Professional Documents
Culture Documents
Respiratory Distress in Newborn: Learning Objectives
Uploaded by
Satya Prakash TiwariOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Respiratory Distress in Newborn: Learning Objectives
Uploaded by
Satya Prakash TiwariCopyright:
Available Formats
Chapter 10
RESPIRATORY DISTRESS IN NEWBORN
Respiratory distress accounts for significant morbidity and mortality in neonates. It
occurs in 4 to 6 percent of neonates. Many of the conditions causing respiratory distress
are preventable. Early recognition and prompt management are required
Learning objectives
After completion of this module the participant should be able to-
• Diagnose common causes of respiratory distress in Term and Preterm newborns
• Identify babies with respiratory distress and assess severity of respiratory distress
• Deliver oxygen and manage babies with respiratory distress
• Monitor babies on oxygen therapy
Common causes of respiratory distress
Preterm baby
• Respiratory distress syndrome
• Congenital Pneumonia
• Miscellaneous causes: hypothermia, hypoglycemia
Term baby
• Transient tachypnea of newborn (TTNB)
• Meconium aspiration
• Pneumonia,
• Asphyxia
Surgical causes
• Diaphragmatic hernia
• Tracheo-esophageal fistula
• B/L choanal atresia
Other causes
• Cardiac
• Metabolic
NATIONAL NEONATOLOGY FORUM
61
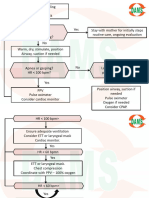
Approach to respiratory distress
History A detailed relevant antenatal and perinatal history should be taken based on the
common causes:
• Gestation
• Onset of distress
• Previous preterm babies with respiratory distress
• Antenatal steroid prophylaxis if preterm delivery
• Rupture of Membranes > 24 hours, Intrapartum fever, chorioamnionitis
• Meconium stained amniotic fluid
• Asphyxia
• Maternal diabetes mellitus
Examination
• Severity of respiratory distress
• Neurological status
• CFT
• Hepatomegaly
• Cyanosis
• Features of sepsis
• Look for malformations
Assessment of severity of respiratory distress
Table 10.1: Silverman Anderson Score and its interpretation
Score Upper chest Lower chest Xiphoid Nasal Grunt
retraction retraction retraction flaring
0 Synchronised None None None None
1 Lag during Just visible Just visible Minimal Audible with
inspiration Stethoscope
2 See-Saw Marked Marked Marked Audible with
unaided ear
Interpretation
Score 0-3 = Mild respiratory distress – O2 by hood
Score 4-6 = Moderate respiratory distress - CPAP
Score > 6 = Impending respiratory failure
Table 10.2 : Downe’s score and its interpretation
NATIONAL NEONATOLOGY FORUM
62
Score Respiratory Cyanosis Air entry Grunt Retraction
rate
0 <60/min Nil Normal None Nil
1 60-80/min In room air Mild Audible with Mild
decrease Stethoscope
2 >80/min In >40% Marked Audible with Moderate
FiO2 decrease unaided ear
Interpretation
Score <6 = Respiratory distress
Score > 6 = Impending respiratory failure
Investigations
The diagnosis is based on the x-ray findings and the sepsis screen.
Chest X-ray
To look for
• Respiratory Distress Syndrome (RDS) - Air bronchogram, decreased lung volume
and hazy lungs
• Meconium Aspiration Syndrome (MAS) - Fluffy shadows involving both lungs
with hyperinflation
• Pneumonia - Infiltrates
• Pulmonary hemorrhage, RDS - White out (Opaque lung)
Sepsis screen : TLC, DLC, CRP, Micro ESR, IT Ratio, ANC
Blood Culture: This may give a clue to the infectious etiology of the respiratory distress
Management
General management
• Give oxygen with oxygen hood or nasal cannula to achieve appropriate oxygen
saturation
• Maintain normal body temperature (see section on hypothermia)
• Give IV fluids if the baby does not accept feeds or has severe respiratory distress
• Maintain blood glucose, if low treat hypoglycemia
• If baby has apnea
a. Stimulate to breathe by rubbing the back or flicking the sole
b. If does not begin to breathe immediately provide positive-pressure
ventilation with bag and mask
c. Aminophylline if baby is preterm
NATIONAL NEONATOLOGY FORUM
63
d. If recurrent apneic spells, treat for sepsis and organize transfer to a
specialized centre for assisted ventilation.
Specific management
Moderate to Severe breathing difficulty
• Monitor and record the baby’s respiratory rate, presence of chest indrawing or
grunting on expiration, and episodes of apnoea every hour until the baby no longer
requires oxygen and then for an additional 24 hours.
• Monitor the baby’s response to oxygen by oxygen saturations.
• Insert an oro-gastric tube to empty the stomach of air and secretions.
• After taking a sepsis screen including blood culture start antibiotics.
• When the baby begins to show signs of improvement:
o Give expressed breast milk by oro-gastric tube
o Allow the baby to begin breastfeeding as the respiratory distress settles. Baby can
be put on to breast while on oxygen by nasal cannula with continuous monitoring.
o If the baby cannot be breastfed, give expressed breast milk using a cup & spoon
or paladai.
TABLE 10.3: Methods for administering oxygen
Method Nasal catheter Head box
Flow • Low = 0.5 L per minute • Low = 3 L per minute
• Moderate = 0.5 to 1 L per min • Moderate = 3 to 5 L per min
• High = more than 1 L per min • High = more than 5 L per min
Nasal Prongs :
These are a useful means of delivering oxygen. Appropriate size prongs, which fit the
neonate well, should be used. If a large size of the nasal cannula is used, it may cause
blanching of the ala nasi and injure the nose.
NATIONAL NEONATOLOGY FORUM
64
Nasal Catheter
• Use a 6-8 french catheter.
• Determine the distance the tube should be passed by measuring the distance from the
nostril to the inner margin of the eyebrow.
• Gently insert the catheter into the nostril.
• Ensure that the catheter is correctly positioned.
- Look into the baby’s mouth;
- The catheter should not be visible at the back of the mouth;
- If the catheter is visible at the back of the mouth, pull the catheter out slowly until it
is no longer visible.
• Adjust the flow of oxygen to achieve the desired oxygen saturation.
• Change the nasal catheter twice daily. Give oxygen using a face mask while changing
the catheter if necessary.
Head Box
• Place a head box over the baby’s head.
• Ensure that the baby’s head stays within the head box, even when the baby moves.
• Adjust the flow of oxygen to achieve the desired oxygen saturation.
If the baby’s breathing difficulty worsens or the baby is desaturating or has central
cyanosis:
• Give oxygen at a high flow rate
• If breathing difficulty is so severe that the baby has central cyanosis even in 100%
oxygen, organize transfer and urgently refer the baby to a tertiary hospital or
specialized centre capable of assisted ventilation.
If investigations reveal evidence of sepsis, stop antibiotics after 7 – 10 day and observe
the baby for 24 hours after discontinuing antibiotics.
If the baby’s oxygen saturation on pulse oximetry are acceptable, gradually wean from
oxygen. If he baby has no difficulty breathing and is feeding well, discharge the baby.
Pulse oximetry : Maintain a saturation of 88 – 92% in preterm and 90-93 % in term
neonates
NATIONAL NEONATOLOGY FORUM
65
Mild breathing difficulty
• Monitor for respiratory distress and oxygen saturation. Give oxygen if needed.
• Give expressed breast milk by gastric tube
• When oxygen is no longer needed, allow the baby to begin breastfeeding. If the baby
cannot be breastfed, continue giving expressed breast milk using an alternative
feeding method.
• If the breathing difficulty worsens at any time during the observation period: treat for
moderate breathing difficulty
• All babies with mild and transient respiratory distress, do not need antibiotics.
However, if the respiratory distress persists for more than 6 hour or there are risk
factors, start antibiotics after taking a sepsis screen. Once respiratory distress settles
and the sepsis screen is negative – STOP ANTIBIOTICS.
Antenatal corticosteroids for prevention of RDS
• Antenatal corticosteroid therapy is a simple and effective therapy that
prevents RDS.
• Optimal effect of antenatal steroids is seen if delivery occurs after 24 hrs of
starting therapy.
• Recommended Dose is Inj Betamethasone 12 mg IM every 24 hrs X 2 doses or
Inj. Dexamethasone 6 mg IM every 12 hrs X 4 doses.
• Give to mothers with preterm labour or APH before 34 wks of gestation.
NATIONAL NEONATOLOGY FORUM
66
VIDEO DEMONSTRATION OF DIFFICULTY IN BREATHING
This video demonstrates a neonate with fast breathing, chest retractions, nasal flaring and
grunting.
NATIONAL NEONATOLOGY FORUM
67
EVALUATION
A 7 day old baby born at term with a birth weight of 2.8 kg is brought with complaints of
difficulty in breathing and inability to feed at the breast. The present weight is 2.65 kg,
temperature is 36oC, and respiratory rate is 96 / min with moderate retraction with
grunting and central cyanosis.
1. What is your assessment about the respiratory status of this baby and what is the likely
diagnosis?
_____________________________________________________________________
_____________________________________________________________________
_____________________________________________________________________
_____________________________________________________________________
2. What supportive management would you do for this baby?
_____________________________________________________________________
_____________________________________________________________________
_____________________________________________________________________
_____________________________________________________________________
3. What are the ways of giving oxygen to the baby and how will you monitor efficacy of
oxygen delivery.
_____________________________________________________________________
_____________________________________________________________________
_____________________________________________________________________
_____________________________________________________________________
4. A baby is born prematurely at 32 weeks of gestation and develops respiratory distress
soon after birth with grunting and chest retractions. What is the likely diagnosis.
_____________________________________________________________________
_____________________________________________________________________
_____________________________________________________________________
_____________________________________________________________________
5. What are the principles of management of severe breathing difficulty?
_____________________________________________________________________
_____________________________________________________________________
_____________________________________________________________________
_____________________________________________________________________
6. How will you manage a baby who is brought with breathing difficulty and develops
apneic spells.
_____________________________________________________________________
_____________________________________________________________________
_____________________________________________________________________
____________________________________________________________________
NATIONAL NEONATOLOGY FORUM
68
You might also like
- Mutants & Masterminds 3e - Power Profile - Death PowersDocument6 pagesMutants & Masterminds 3e - Power Profile - Death PowersMichael MorganNo ratings yet
- NeonatalresuscitationDocument67 pagesNeonatalresuscitationfidaNo ratings yet
- Test Bank For Cognitive Psychology Connecting Mind Research and Everyday Experience 3rd Edition e Bruce GoldsteinDocument24 pagesTest Bank For Cognitive Psychology Connecting Mind Research and Everyday Experience 3rd Edition e Bruce GoldsteinMichaelThomasyqdi100% (49)
- The Structure of The Nazi Economy - Maxine Yaple SweezyDocument273 pagesThe Structure of The Nazi Economy - Maxine Yaple Sweezygrljadus100% (2)
- Pediatric Emergency Summary For Osce ExamDocument84 pagesPediatric Emergency Summary For Osce ExamAlwaallh Mohammed100% (1)
- Mwami Schools of Nursing and Midwifery: by Baldwin Hamoonga 5 Year Nursing Student (Ru) Topic: Small For Dates BabyDocument26 pagesMwami Schools of Nursing and Midwifery: by Baldwin Hamoonga 5 Year Nursing Student (Ru) Topic: Small For Dates BabyBaldwin Hamzcorp HamoongaNo ratings yet
- New Born ResuscitationDocument34 pagesNew Born ResuscitationPAUL NDEKINo ratings yet
- CroupDocument13 pagesCroupEdu William100% (1)
- Neonatal Resuscitation: Vineetha.T 1 Year MSC NursingDocument106 pagesNeonatal Resuscitation: Vineetha.T 1 Year MSC NursingVineetha ThachedathNo ratings yet
- Neonatal ResuscitationDocument15 pagesNeonatal Resuscitationpriyanka88% (8)
- Triase Dan KegawatdaruratanDocument89 pagesTriase Dan KegawatdaruratanDarma KomboNo ratings yet
- HypothermiaDocument5 pagesHypothermiaMRS CHAKRAPANINo ratings yet
- Breastfeeding PDFDocument11 pagesBreastfeeding PDFSatya Prakash TiwariNo ratings yet
- Neonatal ResuscitationDocument15 pagesNeonatal ResuscitationAmruta GadeNo ratings yet
- Asphyxia NeonatorumDocument34 pagesAsphyxia NeonatorumListya Paramita100% (1)
- Respiratory Management in Pediatrics PDFDocument68 pagesRespiratory Management in Pediatrics PDFPAKINUGNo ratings yet
- Dr. Rosi - CPAPDocument65 pagesDr. Rosi - CPAPtom24No ratings yet
- Dialogue About Handling ComplaintDocument3 pagesDialogue About Handling ComplaintKarimah Rameli100% (4)
- ARI Control ProgrammeDocument13 pagesARI Control ProgrammeArun George50% (8)
- Neonatal ResuscitationDocument19 pagesNeonatal ResuscitationDavina DakapNo ratings yet
- NRPDocument15 pagesNRPmohamed mowafeyNo ratings yet
- Neonatal Resuscitation JincyDocument78 pagesNeonatal Resuscitation JincyVivek PrabhakarNo ratings yet
- 39 Neonatal ResuscitationDocument38 pages39 Neonatal ResuscitationbenNo ratings yet
- Immediate Physical CareDocument73 pagesImmediate Physical CareronelnNo ratings yet
- Neonatal ResuscitationDocument138 pagesNeonatal ResuscitationAbcdeNo ratings yet
- Neonatal Resuscitation - 1 8 10Document54 pagesNeonatal Resuscitation - 1 8 10drkiranmNo ratings yet
- Birth AsphyxiaDocument10 pagesBirth Asphyxiasarita Singh MaharjanNo ratings yet
- Cough and Dyspnea Case StudyDocument4 pagesCough and Dyspnea Case StudyAbigail Balbuena100% (1)
- Bronchiolitis Starship GuidelineDocument7 pagesBronchiolitis Starship Guidelinechicky111No ratings yet
- Cme NRPDocument73 pagesCme NRPpayapaya.pipacyclineNo ratings yet
- Welcome RSVDocument32 pagesWelcome RSVapi-260357356No ratings yet
- Tracheoesophageal Fistula: Case PresentationDocument50 pagesTracheoesophageal Fistula: Case PresentationAmit KochetaNo ratings yet
- Respiratory Disorders 2.1Document70 pagesRespiratory Disorders 2.1Deenjane Nishi IgnacioNo ratings yet
- Chapter 24Document26 pagesChapter 24Susanna ConigliaroNo ratings yet
- Pedia Concepts 2:: From Respiratory Problems To HematologicDocument119 pagesPedia Concepts 2:: From Respiratory Problems To HematologicarudarbmeeNo ratings yet
- Acute Conditions of The NeonatesDocument4 pagesAcute Conditions of The NeonatesShermina JalaniNo ratings yet
- Special Neonatal ConditionsDocument37 pagesSpecial Neonatal ConditionsSanthosh.S.UNo ratings yet
- Neonatal ResuscitationDocument51 pagesNeonatal ResuscitationAbdulkadir HasanNo ratings yet
- Respiratory Distress SyndromeDocument13 pagesRespiratory Distress SyndromeKenneth UbaldeNo ratings yet
- Asphyxia Ik 2Document74 pagesAsphyxia Ik 2Ste VenNo ratings yet
- Neonatal CareDocument59 pagesNeonatal CareKeith LajotNo ratings yet
- ITISMITA Biswal MSC, Nursing 2 YearDocument48 pagesITISMITA Biswal MSC, Nursing 2 YearGandimareiNo ratings yet
- Physiologic Assessment of Newborn, Newborn Adaptation and Normal Growth & DevelopmentDocument4 pagesPhysiologic Assessment of Newborn, Newborn Adaptation and Normal Growth & DevelopmentBernard M. Lapuz FullNo ratings yet
- Delivery and Care of The NewbornDocument57 pagesDelivery and Care of The NewbornJerry AbleNo ratings yet
- DR D R Aryal May, 2014Document109 pagesDR D R Aryal May, 2014kamalshrishNo ratings yet
- Neonatal Resuscitation in FMC NigeriaDocument55 pagesNeonatal Resuscitation in FMC NigeriaIghodaro IsokenNo ratings yet
- Immediate Care of The NewbornDocument3 pagesImmediate Care of The NewbornBianca CamilleNo ratings yet
- Immediate Care of NewbornDocument4 pagesImmediate Care of NewbornjvjohnNo ratings yet
- Meconium Aspiration: Evolve. Adapt. Overcome. Is Now ReadyDocument19 pagesMeconium Aspiration: Evolve. Adapt. Overcome. Is Now ReadyPrincess Loreto AlegreNo ratings yet
- 9 10 2010 0-42-42 R Neonatal-ResuscitationDocument21 pages9 10 2010 0-42-42 R Neonatal-ResuscitationSamsiah ChaNo ratings yet
- Nclex (1301) (1) (1315)Document43 pagesNclex (1301) (1) (1315)Elizabeth SharmaNo ratings yet
- Transient Tachypnea of The Newborn: Fetal LungDocument5 pagesTransient Tachypnea of The Newborn: Fetal LungNurul HafizahNo ratings yet
- II. AsfiksiaDocument41 pagesII. AsfiksiahazelelNo ratings yet
- Immediate Care of The NewbornDocument4 pagesImmediate Care of The Newbornmelinda100% (1)
- Help Baby To BreathDocument49 pagesHelp Baby To BreathmohdmaghyrehNo ratings yet
- Neonatal Resuscitation ProgramDocument40 pagesNeonatal Resuscitation ProgramJharaNo ratings yet
- 01 - Management of Critically Ill ChildrenDocument42 pages01 - Management of Critically Ill ChildrenMin MinTheinNo ratings yet
- 17 Jan - Paediatrics (DR Ashutosh) DAMS DVT 2022Document60 pages17 Jan - Paediatrics (DR Ashutosh) DAMS DVT 2022Lutfi HakimNo ratings yet
- Skenario E Blok 23 Kelompok 3: Tutor: DR - Nursanti Apriyanti, SP - PADocument20 pagesSkenario E Blok 23 Kelompok 3: Tutor: DR - Nursanti Apriyanti, SP - PAMentari Indah SariNo ratings yet
- Pediatric Advanced Life Support: Jan Bazner-Chandler CPNP, CNS, MSN, RNDocument65 pagesPediatric Advanced Life Support: Jan Bazner-Chandler CPNP, CNS, MSN, RNد. محمد فريد الغنامNo ratings yet
- Respiratory Distress SyndromeDocument54 pagesRespiratory Distress SyndromeKristine CaringalNo ratings yet
- Nasal IMV - Gatot PDFDocument43 pagesNasal IMV - Gatot PDFtutiarlyNo ratings yet
- Asphyxia Neonatorum Main GRP 1 WorkDocument10 pagesAsphyxia Neonatorum Main GRP 1 WorkChelsy RomaNo ratings yet
- Asphyxia 2Document55 pagesAsphyxia 2api-19916399100% (1)
- Neonatalresuscitationmanual2 PDFDocument75 pagesNeonatalresuscitationmanual2 PDFSatya Prakash TiwariNo ratings yet
- Equipment Demonstration: National Neonatology ForumDocument53 pagesEquipment Demonstration: National Neonatology ForumSatya Prakash TiwariNo ratings yet
- Fluid Management: Learning ObjectivesDocument6 pagesFluid Management: Learning ObjectivesSatya Prakash TiwariNo ratings yet
- Neonatal Sepsis: Learning ObjectivesDocument10 pagesNeonatal Sepsis: Learning ObjectivesSatya Prakash TiwariNo ratings yet
- NRP PDFDocument6 pagesNRP PDFSatya Prakash TiwariNo ratings yet
- Neonatal Seizures: Learning ObjectivesDocument6 pagesNeonatal Seizures: Learning ObjectivesSatya Prakash TiwariNo ratings yet
- Emergency Triage Assessment and Treatment: National Neonatology ForumDocument6 pagesEmergency Triage Assessment and Treatment: National Neonatology ForumSatya Prakash TiwariNo ratings yet
- Care of A Normal Newborn at Birth and Beyond: Learning ObjectivesDocument8 pagesCare of A Normal Newborn at Birth and Beyond: Learning ObjectivesSatya Prakash TiwariNo ratings yet
- EEN 203 Slide Notes Year 2018: PART I - Numbers and CodesDocument78 pagesEEN 203 Slide Notes Year 2018: PART I - Numbers and CodesSHIVAM CHOPRANo ratings yet
- Lyndhurst OPRA Request FormDocument4 pagesLyndhurst OPRA Request FormThe Citizens CampaignNo ratings yet
- Peacekeepers: First Term ExamDocument2 pagesPeacekeepers: First Term ExamNoOry foOT DZ & iNT100% (1)
- Hayat ProposalDocument22 pagesHayat Proposalsebehadinahmed1992No ratings yet
- GMAT Sentence Correction Practice Test 03Document5 pagesGMAT Sentence Correction Practice Test 03krishnachivukulaNo ratings yet
- Maratua Island Survey ReportDocument8 pagesMaratua Island Survey ReportJoko TrisyantoNo ratings yet
- Ham (Son of Noah) - WikipediaDocument3 pagesHam (Son of Noah) - Wikipediamike bNo ratings yet
- JurisprudenceDocument11 pagesJurisprudenceTamojit DasNo ratings yet
- Vocabulary Inglés.Document14 pagesVocabulary Inglés.Psicoguía LatacungaNo ratings yet
- Does Social Media Influence Consumer Buying Behavior An Investigation of Recommendations and PurchasesDocument7 pagesDoes Social Media Influence Consumer Buying Behavior An Investigation of Recommendations and Purchasesyash_28No ratings yet
- Peptic UlcerDocument48 pagesPeptic Ulcerscribd225No ratings yet
- Filipino Chicken Cordon BleuDocument7 pagesFilipino Chicken Cordon BleuHazel Castro Valentin-VillamorNo ratings yet
- ViTrox 20230728 HLIBDocument4 pagesViTrox 20230728 HLIBkim heeNo ratings yet
- Especificação - PneusDocument10 pagesEspecificação - Pneusmarcos eduNo ratings yet
- Evolution Epidemiology and Etiology of Temporomandibular Joint DisordersDocument6 pagesEvolution Epidemiology and Etiology of Temporomandibular Joint DisordersCM Panda CedeesNo ratings yet
- CO-PO MappingDocument6 pagesCO-PO MappingArun Kumar100% (1)
- EFL Listeners' Strategy Development and Listening Problems: A Process-Based StudyDocument22 pagesEFL Listeners' Strategy Development and Listening Problems: A Process-Based StudyCom DigfulNo ratings yet
- Adrenal Cortical TumorsDocument8 pagesAdrenal Cortical TumorsSabrina whtNo ratings yet
- PH Water On Stability PesticidesDocument6 pagesPH Water On Stability PesticidesMontoya AlidNo ratings yet
- Sorsogon State College: Republic of The Philippines Bulan Campus Bulan, SorsogonDocument4 pagesSorsogon State College: Republic of The Philippines Bulan Campus Bulan, Sorsogonerickson hernanNo ratings yet
- Anglicisms in TranslationDocument63 pagesAnglicisms in TranslationZhuka GumbaridzeNo ratings yet
- A Mercy Guided StudyDocument23 pagesA Mercy Guided StudyAnas HudsonNo ratings yet
- 12-Zoomlion 70t Crawler Crane Specs - v2.4Document2 pages12-Zoomlion 70t Crawler Crane Specs - v2.4Athul BabuNo ratings yet
- HSE Induction Training 1687407986Document59 pagesHSE Induction Training 1687407986vishnuvarthanNo ratings yet
- Chapter 14ADocument52 pagesChapter 14Arajan35No ratings yet
- Seminars - 09-12-2022 - Vanessa AQUINO CHAVESDocument3 pagesSeminars - 09-12-2022 - Vanessa AQUINO CHAVESVanessa AquinoNo ratings yet