulmonary complications:
your lungs. Barotrauma
may lead to death if it’s not treated quickly. Pulmonary fibrosis
Two types: Nosocomial pneumonia
a. Acute hypercapnic Acute lung injury
Develops over minutes to hours Cardiovascular complications:
there’s too much carbon dioxide in your Hypotension
blood, and near normal or not enough Reduced cardiac output
oxygen in your blood. Arrhythmia
pH is less than 7.3 Endocarditis
Causes: Acute myocardial infarction
COPD GI complications:
Severe asthma Hemorrhage
Drug overdose Gastric distention
Poisonings Ileus
Head and cervical injury Diarrhea
Pulmonary edema Pneumoperitoneum
ARDS Ulceration
b. Acute hypoxemic Acute renal failure
Don’t have enough oxygen in your Abnormalities of electrolytes and acid-
blood, but your levels of carbon dioxide base homeostasis
are close to normal. Malnutrition
Causes:
COPD DIFFERENTIAL DIAGNOSIS
Pneumonia
Pulmonary edema
Pulmonary fibrosis
Asthma
Pneumothorax
CLINICAL PRESENTATION
Common manifestations of Acute Respiratory
Failure
depend on its underlying cause and the levels of
carbon dioxide and oxygen in your blood.
People with a high carbon dioxide
level may experience:
• rapid breathing
• confusion
People with low oxygen levels may
experience:
• an inability to breathe
• bluish coloration in the skin,
fingertips, or lips
People with acute failure of the lungs
and low oxygen levels may
experience:
• restlessness
• anxiety
• sleepiness
• loss of consciousness
• rapid and shallow breathing
• racing heart
• irregular heartbeats
WORKUP
a. Laboratory Studies 8. Corticosteroids
ABG a. Methylprednisolone
A complete blood cell (CBC) count
serum creatine kinase with fractionation and TREATMENT AND MANAGEMENT
troponin I Medical Management
b. Radiography The objectives of treatment are:
Chest radiography a.) to correct the underlying cause
c. Echocardiography b.) to restore adequate gas exchange in the lung.
d. Pulmonary Function Test Intubation and mechanical ventilation
may be required.
MEDICATION
Goal: Nursing Management
o to achieve a pulmonary capillary wedge Nursing management of patients with acute respiratory
pressure of 15-18 mm Hg failure includes:
o a cardiac index greater than 2.2 a.) Assisting with intubation and maintaining
L/min/m2 while maintaining adequate mechanical ventilation.
blood pressure and organ perfusion b.) Assess respiratory status
1. Diuretics c.) Assess the entire respiratory system and
inhibits sodium chloride reabsorption in the implements strategies
ascending loop of Henle. d.) Assess the patient’s understanding of the
a. Furosemide (Lasix) management strategies that are used and initiates
b. Metolazone (Zaroxolyn) some form of communication
e.) Finally, the nurse must address the problems
2. Nitrates that led to the acute respiratory failure:
reduces myocardial oxygen demand by lowering
preload and afterload. Treatments:
a. Nitroglycerin sublingual
b. Nitroprusside sodium (Nitropress) pain medications or other medicines
Oxygen
3. Opioid Analgesics breathing tube / ventilator to help you breathe.
Morphine IV is an excellent adjunct in the tracheostomy may be necessary.
management of acute pulmonary edema.
venodilation, Other Treatments Help You Breathe
It also causes arterial dilatation
rocking bed consists of a mattress on a motorized
4. Inotropic Agents platform.
a. Dopamine
b. Norepinephrine (Levophed)
Fluids
c. Dobutamine
You may be given fluids to improve blood flow
5. Beta2 Agonists Too much fluid can fill the lungs and make it hard
act to decrease muscle tone in both small and for you to get the oxygen you need.
large airways in the lungs. Not enough fluid can limit the flow of oxygen-rich
a. Terbutaline (Brethaire, Bricanyl) blood to the body's organs.
b. Albuterol (Proventil)
6. Xanthine Derivatives
may relax smooth muscle of the bronchi.
a. Theophylline (Elixophyllin Elixir, Theo-24)
7. Anticholinergics,
antagonize the action of acetylcholine with
muscarinic receptor on bronchial smooth
muscle.
a. Ipratropium bromide (Atrovent HFA)
You might also like
- Postpartum ComplicationsDocument39 pagesPostpartum ComplicationsErica DagdagNo ratings yet
- Ob8pg PDFDocument8 pagesOb8pg PDFErica DagdagNo ratings yet
- 5 Health Laws, 1 Administration: With Grit and Determination, Crucial Laws Passed That Can Enhance Attainment of KPDocument8 pages5 Health Laws, 1 Administration: With Grit and Determination, Crucial Laws Passed That Can Enhance Attainment of KPErica DagdagNo ratings yet
- Malnutrition PDFDocument6 pagesMalnutrition PDFErica DagdagNo ratings yet
- Characteristics of A Good SummaryDocument7 pagesCharacteristics of A Good SummaryErica DagdagNo ratings yet
- Dagdag, Erica BSN Iv-BDocument4 pagesDagdag, Erica BSN Iv-BErica DagdagNo ratings yet
- Tumor Markers Common Manifestations Therapy/Treatment Others: Male CancersDocument9 pagesTumor Markers Common Manifestations Therapy/Treatment Others: Male CancersErica DagdagNo ratings yet
- Calorie Requirements For Growth After Severe Undernutrition: H. Rutishauser and A. MccanceDocument6 pagesCalorie Requirements For Growth After Severe Undernutrition: H. Rutishauser and A. MccanceErica DagdagNo ratings yet
- Circumstances Affecting Obligations: Law On Obligations Negligence/"Culpa"Document5 pagesCircumstances Affecting Obligations: Law On Obligations Negligence/"Culpa"Erica DagdagNo ratings yet
- RA 9173 Date: November 20, 1018Document2 pagesRA 9173 Date: November 20, 1018Erica DagdagNo ratings yet
- Filipino Word SearchDocument1 pageFilipino Word SearchErica Dagdag100% (1)
- A Study On Patient Satisfaction of Outpatient DepartmentDocument5 pagesA Study On Patient Satisfaction of Outpatient DepartmentErica DagdagNo ratings yet
- General Aspects On Post Partum Care of Laparoschisis in NewbornsDocument8 pagesGeneral Aspects On Post Partum Care of Laparoschisis in NewbornsErica DagdagNo ratings yet
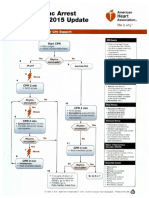
- ACLS 2015 AlgorithmDocument8 pagesACLS 2015 AlgorithmErica DagdagNo ratings yet
- ACLS 2015 Algorithm PDFDocument8 pagesACLS 2015 Algorithm PDFErica DagdagNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5795)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Denglish TestDocument139 pagesDenglish TestNabil HasanNo ratings yet
- MAPEH Q4 ScriptDocument4 pagesMAPEH Q4 Scriptcharice maanoNo ratings yet
- Lesson 4.2 - Operations On Modular ArithmeticDocument12 pagesLesson 4.2 - Operations On Modular ArithmeticMYLS SHRYNN ELEDANo ratings yet
- Vmware Virtualization Health Check ServiceDocument13 pagesVmware Virtualization Health Check ServicetvuongphamNo ratings yet
- Founders' ShareDocument2 pagesFounders' ShareHenry BerlangaNo ratings yet
- The Magical Diaries of Ethel ArcherDocument7 pagesThe Magical Diaries of Ethel Archerleeghancock100% (1)
- Police Forces and The Administration of Justice in Tanzania.Document6 pagesPolice Forces and The Administration of Justice in Tanzania.Praygod Manase100% (2)
- Catherine Davies - Modernity, Masculinity, and Imperfect Cinema in CubaDocument16 pagesCatherine Davies - Modernity, Masculinity, and Imperfect Cinema in CubakahlilchaarNo ratings yet
- Pale ExamDocument4 pagesPale ExamPatrick Tan100% (1)
- Program 2019 MTAPTL Annual Convention PDFDocument3 pagesProgram 2019 MTAPTL Annual Convention PDFrichardlfigueroaNo ratings yet
- A Feasibility/Project Study OnDocument14 pagesA Feasibility/Project Study OnWilson Domingo LazarteNo ratings yet
- Melo V PeopleDocument1 pageMelo V PeoplejjangNo ratings yet
- Rob Corry: People's Motion For Hearing To Determine Existence of Conflict-Free RepresentationDocument4 pagesRob Corry: People's Motion For Hearing To Determine Existence of Conflict-Free RepresentationMichael_Lee_RobertsNo ratings yet
- Math Studies Financial MathsDocument7 pagesMath Studies Financial MathsGirish MishraNo ratings yet
- Kids Cooking Teams: That's FreshDocument74 pagesKids Cooking Teams: That's FreshNCB School of Herbalism & Holistic HealthNo ratings yet
- 10 Rules of Statcon by Atty Marcus NeelyDocument4 pages10 Rules of Statcon by Atty Marcus NeelyMorin OcoNo ratings yet
- Distortion of The Ecclesiological Views of Metropolitan Chrysostomos of PhlorinaDocument11 pagesDistortion of The Ecclesiological Views of Metropolitan Chrysostomos of PhlorinaHibernoSlavNo ratings yet
- Reich 0001 PDFDocument87 pagesReich 0001 PDFYordys Domínguez RodríguezNo ratings yet
- CALDER New Research On Low-Frequency Membrane AbsorbersDocument11 pagesCALDER New Research On Low-Frequency Membrane AbsorbersAndre VareNo ratings yet
- China Email ListDocument3 pagesChina Email ListRosie Brown40% (5)
- Biologic and Biophysical Technologies. FINALDocument28 pagesBiologic and Biophysical Technologies. FINALRafael Miguel MallillinNo ratings yet
- The Real World An Introduction To Sociology Test Bank SampleDocument28 pagesThe Real World An Introduction To Sociology Test Bank SampleMohamed M YusufNo ratings yet
- Openstack Deployment Ops Guide PDFDocument197 pagesOpenstack Deployment Ops Guide PDFBinank PatelNo ratings yet
- Demand, Elasticity of Demand and Demand ForecastingDocument16 pagesDemand, Elasticity of Demand and Demand Forecastingankit thapliyal100% (1)
- Fractal Blaster Trading Strategy ReportDocument22 pagesFractal Blaster Trading Strategy ReportIcky IckyNo ratings yet
- Title Toolbox 1 ADocument2 pagesTitle Toolbox 1 AGet LiveHelpNo ratings yet
- E5170s-22 LTE CPE - Quick Start Guide - 01 - English - ErP - C - LDocument24 pagesE5170s-22 LTE CPE - Quick Start Guide - 01 - English - ErP - C - LNelsonNo ratings yet
- Entrep Module 4 Q1 Week 4 1Document14 pagesEntrep Module 4 Q1 Week 4 1VirplerryNo ratings yet
- Business Mathematics 11 Q2 Week3 MELC20 MELC21 MOD Baloaloa, JeffersonDocument25 pagesBusiness Mathematics 11 Q2 Week3 MELC20 MELC21 MOD Baloaloa, JeffersonJefferson BaloaloaNo ratings yet
- Reflective Journal 4Document3 pagesReflective Journal 4api-550030025No ratings yet