Professional Documents
Culture Documents
Liu Et Al-2016-Frontiers in Microbiology PDF
Uploaded by
galih widodoOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Liu Et Al-2016-Frontiers in Microbiology PDF
Uploaded by
galih widodoCopyright:
Available Formats
ORIGINAL RESEARCH
published: 19 August 2016
doi: 10.3389/fmicb.2016.01268
Tracking Cefoperazone/Sulbactam
Resistance Development In vivo in
A. baumannii Isolated from a Patient
with Hospital-Acquired Pneumonia
by Whole-Genome Sequencing
Xiaofen Liu 1,2 , Huajun Zheng 3 , Weipeng Zhang 4 , Zhen Shen 1 , Miao Zhao 1 ,
Yuancheng Chen 1,5 , Li Sun 1 , Jun Shi 2 and Jing Zhang 1,5*
1
Institute of Antibiotics, Huashan Hospital, Fudan University, Shanghai, China, 2 Roche Innovation Center Shanghai,
Shanghai, China, 3 Shanghai-MOST Key Laboratory of Health and Disease Genomics, Chinese National Human Genome
Center at Shanghai, Shanghai, China, 4 Division of Life Science, The Hong Kong University of Science and Technology, Hong
Edited by: Kong, China, 5 Key Laboratory of Clinical Pharmacology of Antibiotics, National Population and Family Planning Commission,
Margaret Ip, Shanghai, China
The Chinese University of Hong Kong,
China
Cefoperazone/sulbactam has been shown to be efficacious for the treatment of
Reviewed by:
Soledad Ramirez,
infections caused by Acinetobacter baumannii; however, the mechanism underlying
California State University, Fullerton, resistance to this synergistic combination is not well understood. In the present study,
USA
two A. baumannii isolates, AB1845 and AB2092, were isolated from a patient with
Sónia Gonçalves,
Faculdade de Medicina da hospital-acquired pneumonia before and after 20 days of cefoperazone/sulbactam
Universidade de Lisboa, Portugal therapy (2:1, 3 g every 8 h with a 1-h infusion). The minimum inhibitory concentration
*Correspondence: (MIC) of cefoperazone/sulbactam for AB1845 and AB2092 was 16/8 and 128/64 mg/L,
Jing Zhang
zhangj_fudan@aliyun.com
respectively. Blood samples were collected on day 4 of the treatment to determine the
concentration of cefoperazone and sulbactam. The pharmacokinetic/pharmacodynamic
Specialty section: (PK/PD) indices (%T>MIC ) were calculated to evaluate the dosage regimen and
This article was submitted to
Antimicrobials, Resistance
resistance development. The results showed that %T>MIC of cefoperazone and
and Chemotherapy, sulbactam was 100% and 34.5% for AB1845, and 0% and 0% for AB2092, respectively.
a section of the journal
Although there was no available PK/PD target for sulbactam, it was proposed that
Frontiers in Microbiology
sulbactam should be administered at higher doses or for prolonged infusion times to
Received: 17 May 2016
Accepted: 02 August 2016 achieve better efficacy. To investigate the mechanism of A. baumannii resistance to
Published: 19 August 2016 the cefoperazone/sulbactam combination in vivo, whole-genome sequencing of these
Citation: two isolates was further performed. The sequencing results showed that 97.6% of the
Liu X, Zheng H, Zhang W, Shen Z,
Zhao M, Chen Y, Sun L, Shi J and
genome sequences were identical and 33 non-synonymous mutations were detected
Zhang J (2016) Tracking between AB1845 and AB2092. The only difference of these two isolates was showed
Cefoperazone/Sulbactam Resistance
in sequencing coverage comparison. There was a 6-kb amplified DNA fragment which
Development In vivo in A. baumannii
Isolated from a Patient with was three times higher in AB2092, compared with AB1845. The amplified DNA fragment
Hospital-Acquired Pneumonia by containing the blaOXA−23 gene on transposon Tn2009. Further quantitative real-time
Whole-Genome Sequencing.
Front. Microbiol. 7:1268.
PCR results demonstrated that gene expression at the mRNA level of blaOXA−23 was
doi: 10.3389/fmicb.2016.01268 >5 times higher in AB2092 than in AB1845. These results suggested that the blaOXA−23
Frontiers in Microbiology | www.frontiersin.org 1 August 2016 | Volume 7 | Article 1268
Liu et al. Cefoperazone/Sulbactam Resistance Development In vivo
gene had higher expression level in AB2092 via gene amplification and following
transcription. Because gene amplification plays a critical role in antibiotic resistance in
many bacteria, it is very likely that the blaOXA−23 amplification results in the development
of cefoperazone/sulbactam resistance in vivo.
Keywords: cefoperazone/sulbactam, Acinetobacter baumannii, whole-genome sequencing, resistance
development, PK/PD indices
INTRODUCTION sequencing revealing the mechanism of bacterial pathogen
resistance that develops in patients (Snitkin et al., 2011; Wright
Acinetobacter baumannii is a non-fermentative, gram-negative et al., 2014; Holt et al., 2015). Wright et al. (2016) sequenced 136
opportunistic pathogen that can cause hospital-acquired strains of A. baumannii isolated from patients and showed the
pneumonia (HAP), blood infections and urinary tract infection, genome changes occurred mainly due to the single nucleotide
among others (Perez et al., 2007). The rapid spread of the variance in protein coding regions and IS element. Genome
multi-drug-resistant A. baumannii has resulted in very limited sequenced A. baumannii showed the colistin resistance was due
therapeutic options in the clinic. Sulbactam, a β-lactamase to the mutations in transcriptional regulatory genes (Cheah et al.,
inhibitor, has intrinsic antimicrobial effects against A. baumannii 2016). Susceptible S. aureus evolved resistance via a 35-point
by binding to penicillin-binding protein 2 (Peleg et al., 2008). mutation in 31 loci in a patient with a bloodstream infection
It is commercially available in a combined formulation receiving vancomycin therapy (Mwangi et al., 2007). Tigecycline
of ampicillin and cefoperazone. The clinical efficacy of resistance to A. baumannii has been reported to be due to
cefoperazone/sulbactam has been shown in previous work the deletion of three contigs in vivo (Hornsey et al., 2011).
(Xin et al., 2013; Sipahi et al., 2014; Xia et al., 2014). This Additionally, gene amplification was frequently detected due to
combination has recently been applied to treat critically ill the antibiotic pressure. The evolution of β-lactamase resistance
patients receiving continuous venovenous hemofiltration, and was studied by exposing Salmonella typhimurium, which
11 of 14 patients survived (Gao et al., 2016). This combination contain low level β-lactamase resistance, in an environment
was also administrated to treat neurosurgical patients in a of progressively increasing concentrations of cephalosporin.
pilot study, with the results showing that cerebrospinal fluid The results showed an amplification of blaTEM−1 gene copy
penetration of cefoperazone/sulbactam could be enhanced after number followed by acquisition of gene mutations (Sun et al.,
neurosurgical impairment of the blood-brain barrier (Wang 2009). A genome-wide assay of E. coli strain in 78 different
et al., 2015). In a retrospective review of the outcomes for antibiotic environments found that 56 genes were amplified to
patients with cefoperazone/sulbactam treated A. baumannii fit the environment and reproducible increasing in MIC for
bacteremia, 77% of the patients (27/35) presented successful their corresponding antibiotics was detected (Soo et al., 2011).
clinical efficacy (Choi et al., 2006). Because the combination has The amplification of aminoglycoside resistance gene aphA1
been widely used in the clinic, the resistance rate was monitored in A. baumannii has been considered to be the mechanism
and observed to increase from 25.0 to 37.7% from 2004 to 2010 underlying the development of tobramycin in vivo (McGann
in China (Hu et al., 2016). However, the underlying mechanism et al., 2014).
is not well understood in vitro or in vivo, for sulbactam alone In the present study, two A. baumannii isolates,
or the combination. Sulbactam alone has been reported to AB1845 and AB2092, were collected before and after
cause resistance in A. baumannii via PBP3 mutation in vitro, cefoperazone/sulbactam therapy from a patient with HAP.
despite a lack of information regarding natural pbp3 mutations Pharmacokinetics/pharmacodynamics (PK/PD) was applied to
in clinical isolates (Penwell et al., 2015). The detection and evaluate the dosage regimen and development of resistance.
expression of blaTEM−1 has been suggested to relate to the Moreover, whole-genome sequencing was employed to
minimum inhibitory concentration (MIC) of sulbactam in investigate the mechanism of cefoperazone/sulbactam resistance
A. baumannii (Waltner-Toews et al., 2011). The combination of the two isolates developed in vivo.
resistance in Klebsiella pneumoniae in an in vitro study was
reported owing to two different mechanisms, loss of a 39-kDa
outer membrane protein and presence of TEM-2 β-lactamase MATERIALS AND METHODS
(Rice et al., 1993).
Whole-genome sequencing is powerful and can reveal a Medical Records and Treatment
vast amount of DNA information from a global perspective. This study was approved by the institutional review board
The published complete genome sequences for many bacteria of Huashan Hospital affiliated to Fudan University. Written
are beneficial and efficient for strain-to-reference sequencing informed consent was obtained from the patient. A 19-year-
and bioinformatics analysis (Mardis, 2008). They can be used old male patient with serious brain trauma was admitted
to identify resistance genes as well as minor changes in the to Huashan Hospital (Shanghai, China). The patient had a
genome due to mutation, gene transfer, gene duplication, and high fever with white blood cell counts out of the normal
amplification. It has been seen as a basis for whole-genome range after being checked into bed for 48 h. Both chest
Frontiers in Microbiology | www.frontiersin.org 2 August 2016 | Volume 7 | Article 1268
Liu et al. Cefoperazone/Sulbactam Resistance Development In vivo
X-Ray radiophotography and computed tomography showed were cleaned using the FASTX toolkit1 . Genome assembly
pneumonia. A. baumannii (AB1845) was isolated from the was performed using Velvet (Ver 1.0.15) (Zerbino and Birney,
sputum of the patient, revealing bacterial infection. Hence, 2008). Putative protein-coding sequences were determined by
the patient was treated with meropenem 0.5 g q8h without combining the prediction results of the glimmer 3.02 (Delcher
clinical efficacy. On day 6, the dosage regimen was changed to et al., 2007) and Z-Curve (Guo and Zhang, 2006) program. The
cefoperazone/sulbactam (2:1, 3 g every 8 h with a 1-h infusion, phylogenetic tree was constructed using PHYML (Guindon and
SULPERAZON
, batch no. 95839116) for 20 days. The treatment
R
Gascuel, 2003) by concatenating orthologs based on the protein
was stopped when body temperature and white blood cell counts sequences in the published genome. Functional annotation of
returned to the normal range; additionally, A. baumannii was CDS was performed by searching the NCBI non-redundant
not detected in the sputum. However, the patient had a fever, protein database and the KEGG protein database (Kanehisa
and A. baumannii (AB2092) was again isolated 4 days after et al., 2016). Gene annotation was mapped to the A. baumannii
cefoperazone/sulbactam treatment. The cefoperazone/sulbactam MDR-ZJ06 genome (from the phylogenetic tree) using Bowtie2
treatment was finally considered to have failed both clinically and with default settings (Langmead and Salzberg, 2012). Single
microbiologically efficacy. Nucleotide Polymorphisms (SNPs) from alignments were called
using Samtools-0.1.16 (Li et al., 2009), and the output was
generated in the pileup format. Gene amplification was detected
Pharmacokinetics of by comparing the coverage of the reads in AB1845 and Ab2092
Cefoperazone/Sulbactam Treatment using the read depth method (Redon et al., 2006).
Blood samples were collected before the first infusion,
immediately after the infusion (0 h), and at 0.5, 1, 2, Quantitative Real-Time PCR Analysis of
4, 6 h afterward on day 4 (i.e., steady state) of the
cefoperazone/sulbactam treatment. The drug concentration
blaOXA−23
The mRNA expression level of blaOXA−23 was quantified by
was determined using the LC-MS/MS method (Zhou et al.,
real-time PCR. AB1845 and AB2092 were cultured in cation-
2010), which was validated according to the CFDA guidelines
adjusted Mueller-Hinton broth and collected during the early
on bioanalytical method validation. The pharmacokinetic
log phase. Total RNA was extracted using a TaKaRa Mini
parameters of the patients were calculated by Winnonlin (v6.0,
BEST Universal RNA Extraction Kit (TaKaRa Biotechnology,
phoenix). The patient’s pharmacokinetic profiles of cefoperazone
Dalian, China) according to the manufacturer’s instruction.
and sulbactam were fit into a well-developed population PK
Quantitative real-time PCR (qPCR) was performed using a
model (Chen et al., 2015). The PK/PD indice of cefoperazone
two-step process. RNA was first reverse-transcribed to cDNA
and sulbactam was %T>MIC , namely the percentage of the dosing
(TaKaRa Biotechnology, Dalian, China), and real-time PCR
interval for which the plasma concentration of cefoperazone or
was conducted on an ABI Vii7 (Applied Biosystems, Carlsbad,
sulbactam above the MIC. It was calculated based on the drug
CA, USA) using a TaKaRa SYBR
FAST qPCR Kit with 40
R
pharmacokinetic profile and MICs of the combination (Lips
cycles of denaturation for 5 s at 95◦ C, annealing for 30 s at
et al., 2014).
50◦ C, and extension for 20 s at 72◦ C. The PCR primers for
the blaOXA−23 gene were F: CCGAGTCAGATTGTTCAAGGA
Bacterial Isolates and Susceptibility and R: TGTAGAGGCTGGCACATATTC; and those for 16S
Testing rRNA were F: GGCGGCTTATTAAGTCGGATG and R:
Acinetobacter baumannii AB1845 and AB2092 were TTCGTACCTCAGCGTCAGTATT. The melting curve analysis
isolated from the sputum of the patient before and after was performed immediately after amplification to verify the
cefoperazone/sulbactam therapy. Both isolates were stored specificity of the PCR amplification products.
at −80◦ C. The MIC was determined in cation-adjusted Fluorescence was measured at the end of the annealing-
Mueller-Hinton broth (Becton-Dickinson, Sparks, MD, extension phase of each cycle. A threshold value for the
USA) using a broth microdilution according to Clinical fluorescence of all samples was set manually. The reaction cycle at
and Laboratory Standards Institute (CLSI) standards. The MICs which the PCR product exceeded this fluorescence threshold was
of the β-lactam/β-lactamase inhibitor combination, including identified as the threshold cycle (CT). The relative quantitation
cefoperazone/sulbactam, carbapenems, colistin, and polymyxin was calculated by the 2-11CT method (Schmittgen and Livak,
B, were determined. 2008). The student t-test was applied to evaluate the significance
of the gene expression level of the two isolates.
Genome Sequencing and Analysis
Genomic DNA was extracted using a Genomic DNA Purification RESULTS
Kit (Tiangen, Beijing, China) according to the instruction manual
and stored at −80◦ C before sequencing. A 300-bp paired-end Antibiotic Susceptibility
library was constructed for the purified DNA sample following Minimum inhibitory concentrations were obtained for
the standard Illumina paired-end protocol. Cluster generation cefoperazone/sulbactam combinations, carbapenems, colistin
was performed in C-bot, and sequencing was performed on
the Illumina Hiseq2500 with 150 cycles. The sequence reads 1
http://hannonlab.cshl.edu/fastx_toolkit/
Frontiers in Microbiology | www.frontiersin.org 3 August 2016 | Volume 7 | Article 1268
Liu et al. Cefoperazone/Sulbactam Resistance Development In vivo
and polymyxin B for the pre-therapy isolate AB1845 and Pharmacokinetics and
the post-therapy isolate AB2092 (Table 1). The MICs of the Pharmacodynamics (PK/PD)
cefoperazone/sulbactam combination were 16/8 mg/L for
Plasma concentrations of cefoperazone and sulbactam at steady
AB1845; and the MICs of mono cefoperazone and sulbactam
state were determined using the validated LC-MS/MS method,
were >128 mg/L and 32 mg/L. The results supported a synergistic
and the data were fitted into a developed population PK model
effect of the combination (FICI < 0.5, MIC of cefoperazone
(Figure 1). The pharmacokinetic parameters of cefoperazone and
was set at 128 mg/L for the FICI calculation). However, the
sulbactam are summarized in Table 2. The T1/2 of cefoperazone
MICs of the combination and mono drugs were 128/64, >128,
was 4.1 h, which was a bit longer than the reported 1.8 h (Reitberg
and 128 mg/L for AB2092. The combination did not display a
et al., 1988). This could attribute to liver dysfunction (Boscia et al.,
synergistic effect on AB2092.
1983) according to the medical records of the patients. The T1/2
Interestingly, AB1845 and AB2092 also developed
of sulbactam was 1.3 h, which was comparable to the published
meropenem resistance with MIC increased from 16 to 64 mg/L,
data (Reitberg et al., 1988).
although the bacteria only exposed to meropenem for a
Pharmacokinetic/pharmacodynamic indices were calculated
short term (0.5 g every 8 h for 4 days). The isolates also
to evaluate the drug dosage regimen. The %T>MIC was the most
developed resistance to imipenem and doripenem. Since
predictive PK/PD index for cefoperazone and sulbactam (Cooper
both cefoperazone and meropenem are β-lactam antibiotics,
et al., 2011; Sy et al., 2015), and the MIC of the combination was
the increased MIC in both cefoperazone/sulbactam and
used for the %T>MIC calculation. In this study, the %T>MIC was
carbapenems may imply the similar underlying resistance
100% for cefoperazone and 34.5% for sulbactam for AB1845; and
mechanism. The isolates were only sensitive to colistin
the %T>MIC was 0% for both cefoperazone and sulbactam for
and polymyxin B, indicating an alternative choice for the
AB2092.
AB2092 treatment. The MICs of the antibiotics are shown in
Table 1.
Whole-Genome Sequencing of AB1845
and AB2092
The two isolates were initially typed by PFGE of ApaI-digested
TABLE 1 | The minimum inhibitory concentrations (MICs) of different
antibiotics for AB1845 and AB2092.
genomic DNA and shown to be the same strain. Whole-genome
Antibiotics MIC (mg/L)
TABLE 2 | Pharmacokinetic parameters of cefoperazone and sulbactam.
AB1845 AB2092
Parameters Units Cefoperazone Sulbactam
Cefoperazone/sulbactam 16/8∗ 128/64
Cefoperazone >128 >128 T 1/2 h 4.1 1.3
Sulbactam 32 128 T max h 1.4 1.3
Meropenem 16 64 Cmax mg/L 129.6 37.2
Imipenem 16 64 AUC0−8 mg h/L 529.1 66.5
Doripenem 32 128 AUC0−inf mg h/L 766.0 68.3
Colistin 2 2 Vd L 15.5 26.6
Polymyxin B 1 1 CLt L/h 2.6 14.6
∗ FICI= 0.375; FICI = MIC(A) /MIC(A in combination) + MIC(B) /MIC(B in combination) . The MRT0−8 h 2.6 1.5
bold values showed the increasing MIC of AB1845 compared with AB2092. MRT0−inf h 5.7 1.6
FIGURE 1 | The pharmacokinetic profiles of cefoperazone (A) and sulbactam (B). The dots in (A,B) are the concentration determined by LC-MS/MS (before
the first infusion on Day 4 and 0.5, 1, 2, 4, 6 h after the infusion), and the curves are the profiles fitted to the population pharmacokinetic model. The red lines were
indicated the concentration for the MIC of AB1845.
Frontiers in Microbiology | www.frontiersin.org 4 August 2016 | Volume 7 | Article 1268
Liu et al. Cefoperazone/Sulbactam Resistance Development In vivo
A comparison of the CDS of AB1845 and AB2092 revealed
only 33 SNPs. All of these SNPs were synonymous, indicating that
SNP was not the main reason for the development of resistance
(Supplementary Table S1).
β-Lactamase and Gene Amplification
A well-known resistance enzyme for β-lactam antibiotics is
β-lactamase. The class A, C, and D classes (blaOXA−23 and
blaOXA−51 ) β-lactamase were identified in both AB1845 and
AB2092 (Supplementary Table S2).
Gene amplification was detected by whole-genome
sequencing in combination with the read depth method
(Cantsilieris et al., 2012). Approximately 99.9% of the genes
had a coverage ratio of AB2092 to AB1845 of approximately
1.0, but six genes (out of 3871 genes) had a coverage ratio
over 3.0 (Supplementary Table S3). These six genes were AAA
ATPase, DEAD/DEAH box helicases, blaOXA−23 , and three
hypothetical genes. Among these genes, AAA ATPase and
DEAD/DEAH box helicases are involved in the function of
DNA replication, repair, transcription, and two uncharacterized
genes (Johnson and Mckay, 1999; Iyer et al., 2004). The
blaOXA−23 was gene encoded class D β-lactamase and conferred
FIGURE 2 | Phylogenetic tree of AB1845 and AB2092 with 16 complete
genomes of A. baumannii isolates in ftp://ftp.ncbi.nlm.nih.gov/
resistance to carbapenems and cefoperazone (Pascale and
genomes/archive/old_genbank/. Wright, 2010; Bush, 2013). All six genes were located in a
6-kb sequence fragment in AB1845 designated as Tn2009.
Tn2009 was flanked by two ISAba1 elements that contributed
to the duplication of Tn2009 in AB2902 (Liu et al., 2015).
sequencing produced 12,050,346 and 12,191,576 pairs of 150- The amplified genes were transcribed in the same orientation
bp reads for AB1845 and AB2092, respectively. Assembly of the (Figure 4).
AB1845 and AB2092 genomes resulted in 132 and 131 contigs
larger than 500 bp, comprising 4.0 megabases of sequence and mRNA Level of blaOXA−23 in AB1845 and
representing a median 930-fold coverage. The AB1845 draft AB2092
assembly has been deposited in GenBank (accession number Quantitative real-time PCR was conducted to measure the
LVYA00000000), and raw sequence reads for AB1845 and mRNA levels of blaOXA−23 in AB1845 and AB2092. Both
AB2092 have been submitted to NCBI’s Sequence Read Archive isolates were collected at the early log phase, and the qPCR
under the study accession number SRP072783. results showed that the mRNA level of blaOXA−23 was
Automated gene prediction detected 3,811 and 3,810 putative five times higher in AB2092 than in AB1845 (Figure 5).
coding sequences (CDSs) for AB1845 and AB2092, respectively. This finding was consistent with the gene amplification
A phylogenetic tree was constructed, and the genome similarity results.
was compared (Figure 2). The 3,718 CDSs were homologous
(defined as a BLASTN e-value ≤ 1e−10 ) to the genome of
A. baumannii MDR-ZJ06, which was a multi-drug-resistant DISCUSSION
isolate belonging to International clone II and wide spreading
in China (Zhou et al., 2011). MDR-ZJ06 was used as a reference Acinetobacter baumannii commonly colonizes in respiratory
genome for annotating genes in AB1845 and AB2092 (Figure 3). tract of the hospitalized patients (Peleg et al., 2008). It is
The results showed that the two isolates possess 97.6% similarity difficult to characterize A. baumannii isolated from sputum
to MDR-ZJ06, with 921 and 915 SNPs, respectively. Certain belongs to the upper airway colonization or the causative
genes were missing in both AB1845 and AB2092 compared pathogen of pneumonia. In this study, the two isolates were
with MDR-ZJ06. For example, 17 genes had a 15-kb fragment considered causative pathogens, as verified by pneumonia
that was missing in the resistant island AbaR22, which includes testing and symptoms such as cough, fever, and high white
transposition helper proteins, site-specific tyrosine recombinase, blood cell counts. To examine the mechanism of resistance
transposase protein A and conserved hypothetical proteins, development during cefoperazone/sulbactam treatment, both
among others. PK/PD indices and genomic sequencing were employed
The CDS of AB1845 was also mapped to the published to understand the problem from a PK/PD and molecular
plasmid sequence. It showed that certain AB1845 genes mapped perspective.
to plasmid ABKp1 from the A. baumannii 1656-2 plasmid with Exposure to a sub-optimal antibiotic concentration is the most
97.6% similarity. important factor in the development of bacterial resistance. To
Frontiers in Microbiology | www.frontiersin.org 5 August 2016 | Volume 7 | Article 1268
Liu et al. Cefoperazone/Sulbactam Resistance Development In vivo
FIGURE 3 | Atlas of the A. baumannii AB1845 draft genome. Each concentric circle represents the genomic data for AB1845. The two outer circles illustrate the
predicted coding sequences on the plus and minus strands, respectively, colored by functional categories according to the COG classification. The third circle
represents the location of the nucleotide substitution between AB1845 and AB2092, with blue representing genes affected by synonymous Single Nucleotide
Polymorphisms (SNPs) and red representing SNPs in the intergenic region. The fourth circle displays the loci of the β-lactamase genes (pink) and genes around
blaOXA−23 (gray). The fifth circle shows the GC content, and the 6th circle (innermost) represents GC skew (G–C)/(G+C) calculated using a 1-kb window.
FIGURE 4 | The illustration of the 6-kb DNA fragment of Tn2009 in AB1845 and AB2092. The fragment was amplified three times in AB2092.
optimize the antibiotic dosage regimen and prevent resistance, drug concentrations (Martinez et al., 2012). In this study, blood
the PK/PD which bridges drug exposure and effect, has been samples were collected at steady state, and the MIC of the
widely applied in the clinics (Abdulaziz et al., 2015; Asín- bacteria was determined. As the most predictive PK/PD index,
Prieto et al., 2015; Monogue et al., 2015). To date, the PK/PD the %T>MIC of cefoperazone and sulbactam was calculated
helps adjust dosage based on the evaluation of steady-state and compared with published PK/PD targets. The published
Frontiers in Microbiology | www.frontiersin.org 6 August 2016 | Volume 7 | Article 1268
Liu et al. Cefoperazone/Sulbactam Resistance Development In vivo
2015). IS elements are associated with the genome gain/loss
of genes, especially resistant genes. These two transposons
share ISAba1 upstream from blaOXA−23 , which belongs to
the IS4 family, provides promoter for blaOXA−23 (Turton
et al., 2006; Mugnier et al., 2009), which could explain the
gene duplication or amplification in this study. The mRNA
level of blaOXA−23 confirmed the higher expression level of
AB2092 and AB1845. There is evidence that gene duplication
and amplification in bacteria was directly associated with
adaptation to environmental changes, including antibiotic
stress (Sandegren and Andersson, 2009). In a study testing the
relationships of gene amplification and β-lactams resistance
increase showed that 70% colonies of S. Typhimurium with
increased resistance to cephalosporin had increased blaTEM
gene copy numbers (Sun et al., 2009). Recent study showed
FIGURE 5 | Quantitative real-time PCR results for blaOXA−23 in AB1845 the heteroresistance of E. Coli and S. Typhimurium was due
and AB2092 (∗ student t-test p < 0.05). to the amplification of pmrD gene which encoded a protein
modifying lipid A. Moreover, the heteroresistance phenotype
is associated with different copy numbers of the pmrD gene
(Hjort et al., 2016). Numerous studies have reported gene
target %T>MIC of β-lactam antibiotics was 40–70% (Drusano, duplication and amplification related to bacterial resistance to
2004); however, there was no published target of sulbactam antibiotics in vitro (Bertini et al., 2007). During the macrolide
because of a lack of pharmacodynamic data. In our present treatment of a Streptococcus pneumoniae infection, the bacterium
dosage regimen (3 g q8h, infusion for 1 h), the target was developed resistance due to an 18 bp duplication in the rplV
100% of cefoperazone and 34.5% of sulbactam for AB1845. gene, leading to the treatment failure. The duplication of
Cefoperazone clearly reached its target, whereas there were no rplV gene led to the blocking of macrolide binding site on
criteria for sulbactam. In a study of PK/PD simulation for ribosome (Musher et al., 2002). Another example of gene
sulbactam in healthy volunteers, in order for A. baumannii amplification in bacterial isolates from human patients involves
with an MIC of 8 mg/L to achieve the target of 40%, the the Streptococcus agalactiae, a leading cause of neonatal
sulbactam had to be administered as a 4-h infusion of 3 g q8h infection. The amplification of a four-fold tandemly amplified
(Jaruratanasirikul et al., 2013). It has even been suggested that 13.5-kbp region and a 92 kbp duplication conferred drug
the daily dose of sulbactam can be administered up to 6 g for resistance to both sulfonamide and trimethoprim (Brochet et al.,
A. baumannii infection (Argyres, 2010) to achieve enhanced 2008).
efficacy. A comparison of these data revealed that sulbactam
In this study, the isolates developed resistance to
should be administered at a much higher dose or prolonged
cefoperazone/sulbactam as well as carbapenem antibiotics.
infusion time. A suboptimal dose of sulbactam could lead to
The whole-genome sequencing showed the amplified
the development of resistance during treatment. Additional
blaOXA−23 in the isolates is very likely the contribution
research to identify the PK/PD target of sulbactam specific to
to the resistance. It is rational to conferred resistance to
Acinetobacter is needed.
carbapenem antibiotics by the amplification of blaOXA−23 .
Whole-genome sequencing was further employed to
However, this is the first time to report the amplification of
investigate the mechanism of resistance from a molecular
blaOXA−23 results in cefoperazone/sulbactam combination
perspective. Comparison of the genome between AB1845
resistance. Further studies will be focused on collecting more
and AB2092 revealed no gene deletions or mutations (only
clinical isolates pairs of A. baumannii to support the mechanism
33 synonymous SNPs). However, the reads depth method
proposed.
showed six amplified genes on Tn2009, including blaOXA−23 .
The blaOXA−23 gene encodes the class D β-lactamase which
confers resistance to the last resort carbapenem antibiotics. The
OXA-23-producing A. baumannii is widely disseminated in AUTHOR CONTRIBUTIONS
multi-drug-resistant A. baumannii. Although the blaOXA−23
gene has been mainly identified on plasmids, its chromosomal XL designed the genomic sequencing experiments. XL and
location has also been reported (Zhou et al., 2011). The HZ performed the data analysis. XL and ZS conducted
transportable elements, Tn2006, Tn2007, Tn2008, and Tn2009, the qPCR experiments. YC conducted the pharmacokinetic
play a key role in the transfer of the blaOXA−23 gene to parameter calculation. LS extracted the genomic DNA for
different locations in one bacterium or to different isolates sequencing. MZ conducted the MIC test and the PFGE test.
(Corvec et al., 2007; Liu et al., 2015). Tn2008 and Tn2009 JS and JZ conceived of the study and devised the overall
have mostly been associated with the transfer of blaOXA−23 in study strategy. XL wrote the manuscript with input from all
China (Adams-Haduch et al., 2008; Zhou et al., 2011; Liu et al., authors.
Frontiers in Microbiology | www.frontiersin.org 7 August 2016 | Volume 7 | Article 1268
Liu et al. Cefoperazone/Sulbactam Resistance Development In vivo
ACKNOWLEDGMENT SUPPLEMENTARY MATERIAL
This research is supported by the National Natural The Supplementary Material for this article can be found
Science Foundation of China (Grant No. 8150130235 and online at: http://journal.frontiersin.org/article/10.3389/fmicb.
81373493). 2016.01268
REFERENCES Gao, C., Tong, J., Yu, K., Sun, Z., An, R., and Du, Z. (2016). Pharmacokinetics
of cefoperazone/sulbactam in critically ill patients receiving continuous
Abdulaziz, M. H., Lipman, J., Mouton, J. W., Hope, W. W., and Roberts, J. A. venovenous hemofiltration. Eur. J. Clin. Pharmacol. 72, 823–830. doi:
(2015). Applying pharmacokinetic/pharmacodynamic principles in critically 10.1007/s00228-016-2045-x
ill patients: optimizing efficacy and reducing resistance development. Semin. Guindon, S., and Gascuel, O. (2003). A simple, fast, and accurate algorithm to
Respir. Crit. Care Med. 36, 136–153. doi: 10.1055/s-0034-1398490 estimate large phylogenies by maximum likelihood. Syst. Biol. 52, 696–704. doi:
Adams-Haduch, J. M., Paterson, D. L., Sidjabat, H. E., Pasculle, A. W., 10.1080/10635150390235520
Potoski, B. A., Muto, C. A., et al. (2008). Genetic basis of multidrug Guo, F.-B., and Zhang, C.-T. (2006). ZCURVE_V: a new self-training system
resistance in Acinetobacter baumannii clinical isolates at a tertiary medical for recognizing protein-coding genes in viral and phage genomes. BMC
center in Pennsylvania. Antimicrob. Agents Chemother. 52, 3837–3843. doi: Bioinformatics 10:9. doi: 10.1186/1471-2105-7-9
10.1128/aac.00570-08 Hjort, K., Nicoloff, H., and Andersson, D. I. (2016). Unstable tandem
Argyres, M. I. (2010). Hospital-acquired infections due to gram-negative bacteria. gene amplification generates heteroresistance (variation in resistance within
New Engl. J. Med. 363, 1483–1483. a population) to colistin in Salmonella enterica. Mol. Microbiol. doi:
Asín-Prieto, E., Rodríguez-Gascón, A., and Isla, A. (2015). Applications of the 10.1111/mmi.13459 [Epub ahead of print].
pharmacokinetic/pharmacodynamic (PK/PD) analysis of antimicrobial agents. Holt, K. E., Wertheim, H., Zadoks, R. N., Baker, S., Whitehouse, C. A.,
J. Infect. Chemother. 21, 319–329. doi: 10.1016/j.jiac.2015.02.001 Dance, D., et al. (2015). Genomic analysis of diversity, population structure,
Bertini, A., Poirel, L., Bernabeu, S., Fortini, D., Villa, L., Nordmann, P., et al. (2007). virulence, and antimicrobial resistance in Klebsiella pneumoniae, an urgent
Multicopy blaOXA-58 gene as a source of high-level resistance to carbapenems threat to public health. Proc. Natl. Acad. Sci. U.S.A. 112, E3574–E3581. doi:
in Acinetobacter baumannii. Antimicrob. Agents Chemother. 51, 2324–2328. doi: 10.1073/pnas.1501049112
10.1128/AAC.01502-06 Hornsey, M., Loman, N., Wareham, D. W., Ellington, M. J., Pallen, M. J., Turton,
Boscia, J. A., Korzeniowski, O. M., Snepar, R., Kobasa, W. D., Levison, M. E., J. F., et al. (2011). Whole-genome comparison of two Acinetobacter baumannii
and Kaye, D. (1983). Cefoperazone pharmacokinetics in normal subjects isolates from a single patient, where resistance developed during tigecycline
and patients with cirrhosis. Antimicrob. Agents Chemother. 23, 385–389. doi: therapy. J. Antimicrob. Chemother. 66, 1499–1503. doi: 10.1093/jac/dkr168
10.1128/AAC.23.3.385 Hu, F. P., Guo, Y., Zhu, D. M., Wang, F., Jiang, X. F., Xu, Y. C., et al.
Brochet, M., Couve, E., Zouine, M., Poyart, C., and Glaser, P. (2008). A naturally (2016). Resistance trends among clinical isolates in China reported from
occurring gene amplification leading to sulfonamide and trimethoprim CHINET surveillance of bacterial resistance, 2005-2014. Clin. Microbiol. Infect.
resistance in Streptococcus agalactiae. J. Bacteriol. 190, 672–680. doi: 22(Suppl. 1), S9–S14. doi: 10.1016/j.cmi.2016.01.001
10.1128/jb.01357-07 Iyer, L. M., Leipe, D. D., Koonin, E. V., and Aravind, L. (2004). Evolutionary history
Bush, K. (2013). The ABCD’s of β-lactamase nomenclature. J. Infect. Chemother. and higher order classification of AAA+ ATPases. J. Struct. Biol. 146, 11–31.
19, 549–559. doi: 10.1007/s10156-013-0640-7 doi: 10.1016/j.jsb.2003.10.010
Cantsilieris, S., Baird, P. N., and White, S. J. (2012). Molecular methods for Jaruratanasirikul, S., Wongpoowarak, W., Aeinlang, N., and Jullangkoon, M.
genotyping complex copy number polymorphisms. Genomics 101, 86–93. doi: (2013). Pharmacodynamics modeling to optimize dosage regimens
10.1016/j.ygeno.2012.10.004 of sulbactam. Antimicrob. Agents Chemother. 57, 3441–3444. doi:
Cheah, S. E., Johnson, M. D., Zhu, Y., Tsuji, B. T., Forrest, A., Bulitta, J. B., et al. 10.1128/AAC.00342-13
(2016). Polymyxin resistance in Acinetobacter baumannii: genetic mutations Johnson, E. R., and Mckay, D. B. (1999). Crystallographic structure of the amino
and transcriptomic changes in response to clinically relevant dosage regimens. terminal domain of yeast initiation factor 4A, a representative DEAD-box RNA
Sci. Rep. 6, 26233. doi: 10.1038/srep26233 helicase. RNA 5, 1526–1534. doi: 10.1017/S1355838299991410
Chen, Y.-C., Zhou, Y.-J., Zhang, J., Wu, J.-F., Guo, B.-N., Wu, X.-J., Kanehisa, M., Sato, Y., Kawashima, M., Furumichi, M., and Tanabe, M. (2016).
et al. (2015). “Population pharmacokinetics and pharmacodynamics of KEGG as a reference resource for gene and protein annotation. Nucleic Acids
cefoperazone/sulbactam (2:1) in adult patients with hospital-acquired Res. 44, D457–D462. doi: 10.1093/nar/gkv1070
pneumoniae,” in Proceedings of the Interscience Conference of Antimicrobial Langmead, B., and Salzberg, S. L. (2012). Fast gapped-read alignment with
Agents and Chemotherapy, San Diego, CA. Bowtie 2. Nat. Methods 9, 357–359. doi: 10.1038/nmeth.1923
Choi, J. Y., Kim, C. O., Park, Y. S., Yoon, H. J., Shin, S. Y., Kim, Y. K., et al. (2006). Li, H., Handsaker, B., Wysoker, A., Fennell, T., Ruan, J., Homer, N., et al. (2009).
Comparison of efficacy of cefoperazone/sulbactam and imipenem/cilastatin The Sequence Alignment/Map format and SAMtools. Bioinformatics 25, 2078–
for treatment of Acinetobacter bacteremia. Yonsei Med. J. 47, 63–69. doi: 2079. doi: 10.1093/bioinformatics/btp352
10.3349/ymj.2006.47.1.63 Lips, M., Siller, M., Strojil, J., Urbanek, K., Balik, M., and Suchankova, H.
Cooper, T. W., Pass, S. E., Brouse, S. D., and Hall, R. G. I. I. (2011). Can (2014). Pharmacokinetics of imipenem in critically ill patients during empirical
pharmacokinetic and pharmacodynamic principles be applied to the treatment treatment of nosocomial pneumonia: a comparison of 0.5-h and 3-h infusions.
of multidrug-resistant Acinetobacter? Ann. Pharmacother. 45, 229–240. doi: Int. J. Antimicrob. Agents 44, 358–362. doi: 10.1016/j.ijantimicag.2014.05.011
10.1345/aph.1P187 Liu, L. L., Ji, S. J., Ruan, Z., Fu, Y., Fu, Y. Q., Wang, Y. F., et al. (2015). Dissemination
Corvec, S., Poirel, L., Naas, T., Drugeon, H., and Nordmann, P. (2007). Genetics of blaOXA-23 in Acinetobacter spp. in China: main roles of conjugative plasmid
and expression of the carbapenem-hydrolyzing oxacillinase gene blaOXA-23 in pAZJ221 and transposon Tn2009. Antimicrob. Agents Chemother. 59, 1998–
Acinetobacter baumannii. Antimicrob. Agents Chemother. 51, 1530–1533. doi: 2005. doi: 10.1128/AAC.04574-14
10.1128/AAC.01132-06 Mardis, E. R. (2008). The impact of next-generation sequencing technology on
Delcher, A. L., Bratke, K. A., Powers, E. C., and Salzberg, S. L. (2007). Identifying genetics. Trends Genet. 24, 133–141. doi: 10.1016/j.tig.2007.12.007
bacterial genes and endosymbiont DNA with Glimmer. Bioinformatics 23, Martinez, M. N., Papich, M. G., and Drusano, G. L. (2012). Dosing regimen
673–679. doi: 10.1093/bioinformatics/btm009 matters: the importance of early intervention and rapid attainment of the
Drusano, G. L. (2004). Antimicrobial pharmacodynamics: critical interactions of pharmacokinetic/pharmacodynamic target. Antimicrob. Agents Chemother. 56,
‘bug and drug.’ Nat. Rev. Microbiol. 2, 289–300. doi: 10.1038/nrmicro862 2795–2805. doi: 10.1128/AAC.05360-11
Frontiers in Microbiology | www.frontiersin.org 8 August 2016 | Volume 7 | Article 1268
Liu et al. Cefoperazone/Sulbactam Resistance Development In vivo
McGann, P., Courvalin, P., Snesrud, E., Clifford, R. J., Yoon, E.-J., Onmus- in Escherichia coli. Proc. Natl. Acad. Sci. U.S.A. 108, 1484–1489. doi:
Leone, F., et al. (2014). Amplification of aminoglycoside resistance gene 10.1073/pnas.1012108108
aphA1 in Acinetobacter baumannii results in tobramycin therapy failure. MBio Sun, S., Berg, O. G., Roth, J. R., and Andersson, D. I. (2009). Contribution of
5:e00915-14. doi: 10.1128/mBio.00915-14 gene amplification to evolution of increased antibiotic resistance in Salmonella
Monogue, M. L., Kuti, J. L., and Nicolau, D. P. (2015). Optimizing antibiotic dosing typhimurium. Genetics 182, 1183–1195. doi: 10.1534/genetics.109.103028
strategies for the treatment of gram-negative infections in the era of resistance. Sy, S. K., Zhuang, L., and Derendorf, H. (2015). Pharmacokinetics and
Expert Rev. Clin. Pharmacol. 9, 459–476. doi: 10.1586/17512433.2016.1133286 pharmacodynamics in antibiotic dose optimization. Expert Opin. Drug Metab.
Mugnier, P. D., Poirel, L., and Nordmann, P. (2009). Functional analysis of Toxicol. 12, 94–114.
insertion sequence ISAba1, responsible for genomic plasticity of Acinetobacter Turton, J. F., Ward, M. E., Woodford, N., Kaufmann, M. E., Pike, R., Livermore,
baumannii. J. Bacteriol. 191, 2414–2418. doi: 10.1128/JB.01258-08 D. M., et al. (2006). The role of ISAba1 in expression of OXA carbapenemase
Musher, D. M., Dowell, M. E., Shortridge, V. D., Flamm, R. K., Jorgensen, J. H., genes in Acinetobacter baumannii. FEMS Microbiol. Lett. 258, 72–77. doi:
Le Magueres, P., et al. (2002). Emergence of macrolide resistance during 10.1111/j.1574-6968.2006.00195.x
treatment of pneumococcal pneumonia. N. Engl. J. Med. 346, 630–631. doi: Waltner-Toews, R. I., Paterson, D. L., Qureshi, Z. A., Sidjabat, H. E., Adams-
10.1056/nejm200202213460820 Haduch, J. M., Shutt, K. A., et al. (2011). Clinical characteristics of
Mwangi, M. M., Wu, S. W., Zhou, Y., Sieradzki, K., de Lencastre, H., Richardson, P., bloodstream infections due to ampicillin-sulbactam-resistant, non-extended-
et al. (2007). Tracking the in vivo evolution of multidrug resistance in spectrum-beta-lactamase-producing Escherichia coli and the role of TEM-
Staphylococcus aureus by whole-genome sequencing. Proc. Natl. Acad. Sci. 1 hyperproduction. Antimicrob. Agents Chemother. 55, 495–501. doi:
U.S.A. 104, 9451–9456. doi: 10.1073/pnas.0609839104 10.1128/aac.00797-10
Pascale, G. D., and Wright, G. D. (2010). Antibiotic resistance by enzyme Wang, Q., Wu, Y., Chen, B., and Zhou, J. (2015). Drug concentrations in the serum
inactivation: from mechanisms to solutions. Chembiochem 11, 1325–1334. doi: and cerebrospinal fluid of patients treated with cefoperazone/sulbactam after
10.1002/cbic.201000067 craniotomy. BMC Anesthesiol. 15:33. doi: 10.1186/s12871-015-0012-1
Peleg, A. Y., Seifert, H., and Paterson, D. L. (2008). Acinetobacter baumannii: Wright, M. S., Haft, D. H., Harkins, D. M., Perez, F., Hujer, K. M., Bajaksouzian, S.,
emergence of a successful pathogen. Clin. Microbiol. Rev. 21, 538–582. doi: et al. (2014). New insights into dissemination and variation of the health care-
10.1128/cmr.00058-07 associated pathogen Acinetobacter baumannii from genomic analysis. MBio
Penwell, W. F., Shapiro, A. B., Giacobbe, R. A., Gu, R. F., Gao, N., Thresher, J., et al. 5:e00963-13. doi: 10.1128/mBio.00963-13
(2015). Molecular mechanisms of sulbactam antibacterial activity and resistance Wright, M. S., Iovleva, A., Jacobs, M. R., Bonomo, R. A., and Adams, M. D. (2016).
determinants in Acinetobacter baumannii. Antimicrob. Agents Chemother. 59, Genome dynamics of multidrug-resistant Acinetobacter baumannii during
1680–1689. doi: 10.1128/aac.04808-14 infection and treatment. Genome Med. 8, 26. doi: 10.1186/s13073-016-0279-y
Perez, F., Hujer, A. M., Hujer, K. M., Decker, B. K., Rather, P. N., and Xia, J., Zhang, D., Xu, Y., Gong, M., Zhou, Y., and Fang, X. (2014).
Bonomo, R. A. (2007). Global challenge of multidrug-resistant Acinetobacter A retrospective analysis of carbapenem-resistant Acinetobacter
baumannii. Antimicrob. Agents Chemother. 51, 3471–3484. doi: 10.1128/aac. baumannii-mediated nosocomial pneumonia and the in vitro therapeutic
01464-06 benefit of cefoperazone/sulbactam. Int. J. Infect. Dis. 23, 90–93. doi:
Redon, R., Ishikawa, S., Fitch, K. R., Feuk, L., Perry, G. H., Andrews, T. D., et al. 10.1016/j.ijid.2014.01.017
(2006). Global variation in copy number in the human genome. Nature 444, Xin, X., Jian, L., Xia, X., Jia, B., Huang, W., Li, C., et al. (2013). A multicentre
444–454. doi: 10.1038/nature05329 clinical study on the injection of ceftriaxone/sulbactam compared with
Reitberg, D. P., Whall, T. J., Chung, M., Blickens, D., Swarz, H., and Arnold, J. cefoperazone/sulbactam in the treatment of respiratory and urinary tract
(1988). Multiple-dose pharmacokinetics and toleration of intravenously infections. Ann. Clin. Microbiol. Antimicrob. 12, 38. doi: 10.1186/1476-0711-
administered cefoperazone and sulbactam when given as single agents 12-38
or in combination. Antimicrob. Agents Chemother. 32, 42–46. doi: Zerbino, D. R., and Birney, E. (2008). Velvet: algorithms for de novo short
10.1128/AAC.32.1.42 read assembly using de Bruijn graphs. Genome Res. 18, 821–829. doi:
Rice, L. B., Carias, L. L., Etter, L., and Shlaes, D. M. (1993). Resistance 10.1101/gr.074492.107
to cefoperazone-sulbactam in Klebsiella pneumoniae: evidence for Zhou, H., Zhang, T., Yu, D., Pi, B., Yang, Q., Zhou, J., et al. (2011). Genomic analysis
enhanced resistance resulting from the coexistence of two different of the multidrug-resistant Acinetobacter baumannii strain MDR-ZJ06 widely
resistance mechanisms. Antimicrob. Agents Chemother. 37, 1061–1064. spread in China. Antimicrob. Agents Chemother. 55, 4506–4512.
doi: 10.1128/AAC.37.5.1061 Zhou, Y., Zhang, J., Guo, B., Yu, J., Shi, Y., Wang, M., et al. (2010).
Sandegren, L., and Andersson, D. I. (2009). Bacterial gene amplification: Liquid chromatography/tandem mass spectrometry assay for the simultaneous
implications for the evolution of antibiotic resistance. Nat. Rev. Microbiol. 7, determination of cefoperazone and sulbactam in plasma and its application to a
578–588. doi: 10.1038/nrmicro2174 pharmacokinetic study. J. Chromatogr. B Analyt. Technol. Biomed. Life Sci. 878,
Schmittgen, T. D., and Livak, K. J. (2008). Analyzing real-time PCR data 3119–3124. doi: 10.1016/j.jchromb.2010.09.021
by the comparative C(T) method. Nat. Protoc. 3, 1101–1108. doi:
10.1038/nprot.2008.73 Conflict of Interest Statement: The authors declare that the research was
Sipahi, O. R., Arda, B., Nazli-Zeka, A., Pullukcu, H., Tasbakan, M., Yamazhan, T., conducted in the absence of any commercial or financial relationships that could
et al. (2014). Piperacillin/tazobactam vs. cefoperazone/sulbactam in adult be construed as a potential conflict of interest.
low-risk febrile neutropenia cases. Int. J. Clin. Pract. 68, 230–235. doi:
10.1111/ijcp.12279 Copyright © 2016 Liu, Zheng, Zhang, Shen, Zhao, Chen, Sun, Shi and Zhang.
Snitkin, E. S., Zelazny, A. M., Montero, C. I., Stock, F., Mijares, L., Murray, P. R., This is an open-access article distributed under the terms of the Creative Commons
et al. (2011). Genome-wide recombination drives diversification of epidemic Attribution License (CC BY). The use, distribution or reproduction in other forums
strains of Acinetobacter baumannii. Proc. Natl. Acad. Sci. U.S.A. 108, 13758– is permitted, provided the original author(s) or licensor are credited and that the
13763. doi: 10.1073/pnas.1104404108 original publication in this journal is cited, in accordance with accepted academic
Soo, V. W., Hanson-Manful, P., and Patrick, W. M. (2011). Artificial gene practice. No use, distribution or reproduction is permitted which does not comply
amplification reveals an abundance of promiscuous resistance determinants with these terms.
Frontiers in Microbiology | www.frontiersin.org 9 August 2016 | Volume 7 | Article 1268
You might also like
- Central Dogma of Molecular BiologyDocument30 pagesCentral Dogma of Molecular BiologyAlthea Mandal100% (1)
- BLANK Biology EOC - Review - Packet by StandardDocument14 pagesBLANK Biology EOC - Review - Packet by StandardmspallardNo ratings yet
- Modified P.aerugenosaDocument21 pagesModified P.aerugenosaranjitsinghNo ratings yet
- Modified P.aerugenosaDocument21 pagesModified P.aerugenosaranjitsinghNo ratings yet
- DISSEMINATIONDocument8 pagesDISSEMINATIONAbbireddy SairamNo ratings yet
- 2JMAA-8-12 - 2015sharma PDFDocument5 pages2JMAA-8-12 - 2015sharma PDFAMBS ABMS JMAANo ratings yet
- NaraawadeeniamhundkkDocument6 pagesNaraawadeeniamhundkkDevanti EkaNo ratings yet
- Paterson Et Al., 2021Document3 pagesPaterson Et Al., 2021Caio Bonfim MottaNo ratings yet
- Trabajo 2Document7 pagesTrabajo 2Juan Martín VargasNo ratings yet
- Genetic and Antibiotic Susceptibility Profiles of Drug - Resistant Acinetobacter Baumannii From Various Parts of LebanonDocument9 pagesGenetic and Antibiotic Susceptibility Profiles of Drug - Resistant Acinetobacter Baumannii From Various Parts of LebanonInternational Medical PublisherNo ratings yet
- Trabajo 2Document7 pagesTrabajo 2Juan Martín VargasNo ratings yet
- Fphar 13 856792Document9 pagesFphar 13 856792Nur Fadhilah SyahidNo ratings yet
- First Detection of Bla TEM, SHV and CTX-M AmongDocument7 pagesFirst Detection of Bla TEM, SHV and CTX-M AmongHamidou OuedraogoNo ratings yet
- Antibiotic Impregnated Tablets For Screening Esbl and Ampc Beta LactamasesDocument4 pagesAntibiotic Impregnated Tablets For Screening Esbl and Ampc Beta LactamasesIOSR Journal of PharmacyNo ratings yet
- Current Senerio of Antimicrobial Resistance Patterns of Pseudomonas Aeruginosa Clinical Isolates in East Uttar Pradesh, IndiaDocument4 pagesCurrent Senerio of Antimicrobial Resistance Patterns of Pseudomonas Aeruginosa Clinical Isolates in East Uttar Pradesh, IndiaPraveen GautamNo ratings yet
- Evolution of Carbapenem-Resistant Acinetobacter Baumannii Revealed Through Whole-Genome Sequencing and Comparative Genomic AnalysisDocument9 pagesEvolution of Carbapenem-Resistant Acinetobacter Baumannii Revealed Through Whole-Genome Sequencing and Comparative Genomic AnalysisKlauss Castillo PardoNo ratings yet
- Bioorganic & Medicinal Chemistry Letters: ArticleinfoDocument8 pagesBioorganic & Medicinal Chemistry Letters: ArticleinfoMehari AsratNo ratings yet
- Xin 2016, Pfge&MlstDocument8 pagesXin 2016, Pfge&MlstSarah KKCNo ratings yet
- Antibiotic Resistance Pattern in Pseudomonas Aeruginosa Species Isolated at A Tertiary Care Hospital, AhmadabadDocument4 pagesAntibiotic Resistance Pattern in Pseudomonas Aeruginosa Species Isolated at A Tertiary Care Hospital, AhmadabadDrashua AshuaNo ratings yet
- Molecular Characterisation of An Acinetobacter Baumannii OutbreakDocument9 pagesMolecular Characterisation of An Acinetobacter Baumannii OutbreakRamón RicardoNo ratings yet
- Detection OF IN Carbapenem-Resistant Isolated From Clinical Samples in Wasit Province HospitalsDocument15 pagesDetection OF IN Carbapenem-Resistant Isolated From Clinical Samples in Wasit Province HospitalsZainab SattarNo ratings yet
- Antibiotic Susceptibility Profile and Prevalence of AmpC Among Clinical Bacterial Isolates Obtained From Northwestern NigeriaDocument9 pagesAntibiotic Susceptibility Profile and Prevalence of AmpC Among Clinical Bacterial Isolates Obtained From Northwestern NigeriaUMYU Journal of Microbiology Research (UJMR)No ratings yet
- Niños Clin - Infect - Dis - 2014 - May - 15 - 58 (10) - 1439-48Document10 pagesNiños Clin - Infect - Dis - 2014 - May - 15 - 58 (10) - 1439-48mariangelNo ratings yet
- Ofac 034Document6 pagesOfac 034Imene FlNo ratings yet
- Klebsiella Pneumoniae: Trends in The Hospital and Community SettingsDocument5 pagesKlebsiella Pneumoniae: Trends in The Hospital and Community SettingskhanfahsNo ratings yet
- Molecular ImmunologyDocument10 pagesMolecular ImmunologyDiego TulcanNo ratings yet
- CeftolozaneTazobactam A New Option in The TreatmenDocument7 pagesCeftolozaneTazobactam A New Option in The TreatmenAisyah RohieNo ratings yet
- Annrheumdis 2019 Eular.6888Document1 pageAnnrheumdis 2019 Eular.6888muamarrayNo ratings yet
- Isolation of Carbapenem-Resistant Pseudomonas Spp. From FoodDocument6 pagesIsolation of Carbapenem-Resistant Pseudomonas Spp. From FoodValentina RondonNo ratings yet
- Antimicrobial Resistance and Molecular Characterization of Gene Cassettes From Class 1 Integrons in Pseudomonas Aeruginosa S PDFDocument7 pagesAntimicrobial Resistance and Molecular Characterization of Gene Cassettes From Class 1 Integrons in Pseudomonas Aeruginosa S PDFValentina RondonNo ratings yet
- Risk Factors and The Resistance Mechanisms Involved in Pseudomonas Aeruginosa Mutation in Critically Ill PatientsDocument9 pagesRisk Factors and The Resistance Mechanisms Involved in Pseudomonas Aeruginosa Mutation in Critically Ill PatientsElsiana LaurenciaNo ratings yet
- Correspondence: Whole-Genome Sequencing For The Diagnosis of Drug-Resistant TuberculosisDocument2 pagesCorrespondence: Whole-Genome Sequencing For The Diagnosis of Drug-Resistant TuberculosisAdriani HartantoNo ratings yet
- BBRC Vol 14 No 04 2021-69Document7 pagesBBRC Vol 14 No 04 2021-69Dr Sharique AliNo ratings yet
- Jiw 632Document10 pagesJiw 632Robert StryjakNo ratings yet
- RAPD AcinetoDocument8 pagesRAPD AcinetokiflyNo ratings yet
- Prevalence of Class 1 Integron Among Multidrug-Resistant Acinetobacter Baumannii in Tabriz, Northwest of IranDocument4 pagesPrevalence of Class 1 Integron Among Multidrug-Resistant Acinetobacter Baumannii in Tabriz, Northwest of IranDrashua AshuaNo ratings yet
- Antibiotic Resistancein Clinical Isolatesof PseudomonasDocument7 pagesAntibiotic Resistancein Clinical Isolatesof PseudomonasElsiana LaurenciaNo ratings yet
- Prevalence of Extended-Spectrum Beta-Lactamases Among Isolated Isolated From Blood Culture in A Tertiary Care HospitalDocument4 pagesPrevalence of Extended-Spectrum Beta-Lactamases Among Isolated Isolated From Blood Culture in A Tertiary Care HospitalMohammad K AlshomraniNo ratings yet
- (M299) RL4Document9 pages(M299) RL4Jessa Louise TurredaNo ratings yet
- Uji Resistensi Antibiotik Terhadap Kultur Bakteri Staphylococcus Aureus PADA RUANG Intensive Care Unit (ICU) RUMAH Sakit Y Kota JambiDocument7 pagesUji Resistensi Antibiotik Terhadap Kultur Bakteri Staphylococcus Aureus PADA RUANG Intensive Care Unit (ICU) RUMAH Sakit Y Kota JambiObrilian Waisman MNo ratings yet
- Synergistic Effect of Artocarpin On Antibacterial Activity of Some Antibiotics Against Methicillin Resistant Staphylococcus Aureus PseudomonasDocument7 pagesSynergistic Effect of Artocarpin On Antibacterial Activity of Some Antibiotics Against Methicillin Resistant Staphylococcus Aureus PseudomonasiswanNo ratings yet
- Efficacy of Practised Screening Methods For Detection of Cephalosporin-Resistant EnterobacteriaceaeDocument4 pagesEfficacy of Practised Screening Methods For Detection of Cephalosporin-Resistant EnterobacteriaceaeCoquelicot Éphémère ÉphémèreNo ratings yet
- Development and Evaluation of A Loop-Mediated Isothermal Ampliication (LAMP) Assay For Rapid Detection of ActinobacillusDocument4 pagesDevelopment and Evaluation of A Loop-Mediated Isothermal Ampliication (LAMP) Assay For Rapid Detection of ActinobacillusLuis Ernesto Mena ZapataNo ratings yet
- Background Changing Patterns of Neonatal Fungal Sepsis in A Developing CountryDocument5 pagesBackground Changing Patterns of Neonatal Fungal Sepsis in A Developing CountryNada AhmedNo ratings yet
- Discussion: Mac Faddin, 1976Document8 pagesDiscussion: Mac Faddin, 1976Salma MohamedNo ratings yet
- (M299) RL3Document11 pages(M299) RL3Jessa Louise TurredaNo ratings yet
- 11 Richa EtalDocument6 pages11 Richa EtaleditorijmrhsNo ratings yet
- BBRC Vol 14 No 04 2021-43Document6 pagesBBRC Vol 14 No 04 2021-43Dr Sharique AliNo ratings yet
- Oral Cephalosporin and B-Lactamase Inhibitor Combinations For ESBL-producing Enterobacteriaceae Urinary Tract InfectionsDocument13 pagesOral Cephalosporin and B-Lactamase Inhibitor Combinations For ESBL-producing Enterobacteriaceae Urinary Tract InfectionsJosaphat NuñezNo ratings yet
- Performance and Feasibility of Using Both Stool Culture and Nested PCR For Improved Detection of Typhoid Fever in Buea Health District, South West CameroonDocument9 pagesPerformance and Feasibility of Using Both Stool Culture and Nested PCR For Improved Detection of Typhoid Fever in Buea Health District, South West CameroonInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Ultimos AntimicrobianosDocument3 pagesUltimos Antimicrobianosmargarita rodriguezNo ratings yet
- 353 jmm036939Document8 pages353 jmm036939Andy SetiawanNo ratings yet
- Rood 2017Document19 pagesRood 2017Estefany HurtadoNo ratings yet
- Ceftobiprole, A Broad-Spectrum Cephalosporin With Activity Against Methicillin-Resistant Staphylococcus Aureus (MRSA)Document7 pagesCeftobiprole, A Broad-Spectrum Cephalosporin With Activity Against Methicillin-Resistant Staphylococcus Aureus (MRSA)Esther TobingNo ratings yet
- Atbs Cocos Pos MDRDocument24 pagesAtbs Cocos Pos MDRvascoNo ratings yet
- BELGIA NDM J. Antimicrob. Chemother. 2012 Bogaerts 1552 3Document2 pagesBELGIA NDM J. Antimicrob. Chemother. 2012 Bogaerts 1552 3Mihaela RoxanaNo ratings yet
- Emergence of Plasmid-Mediated Quinolone-Resistant SalmonellaTyphi Clinical Isolates From Punjab, PakistanDocument1 pageEmergence of Plasmid-Mediated Quinolone-Resistant SalmonellaTyphi Clinical Isolates From Punjab, Pakistanali zohaibNo ratings yet
- Cefoperazone Sulbactam en RNDocument4 pagesCefoperazone Sulbactam en RNchieneralbaNo ratings yet
- An Insight Into The Emergence of Acinetobacter Baumannii As An Oro - 2018 - HelDocument18 pagesAn Insight Into The Emergence of Acinetobacter Baumannii As An Oro - 2018 - HelKhánh HoàngNo ratings yet
- Serodiagnosis of Bartonella Bacilliformis Infection by Indirect Fluorescence Antibody Assay: Test Development and Application To A Population in An Area of Bartonellosis EndemicityDocument3 pagesSerodiagnosis of Bartonella Bacilliformis Infection by Indirect Fluorescence Antibody Assay: Test Development and Application To A Population in An Area of Bartonellosis EndemicitySOFIA ESTHER ROMERO MEDEROSNo ratings yet
- 2017 Article 141 Part1Document5 pages2017 Article 141 Part1Karina MonasaNo ratings yet
- Sabtuan Wonogiri 5 MowDocument3 pagesSabtuan Wonogiri 5 Mowgalih widodoNo ratings yet
- Koreksi Sabtuan Wonogiri 2Document8 pagesKoreksi Sabtuan Wonogiri 2galih widodoNo ratings yet
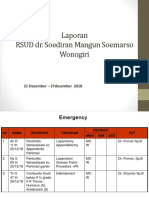
- Laporan RSUD Dr. Soediran Mangun Soemarso Wonogiri: 21 Desember - 27desember 2018Document6 pagesLaporan RSUD Dr. Soediran Mangun Soemarso Wonogiri: 21 Desember - 27desember 2018galih widodoNo ratings yet
- 2015 Article 12 PDFDocument9 pages2015 Article 12 PDFgalih widodoNo ratings yet
- Case DR SADocument16 pagesCase DR SAgalih widodoNo ratings yet
- Sabtuan Onko 19 - 25 Jan 18Document7 pagesSabtuan Onko 19 - 25 Jan 18galih widodoNo ratings yet
- Clinical Case Advanced Breast CancerDocument10 pagesClinical Case Advanced Breast Cancergalih widodoNo ratings yet
- Bedah Anak: Peta Pasien Sabtu 31 Oktober 2015 Ayt/Dna/Pur/Imp/FerDocument2 pagesBedah Anak: Peta Pasien Sabtu 31 Oktober 2015 Ayt/Dna/Pur/Imp/Fergalih widodoNo ratings yet
- Clinical Case Advanced Breast CancerDocument8 pagesClinical Case Advanced Breast Cancergalih widodoNo ratings yet
- Fracture of Shaft Tibia FibulaDocument26 pagesFracture of Shaft Tibia Fibulagalih widodoNo ratings yet
- Burns ChapterDocument8 pagesBurns Chaptergalih widodoNo ratings yet
- Laporan Kegiatan IBS: Bagian Bedah RSUD Dr. MoewardiDocument7 pagesLaporan Kegiatan IBS: Bagian Bedah RSUD Dr. Moewardigalih widodoNo ratings yet
- Bedah Anak: Peta Pasien Jum'At 30 Oktober 2015 Ayt/Dna/Pur/Imp/FerDocument2 pagesBedah Anak: Peta Pasien Jum'At 30 Oktober 2015 Ayt/Dna/Pur/Imp/Fergalih widodoNo ratings yet
- Bedah Anak: Peta Pasien Senin 2 November 2015 Galih/Ariya/Ond/Edr/Ayt/Map/Pur/Ben/Fer/VelDocument2 pagesBedah Anak: Peta Pasien Senin 2 November 2015 Galih/Ariya/Ond/Edr/Ayt/Map/Pur/Ben/Fer/Velgalih widodoNo ratings yet
- Clinical Case Advanced Breast CancerDocument8 pagesClinical Case Advanced Breast Cancergalih widodoNo ratings yet
- Overgranulation: A. Muhammad Reva A.MDocument21 pagesOvergranulation: A. Muhammad Reva A.Mgalih widodoNo ratings yet
- Clinical Case Advanced Breast CancerDocument8 pagesClinical Case Advanced Breast Cancergalih widodoNo ratings yet
- 29 September 2017 Bedah OnkologiDocument2 pages29 September 2017 Bedah Onkologigalih widodoNo ratings yet
- WHO-SEARO Snakebite Guidelines 2010Document162 pagesWHO-SEARO Snakebite Guidelines 2010Galantry Ahmad AzhariNo ratings yet
- 5638451Document6 pages5638451galih widodoNo ratings yet
- 5638451Document6 pages5638451galih widodoNo ratings yet
- Maping Plastik 4 April 2017Document2 pagesMaping Plastik 4 April 2017galih widodoNo ratings yet
- A New Surgical Treatment of Keloid Keloid Core ExcisionDocument7 pagesA New Surgical Treatment of Keloid Keloid Core Excisiongalih widodoNo ratings yet
- A New Surgical Treatment of Keloid Keloid Core ExcisionDocument7 pagesA New Surgical Treatment of Keloid Keloid Core Excisiongalih widodoNo ratings yet
- Mapping Onko 2 JuniDocument2 pagesMapping Onko 2 Junigalih widodoNo ratings yet
- 4transf MaizDocument13 pages4transf MaizIris MoralesNo ratings yet
- Linkage and Genetic Mapping EukaryotesDocument66 pagesLinkage and Genetic Mapping EukaryotesSITI BAZILAH BINTI BILAK KPM-GuruNo ratings yet
- Salmonella Enterica Salmonella EntericaDocument10 pagesSalmonella Enterica Salmonella EntericaBrasco KaramNo ratings yet
- Lesson 5 - Central Dogma of Molecular BiologyDocument33 pagesLesson 5 - Central Dogma of Molecular BiologySherwin YenogacioNo ratings yet
- Syllabus of Zoology (B.Sc. Ist Year) SESSION - 2011-12Document7 pagesSyllabus of Zoology (B.Sc. Ist Year) SESSION - 2011-12Anonymous 15awgX0NaNo ratings yet
- Leukocyte Adhesion Deficiency II Patients With A Dual Defect of TheDocument8 pagesLeukocyte Adhesion Deficiency II Patients With A Dual Defect of TheCosmin BarbosNo ratings yet
- Gene Therapy ReportDocument2 pagesGene Therapy ReportKaren Jane YapNo ratings yet
- Department of Molecular Biology. Covid 19 RTPCR With Home Collection Test Name Result Unit Bio. Ref. Range MethodDocument2 pagesDepartment of Molecular Biology. Covid 19 RTPCR With Home Collection Test Name Result Unit Bio. Ref. Range MethodGirija Prasad SwainNo ratings yet
- 218 ภัทรดนัย ธูปสุวรรณ 4Document1 page218 ภัทรดนัย ธูปสุวรรณ 4Mr. ACDCNo ratings yet
- UG022524 International GCSE in Human Biology 4HB0 For PrintDocument42 pagesUG022524 International GCSE in Human Biology 4HB0 For PrintHosni ShowikeNo ratings yet
- SSCT Xii Biology-Ms Term - 1Document4 pagesSSCT Xii Biology-Ms Term - 1TECHNIQUED review channelNo ratings yet
- Biology: Pearson Edexcel GCEDocument8 pagesBiology: Pearson Edexcel GCEDaniel ConwayNo ratings yet
- 12th STD Bio-Botany EM Practical NotesDocument12 pages12th STD Bio-Botany EM Practical NotesSanthosh 143No ratings yet
- Virus Replication StrategyDocument6 pagesVirus Replication StrategyShreyash Raj100% (1)
- Prac 12 Đội Tuyển Đã LàmDocument7 pagesPrac 12 Đội Tuyển Đã Làmminhngoc phamNo ratings yet
- Basic Cat GeneticsDocument12 pagesBasic Cat GeneticsFunda GençlerNo ratings yet
- 10 1111@zsc 12346Document14 pages10 1111@zsc 12346Anonymous VqDPRFNo ratings yet
- Activities To Develop Pre-TaskDocument6 pagesActivities To Develop Pre-Taskeduardo arenasNo ratings yet
- Biology 1A03 Exam ReviewDocument69 pagesBiology 1A03 Exam Review0xVi3tfireNo ratings yet
- Indian Forest Service Examination SyllabusDocument46 pagesIndian Forest Service Examination SyllabusamulrajvincentNo ratings yet
- Extranuclear Inheritance-3Document33 pagesExtranuclear Inheritance-3Tony BernardNo ratings yet
- Caiet BM MG Eng PDFDocument188 pagesCaiet BM MG Eng PDFИрина АндреевнаNo ratings yet
- BIO107 INTRO TO MolBioDocument17 pagesBIO107 INTRO TO MolBioLaline Magdale ZalzosNo ratings yet
- Biotechnological Strains of Komagataella (Pichia) PastorisDocument4 pagesBiotechnological Strains of Komagataella (Pichia) PastorisDavi MouraNo ratings yet
- © Lesson Plans Inc. 2007Document9 pages© Lesson Plans Inc. 2007Fatima Nur Faiza HandaNo ratings yet
- SIHAY - Plugged 2023 BIOLOGY QUIZ OLYMPIAD-2-26Document25 pagesSIHAY - Plugged 2023 BIOLOGY QUIZ OLYMPIAD-2-26LEANNE CLARISSE LOSANESNo ratings yet
- BioinformaticsProjects IntroductionDocument2 pagesBioinformaticsProjects IntroductionTheUnseenBeforeNo ratings yet
- MHC Chpt. 7Document21 pagesMHC Chpt. 7Julio MansoNo ratings yet