Professional Documents
Culture Documents
Exercise7 (Histo) Digestive System Edited
Uploaded by
Christi Lorraine LayogOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Exercise7 (Histo) Digestive System Edited
Uploaded by
Christi Lorraine LayogCopyright:
Available Formats
Zoology 115 Animal Histology Laboratory Exercises 1
Exercise 7
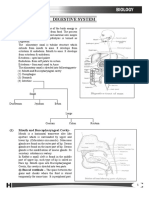
THE DIGESTIVE SYSTEM
The digestive system consists of a long, tortuous tube that begins at the lips and ends at the
anus. During ontogeny, the digestive system initially develops as a closed, endodermal-lined
mesenchymal tube, which secondarily gains communication with the external (ectodermal) surface of
the embryo by the rupture of the oral and anal membranes. Thus, in the adult, the digestive system is
continuous with the external surface of the body only at the oral and anal openings.
The digestive system is a continuous series of organs that are involved in the intake and
propulsion of food, its mechanical and chemical breakdown (digestion), the absorption of a portion of
the digested substances, and the elimination of undigested material from the body. It may be
subdivided into: (1) the oral cavity; (2) the pharynx; (3) the alimentary tract or canal and (4) the anal
canal. In addition to this elongate tubular portion of the digestive system, there are both intrinsic and
extrinsic glands derived from the primitive tubular gut; these glands may elaborate digestive enzymes
or mucus to facilitate the digestion and transport of foodstuffs. The intrinsic glands lie within the
mucosa or submucosa of their organ of origin, and will be discussed with each of these organs. The
extrinsic glands communicate with their organ of origin by means of excretory ducts. A useful concept
in the study of extrinsic glands is that the site of termination of their excretory ducts denotes their
embryological origin. Thus, the opening of the common bile duct into the duodenum is a reminder that
both the liver and the pancreas develop as outgrowths from the foregut (duodenum). The extrinsic
digestive glands are: (1) the major salivary glands - the parotid, sublingual and submandibular
(submaxillary) glands; (2) the pancreas; and (3) the liver. These are the subject of the next laboratory.
The following is the general structural plan that is characteristic for most of the digestive
system. Typically, there are 4 concentric coats; proceeding outward from the lumen, these are: (1) the
mucosa (mucous membrane); (2) the submucosa; (3) the muscularis (muscularis externa); and (4) the
adventitia or serosa.
1. The mucosa has three components: (a) the epithelium and its underlying basement
membrane; (b) a thin underlying layer of loose, cellular connective tissue, the lamina propria; and (c) a
relatively thin layer of smooth muscle, the muscularis mucosae. The latter may consist of both circular
and longitudinally arranged layers.
2. The submucosa is composed of a layer of dense, irregularly arranged connective tissue that
contains nervous tissue (the submucosal plexus of Meissner), as well as blood vessels.
3. The muscularis externa consists of at least 2 layers of smooth muscle; an inner circular and
outer longitudinal layer. Connective tissue, separating the muscle layers, contains nerves (myenteric
plexus of Auerbach) and blood vessels.
4. The outermost layer or adventitia consists of a thin layer of loose connective tissue; where the
digestive system is covered by peritoneum the adventitial layer is called the serosa.
Locate and label specific parts mentioned in bold face.
OBJECTIVES: After completing the laboratory exercises for the digestive system, you should be able
to:
● Identify in the light microscope sections of the oral cavity, esophagus, stomach, and intestines.
● Determine the fundamental organization of the GI tract and how it is modified along its course
from the esophagus through large intestine.
● Identify in the light microscope sections of the liver, pancreas, and gall bladder.
ATES-CAMINO, Fritzie B. (AY 2011-2012), BSES-CSM, UPMindanao
Zoology 115 Animal Histology Laboratory Exercises 2
The Oral Cavity
The oral cavity is the first portion of the digestive tract, and consists of the mouth and the
structures which are enclosed within it. The mouth isn't merely a hole in the face. It's a complex
structure with nutritional, respiratory, and communicative functions in all mammals and most other
groups of animals.
Additionally, it serves as the principal means of manipulating the environment for those animals
which don't have hands, such as dogs. A dog carries things in his mouth because he has no other way to
do it.
Accessory structures which contribute to the mouth's function include the tongue, the teeth, and
the salivary glands.
1. The Oral Epithelium, The Lip, H&E
Examine a section of the oral sideof the lip. Notice that the epithelial lining of the oral cavity is
of the stratified squamous type. In contrast to the skin it is nonkeratinized. The oral cavity side totally
lacks any of the adnexal structures associated with skin: no hairs, sebaceous or sweat glands, etc. The
place of continuity between the "dry" integument and the "wet" oral mucosa is located at the top of this
section. This sort of transition point is a mucocutaneous junction. Mucocutaneous junctions exist in
several other sites: the anus, the nostrils, the vulva and the urethra.
2. The Tongue, H&E
The tongue is easily recognized because of its interlacing bundles of skeletal muscle that are
disposed in three planes, all at right angles to each other, and by its covering of stratified squamous
epithelium that is elevated on the dorsal surface of the tongue, into papillae. These special regions of
the stratified squamous epithelium covers the entire organ. There are three types of papillae in man:
filiform, fungiform and cicumvallate. A fourth type, which is not well-developed in man is the foliate
papilla.
Locate the tongue's dorsal surface by focusing on the organ's epithelial region and notice the
numerous filiform papillae. These are slender conical structures, which project upwards forming a
velvety covering on the tongue. Its function is purely mechanical; it has no sensory structures
associated with it, as do the others. In some species (such as cats and cattle) filiform papillae are
extremely large and rough, and the peculiar rasping effect of a cat's tongue is due to these papillae. It's
also what a cat uses to clean her fur. The stiff papillae make effective bristles for removing debris. The
filiform papillae are by far the most common type, and sometimes are "swallow tailed" in shape.
The remaining types of lingual papillae are sensory in function. They include: the fungiform
papillae, which are less common than the filiforms; the vallate (or circumvallate) the largest and most
prominent; and the foliate papillae, which are most easily seen in the Order Lagomorpha (rabbits,
hares, and conies).
A vallate papilla is set into a deep pocket in the tongue's surface, and anchored at the bottom
by a short broad stalk. It doesn't protrude above the general level of the surface by much, but it's
surrounded by a deep "moat" into which some of the lingual salivary glands secrete. Vallate papillae
are easily visible with the naked eye in most animals. They're paired and located near the back of the
tongue. They're the least numerous type. This very large structure has a core of connective tissue (CT)
and nerve fibers are often seen in it, serving the taste buds. Taste buds (TB) are present on the sides of
the papilla, and also frequently on the side of the moat. Taste buds, seen as well defined, lightly
staining areas which enclose several banana shaped sensory transducer cells. The sensory cells of the
ATES-CAMINO, Fritzie B. (AY 2011-2012), BSES-CSM, UPMindanao
Zoology 115 Animal Histology Laboratory Exercises 3
buds are located below the level of the epithelium, and they communicate with the outside via a so-
called taste pore, a break in the epithelium.
The fungiform papillae, as the name implies, are mushroom shaped structures. They rise above
the general level of the filiform papillae, and they usually have taste buds. Fungiform papillae are far
less numerous than the filiform type, and scattered in among them. They're not nearly as large as the
vallate papillae, but they are large enough to have a core of CT. The fungiform papillae stick up above
the surrounding filiforms, and here you can see the relationship pretty well. A swallow-tailed filiform
papilla flanks this fungiform one on either side.
The foliate papilla is best seen in rabbits. The term means "leaflike" as in the leaves of a book.
They are set in the sides of the tongue. The papillae themselves are flat-topped and have deep clefts
between them. The clefts are lined with epithelium, and there are taste buds embedded in them.
3. The Salivary Glands, Parotid Gland, Human, H&E
The parotids are the largest of the salivary glands but produce only about 30% of the saliva.
They are generally described as purely serous glands. Differentiate connective tissue stroma from
parenchyma (secretory cells and ducts). With advancing age white adipose tissue infiltrates the human
parenchyma. Dense connective tissue roughly divides the gland into lobules. The interlobular
connective tissue contains the larger excretory ducts as well as nerves and blood vessels. Note the
arrangement of the serous acinar secretory cells. The zymogenic granules in the apices of the cells are
small and variable in staining reaction. Find representative intralobular ducts, namely, the small
intercalated and larger striated ducts. The striated ducts are best seen in the human H&E slide
although they are not easy to distinguish. The nuclei of the cells that line the striated ducts are closer to
the apical surface. Infoldings of the basal membrane of the striated duct cells result in the unusual
location of the nuclei. The nuclei of intercalated duct cells are in the center of the cell.
4. The Salivary Gland, Submandibular Gland, H&E
These glands produce about 65% of the saliva and are of the mixed seromucous type. Like the
parotids the parenchyma of these glands is divided into lobules by connective tissue septa. Note serous
secretory acini are far more numerous than mucous types. Some of the mucous secretory units are
capped with serous demilunes (see atlas). Try to find intercalated and striated secretory ducts in the
lobules and the larger ducts into which these drain located in the interlobular connective tissue.
The Alimentary Canal
1. The Esophagus
The esophagus is a distensible cranial portion of the tract, formed as a simple tube. At the top it
receives a food bolus from the pharynx, and at the bottom it discharges it into the first portion of the
stomach. Diagnostic features of the esophagus are the combination of stratified squamous surface
epithelium, the considerable thickness of the muscularis mucosae (up to 0.2 - 0.4 mm thick). In the
upper third the muscularis externa contains largely skeletal muscle, in the middle third, a mixture
of skeletal and smooth, and in the lower third, only smooth muscle.
a. Human, Middle Third, H&E
Try to identify the layers of the esophagus. The lumen is surrounded by the mucosa. Note non-
keratinized stratified squamous epithelium lining the lumen. As in both the oral cavity and in the
ATES-CAMINO, Fritzie B. (AY 2011-2012), BSES-CSM, UPMindanao
Zoology 115 Animal Histology Laboratory Exercises 4
pharynx, the mucosal surface of the esophagus is lined by stratified squamous epithelium that is
nonkeratinized in man. In herbivores, the esophagus has a keratinized epithelium.In most sections, the
lamina propria and the muscularis mucosa are poorly developed at this level. But note the distinct
muscularis mucosa (smooth muscle cut mostly transversely). It separates a delicate lamina propria
from the more robust submucosa.
The submucosa is well developed. Mucous type glands may be found in the submucosa of the
human esophagus. These are referred to as esophageal glands proper, a term that implies they're a
specific part of this organ, and are distinct from glands in the mucosal layer.
In the upper portion of the esophagus in most, if not all, mammals, the muscularis externa is
composed of skeletal muscle arranged in two layers (ill-defined): inner circular and outer
longitudinal. In the middle third section of the esophagus, however, a mix of skeletal and smooth
muscle constitute the muscularis externa.The well-developed muscularis externa and the stratified
squamous epithelial lining are well adapted for the rapid transport of food from the pharynx to the
stomach.
Identify the outermost layer of the esophagus in this section, the adventitia.
Question: What type of tissue comprises the submucosa?
b. Human, Lower Third, H&E
Focus on the muscularis externa and notice that the skeletal muscle is replaced by smooth
muscle as one descends deeper into the organ; the muscularis externa near the junction with the
stomach (lower third) is wholly smooth muscle in most animals. Dogs and ruminants are exceptions to
this statement. In these animals, the tunica muscularis is entirely skeletal muscle for the entire length of
the esophagus, which facilitates vomiting.
2. Stomach, human, fundic region, H&E
The stomach is a muscular bag whose principal function in most groups is acidification and
maceration of the food to the liquid state, and temporary storage until it is passed to the intestines.
Extending from the esophagus to the duodenum; it is divisible into the cardiac, fundus, body, and
pyloric regions. Its epithelium is specialized for secretion and is of the simple columnar type. The
gastric mucosa contains gastric pits (foveolae); these are surface invaginations that also serve as the
ducts of the underlying intrinsic gastric glands. Three basic cell types contribute to the secretion of
gastric juice (mucous-secreting cells, parietal cells, chief cells), and each has a characteristic
appearance under the light and electron microscope. All of these cell types can be seen in the fundus
and body of the stomach.
Identify the mucosa, submucosa, muscularis externa and serosa. In the mucosa, you should
be able to see that the lumen of the stomach is lined with an ordinary looking simple columnar
epithelium. There are no goblet cells in it (in which respect it differs from the intestines). Locate the
following elements of the mucosa: the luminal surface mucous secreting cells, the gastric pits and the
cells lining them.The surface mucous cells of the mucosa are well shown. Parietal cells are particularly
prominent and chief cells and mucous neck cells are present. In this section chief cells and parietal cells
can be distinguished from each other since the chief cells show a cytoplasmic basophilia.
Enteroendocrine cells are also present in the basal part of the glands but can be positively identified
only with the use of appropriate immunochemical markers. Be aware that these cells secrete many
endocrine/paracrine substances.
ATES-CAMINO, Fritzie B. (AY 2011-2012), BSES-CSM, UPMindanao
Zoology 115 Animal Histology Laboratory Exercises 5
If you were somehow able to stand inside the stomach and look at it en face, you'd see deep
depressions in the "floor" representing gastric pits or foveolae, also lined with simple columnar
epithelium. Small openings into the underlying regions of the mucosal tunic are found at the bottom of
these pits. If you took out your Swiss Army Knife and started excavations into the lamina propria and
the regions beneath the pits, you'd find the actual secretory structures, the various types of gastric
mucosal glands. Identify gastric pits and gastric glands. The parts of gastric glands are the isthmus,
neck and base. Note the lamina propria , the loose, cellular areolar connective tissue surrounding the
gastric pits. Identify the muscularis mucosae, which forms a boundary between the mucosa and
submucosa, and the blood vessels in the submucosa.
The muscularis of the stomach is usually described as being three-layered: inner oblique,
middle circular, outer longitudinal.
Identify the outermost layer delimiting the stomach, the serosa.
Question: (a) What is the secretion of each of these cell types: parietal cell, surface mucuos cells, and
chief cells?; (b) Which of these three muscle layers hypertrophies to form the pyloric sphincter?
3. Intestine
The intestines are the parts of the digestive system responsible for the absorption of nutrients
and water. Two anatomic regions exist, the small intestine and the large intestine. Both of these are
further subdivided into anatomically discernible subdivisions. The small intestine has three parts: the
duodenum, the jejunum, and the ileum; the large intestine is subdivided into the colon, cecum, rectum,
and is continuous with the anus, the last portion of the alimentary canal.
a. Small intestines, duodenum, human, H&E
The small intestine is a place in which nutrients are absorbed, and it has a huge surface area to
fulfill this role. Material moving through here is in liquid form. The villi are a means to enhance the
absorptive surface, and the contents can flow around and over them efficiently.
Most of the general structure of the intestine is similar throughout, and the overall description
given here for duodenum is appropriate for the jejunum and the ileum, with some specific regional
variations. These structural variations serve as "landmarks" in the histological identification of different
areas. Overall the small intestines have the normal form expected of tubular organs, including the four
tunics: mucosa, submucosa, muscularis externa, and the serosa. Identify these four layers.
Examine the mucosa, particularly the surface epithelium. The mucosal surface of the duodenum
is thrown up into grossly visible plicae circulares (circular folds) by the elevation of submucosal folds.
The most visible and significant feature of the small intestine is the presence of finger-like outpockets,
or villi in the intestinal mucosa. The villi of the initial part of the duodenum are short, broad and rather
atypical. In the intestinal villi, most of the cells are absorptive cells, and interspersed between these are
the characteristic mucous-secreting goblet cells. Goblet cells of the intestine will stand out when the
slide is scanned under low power. In addition, a striate border can sometimes be seen on the free
surface of the absorptive cells in well-preserved intestinal villi. Identify the three components of the
mucosa: epithelium, lamina propria and muscularis mucosae. The epithelium is simple columnar
with microvilli forming a continuous brush border visible under high magnification as a refractile band
along the apical surface of the cells.
The lamina propria , the delicate CT that fills the cores of the villi and the spaces between the
crypts, is demarcated from the more peripheral layers by the muscularis mucosae, a thin band of
smooth muscle which runs all the way around the mucosal layer and which sends strands up into the
ATES-CAMINO, Fritzie B. (AY 2011-2012), BSES-CSM, UPMindanao
Zoology 115 Animal Histology Laboratory Exercises 6
villi. It's believed these strands cause the villi to contract, expelling the contents of the crypts and the
intervillous spaces. The muscularis mucosae is the outermost and last layer of the tunica mucosa of the
intestine. Identify and also note the presence of diffuse lymphatic tissue in the mucosa (GALT). (In the
ileum there are accumulations of lymph nodules called Peyer's patches). Locate also the intestinal
glands called crypts of Lieberkühn. Note that they are confined to the lamina propria.
The duodenum is also characterized by the presence of mucus-secreting duodenal glands (of
Brunner) in its submucosa. The submucusa is visible outside the muscularis mucosae and has the
presence of the submucosal glands or "Brunner's glands" for its "landmark." Only in the esophagus and
in the duodenum are glands found in the submucosa, so the presence of these profiles definitively
identifies this region for the histologist. The submucosal glands make an alkaline material that acts to
neutralize the acidic chyme entering the duodenum through the pylorus. If this were not done the
epithelium would soon be eroded by the chyme and an ulceration would result. Present also in the
submucosa are localized collections of neuron cell bodies, elements of the submucosal plexus
discovered by Georg Meissner (1829-1905), a German histologist.
The two layers of the muscularis externa are present and outside these is the adventitia and
serosa. Between the two layers of the muscularis externa, identify elements of the myenteric plexus,
whose function is to coordinate their peristaltic contraction.
b. Large intestines, H&E
The large intestine has subdivisions, as the small intestine does; but distinguishing them in
histological specimens is difficult, since they pretty much look alike and special landmarks are absent.
For the record, the three sections of the large intestine are the cecum, colon, and rectum. The cecum is
a diverticulum located between the ileum and the colon proper, and has openings into both.
Since the function of the large intestine is to desiccate and compact and lubricate the fecal
bolus, villi are absent; there are only crypts. The layers present are similar to those of the small
intestine. However, the number of goblet cells is greatly increased compared to the small intestine. The
muscularis externa is scantier, and there may well be some small lymphatic nodules present.
The mucosa is simple columnar epithelium characterized by deep, straight crypts (unbranched,
tubular intestinal glands) in which are found large numbers of goblet cells. Since most nutrients have
already been extracted, surface area enhancement isn't as important as it is in the small intestine, but
when you're moving large amounts of relatively dry material,what you need is lubrication, and a good
deal of it. Note that the surface epithelium is continuous with the straight, unbranched, tubular
intestinal glands. There are NO villi.Do not mistake intestinal glands for villi. The crypts are much
more open to the lumen than those of the small intestine, which is to be expected. The crypts of the
large intestine are filled with vast numbers of goblet cells that secrete slimy mucus to lubricate the
poop facilitating its ejection. The lamina propria underlying the lumen fills the spaces between the
crypts There is only little lamina propria squeezed between the glands. The muscularis mucosae again
forms two layers.
Considerable amounts of fat may be found in the submucosa. Lymphoid nodules are also
present in the submucosa.
The appearance of the muscularis externa is different from that of the small intestine. The
inner circular layer of muscle forms the usual sheath around the large intestine, but the outer
longitudinal muscle layer forms three flattened strands, the taenia coli. Only a thin layer of
longitudinal muscle surrounds the inner circular muscle layer between the taenia coli .
The adventitia forms small pouches (appendices epiploicae) filled with fatty tissue along the
ATES-CAMINO, Fritzie B. (AY 2011-2012), BSES-CSM, UPMindanao
Zoology 115 Animal Histology Laboratory Exercises 7
large intestine.
c. Ano-rectal junction, Human, H&E
The rectum is the last part of the colon, and it is distinguished by the presence of an enormously
enlarged muscularis externa, forming the anal sphincter. The rectum is histologically similar to the
colon, and there is an abrupt transition between the rectal simple columnar epithelium and the
stratified squamous, (usually keratinized as the lining of the anus makes a transition to the general
integument) epithelium of the anal canal. The anal epithelium may appear stratified cuboidal at the
junction with the rectum, but it assumes a typical stratified squamous appearance more distally. The
intestinal glands end abruptly at the recto-anal junction. The inner circular layer of the muscularis
externa is thickened considerably to form the internal anal sphincter. The submucosa of the anal
canal is characterized by an extensive plexus of hemorrhoidal vessels. The abnormal dilation and
varicosity of these vessels causes an inward bulging of the mucous membrane and a partial occlusion of
the anal canal, resulting in internal hemorrhoids.
d. Appendix, human, H&E
This is a small blind-ending diverticulum from the cecum. Identify the layers and features
typical of the large bowel. However, note that the appendix does not have taeniae coli. The most
important features of the appendix is the thickening of its wall, which is mainly due to large
accumulations of lymphoid tissue in the lamina propria and submucosa. Dense aggregations of
lymphoid tissue, nodular and non-nodular, are characteristic of the appendix. This lymphoid tissue is
present beneath the epithelium around almost the entire circumference of the appendix and does (try to
identify the muscularis mucosae) extend into the submucosa. The heaviest infiltrations extend from the
lamina propria into the submucosa. There is often fatty tissue in the submucosa. The muscularis
externa is thinner than in the remainder of the large intestine and, the outer, longitudinal smooth
muscle layer of the muscularis externa does NOT aggregate into taenia coli. Note the even thickness of
the muscularis externa and the smooth outline of the lumen of the appendix.
The Accessory Glands
1. The Pancreas, Human, H&E
Look at the slide at low magnification and note the subdivision of the pancreas into numerous
lobes and lobules. Identify the connective tissue between the lobes and lobules and try to find
interlobar or interlobular excretory ducts. Their outline is often irregular and their lumen is lined by
a tall columnar epithelium. If you find a large duct you may see a number of smaller ducts streaming
towards the larger duct and, occasionally, connecting with it.
Now have a closer look at the secretory tissue within the lobules. At low magnification most of
the tissue appears to be composed of small reddish packages, the secretory acini. Intercalated ducts are
difficult to find and so are the initial segments of the (non-secretory) intralobular ducts (cuboidal
epithelium). You may try to find them and include them in your drawing, but don't get upset if you or
the demonstrators have difficulties locating them.
Islands of Langerhans, usually containing several hundred endocrine cells, are scattered
throughout the exocrine tissue of the pancreas. The vascularization, composed of many fenestrated
capillaries, is more extensive than that of the exocrine tissue. If you scan over the secretory tissue at
low or medium magnification, you may be able to identify areas of tissue with a slightly different hue
ATES-CAMINO, Fritzie B. (AY 2011-2012), BSES-CSM, UPMindanao
Zoology 115 Animal Histology Laboratory Exercises 8
and texture. These areas are likely to represent the islands of Langerhans.
2. Liver, Human, H&E
The liver is surrounded by a well defined but thin capsule of connective tissue. The connective
tissue extends into the liver parenchyma and divides it into the basic structural units of the liver, the
"classical" liver lobules. A central vein can be seen in the center of many lobules. The portal vein,
hepatic artery and bile duct enter the liver through the porta hepatis. These three vessels travel together
through the liver parenchyma. These groups of three tubes - a branch of the portal vein, a branch of the
hepatic artery and a branch of the bile duct - are called portal triads. Situated in the interlobular
connective tissue are portal triads where branches of the portal vein, hepatic artery, and bile duct
and often a lymphatic vessel can be found. Portal triads are a key feature of the organization of the
liver.
Scan over the tissue at low magnification and identify lobules. It is difficult, if not impossible,
to clearly identify liver lobules in the H&E stained section. The best indication of a liver lobule are the
large central veins and the strands/sheets of hepatocytes, which seem to radiate out from the central
veins. Note that they appear cuboidal in section (actually most are 14-sided cells) and are arranged in
plates that are one cell thick usually separated by blood sinusoids. Many cells are binucleate and some
have an unusually large nucleus. The hepatic sinusoids usually contain some blood cells (unless the
liver was fixed by perfusion). Change to a higher magnification in the region of a central vein and try to
identify the epithelial cells forming the walls of the liver sinusoids. The sinusoids are lined by highly
fenestrated endothelial cells and phagocytic Kupffer cells (“fixed macrophages”), but these are not
easily discerned in this preparation. Refer to your textbooks for the EM structural details of hepatocytes
and sinusoids.
3. Gall bladder, Human, H&E
Have a look at the slide at low magnification. Note the irregular outlines of the epithelium, the
relatively dense irregular connective tissue beneath it, and the irregular appearance of the muscular
layer of the gall bladder. Now take a close look at the epithelium. Observe that the mucosa consists of
a simple columnar epithelium and a lamina propria. There is no muscularis mucosa nor submucosa.
Note that the muscularis is in irregular bundles and does not show the inner circular and outer
longitudinal arrangement found in the gut. External to the muscularis is some moderately dense
connective tissue. Using higher power, return to the mucosa. Note that it is thrown up into folds. The
columnar epithelial cells are quite tall. The function of the epithelium is to transport water out of the
lumen thereby concentrating bile. This, coupled with local inflammation, can contribute to stone
formation. A section of gallbladder should not be confused with sections taken from elsewhere in the
gastrointestinal tract: the gallbladder has NO villi, NO crypts, NO muscularis mucosa and NO goblet
cells in its epithelium.
ATES-CAMINO, Fritzie B. (AY 2011-2012), BSES-CSM, UPMindanao
You might also like
- A Guide for the Dissection of the Dogfish (Squalus Acanthias)From EverandA Guide for the Dissection of the Dogfish (Squalus Acanthias)No ratings yet
- Digestive System I The Oral CavityDocument9 pagesDigestive System I The Oral CavitySUTHANNo ratings yet
- Vet Histology Lecture Notes on Digestive System IDocument62 pagesVet Histology Lecture Notes on Digestive System IDEV3LLS100% (3)
- The Digestive System: Anatomy and Histology of the Tongue and EsophagusDocument42 pagesThe Digestive System: Anatomy and Histology of the Tongue and EsophaguslaithjnbNo ratings yet
- Digestive System GuideDocument26 pagesDigestive System GuideKent Solis VicenteNo ratings yet
- Digestive System Part 1Document10 pagesDigestive System Part 1bazingaNo ratings yet
- @ Histol DigestiveDocument65 pages@ Histol DigestiveAyele AsefaNo ratings yet
- Human Anatomy The Gastrointestinal TractDocument53 pagesHuman Anatomy The Gastrointestinal TractGadzikaNo ratings yet
- Midterm Examination-BiochemDocument10 pagesMidterm Examination-BiochemRhizel Marie Cauilan FariñasNo ratings yet
- Digestive - Histoworld ReferenceDocument12 pagesDigestive - Histoworld ReferenceKarl Torres Uganiza RmtNo ratings yet
- Digestive SystemDocument9 pagesDigestive System79ctq9xpf7No ratings yet
- Digestive System Lecture NotesDocument39 pagesDigestive System Lecture NotesIvan FernandezNo ratings yet
- III. Anatomy and Physiology of the Digestive SystemDocument18 pagesIII. Anatomy and Physiology of the Digestive SystemJoanna_Edna_C__6752No ratings yet
- 06 Digestive SystemDocument101 pages06 Digestive SystemcelynjasminegNo ratings yet
- EntomologyDocument50 pagesEntomologyapi-19960301100% (1)
- Histologi Saluran CernaDocument57 pagesHistologi Saluran CernaAdinda TobingNo ratings yet
- Lecture Notes in Anatomy Histology of The Oral CavityDocument9 pagesLecture Notes in Anatomy Histology of The Oral Cavitykasonde bowaNo ratings yet
- Digestive SystemDocument73 pagesDigestive SystemWakjira GemedaNo ratings yet
- Part Ii Splanchnology Chapter 1 Introduction: Alimentary System Respiratory System Urinary System Genital SystemDocument49 pagesPart Ii Splanchnology Chapter 1 Introduction: Alimentary System Respiratory System Urinary System Genital Systemsomebody_maNo ratings yet
- Anatomy of the tongue and related mouth structuresDocument13 pagesAnatomy of the tongue and related mouth structureslala landNo ratings yet
- Digestion and AbsorptionDocument6 pagesDigestion and AbsorptionMahafuj DudhaknojNo ratings yet
- EssaysDocument176 pagesEssaysppdzssx7ghNo ratings yet
- Gastrointestinal System ExplainedDocument10 pagesGastrointestinal System ExplainedOdi DavidNo ratings yet
- PRACTICA FINAL DE INGLE. DIGESTIVE SYSTEM. AnaDocument18 pagesPRACTICA FINAL DE INGLE. DIGESTIVE SYSTEM. AnaChantal PantaleonNo ratings yet
- Digestive SystemDocument67 pagesDigestive SystemShacquille Suelto Bautista0% (1)
- Lamprey DissectionDocument7 pagesLamprey DissectionAnnas KurniawanNo ratings yet
- Digestive SYSTEMDocument53 pagesDigestive SYSTEMPrincess AnnNo ratings yet
- Gastrointestinal Tract (GIT) - A Continuous Tube That Begins atDocument5 pagesGastrointestinal Tract (GIT) - A Continuous Tube That Begins atBestoon SaifaddinNo ratings yet
- Anatomy and Physiology of the Digestive SystemDocument17 pagesAnatomy and Physiology of the Digestive SystemFahmi IlyasNo ratings yet
- Kelompok 3-SIstem PencernaanDocument103 pagesKelompok 3-SIstem PencernaanNurul Fadhillah IsaNo ratings yet
- Upper GIT System CPPP Lecture 2020-21Document33 pagesUpper GIT System CPPP Lecture 2020-21NoraNo ratings yet
- Alimentary Canal of HumanDocument37 pagesAlimentary Canal of Humanمحمد العراقيNo ratings yet
- Digestive SystemDocument162 pagesDigestive SystemSadhu PriyankaNo ratings yet
- Digestive System Anatomy 1 1Document17 pagesDigestive System Anatomy 1 1jsrz9vmj5jNo ratings yet
- Digestive SystemDocument73 pagesDigestive Systemsnp88No ratings yet
- Digestive System: Food Uptake and UtilizationDocument12 pagesDigestive System: Food Uptake and UtilizationKarthi KarthiNo ratings yet
- 12 B Digestivesystem 1 TextDocument68 pages12 B Digestivesystem 1 TextEINSTEIN2DNo ratings yet
- Phylum CtenophoraDocument23 pagesPhylum CtenophoramsnidanusratNo ratings yet
- Tongue I LastDocument30 pagesTongue I LastEmuyeNo ratings yet
- Histology of GitDocument31 pagesHistology of GitLucky LuckyNo ratings yet
- BiologyDocument13 pagesBiologyMITHUN CHATTERJEENo ratings yet
- Module 3 PDFDocument6 pagesModule 3 PDFLittle Miss CeeNo ratings yet
- Aurelia MaqniDocument6 pagesAurelia MaqniEhm MelsNo ratings yet
- Upper Git FinalDocument11 pagesUpper Git Finalgergeskamal020No ratings yet
- Anatomy of the Digestive System and Associated OrgansDocument50 pagesAnatomy of the Digestive System and Associated OrgansEldar Sulejmanovic100% (2)
- Mammalian System-01 (Digestive System)Document35 pagesMammalian System-01 (Digestive System)Saumya99No ratings yet
- Digestive SystemDocument16 pagesDigestive Systemراوند اعبيدNo ratings yet
- Module 5 Anatomy I Splanchnology 1Document17 pagesModule 5 Anatomy I Splanchnology 1neannaNo ratings yet
- Human Digestive System, The System Used in TheDocument10 pagesHuman Digestive System, The System Used in Theعلي رسن رداد حمد ANo ratings yet
- Digestive and Respiratory Organs DefinitionDocument4 pagesDigestive and Respiratory Organs DefinitionSidne E. AgorNo ratings yet
- Clinical Anatomy, Physiology and Methods of Examination of The Pharynx. Acute and Chronic Tonsillitis and Their Complications. Hypertrophy of The Lymph Tissue of The PharynxDocument55 pagesClinical Anatomy, Physiology and Methods of Examination of The Pharynx. Acute and Chronic Tonsillitis and Their Complications. Hypertrophy of The Lymph Tissue of The PharynxNicolás Barrios MagnaNo ratings yet
- Nematode StructureDocument31 pagesNematode StructureShadab HanafiNo ratings yet
- Filum Platyhelmintes I. DefinitionDocument38 pagesFilum Platyhelmintes I. DefinitionNsc Rhyrin 'syafa' LestariniNo ratings yet
- Detailed Study of FrogDocument20 pagesDetailed Study of FrogM. MuvafficaNo ratings yet
- Human Anatomy Physiology Chapter 12 Sensory Organ NotesDocument9 pagesHuman Anatomy Physiology Chapter 12 Sensory Organ NotesadarshNo ratings yet
- Problem 1Document111 pagesProblem 1Agustina CynthiaNo ratings yet
- TongueDocument162 pagesTongueDevendra ChhonkarNo ratings yet
- Millan, Shaina Marie B. 12-04-2018 BSN-103 Ms. Riza MagsinoDocument3 pagesMillan, Shaina Marie B. 12-04-2018 BSN-103 Ms. Riza MagsinoShaina MillanNo ratings yet
- Human Physiology - Practice Sheet - NSEJS Batch 2024Document12 pagesHuman Physiology - Practice Sheet - NSEJS Batch 2024sciencelover.2027No ratings yet
- Diverticulitis Pathophysiology & EtiologyDocument3 pagesDiverticulitis Pathophysiology & EtiologyDanielle Felize MaramagNo ratings yet
- Constipation AlgorithmDocument1 pageConstipation AlgorithmIYERBKNo ratings yet
- Git GutDocument4 pagesGit GutAngelica Murillo Ang-AngcoNo ratings yet
- Liver, Biliary Tract and Pancreas ProblemsDocument95 pagesLiver, Biliary Tract and Pancreas ProblemsBav VAansoqnuaetzNo ratings yet
- Abdominal Assessment: Jonalyn S. Esco,.Rn.,ManDocument77 pagesAbdominal Assessment: Jonalyn S. Esco,.Rn.,ManClifford Subagan Patil-aoNo ratings yet
- 較常使用之乳酸桿菌屬菌種學名變更對照表Document1 page較常使用之乳酸桿菌屬菌種學名變更對照表YS LNo ratings yet
- CHOLECYSTITISDocument4 pagesCHOLECYSTITISMarcieNo ratings yet
- JaundiceDocument36 pagesJaundiceNasser SalahNo ratings yet
- Colonoscopy BrochureDocument2 pagesColonoscopy BrochureVeronica Wong Huey Shin100% (1)
- Anatomy and Physiology of the PancreasDocument4 pagesAnatomy and Physiology of the PancreasJohn Rey Abad67% (3)
- PASIEN DIGESTIF OHO - 2 Januari 2019 (R1, R2B, R3, R4B)Document2 pagesPASIEN DIGESTIF OHO - 2 Januari 2019 (R1, R2B, R3, R4B)Wahyu Hendra PrabowoNo ratings yet
- Anatomy of PancreasDocument2 pagesAnatomy of PancreasAubrey MacNo ratings yet
- Manfaat Nutrisi Bagi Performa Burung Kicauan: Keywords: Nutrition, Performance, Pet BirdsDocument12 pagesManfaat Nutrisi Bagi Performa Burung Kicauan: Keywords: Nutrition, Performance, Pet BirdsMumutTeaNo ratings yet
- Drug-Induced Acute-onChronic Liver FailureDocument18 pagesDrug-Induced Acute-onChronic Liver FailureVerónica Bello HorizonteNo ratings yet
- AP Bio Digestion System (Kfogler)Document34 pagesAP Bio Digestion System (Kfogler)julie rainesNo ratings yet
- COMPARISON BETWEEN ULTRASONOGRAPHIC AND CLINICAL FINDINGS IN 43 DOGS WITH GB MUCOCELEchoi2013Document6 pagesCOMPARISON BETWEEN ULTRASONOGRAPHIC AND CLINICAL FINDINGS IN 43 DOGS WITH GB MUCOCELEchoi2013Thaís ChouinNo ratings yet
- Pharmacology of The Gastrointestinal Drugs (Ii) Choleretics, Cholagogues and Other Biliary Secretion ModifiersDocument14 pagesPharmacology of The Gastrointestinal Drugs (Ii) Choleretics, Cholagogues and Other Biliary Secretion ModifiersanaNo ratings yet
- Chapter 6 Nutrition in HumansDocument3 pagesChapter 6 Nutrition in Humansno one0% (1)
- Patient Instructions For Colonoscopy and Upper GI EndosDocument4 pagesPatient Instructions For Colonoscopy and Upper GI EndosJm NitrileNo ratings yet
- J. Paulo Sousa e Silva, Ana Cristina Freitas - Probiotic Bacteria - Fundamentals, Therapy, and Technological Aspects-Pan Stanford Publishing (2014)Document310 pagesJ. Paulo Sousa e Silva, Ana Cristina Freitas - Probiotic Bacteria - Fundamentals, Therapy, and Technological Aspects-Pan Stanford Publishing (2014)Jorge AlbertoNo ratings yet
- Gastrointestinal Physiology MOSBYDocument309 pagesGastrointestinal Physiology MOSBYUlquiorra SchifferNo ratings yet
- Dis LiverDocument40 pagesDis LiverPrem MorhanNo ratings yet
- 1) GerdDocument28 pages1) GerdmohamadamirulariffinNo ratings yet
- Virtual Colonoscopy (VC, Also Called CT ColonographyDocument4 pagesVirtual Colonoscopy (VC, Also Called CT ColonographyAbhay KumarNo ratings yet
- Gall Bladder Stone RemovalDocument1 pageGall Bladder Stone RemovalLV Lolong ANo ratings yet
- Chronicpankreatitis CopieDocument18 pagesChronicpankreatitis Copieomarelbihi8No ratings yet
- Chapter 5 and 6 Nutrition in Humans (CE - Structured Questions Marking Scheme)Document5 pagesChapter 5 and 6 Nutrition in Humans (CE - Structured Questions Marking Scheme)Emily LiNo ratings yet
- Daftar Pustaka Refarat RadiologiDocument6 pagesDaftar Pustaka Refarat RadiologiOvelin LarasatiNo ratings yet
- DUODENAL PROCEDUREDocument5 pagesDUODENAL PROCEDUREeka nurjanahNo ratings yet