Professional Documents
Culture Documents
New England Journal Medicine: The of
Uploaded by
GhufranOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
New England Journal Medicine: The of
Uploaded by
GhufranCopyright:
Available Formats
new england
The
journal of medicine
established in 1812 june 26, 2014 vol. 370 no. 26
Atrial Fibrillation in Patients with Cryptogenic Stroke
David J. Gladstone, M.D., Ph.D., Melanie Spring, M.D., Paul Dorian, M.D., Val Panzov, M.D., Kevin E. Thorpe, M.Math.,
Judith Hall, M.Sc., Haris Vaid, B.Sc., Martin O’Donnell, M.B., Ph.D., Andreas Laupacis, M.D., Robert Côté, M.D.,
Mukul Sharma, M.D., John A. Blakely, M.D., Ashfaq Shuaib, M.D., Vladimir Hachinski, M.D., D.Sc.,
Shelagh B. Coutts, M.B., Ch.B., M.D., Demetrios J. Sahlas, M.D., Phil Teal, M.D., Samuel Yip, M.D., J. David Spence, M.D.,
Brian Buck, M.D., Steve Verreault, M.D., Leanne K. Casaubon, M.D., Andrew Penn, M.D., Daniel Selchen, M.D.,
Albert Jin, M.D., David Howse, M.D., Manu Mehdiratta, M.D., Karl Boyle, M.B., B.Ch., Richard Aviv, M.B., Ch.B.,
Moira K. Kapral, M.D., and Muhammad Mamdani, Pharm.D., M.P.H., for the EMBRACE Investigators and Coordinators*
A BS T R AC T
BACKGROUND
Atrial fibrillation is a leading preventable cause of recurrent stroke for which From the Division of Neurology (D.J.G.), De-
early detection and treatment are critical. However, paroxysmal atrial fibrillation partment of Medicine (D.J.G., P.D., A.L., M.S.,
J.A.B., L.K.C., D.S., M. Mehdiratta, K.B.,
is often asymptomatic and likely to go undetected and untreated in the routine M.K.K.), and Dalla Lana School of Public
care of patients with ischemic stroke or transient ischemic attack (TIA). Health (K.E.T.), University of Toronto, the Uni-
versity of Toronto Stroke Program (D.J.G.),
METHODS Division of Neurology, Department of Medi-
We randomly assigned 572 patients 55 years of age or older, without known cine, and Brain Sciences Program, Sunny-
atrial fibrillation, who had had a cryptogenic ischemic stroke or TIA within the brook Health Sciences Centre and Sunny-
brook Research Institute (D.J.G., R.A.), the
previous 6 months (cause undetermined after standard tests, including 24-hour Heart and Stroke Foundation Canadian Part-
electrocardiography [ECG]), to undergo additional noninvasive ambulatory ECG nership for Stroke Recovery (D.J.G.), and the
Applied Health Research Centre, Li Ka Shing
monitoring with either a 30-day event-triggered recorder (intervention group) or Knowledge Institute of St. Michael’s Hospital
a conventional 24-hour monitor (control group). The primary outcome was newly (V.P., K.E.T., J.H., H.V., A.L., M. Mamdani), To-
detected atrial fibrillation lasting 30 seconds or longer within 90 days after ran- ronto, McMaster University, Hamilton, ON
(M.S., D.J.S.), McGill University, Montreal
domization. Secondary outcomes included episodes of atrial fibrillation lasting (R.C.), University of Alberta, Edmonton (A.S.,
2.5 minutes or longer and anticoagulation status at 90 days. B.B.), Western University, London, ON (V.H.,
J.D.S.), Department of Clinical Neurosciences
RESULTS
and Radiology, Hotchkiss Brain Institute, Uni-
Atrial fibrillation lasting 30 seconds or longer was detected in 45 of 280 patients versity of Calgary, Calgary, AB (S.B.C.), Uni-
(16.1%) in the intervention group, as compared with 9 of 277 (3.2%) in the con- versity of British Columbia, Vancouver (P.T.,
S.Y.), Queen’s University, Kingston, ON (A.J.),
trol group (absolute difference, 12.9 percentage points; 95% confidence interval Thunder Bay Regional Health Sciences Centre,
[CI], 8.0 to 17.6; P<0.001; number needed to screen, 8). Atrial fibrillation lasting Thunder Bay, ON (D.H.), Université Laval,
2.5 minutes or longer was present in 28 of 284 patients (9.9%) in the intervention Quebec City (S.V.), and Vancouver Island
Health Research Centre, Victoria, BC (A.P.)
group, as compared with 7 of 277 (2.5%) in the control group (absolute differ- — all in Canada; and the National University
ence, 7.4 percentage points; 95% CI, 3.4 to 11.3; P<0.001). By 90 days, oral anti- of Ireland, Galway (M.O.). Address reprint
coagulant therapy had been prescribed for more patients in the intervention requests to Dr. Gladstone at the Regional
Stroke Centre, Sunnybrook Health Sciences
group than in the control group (52 of 280 patients [18.6%] vs. 31 of 279 [11.1%]; Centre, A442-2075 Bayview Ave., Toronto, ON
absolute difference, 7.5 percentage points; 95% CI, 1.6 to 13.3; P = 0.01). M4N 3M5, Canada, or at david.gladstone@
sunnybrook.ca.
CONCLUSIONS
* A complete list of participating sites, investi-
Among patients with a recent cryptogenic stroke or TIA who were 55 years of gators, and coordinators for the 30-Day Car-
age or older, paroxysmal atrial fibrillation was common. Noninvasive ambula- diac Event Monitor Belt for Recording Atrial
tory ECG monitoring for a target of 30 days significantly improved the detection Fibrillation after a Cerebral Ischemic Event
(EMBRACE) trial is provided in the Supple-
of atrial fibrillation by a factor of more than five and nearly doubled the rate of mentary Appendix, available at NEJM.org.
anticoagulant treatment, as compared with the standard practice of short-duration N Engl J Med 2014;370:2467-77.
ECG monitoring. (Funded by the Canadian Stroke Network and others; EMBRACE DOI: 10.1056/NEJMoa1311376
Copyright © 2014 Massachusetts Medical Society.
ClinicalTrials.gov number, NCT00846924.)
n engl j med 370;26 nejm.org june 26, 2014 2467
The New England Journal of Medicine
Downloaded from nejm.org on November 2, 2014. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
T
he prevention of stroke related to We conducted a randomized trial of prolonged
atrial fibrillation is a global public health noninvasive ambulatory ECG monitoring to guide
priority. Strokes due to atrial fibrillation the treatment of patients with unexplained stroke
are common and frequently devastating (70 to or TIA. We hypothesized that monitoring for
80% of patients die or become disabled1,2), yet 30 days with the use of an automated device for
they are largely preventable with anticoagulant detecting atrial fibrillation, as compared with
therapy (64% reduction in the risk of stroke and one additional round of conventional 24-hour
25% reduction in mortality).3 However, because ECG monitoring, would enhance the detection
atrial fibrillation is often intermittent and asymp- and treatment of atrial fibrillation in high-risk
tomatic, it can be a silent risk factor that easily patients who would be candidates for anticoagu-
evades detection.4,5 lant therapy.
Since patients who have had a stroke or tran-
sient ischemic attack (TIA) due to atrial fibrilla- ME THODS
tion face a high annual risk of stroke recur-
rence,6 strategies to improve the detection and STUDY POPULATION
treatment of atrial fibrillation promise to reduce Patients were eligible for enrollment if they were
the burden of recurrent strokes. In the absence 55 years of age or older, did not have known atrial
of atrial fibrillation, the standard treatment for fibrillation, and had had an ischemic stroke or
secondary prevention of stroke is antiplatelet TIA of undetermined cause (according to TOAST
therapy; however, when atrial fibrillation is pres- [Trial of Org 10172 in Acute Stroke Treatment]
ent, antiplatelet therapy is only modestly effec- criteria14) within the previous 6 months, diag-
tive (22% reduction in risk, as compared with nosed by a stroke neurologist after a standard
placebo),3 and anticoagulation is strongly recom- workup, including 12-lead ECG, ambulatory ECG
mended instead (39%3 to 63%7 reduction in the monitoring with the use of a Holter monitor for
risk of stroke as compared with antiplatelet thera- a minimum of 24 hours, brain and neurovascular
py). Currently, 1 in 6 strokes is attributed to atrial imaging, and echocardiography (Table S1 in the
fibrillation, but 1 in 4 of the estimated 12 million Supplementary Appendix, available with the full
ischemic strokes annually (and half the TIAs) text of this article at NEJM.org, lists the eligibil-
has no cause identified after a standard diag- ity criteria; Table S2 lists the diagnostic investi-
nostic workup and is labeled “cryptogenic.”8,9 gations). Patients were excluded if the most likely
Undiagnosed atrial fibrillation is often suspected etiologic diagnosis had already been determined
as the cause of many cryptogenic strokes, but anti- (large-vessel or small-vessel disease or other
coagulation is not recommended unless atrial known cause).
fibrillation has been documented.
An unsolved problem is how to detect “covert” STUDY DESIGN AND OVERSIGHT
atrial fibrillation in patients with stroke. Screening In this investigator-initiated, open-label, multi-
is typically limited to electrocardiographic (ECG) center trial, we randomly assigned participants
monitoring for a short period (e.g., 24 hours), in a 1:1 ratio to undergo ambulatory ECG monitor-
which is not sufficiently sensitive for the detec- ing with a 30-day event-triggered loop recorder
tion of paroxysmal atrial fibrillation10-12; as a (intervention group) or one additional round of
result, it is likely that atrial fibrillation is being 24-hour Holter monitoring (control group). Ran
routinely underdiagnosed and undertreated with domization was performed with the use of a Web-
this approach. Observational studies have shown based system and a variable block size. Patients
that there is improved detection of atrial fibril- were enrolled by vascular neurologists at 16 stroke
lation with serial or prolonged ECG monitor- centers within the Canadian Stroke Consortium.
ing,10-13 yet such studies have had little effect The trial was coordinated at the Applied Health
on practice. Without a definitive trial, it is un- Research Centre, Li Ka Shing Knowledge Institute
known whether intensive monitoring would of St. Michael’s Hospital, and Sunnybrook Re
increase atrial fibrillation detection and treat- search Institute, University of Toronto.
ment rates more than standard monitoring and The protocol (available at NEJM.org) was test
follow-up. ed in a pilot study,15 approved by Health Canada
2468 n engl j med 370;26 nejm.org june 26, 2014
The New England Journal of Medicine
Downloaded from nejm.org on November 2, 2014. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
Atrial Fibrillation in Cryptogenic Stroke
and the ethics board at each study site, and em All the reports were reviewed centrally by one
bedded in routine stroke care, with all the par- physician.
ticipants providing written informed consent.
The steering committee, which was independent OUTCOMES
of commercial influence, was responsible for the The primary outcome was the detection of one or
study design and execution, data analysis, and more episodes of ECG-documented atrial fibril-
authorship decisions. The first author wrote the lation or flutter lasting 30 seconds or longer
first and subsequent drafts of the manuscript. within 90 days after randomization (documented
The steering committee made the decision to by the study monitors or detected clinically, apart
submit the manuscript for publication. All the from the study monitors). Secondary outcomes
authors vouch for the accuracy of the data and included oral anticoagulant use at 90 days, atrial
confirm that the contents of this article adhere fibrillation lasting 30 seconds or longer that was
to the specifications in the protocol. detected by the study monitor, atrial fibrillation
The ECG devices were purchased for the trial. of any duration that was detected by the study
The device manufacturers had no role in the monitor, atrial fibrillation lasting 2.5 minutes or
trial design, data accrual, or data analysis and longer (the maximum recording duration per epi
had no access to the study data. sode) that was detected by the study monitor, ad-
herence to monitoring, and a switch from anti
ECG MONITORING platelet to anticoagulant therapy in the period
The event recorder (ER910AF Cardiac Event Mon from randomization to 90 days.
itor, Braemar) automatically recorded atrial fibril
lation on the basis of irregularity in the R-R in- STATISTICAL ANALYSIS
terval, an established method for the detection of The primary analysis compared the proportion of
atrial fibrillation,16 over a period of 30 beats at patients in each group who had the primary out-
any rate. The devices had a 30-minute memory come and was performed with the use of Pearson’s
capacity and were programmed to record up to chi-square test in the intention-to-monitor popu-
2.5 minutes per episode. Recorders were attached lation, which consisted of all patients who under-
to a dry-electrode (nonadhesive) belt worn around went randomization and for whom the atrial-
the chest (Cardiac Bio-Systems)17 to enable better fibrillation status could be assessed (patients
compliance by the patients with prolonged mon- who underwent any amount of monitoring or had
itoring than has been typically observed with 90-day follow-up). Secondary analyses assessed
conventional adhesive skin-contact electrodes. the proportions of patients with atrial fibrilla-
The intervention group was instructed to wear tion detected by means of the study monitors
the monitor as much as possible for 30 days. If among patients who underwent any monitoring.
atrial fibrillation was detected before 30 days, We used Pearson’s chi-square test to compare the
patients could stop wearing the monitor. proportions of patients for whom anticoagulant
Recorded ECG data were transmitted trans- or antiplatelet therapy was prescribed. There were
telephonically for central interpretation. All the no interim analyses. See the Supplementary
episodes of atrial fibrillation were adjudicated Appendix for the sample-size calculation and de-
by a cardiologist and an internist who were un- scriptions of additional analyses.
aware of the patient’s demographic and clinical
characteristics, and any disagreements were re- R E SULT S
solved by discussion with an independent car-
diologist. Results were sent to the study sites, CHARACTERISTICS OF THE PATIENTS
and decisions regarding anticoagulant therapy From June 2009 through March 2012, a total of
were made at the discretion of the treating phy- 572 patients underwent randomization, and 90-
sicians. day follow-up was complete in 97.7% of the pa-
The patients in the control group were assigned tients (Fig. 1). The mean (±SD) age of the patients
to one additional round of conventional 24-hour was 72.5±8.5 years (range, 52 to 96) (Table 1).
ambulatory ECG monitoring with a Holter moni- Randomization occurred a mean of 75.1±38.6 days
tor from the local laboratory at their study site. after the qualifying event (62.9% of patients had
n engl j med 370;26 nejm.org june 26, 2014 2469
The New England Journal of Medicine
Downloaded from nejm.org on November 2, 2014. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
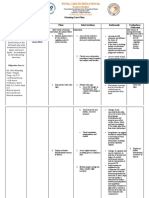
572 Patients were enrolled and underwent
randomization
287 Were assigned to 30-day ECG 285 Were assigned to 24-hour ECG
monitoring monitoring
284 Received assigned intervention 277 Received assigned intervention
3 Did not receive assigned 8 Did not receive assigned
intervention intervention
1 Had new diagnosis of cancer 1 Died from new ischemic
2 Withdrew from study stroke
2 Had medical illness
1 Had pacemaker inserted
1 Moved out of country
3 Withdrew from study
280 Were included in 90-day follow-up 279 Were included in 90-day follow-up
7 Were lost to follow-up 6 Were lost to follow-up
1 Died from new ischemic stroke 1 Died from new ischemic stroke
1 Had adverse skin reaction 5 Withdrew from study
5 Withdrew from study
1 Was excluded from all analyses
owing to withdrawal from study
immediately after randomization
with no baseline data recorded
286 Were included in all analyses 285 Were included in all analyses
280 Were included in primary 277 Were included in primary
analysis analysis
6 Were excluded because the 8 Were excluded because the
primary outcome could not be primary outcome could not be
assessed assessed
284 Were included in secondary 277 Were included in secondary
analysis analysis
2 Were excluded because they did 8 Were excluded because they did
not undergo any monitoring not undergo any monitoring
Figure 1. Randomization, Electrocardiographic (ECG) Monitoring, and Follow-up.
Six patients assigned to 30-day ECG monitoring and eight patients assigned to 24-hour ECG monitoring were ex-
cluded from the analysis of the primary outcome because they did not undergo any monitoring or because there
were no outcome data available at 90-day follow-up.
an ischemic stroke and 36.9% had a TIA). Of the or older are each assigned 1 point, and prior
patients, 93.9% were ambulatory and independent stroke or TIA is assigned 2 points. Before en-
(some patients had initially severe embolic strokes rollment, participants underwent conventional
reversed by means of thrombolysis), and the me- screening for atrial fibrillation with one or more
dian CHADS2 score of the patients was 3 points 12-lead ECGs and one or more 24-hour Holter
(range, 2 to 6). Scores on the CHADS2 range ECG studies, totaling a mean of 32.8±12.9 hours
from 0 to 6, with higher scores indicating a of monitoring; 9.1% of the patients also under-
greater risk of stroke; congestive heart failure, went inpatient telemetry ECG monitoring for a
hypertension, diabetes, and an age of 75 years mean duration of 53.6±42.6 hours.
2470 n engl j med 370;26 nejm.org june 26, 2014
The New England Journal of Medicine
Downloaded from nejm.org on November 2, 2014. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
Atrial Fibrillation in Cryptogenic Stroke
Table 1. Baseline Characteristics of the Patients.*
Intervention Group Control Group
Characteristic (N = 286) (N = 285)
Age
Mean age — yr 72.5±8.5 73.2±8.8
≥75 yr — no. (%) 104 (36.4) 118 (41.4)
Female sex — no. (%) 132 (46.2) 125 (43.9)
Race — no. (%)†
White 257 (89.9) 260 (91.2)
Asian 15 (5.2) 14 (4.9)
Black 6 (2.1) 2 (0.7)
Other 8 (2.8) 9 (3.2)
Modified Rankin scale score ≤2 — no. (%)‡ 274 (95.8) 263 (92.3)
Medical history — no. (%)
Hypertension 204 (71.3) 191 (67.0)
Diabetes 55 (19.2) 55 (19.3)
Hyperlipidemia 191 (66.8) 177 (62.1)
Smoking status
Current smoker 19 (6.6) 24 (8.4)
Previous smoker 141 (49.3) 131 (46.0)
Previous ischemic stroke 45 (15.7) 36 (12.6)
>1 Previous stroke 12 (4.2) 12 (4.2)
Previous transient ischemic attack 42 (14.7) 46 (16.1)
Congestive heart failure 5 (1.7) 7 (2.5)
Myocardial infarction 48 (16.8) 42 (14.7)
Coronary angioplasty or stenting 24 (8.4) 23 (8.1)
Coronary bypass surgery 29 (10.1) 19 (6.7)
Cardiac-valve surgery 6 (2.1) 1 (0.4)
Type of index event — no. (%)
Ischemic stroke 188 (65.7) 172 (60.4)
Transient ischemic attack 98 (34.3) 113 (39.6)
Oxfordshire classification18 of the index event — no. (%)§
Total anterior circulation syndrome 7 (2.4) 5 (1.8)
Partial anterior circulation syndrome 201 (70.3) 216 (75.8)
Posterior circulation syndrome 63 (22.0) 56 (19.6)
Lacunar syndrome 15 (5.2) 7 (2.5)
No. of days from index event to randomization 76.6±37.5 73.7±39.7
* Plus–minus values are means ±SD. There were no significant differences between the two study groups at the 0.05
significance level.
† Race was determined by the investigator.
‡ Scores on the modified Rankin scale range from 0 to 6, with 0 indicating no symptoms and 6 indicating death; a score
of 2 or less indicates that the patient is ambulatory and functionally independent in activities of daily living.
§ Data were missing for one patient in the control group.
ADHERENCE TO THE PROTOCOL ing. Among patients in whom atrial fibrillation
Among the patients in the intervention group was not detected before 30 days, 204 of 240
who started to undergo monitoring, 233 of 284 (85.0%) completed 3 or more weeks, and 148 of
(82.0%) completed 3 or more weeks of monitor- 240 (61.7%) completed 4 weeks.
n engl j med 370;26 nejm.org june 26, 2014 2471
The New England Journal of Medicine
Downloaded from nejm.org on November 2, 2014. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
DETECTION OF ATRIAL FIBRILLATION IN THE TWO A total of 26 of these patients (59.1%) had 2 or
GROUPS more episodes recorded, and 28 patients (63.6%)
The 30-day ECG monitoring strategy was superior had an episode of atrial fibrillation lasting at
to 24-hour ECG monitoring for the detection of least 2.5 minutes (the maximum recordable dura-
at least one episode of atrial fibrillation lasting tion per episode).
30 seconds or longer (the primary outcome). Atrial New instances of atrial fibrillation were de-
fibrillation was detected in 45 of 280 patients tected throughout the 30 days, with half the
(16.1%) in the intervention group, as compared cases captured within the first week of monitor-
with 9 of 277 (3.2%) in the control group, for an ing and three quarters within 2 weeks (Fig. 2).
absolute difference of 12.9 percentage points The detection rate was significantly higher
(95% confidence interval [CI], 8.0 to 17.6; P<0.001; among patients who underwent randomization
number needed to screen, 8) (Table 2). Sensitivity within 3 months after the index stroke or TIA
analysis did not alter the conclusions (see the than among those who underwent randomiza-
Supplementary Appendix). Atrial fibrillation was tion after more than 3 months (36 of 195 patients
detected clinically, rather than by the study mon- [18.5%] vs. 8 of 89 [9.0%]; P = 0.049 for linear
itors, in only 0.5% of patients within 90 days association). The patients with atrial fibrillation
after randomization (see the Supplementary were older and had more atrial ectopic activity
Appendix). Prolonged monitoring was also supe- according to baseline Holter monitoring than
rior for the detection of continuous atrial fibril- those without atrial fibrillation (P<0.001 for both
lation lasting at least 2.5 minutes: in 28 of 284 comparisons) (Table S3 in the Supplementary
patients (9.9%) in the intervention group versus Appendix).
7 of 277 (2.5%) in the control group, for an abso-
lute difference of 7.4 percentage points (95% CI, EFFECT ON TREATMENT
3.4 to 11.3; P<0.001) (Table 2). At randomization, the majority of patients were
receiving antiplatelet therapy, as expected. After
ATRIAL FIBRILLATION IN THE INTERVENTION GROUP monitoring, most of the patients with atrial fi-
The 30-day monitors recorded 218 episodes of brillation received anticoagulant therapy (see the
atrial fibrillation lasting 30 seconds or longer in Supplementary Appendix). Use of oral anticoagu-
44 patients (range, 1 to 29 episodes per patient). lant therapy tripled in the intervention group,
Table 2. Detection of Atrial Fibrillation in the Two Monitoring Groups.
No. of Patients
Intervention Group Control Group Absolute Difference Needed to Screen
Outcome (N = 286) (N = 285) (95% CI) P Value (95% CI)*
number/total number (percent) percentage points
Primary outcome: detection of atrial 45/280 (16.1) 9/277 (3.2) 12.9 (8.0–17.6) <0.001 8 (5.7–12.5)
fibrillation with duration
≥30 sec within 90 days†
Secondary outcomes‡
Detection of atrial fibrillation 44/284 (15.5) 7/277 (2.5) 13.0 (8.4–17.6) <0.001 8 (5.7–11.9)
with duration ≥30 sec
Detection of atrial fibrillation 28/284 (9.9) 7/277 (2.5) 7.4 (3.4–11.3) <0.001 14 (8.8–29.4)
with duration ≥2.5 min
Detection of atrial fibrillation 56/284 (19.7) 13/277 (4.7) 15.0 (9.8–20.3) <0.001 7 (4.9–10.2)
of any duration
* The number of patients needed to screen was defined as the number of patients who would need to be screened in order to detect atrial
fibrillation in one additional patient (with a 30-day monitoring strategy vs. repeat 24-hour Holter monitoring).
† The primary analysis included all the patients who underwent randomization for whom outcome data were available (i.e., patients who un-
derwent any amount of cardiac monitoring or 90-day follow-up in whom the status of atrial fibrillation could be determined). In the primary
analysis, atrial fibrillation was detected either clinically or by means of study monitoring.
‡ The secondary analyses included all the patients who underwent randomization and any amount of cardiac monitoring. The detection of
atrial fibrillation in the secondary analyses was by means of the study monitors.
2472 n engl j med 370;26 nejm.org june 26, 2014
The New England Journal of Medicine
Downloaded from nejm.org on November 2, 2014. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
Atrial Fibrillation in Cryptogenic Stroke
and at 90 days, the proportion of patients treated
with anticoagulants was significantly higher in 20
the intervention group than in the control group:
Patients with Atrial Fibrillation
18.6% (52 of 280 patients) versus 11.1% (31 of 15
14.8
279), for an absolute treatment difference of 7.5 12.3
Detected (%)
11.6
percentage points (95% CI, 1.6 to 13.3; P = 0.01)
(Table 3). In the intervention group, 38 of 280 10
7.4
patients (13.6%) switched from antiplatelet to
anticoagulant therapy, as compared with 13 of 5
279 (4.7%) in the control group, a difference of 8.9 2.2
percentage points (95% CI, 4.2 to 13.6; P<0.001).
0
24 Hr 1 Wk 2 Wk 3 Wk 4 Wk
DISCUSSION Duration of ECG Monitoring
We found that ambulatory ECG monitoring for a Figure 2. Incremental Yield of Prolonged ECG Monitoring for the Detection
target of 30 days was feasible to implement as of Atrial Fibrillation in Patients with Cryptogenic Stroke or TIA.
part of routine stroke care, detected atrial fibril- The proportion of patients in whom atrial fibrillation was detected increased
with increasing duration of ECG monitoring. The data reflect the timing of
lation in one in six patients (which had not previ-
the first detected episode of atrial fibrillation; data for 2 patients are not
ously been detected by means of standard 24 to shown because the exact date of the detection of atrial fibrillation was un-
48 hours of monitoring after stroke), was supe- known. Atrial fibrillation was detected in 6 of 277 patients who underwent
rior to an additional round of 24-hour ECG mon- monitoring with a 24-hour Holter monitor (the control group). In the group
itoring and clinical follow-up (the detection rate of 284 patients who underwent 30-day monitoring, atrial fibrillation was
detected in 21 patients within the first week of monitoring, in 33 within the
with 30-day monitoring was increased by a factor
first 2 weeks of monitoring, in 35 within the first 3 weeks of monitoring, and
of five), and had an incremental yield over a pe- in 42 within 4 weeks of monitoring (including 1 patient with atrial fibrillation
riod of 30 days. Moreover, prolonged monitoring that was first detected on day 34).
nearly doubled the proportion of patients who
subsequently received anticoagulant therapy for
secondary prevention of stroke — a finding we
interpret as a clinically meaningful change in The finding of even brief atrial fibrillation in
treatment that has the potential to avert recur- this population is considered important, given
rent strokes. These findings, taken together with increasing evidence that brief subclinical atrial
mounting observational data linking subclinical fibrillation predicts subsequent episodes of atrial
atrial fibrillation to cryptogenic strokes10-13 and fibrillation and is an independent risk factor for
a randomized trial supporting 7-day monitoring in recurrent stroke.25 In the Asymptomatic Atrial
the acute phase after the occurrence of stroke,19 Fibrillation and Stroke Evaluation in Pacemaker
provide strong evidence supporting adoption of a Patients and the Atrial Fibrillation Reduction
more intensive approach to the detection of atrial Atrial Pacing Trial (ASSERT), any subclinical
fibrillation in patients with unexplained stroke atrial tachyarrhythmia lasting longer than 6 min-
or TIA. utes predicted clinically evident atrial fibrillation
Evaluating patients for atrial fibrillation af- (hazard ratio, 5.6) and stroke or systemic embo-
ter a stroke or TIA is important because of the lism (hazard ratio, 2.5).4 In the Mode Selection
treatment implications. We targeted patients at Trial (MOST), any atrial high-rate episode lasting
risk for stroke recurrence who were potential longer than 5 minutes predicted clinical atrial
candidates for anticoagulant therapy, yet in prac- fibrillation (hazard ratio, 5.9) and stroke or death
tice such patients typically receive only antiplate- (hazard ratio, 2.8).26 Our primary outcome of
let therapy if atrial fibrillation is not detected. atrial fibrillation lasting 30 seconds or longer is
When atrial fibrillation is detected, anticoagula- consistent with guidelines27-30 and, although arbi-
tion is strongly advised, whether the atrial fibril- trary, is a potentially clinically important and
lation is paroxysmal or sustained, because the actionable finding in this population. Expert
stroke risks are similar20-22 and patients with opinion differs regarding the minimum duration
either type of atrial fibrillation benefit from or frequency of atrial fibrillation captured by
anticoagulation.20,23,24 ECG that warrants anticoagulation. Until future
n engl j med 370;26 nejm.org june 26, 2014 2473
The New England Journal of Medicine
Downloaded from nejm.org on November 2, 2014. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
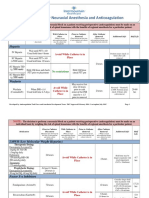
Table 3. Anticoagulant Therapy in the Two Monitoring Groups.*
Intervention Group Control Group Absolute Difference
Therapy (N = 286) (N = 285) (95% CI) P Value
no./total no. (%) percentage points
Baseline
Anticoagulant therapy before the index 3/286 (1.0) 2/285 (0.7) — —
stroke or TIA
Anticoagulant therapy at randomization 16/286 (5.6) 19/285 (6.7) — —
after the index stroke or TIA
After study monitoring
Therapy at 90 days after randomization
Anticoagulant therapy 52/280 (18.6) 31/279 (11.1) 7.5 (1.6 to 13.3) 0.01
Antiplatelet therapy only 223/280 (79.6) 246/279 (88.2) −8.6 (−14.6 to −2.5) 0.006
Therapy at randomization changed
by 90 days
From antiplatelet therapy to 38/280 (13.6) 13/279 (4.7) 8.9 (4.2 to 13.6) <0.001
anticoagulant therapy
From anticoagulant therapy to 3/280 (1.1) 2/279 (0.7) 0.4 (−1.2 to 1.9) 0.66
antiplatelet therapy
* Anticoagulant therapy was defined as the use of any oral anticoagulant (warfarin, dabigatran, rivaroxaban, or apixaban).
Antiplatelet therapy was defined as the use of any antiplatelet medication (aspirin, clopidogrel, aspirin–extended-release
dipyridamole, dipyridamole, or other antiplatelet agent) and no oral anticoagulant therapy.
studies establish this, we believe prolonged mon- antiplatelet therapy and minimize unnecessary
itoring permits more rational decision making long-term anticoagulation in presumably low-risk
regarding antithrombotic therapy, strengthening patients with cryptogenic stroke.
recommendations for or against anticoagulation. These findings have implications for clinical
In this trial, most patients with atrial fibrillation practice and widespread applicability for sec-
received anticoagulant therapy, even though they ondary prevention of stroke in regions where
would not have met the traditional criteria for cardiac monitoring is available. The results of
duration of atrial fibrillation used in published this study support prolonged monitoring after
trials evaluating the treatment of atrial fibrilla- a recent cryptogenic embolic stroke or TIA in
tion.3 Two thirds of the patients with atrial fi- selected patients 55 years of age or older who
brillation detected in the intervention group had would be considered appropriate candidates for
at least 2.5 minutes of continuous atrial fibrilla- anticoagulant therapy if atrial fibrillation were
tion (episodes could have lasted hours or days, found. We think that the common practice of
but only the first 2.5 minutes could be captured). relying on 24 to 48 hours of monitoring for
The threshold for anticoagulation is generally atrial fibrillation after a stroke or TIA of un
lower when it is for secondary prevention than it determined cause is insufficient and consider it
is for primary prevention, and a low threshold ap an initial screen rather than a final test, espe-
pears to be reasonable for our patients who had a cially given our finding that the yield of clinical
high pretest probability of atrial fibrillation,31 ex- follow-up alone as a means of detecting atrial
cess atrial ectopy on baseline Holter monitoring,32 fibrillation was negligible. Improving the detec-
and an elevated stroke risk.33 With the availabil- tion of atrial fibrillation will be increasingly im-
ity of newer anticoagulants, empirical anticoagu- portant for an aging population: the rising preva-
lation for suspected but unproven atrial fibrilla- lence of atrial fibrillation, along with declining
tion is tempting34 but controversial35 and has the rates of large-vessel and small-vessel cerebrovas-
potential for overuse if sufficient ECG screening cular disease, is likely to result in an increasing
is not performed. The absence of atrial fibrilla- number of strokes related to both overt and
tion on prolonged monitoring can help justify covert atrial fibrillation.36
2474 n engl j med 370;26 nejm.org june 26, 2014
The New England Journal of Medicine
Downloaded from nejm.org on November 2, 2014. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
Atrial Fibrillation in Cryptogenic Stroke
This study had several limitations. We could embolic stroke was due to previously undetected
not determine the total burden of atrial fibrilla- atrial fibrillation, we acknowledge that the de-
tion per patient owing to the limited recording tection of atrial fibrillation after stroke cannot
capacity of the ECG device, and patients typically prove causation37 and should not preclude the
stopped the monitoring before 30 days, once any consideration of many other possible causes.9
atrial fibrillation was documented. Our results The longer the delay from stroke to the detec-
therefore represent the minimum amount of tion of atrial fibrillation, the more difficult it is
atrial fibrillation that was possible to record, to infer causation.38 Also, we did not study age-
probably underestimating the total duration and matched controls without stroke or TIA. How
frequency of atrial fibrillation. Newer external ever, even if atrial fibrillation is an incidental
devices allow unlimited recording of the burden finding, it influences risk stratification and
of atrial fibrillation. provides an opportunity to prescribe anticoagu-
In addition, the 16% prevalence of atrial fi- lant therapy for maximum risk reduction. Future
brillation that we observed in the intervention studies are required to determine the extent of
group is likely to be a conservative estimate for risk reduction associated with prolonged moni-
several reasons. First, patients with large, severe toring and its cost-effectiveness.19,39,40
strokes, in which cardioembolism is likely to be In conclusion, the results of our study show
most prevalent, were underrepresented; however, that noninvasive outpatient ECG monitoring for
they were not the target of this trial, which fo- 30 days is superior to the standard practice of
cused on stroke survivors attending outpatient short-term ECG monitoring for the detection of
clinics after hospital discharge, most of whom atrial fibrillation in patients with a stroke or TIA
had had mild, nondisabling strokes and were labeled as cryptogenic. This observation sug-
considered to be ideal candidates for secondary gests that in current practice, a substantial pro-
stroke prevention. Second, monitoring started portion of such patients have paroxysmal atrial
relatively late in many patients (an average of fibrillation that goes undiagnosed and untreated.
75 days after the index stroke or TIA), reducing Prolonged ECG monitoring offers greater oppor-
the overall sensitivity for the detection of atrial tunities for the detection and treatment of one
fibrillation; indeed, the earlier initiation of mon- of the most common and important modifiable
itoring identified more patients with atrial fibril- risk factors for recurrent stroke.
lation than later initiation did. Third, we know Supported by peer-reviewed operating grants from the
that the yield of monitoring increases well be- Canadian Stroke Network, one of the Networks of Centres of
yond 30 days, as shown by studies using im- Excellence of Canada. Dr. Gladstone was supported by a
Clinician-Scientist Award from the Heart and Stroke Foundation
planted devices.4,11,12,27 However, 30 days was a of Ontario, the Bastable-Potts Chair in Stroke, the Heart and
pragmatic choice for this trial, since we thought Stroke Foundation Canadian Partnership for Stroke Recovery,
it was likely to be the upper limit for adherence the University of Toronto Department of Medicine and the Eaton
Scholar Award, the University of Toronto Division of Neurology
to monitoring with the external study devices New Initiatives Program, the Department of Medicine Research
and because subcutaneously implanted recorders Committee and the Brain Sciences Program at Sunnybrook
are invasive (minimally), costly, and not yet Health Sciences Centre, Sunnybrook Research Institute, Sunny
brook Foundation, the Sam Sorbara family, and the Bril Chair in
widely accessible for routine first-line screening Neurology, University of Toronto.
after stroke. Fourth, because cryptogenic stroke Dr. Gladstone reports receiving travel support and fees for
is a heterogeneous entity that has lacked a rigor- participating on advisory boards from Bayer, Boehringer Ingel
heim, Bristol-Myers Squibb, Daiichi Sankyo, and Pfizer and
ous uniform definition and not all our patients consulting and lecture fees from Bayer, Boehringer Ingelheim,
underwent intracranial vascular imaging or trans Bristol-Myers Squibb, and Pfizer; Dr. Dorian, consulting fees
esophageal echocardiography, the trial probably from Servier, lecture fees from Bristol-Myers Squibb, Bayer,
Pfizer, and Boehringer Ingelheim, and grant support through
enrolled patients with other causes of stroke, thus his institution from Bristol-Myers Squibb, Bayer, Pfizer, Boeh
reducing the proportion with atrial fibrillation, as ringer Ingelheim, and Servier; Dr. O’Donnell, honoraria for
compared with a group of more fully evaluated presentations from Pfizer, Bristol-Myers Squibb, Boehringer
Ingelheim, and Pfizer; Dr. Côté, fees for participating on advi-
patients with truly cryptogenic stroke. sory boards from Boehringer Ingelheim, Pfizer, and Bayer; Dr.
Although it is well known that embolism to Sharma, fees for participating on advisory boards from Boeh
the brain can be the first manifestation of atrial ringer Ingelheim, Bayer, Bristol-Myers Squibb, and Pfizer, lecture
fees from Boehringer Ingelheim, Bayer, and Pfizer, and grant
fibrillation, and the discovery of atrial fibrilla- support from Bayer; Dr. Shuaib, lecture fees from Boehringer
tion after stroke increases the likelihood that an Ingelheim, Bristol-Myers Squibb, and Pfizer and grant support
n engl j med 370;26 nejm.org june 26, 2014 2475
The New England Journal of Medicine
Downloaded from nejm.org on November 2, 2014. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
The n e w e ng l a n d j o u r na l of m e dic i n e
from Boehringer Ingelheim; Dr. Coutts, grant support from of Toronto Stroke Program, and Sunnybrook Regional Stroke
Pfizer; Dr. Yip, lecture fees from Bayer, Boehringer Ingelheim, Centre, including the Regional Stroke Prevention Clinic and
Bristol-Myers Squibb, Pfizer, and Servier; Dr. Casaubon, fees for the Dr. Thomas and Harriet Black/Scotiabank Rapid TIA
participating on advisory boards from Covidien and the Bristol- Clinic; K. Sabihuddin, N. Kozlowski, K. Hood, and staff at the
Myers Squibb–Pfizer Alliance, and lecture fees from Bayer and Applied Health Research Centre, Li Ka Shing Knowledge Insti
Sanofi; and Dr. Mamdani, fees for participating on advisory boards tute of St. Michael’s Hospital, Toronto; W. Levinson, K. Imrie,
from AstraZeneca, Bristol-Myers Squibb, Eli Lilly, GlaxoSmithKline, S.E. Black, and J.R. Perry of the University of Toronto De
Roche, Novartis, Novo Nordisk, and Pfizer. No other potential partment of Medicine; M. Braganza, J. Warenycia, M. Cherny-
conflict of interest relevant to this article was reported. Bayer, F. Leibovitch, K. Fan, N. Rashkovan, and B. Linkewich of
Disclosure forms provided by the authors are available with Sunnybrook Health Sciences Centre, Toronto; J. Kane and staff
the full text of this article at NEJM.org. at Remote Cardiac Monitoring Services, Toronto; the staff
We thank all the patients who volunteered to participate in at all the cardiology noninvasive laboratories at the par
this research; A. Hakim, K. Lafferty, K. Willis, and C. Campbell ticipating sites; A. Samson; and M.D. Hill, R.H. Swartz, S.E.
of the Canadian Stroke Network; the members of the Canadian Black, and R.G. Hart for comments on an earlier version of the
Stroke Consortium, the Ontario Stroke Network, the University manuscript.
REFERENCES
1. Gladstone DJ, Bui E, Fang J, et al. Po- 12. Kishore A, Vail A, Majid A, et al. De- Stroke with intermittent atrial fibrillation:
tentially preventable strokes in high-risk tection of atrial fibrillation after ischemic incidence and predictors during aspirin
patients with atrial fibrillation who are stroke or transient ischemic attack: a sys- therapy. J Am Coll Cardiol 2000;35:183-7.
not adequately anticoagulated. Stroke temic review and meta-analysis. Stroke 22. The Boston Area Anticoagulation Trial
2009;40:235-40. 2014 January 2 (Epub ahead of print). for Atrial Fibrillation Investigators. The
2. Saposnik G, Gladstone D, Raptis R, 13. Culebras A, Messe SR, Chaturvedi S, effect of low-dose warfarin on the risk of
Zhou L, Hart RG. Atrial fibrillation in et al. Summary of evidence-based guide- stroke in patients with nonrheumatic
ischemic stroke: predicting response to line update: prevention of stroke in non- atrial fibrillation. N Engl J Med 1990;323:
thrombolysis and clinical outcomes. valvular atrial fibrillation: report of the 1505-11.
Stroke 2013;44:99-104. Guideline Development Subcommittee of 23. Al-Khatib SM, Thomas L, Wallentin L,
3. Hart RG, Pearce LA, Aguilar MI. Meta- the American Academy of Neurology. et al. Outcomes of apixaban vs. warfarin
analysis: antithrombotic therapy to pre- Neurology 2014;82:716-24. by type and duration of atrial fibrillation:
vent stroke in patients who have nonval- 14. Goldstein LB, Jones MR, Matchar DB, results from the ARISTOTLE trial. Eur
vular atrial fibrillation. Ann Intern Med et al. Improving the reliability of stroke Heart J 2013;34:2464-71.
2007;146:857-67. subgroup classification using the Trial of 24. Flaker G, Ezekowitz M, Yusuf S, et al.
4. Healey JS, Connolly SJ, Gold MR, et al. ORG 10172 in Acute Stroke Treatment Efficacy and safety of dabigatran com-
Subclinical atrial fibrillation and the risk (TOAST) criteria. Stroke 2001;32:1091-8. pared to warfarin in patients with paroxys-
of stroke. N Engl J Med 2012;366:120-9. 15. Spring M, Dorian P, Fry B, et al. A 30- mal, persistent, and permanent atrial
5. Camm AJ, Corbucci G, Padeletti L. day cardiac event monitor belt for record- f ibrillation: results from the RE-LY (Ran-
Usefulness of continuous electrocardio- ing paroxysmal atrial fibrillation after a domized Evaluation of Long-Term Antico-
graphic monitoring for atrial fibrillation. cerebral ischemic event. Stroke 2008;39: agulation Therapy) study. J Am Coll Car-
Am J Cardiol 2012;110:270-6. 571-2. diol 2012;59:854-5.
6. Stroke Risk in Atrial Fibrillation 16. Esperer HD, Esperer C, Cohen RJ. 25. Glotzer TV, Ziegler PD. Silent atrial
Working Group. Independent predictors Cardiac arrhythmias imprint specific sig- fibrillation as a stroke risk factor and anti-
of stroke in patients with atrial fibrilla- natures on Lorenz plots. Ann Noninvasive coagulation indication. Can J Cardiol 2013;
tion: a systematic review. Neurology 2007; Electrocardiol 2008;13:44-60. 29:S14-S23.
69:546-54. 17. Advanced Bioelectric Corporation. 26. Glotzer TV, Hellkamp AS, Zimmer-
7. Connolly SJ, Eikelboom J, Joyner C, Breakthrough in long-term cardiac ambu- man J, et al. Atrial high rate episodes de-
et al. Apixaban in patients with atrial fi- latory monitoring — finally a dry elec- tected by pacemaker diagnostics predict
brillation. N Engl J Med 2011;364:806-17. trode for long-term monitoring. Eur Car- death and stroke: report of the Atrial
8. Bal S, Patel SK, Almekhlafi M, Modi J, diol Rev 2005;1:1-3. Diagnostics Ancillary Study of the MOde
Demchuk AM, Coutts SB. High rate of 18. Bamford J, Sandercock P, Dennis M, Selection Trial (MOST). Circulation 2003;
magnetic resonance imaging stroke recur- Burn J, Warlow C. Classification and nat- 107:1614-9.
rence in cryptogenic transient ischemic ural history of clinically identifiable sub- 27. Fuster V, Rydén LE, Cannom DS, et al.
attack and minor stroke patients. Stroke types of cerebral infarction. Lancet 1991; ACC/AHA/ESC 2006 Guidelines for the
2012;43:3387-8. 337:1521-6. Management of Patients with Atrial Fibril-
9. Hart RG, Diener HC, Coutts SB, et al. 19. Higgins P, MacFarlane PW, Dawson J, lation: a report of the American College of
Embolic strokes of undetermined source: McInnes GT, Langhorne P, Lees KR. Non- Cardiology/American Heart Association
the case for a new clinical construct. Lan- invasive cardiac event monitoring to de- Task Force on Practice Guidelines and the
cet Neurol 2014;13:429-38. tect atrial fibrillation after ischemic stroke: European Society of Cardiology Commit-
10. Liao J, Khalid Z, Scallan C, Morillo C, a randomized, controlled trial. Stroke tee for Practice Guidelines (Writing Com-
O’Donnell M. Noninvasive cardiac moni- 2013;44:2525-31. mittee to Revise the 2001 Guidelines for
toring for detecting paroxysmal atrial fi- 20. Hohnloser SH, Pajitnev D, Pogue J, the Management of Patients With Atrial
brillation or flutter after acute ischemic et al. Incidence of stroke in paroxysmal ver- Fibrillation): developed in collaboration
stroke: a systematic review. Stroke 2007; sus sustained atrial fibrillation in patients with the European Heart Rhythm Associ-
38:2935-40. taking oral anticoagulation or combined ation and the Heart Rhythm Society. Cir-
11. Seet RCS, Friedman PAM, Rabinstein antiplatelet therapy: an ACTIVE W Sub- culation 2006;114(7):e257-e354. [Erratum,
AAM. Prolonged rhythm monitoring for study. J Am Coll Cardiol 2007;50:2156- Circulation 2007;116(6):e138.]
the detection of occult paroxysmal atrial 61. 28. Calkins H, Kuck KH, Cappato R, et al.
fibrillation in ischemic stroke of unknown 21. Hart RG, Pearce LA, Rothbart RM, 2012 HRS/EHRA/ECAS expert consensus
cause. Circulation 2011;124:477-86. McAnulty JH, Asinger RW, Halperin JL. statement on catheter and surgical abla-
2476 n engl j med 370;26 nejm.org june 26, 2014
The New England Journal of Medicine
Downloaded from nejm.org on November 2, 2014. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
Atrial Fibrillation in Cryptogenic Stroke
tion of atrial fibrillation: recommenda- tion in stroke patients with suspected Secular trends in ischemic stroke subtypes.
tions for patient selection, procedural atrial fibrillation. Stroke 2013;44:302-3. Stroke 2013;44Suppl:A193. abstract.
techniques, patient management and fol- 32. Binici Z, Intzilakis T, Nielsen OW, 37. Rabinstein AA, Fugate JE, Mandrekar J,
low-up, definitions, endpoints, and re- Køber L, Sajadieh A. Excessive supraven- et al. Paroxysmal atrial fibrillation in
search trial design: a report of the Heart tricular ectopic activity and increased risk cryptogenic stroke: a case-control study.
Rhythm Society (HRS) Task Force on of atrial fibrillation and stroke. Circula- J Stroke Cerebrovasc Dis 2013;22:1405-
Catheter and Surgical Ablation of Atrial tion 2010;121:1904-11. 11.
Fibrillation. Heart Rhythm 2012;9:632-96. 33. Kamel H, Johnson DR, Hegde M, et al. 38. Brambatti M, Connolly SJ, Gold MR,
29. The Task Force for the Management Detection of atrial fibrillation after stroke et al. Temporal relationship between sub
of Atrial Fibrillation of the European So- and the risk of recurrent stroke. J Stroke clinical atrial fibrillation and embolic
ciety of Cardiology. Guidelines for the Cerebrovasc Dis 2012;21:726-31. events. Circulation 2014;129:2094-9.
management of atrial fibrillation. Eur 34. Diener HC. Stroke patients with sus- 39. Kamel H, Hegde M, Johnson DR,
Heart J 2010;31:2369-429. pected atrial fibrillation should be started Gage BF, Johnston SC. Cost-effectiveness
30. Kirchhof P, Auricchio A, Bax J, et al. on anticoagulation pending the results of outpatient cardiac monitoring to detect
Outcome parameters for trials in atrial of long-term cardiac monitoring. Stroke atrial fibrillation after ischemic stroke.
fibrillation: recommendations from a 2013;44:298-9. Stroke 2010;41:1514-20.
consensus conference organized by the 35. Katsnelson M, Sacco RL. Stroke pa- 40. Wachter R, Stahrenberg R, Gröschel
German Atrial Fibrillation Competence tients with suspected atrial fibrillation K. Letter by Wachter et al regarding arti-
NETwork and the European Heart Rhythm should NOT be started on anticoagulation cle “Cost-effectiveness of outpatient car-
Association. Europace 2007;9:1006-23. WHILE AWAITING the results of long- diac monitoring to detect atrial fibrilla-
31. Molina CA, Selim M. “If it looks like a term cardiac monitoring. Stroke 2013;44: tion after ischemic stroke.” Stroke 2011;
duck, walks like a duck, and quacks like a 300-1. 42(3):e36-e37.
duck . . . it must be a duck”: anticoagula- 36. Bogiatzi C, Hackam DG, Spence JD. Copyright © 2014 Massachusetts Medical Society.
n engl j med 370;26 nejm.org june 26, 2014 2477
The New England Journal of Medicine
Downloaded from nejm.org on November 2, 2014. For personal use only. No other uses without permission.
Copyright © 2014 Massachusetts Medical Society. All rights reserved.
You might also like
- Case StudyDocument6 pagesCase StudyMarie-Suzanne Tanyi100% (1)
- CHANCE Trial AND POINT Trial EditDocument16 pagesCHANCE Trial AND POINT Trial EditnurdiansyahNo ratings yet
- Intracerebral HemorrhageDocument281 pagesIntracerebral HemorrhageAnonymous vnv6QF100% (2)
- Nursing Care Plan: by The Wife During InterviewDocument3 pagesNursing Care Plan: by The Wife During InterviewJayson SamonteNo ratings yet
- 6.drugs For Coagulation Disorders NewDocument24 pages6.drugs For Coagulation Disorders NewNaseem Al tajerNo ratings yet
- Tabla Suplementaria SCA SICA AHA 2023Document52 pagesTabla Suplementaria SCA SICA AHA 2023David RojasNo ratings yet
- Heartfailure FixDocument10 pagesHeartfailure FixdhikaNo ratings yet
- Closure of Patent Foramen Ovale Versus Medical Therapy After Cryptogenic StrokeDocument9 pagesClosure of Patent Foramen Ovale Versus Medical Therapy After Cryptogenic StrokelaurasheerNo ratings yet
- New England Journal Medicine: The ofDocument11 pagesNew England Journal Medicine: The ofChanakarn PanNo ratings yet
- Sacks2018 PDFDocument13 pagesSacks2018 PDFJonathan Paucar ArévaloNo ratings yet
- Ticagrelor Versus Aspirin in Acute Stroke or Transient Ischemic AttackDocument9 pagesTicagrelor Versus Aspirin in Acute Stroke or Transient Ischemic AttackTara WandhitaNo ratings yet
- NEJM Defibrilation Strategies For Refractory VFDocument10 pagesNEJM Defibrilation Strategies For Refractory VFScience BrasilNo ratings yet
- Madit CRTNEJMseot 09Document10 pagesMadit CRTNEJMseot 09binh doNo ratings yet
- Race Ii 2010 NejmDocument11 pagesRace Ii 2010 NejmAxel Hiram Hernandez PinedaNo ratings yet
- Eficacia de La Telemedicina en El Manejo de La Insuficiencia CardíacaDocument11 pagesEficacia de La Telemedicina en El Manejo de La Insuficiencia CardíacaSMIBA MedicinaNo ratings yet
- Ticagrelor Versus Aspirin in Acute Stroke or Transient Ischemic AttackDocument10 pagesTicagrelor Versus Aspirin in Acute Stroke or Transient Ischemic AttackMaxend Arselino SilooyNo ratings yet
- Angiography After Out-of-Hospital Cardiac Arrest Without ST-Segment ElevationDocument10 pagesAngiography After Out-of-Hospital Cardiac Arrest Without ST-Segment ElevationYuritza Patricia Vargas OlivaresNo ratings yet
- Nej Mo A 2207304Document10 pagesNej Mo A 2207304julian zuletaNo ratings yet
- In-Hospital Stroke Recurrence and Stroke After Transient Ischemic AttackDocument15 pagesIn-Hospital Stroke Recurrence and Stroke After Transient Ischemic AttackferrevNo ratings yet
- Focus 1 Paper 4 Verheye Et Al 2015Document9 pagesFocus 1 Paper 4 Verheye Et Al 2015Jesson LuiNo ratings yet
- En Do Vascular Stenting or Carotid My For Treatment of Carotid Stenosis A Meta AnalysisDocument6 pagesEn Do Vascular Stenting or Carotid My For Treatment of Carotid Stenosis A Meta Analysisjohn_smith_532No ratings yet
- Cohorte Retrospectivda NOAF in CRITICSLLY ILLDocument8 pagesCohorte Retrospectivda NOAF in CRITICSLLY ILLARTURO YOSHIMAR LUQUE MAMANINo ratings yet
- Biventricular Pacing For Atrioventricular Block and Systolic DysfunctionDocument9 pagesBiventricular Pacing For Atrioventricular Block and Systolic DysfunctionRaul OrtegaNo ratings yet
- Ticagrelor Vs AASDocument9 pagesTicagrelor Vs AASjackusfafafaNo ratings yet
- Nejmoa 2206606Document10 pagesNejmoa 2206606dipan diratuNo ratings yet
- Castle AfDocument11 pagesCastle AfgustavoNo ratings yet
- Jurnal InternalDocument10 pagesJurnal InternalseptikusumaNo ratings yet
- Use of CT To Guide ManagementDocument10 pagesUse of CT To Guide ManagementnatayaregizaNo ratings yet
- Aspirin and Aspilet Compared PDFDocument18 pagesAspirin and Aspilet Compared PDFEfrianti Viorenta HutapeaNo ratings yet
- Fa y StrokeDocument11 pagesFa y StrokeCatherine Galdames HinojosaNo ratings yet
- Packer 2019Document14 pagesPacker 2019Renata D GNo ratings yet
- Defibrillation Strategies For Refractory NEJM Article 2022Document10 pagesDefibrillation Strategies For Refractory NEJM Article 2022Iurascu GeaninaNo ratings yet
- JHLT Abstract 2020-1Document1 pageJHLT Abstract 2020-1G WNo ratings yet
- Artigo HGF Neorologia Maio 2021Document11 pagesArtigo HGF Neorologia Maio 2021Daniela MarinhoNo ratings yet
- Hemicraniectomy in Older PatientsDocument10 pagesHemicraniectomy in Older PatientsMade EryanaNo ratings yet
- Endovascular Therapy For Acute Stroke With A Large Ischemic Region NEJMDocument21 pagesEndovascular Therapy For Acute Stroke With A Large Ischemic Region NEJMSubhashini KNo ratings yet
- Stenting Versus Aggressive Medical Therapy For Intracranial Arterial StenosisDocument11 pagesStenting Versus Aggressive Medical Therapy For Intracranial Arterial StenosisariNo ratings yet
- Annals of Neurology - 2021 - Polymeris - Oral Anticoagulants in The Oldest Old With Recent Stroke and Atrial FibrillationDocument11 pagesAnnals of Neurology - 2021 - Polymeris - Oral Anticoagulants in The Oldest Old With Recent Stroke and Atrial FibrillationJavier RamirezNo ratings yet
- Articles: BackgroundDocument8 pagesArticles: BackgroundrodribeatsNo ratings yet
- (19330693 - Journal of Neurosurgery) Decompressive Hemicraniectomy - Predictors of Functional Outcome in Patients With Ischemic StrokeDocument7 pages(19330693 - Journal of Neurosurgery) Decompressive Hemicraniectomy - Predictors of Functional Outcome in Patients With Ischemic StrokeRandy Reina RiveroNo ratings yet
- Ing 5Document11 pagesIng 5Farida MufidatiNo ratings yet
- Edlow 2018Document15 pagesEdlow 2018arianaNo ratings yet
- Article For Cardiogenic ShockDocument10 pagesArticle For Cardiogenic ShockGrace CallowNo ratings yet
- Provenge 2Document12 pagesProvenge 2api-675909478No ratings yet
- Catheter Ablationin in AF With CHFDocument11 pagesCatheter Ablationin in AF With CHFKristian Sudana HartantoNo ratings yet
- Davis 2008Document11 pagesDavis 2008Suchada SangpetchNo ratings yet
- Treatment Effect of Early Dual Antiplatelet Therapy in Minor StrokeDocument14 pagesTreatment Effect of Early Dual Antiplatelet Therapy in Minor Strokelemonia krakerNo ratings yet
- Goyal Et Al-2015-Annals of NeurologyDocument7 pagesGoyal Et Al-2015-Annals of NeurologyWinda Wahyu IkaputriNo ratings yet
- 2003-Academic Emergency MedicineDocument154 pages2003-Academic Emergency MedicinealiceNo ratings yet
- New England Journal Medicine: The ofDocument14 pagesNew England Journal Medicine: The ofIMNo ratings yet
- Craniectomia DescompresivaDocument51 pagesCraniectomia DescompresivaVlady78No ratings yet
- Articulo 4Document8 pagesArticulo 4Andrea OrtizNo ratings yet
- Pci On Infark MyocardDocument10 pagesPci On Infark MyocardDinny Novia WNo ratings yet
- Ischemia CKD Trial - NEJM 2020Document11 pagesIschemia CKD Trial - NEJM 2020Vicken ZeitjianNo ratings yet
- Journal 4 Nejmoa1215340 NeuroDocument9 pagesJournal 4 Nejmoa1215340 NeuroDyo O RNo ratings yet
- Atrial Fibrillation With PVC Bigeminy in RHD Patient FinalDocument2 pagesAtrial Fibrillation With PVC Bigeminy in RHD Patient FinalNathania HoswandiNo ratings yet
- Jama Kamel 2024 Oi 230163 1706898479.89128Document9 pagesJama Kamel 2024 Oi 230163 1706898479.89128Srinivas PingaliNo ratings yet
- Cairan HangatDocument20 pagesCairan HangatAbuyIlejayNo ratings yet
- Nejmoa2309137 1Document12 pagesNejmoa2309137 1maria espinozaNo ratings yet
- Incidence Severity and Detection of Blood Pressure and Heart Rate Perturbations in Postoperative Ward Patients After Noncardiac Surgery ScienceDirectDocument6 pagesIncidence Severity and Detection of Blood Pressure and Heart Rate Perturbations in Postoperative Ward Patients After Noncardiac Surgery ScienceDirectChristian OpinaldoNo ratings yet
- ATTENTION TrialDocument12 pagesATTENTION TrialmrabhilekhNo ratings yet
- CourageDocument14 pagesCourageSuryaNo ratings yet
- Jamaneurology Jiang 2018 Oi 180048Document9 pagesJamaneurology Jiang 2018 Oi 180048jonas lopetNo ratings yet
- Antiagregacion Vs Anticoagulacion en DiseccionDocument4 pagesAntiagregacion Vs Anticoagulacion en DiseccionCarlos Alberto CorredorNo ratings yet
- Innovations in Modern Endocrine SurgeryFrom EverandInnovations in Modern Endocrine SurgeryMichael C. SingerNo ratings yet
- Xodo Document - Periprocedural - Anticoagulation - GuidelineDocument16 pagesXodo Document - Periprocedural - Anticoagulation - Guidelinebrigde_xNo ratings yet
- Perioperative Considerations and Management of Patients Receiving AnticoagulantsDocument7 pagesPerioperative Considerations and Management of Patients Receiving Anticoagulantsdrvasantha 8No ratings yet
- Asra Anticoag Guidelines PDFDocument47 pagesAsra Anticoag Guidelines PDFVijaya JagtapNo ratings yet
- Basic Principles of Platelet Biology and Clinical ImplicationsDocument11 pagesBasic Principles of Platelet Biology and Clinical ImplicationsIsmael Rivera DiazNo ratings yet
- Dual Antiplatelet Therapy Benefits for Prior MI PatientsDocument40 pagesDual Antiplatelet Therapy Benefits for Prior MI PatientsKarren Taquiqui PleteNo ratings yet
- Cilostazol (Pletal)Document4 pagesCilostazol (Pletal)Maria Leonie Dela CruzNo ratings yet
- Pegasus TIMI 54 TrialDocument13 pagesPegasus TIMI 54 TrialIsaac Aaron Enriquez MonsalvoNo ratings yet
- Document PDFDocument4 pagesDocument PDFDebasis SahooNo ratings yet
- Antithrombotic DrugsDocument11 pagesAntithrombotic DrugsKatyBrnNo ratings yet
- Bonello 2018Document15 pagesBonello 2018Илија РадосављевићNo ratings yet
- Antiplatelet DrugsDocument31 pagesAntiplatelet DrugsSyed Usama Rashid100% (2)
- Pertemuan 7 LiyanaDocument36 pagesPertemuan 7 LiyanaLiyana SafitriNo ratings yet
- THE COMPARISON OF PERKI 2015 AND ESC 2018 GUIDELINE FOR HYPERTENSION MANAGEMENTDocument80 pagesTHE COMPARISON OF PERKI 2015 AND ESC 2018 GUIDELINE FOR HYPERTENSION MANAGEMENTAlif RochmahNo ratings yet
- Brilinta RXDocument10 pagesBrilinta RXravi_bhateja_2No ratings yet
- Preoperative Preparation and Postoperative CareDocument103 pagesPreoperative Preparation and Postoperative Carechowhan04No ratings yet
- Voltaren Rapide - Scrip - eDocument39 pagesVoltaren Rapide - Scrip - eRandom2319No ratings yet
- Classification of Antiplatelet AgentsDocument5 pagesClassification of Antiplatelet AgentsWita Ferani KartikaNo ratings yet
- 03-Ischemic Heart Disease - 2020 OngoingDocument151 pages03-Ischemic Heart Disease - 2020 OngoingDana MohammadNo ratings yet
- Building Your Peripheral Artery Disease Toolkit MDocument11 pagesBuilding Your Peripheral Artery Disease Toolkit MehaffejeeNo ratings yet
- CPG Primary & Secondary Prevention of Cardiovascular DiseaseDocument182 pagesCPG Primary & Secondary Prevention of Cardiovascular Diseasewaniaqilah workNo ratings yet
- CPG Management of Ischaemic Stroke 3rd Edition 2020 v20210228Document156 pagesCPG Management of Ischaemic Stroke 3rd Edition 2020 v20210228Nabilah HariffNo ratings yet
- Aspirin and Aspilet Compared PDFDocument18 pagesAspirin and Aspilet Compared PDFEfrianti Viorenta HutapeaNo ratings yet
- GI Bleeding in Patients Receiving Antiplatelets and Anticoagulant TherapyDocument11 pagesGI Bleeding in Patients Receiving Antiplatelets and Anticoagulant TherapyTony LeeNo ratings yet
- Aew 214Document11 pagesAew 214Heather PorterNo ratings yet