Professional Documents
Culture Documents
Increased Vasopressin
Uploaded by
K K LoachCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Increased Vasopressin
Uploaded by
K K LoachCopyright:
Available Formats
0021-972X/01/$03.00/0 Vol. 86, No.
6
The Journal of Clinical Endocrinology & Metabolism Printed in U.S.A.
Copyright © 2001 by The Endocrine Society
Increased Vasopressin and Adrenocorticotropin
Responses to Stress in the Midluteal Phase of the
Menstrual Cycle
MARGARET ALTEMUS, CATHERINE ROCA, ELISE GALLIVEN,
CATHERINE ROMANOS, AND PATRICIA DEUSTER
Department of Psychiatry, Weill Medical College, Cornell University (M.A., C.R.), New York, New York
10021; Behavioral Endocrinology Branch, National Institute of Mental Health, National Institutes of
Health (C.R.), Bethesda, Maryland 20892; and Department of Military and Emergency Medicine,
Uniformed Services University of the Health Sciences (E.G., P.D.), Bethesda, Maryland 20814
ABSTRACT over 20 min to reach 90% of each subject’s maximal oxygen consump-
Accumulating evidence indicates that gonadal steroids modulate tion during the final 5 min of exercise. Basal plasma lactate, glucose,
functioning of the hypothalamic-pituitary-adrenal (HPA) axis, which ACTH, vasopressin, oxytocin, and cortisol levels were similar in the
has been closely linked to the pathophysiology of anxiety and depres- two cycle phases. However, in response to exercise stress, women in
sion. However, the effect of the natural menstrual cycle on HPA axis the midluteal phase had enhanced ACTH (P ⬍ 0.0001), vasopressin
responsivity to stress has not been clearly described. In nine healthy (P ⬍ 0.01), and glucose (P ⬍ 0.001) secretion. These findings suggest
women, metabolic and hormonal responses to treadmill exercise that relatively low levels of gonadal steroids during the early follicular
stress during the early follicular phase of the menstrual cycle, when phase of the menstrual cycle provide protection from the impact of
gonadal steroid levels are low, were compared with responses in the stress on the HPA axis. (J Clin Endocrinol Metab 86: 2525–2530,
midluteal phase of the cycle, when both progesterone and estrogen 2001)
levels are relatively high. Exercise intensity was gradually increased
C LINICAL OBSERVATIONS suggest that fluctuations in
reproductive hormones influence the course of de-
pression and anxiety disorders, but the biological mecha-
cells during the early follicular phase of the menstrual cycle
relative to the midluteal phase (7). The study described here
was designed to test whether HPA axis responsivity to stress
nisms that may mediate the effects of reproductive hormones is restrained in the early follicular, compared with the mid-
on emotional regulation have not been identified. Accumu- luteal phase of the menstrual cycle. Restrained HPA axis
lating evidence suggests that gonadal steroids modulate reactivity in the early follicular phase would be expected as
functioning of the hypothalamic-pituitary-adrenal (HPA) a consequence of increased glucocorticoid receptor sensitivity.
axis, which has been closely linked to the pathophysiology We chose to deliver exercise as an HPA axis stressor across
of anxiety and depression. On the one hand, HPA axis re- the menstrual cycle because it is a reproducible, quantifiable
sponses to acute stress can reflect the sensitivity of the in- stressor that elicits neuroendocrine and metabolic responses
dividual to a physical or emotional stress. On the other hand, proportional to the intensity and duration of the exercise (8,
glucocorticoids secreted during stress may, in turn, act in the 9). The relative intensity of the exercise can be standardized
central nervous system to regulate mood and other mental across subjects who have different levels of physical condi-
processes (1). Glucocorticoids are also the primary endocrine tioning by setting each subject’s exercise intensity to elicit a
feedback signal for suppression of the HPA axis and nor- specific percentage of that individual’s maximal aerobic ca-
adrenergic responses to stress (2– 4). Alterations in glucocor- pacity (VO2max). Exercise stress stimulates release of cortisol,
ticoid secretion and glucocorticoid receptor sensitivity are ACTH, and vasopressin, which, in turn, promotes mobili-
postulated to play a role in the development of psychiatric zation of the energy stores needed to meet the exercise stress.
disorders (4) and the mechanism of action of antidepressant
medication (5, 6). Subjects and Methods
Our previous clinical studies have shown enhanced sen- Subjects
sitivity of the HPA axis to dexamethasone suppression and Nine healthy women participated in the study after giving written
increases in type II glucocorticoid receptor messenger ribo- informed consent. The protocol had been approved by the intramural
nucleic acid (mRNA) expression in circulating mononuclear institutional review boards of the NIMH and the Uniformed Services
University of the Health Sciences. Subjects were recruited by local ad-
vertisements for paid participation in an exercise study. Subjects were
Received September 12, 2000. Revision received December 14, 2000. 34.2 ⫾ 1.8 (range, 25– 42) yr of age. All subjects were Caucasian, were
Accepted December 23, 2000. in good physical health, had regular menstrual cycles, were nonsmokers,
Address all correspondence and requests for reprints to: Dr. Margaret and were not taking any medications other than vitamins. All subjects
Altemus, Box 244, Weill Medical College, Cornell University, 1300 York completed a medical history and underwent a physical examination and
Avenue, New York, New York 10021. E-mail: maltemus@mail.med. screening laboratory tests, including complete blood count, chemistry
cornell.edu. panel, thyroid function tests, toxicology screen, urinalysis, and preg-
2525
Downloaded from jcem.endojournals.org by on July 26, 2009
2526 ALTEMUS ET AL. JCE & M • 2001
Vol. 86 • No. 6
nancy test. No subject was suffering from anxiety disorders, depression, 3-fold concentration during the extraction procedure. The intraassay
or other mental illnesses, as assessed by a structured diagnostic inter- CVs were less than 10% for vasopressin and oxytocin. The interassay CV
view (10). No subject suffered from premenstrual dysphoric disorder, as for vasopressin was 13%. The detection limit was 0.60 pmol/L for
assessed by clinical interview and 3 months of daily mood ratings vasopressin and 1.0 pmol/L for oxytocin. Oxytocin levels were not
(10, 11). measured in one subject. Basal estradiol and progesterone were mea-
sured by RIA at the NIH Clinical Center Laboratory at the time of
exercise testing. The intraassay CVs were less than 5% for the estradiol
Experimental protocol
and progesterone assays. Detection limits were 37 pmol/L for estradiol
Exercise testing was performed in both the early follicular (3– 6 days and 1.27 nmol/L for progesterone.
after the onset of menses) and midluteal (7–10 days after the LH surge)
phases of the menstrual cycle. Each woman determined the time of her Statistical analyses
LH surge by using a home urine test kit (Clearplan Easy, Unipath Ltd.,
Bedford, UK). Four women performed the follicular phase exercise test Data are presented as the mean ⫾ sem. Two-way repeated measures
first, and five women started with the luteal phase exercise test. Five of ANOVA was used to investigate the effects of exercise and cycle phase
the nine subjects completed exercise testing within one menstrual cycle. on hormonal variables. ACTH data were log transformed before the
The other subjects required up to three cycles to complete testing due ANOVA because the distribution among subjects was not normal. If
to scheduling difficulties and failure to detect an LH surge needed for significant differences were indicated by ANOVA, post-hoc contrasts
scheduling of the luteal test. were used to evaluate differences at each time point. Single time point
Details of the exercise protocol have been reported previously (12). data were compared using two-tailed Student’s t-tests. Relationships
Subjects were instructed not to eat on the morning before the exercise among variables were evaluated using Pearson’s correlation coefficient.
tests and to abstain from caffeine and alcohol consumption and from The area under the curve was used for correlational analyses of multiple
running or other strenuous activity during the 24 h before testing. time point hormonal data and was calculated by the trapezoidal method
VO2max was determined once by a progressive treadmill exercise with subtraction of the baseline. Significance was set at the 0.05 level.
protocol conducted to volitional exhaustion. Oxygen consumption and
carbon dioxide production during the maximal exercise test and the two Results
subsequent follicular and luteal exercise test sessions were measured
with a Metabolic Measurement Cart 2900c (SensorMedics, Inc., Yorba Basal hormone levels
Linda, CA). Electrocardiogram and heart rate were also monitored con- As expected, basal plasma estradiol and progesterone lev-
tinuously during all exercise tests.
For the follicular and luteal exercise test sessions, subjects reported els were lower in the early follicular compared with the
to the laboratory between 0700 – 0800 h. On arrival, all subjects had an midluteal phase of the menstrual cycle [estradiol, 242 ⫾ 48
iv catheter inserted into an antecubital vein and then consumed 5 mL/kg vs. 580 ⫾ 48 pmol/L (P ⬍ 0.001); progesterone, 2.9 ⫾ 1.3 vs.
BW water to ensure uniform hydration. The exercise test began 60 min 47.7 ⫾ 5.1 nmol/L (P ⬍ 0.0001)]. Basal plasma lactate, glu-
after the subject finished drinking. The treadmill exercise test consisted
of 5 min of exercise at 50% of VO2max, 5 min at 70%, a 2-min break for
cose, ACTH, vasopressin, oxytocin, and cortisol levels were
blood drawing, another 5 min at 70%, and 5 min at 90% of VO2max. similar in the early follicular and midluteal phases of the
Exercise intensities of 50%, 70%, and 90% of VO2max were enforced by cycle (Table 1).
adjusting the slope and speed of the treadmill. The exercise was followed
by a cool-down period of 5 min at a minimal workload, then 35 min of
Hormonal responses during exercise
rest in a semirecumbent position. Expired oxygen and carbon dioxide,
electrocardiogram, and heart rate were monitored throughout the ex- Hormonal responses to exercise are shown in Fig. 1. In-
ercise test and for the first 15 min of the recovery period.
duction of anaerobic metabolism during exercise was indi-
Subjects stood for at least 15 min before the first baseline blood sample
was drawn. Samples were collected before exercise (⫺10 and 0 min), cated by marked increases in plasma lactate levels over time
during exercise (⫹10 min), and immediately after exercise (⫹20 min) in [F(6,48) ⫽ 29.3; P ⬍ 0.0001]; values did not differ between
a standing position and subsequently (⫹30, ⫹40, ⫹50, and ⫹60 min) in phases of the menstrual cycle [F(6,48) ⫽ 0.94; P ⫽ 0.47].
a semirecumbent position. Blood was collected into a syringe and dis- As expected, there was a significant increase in ACTH
pensed into chilled tubes containing ethylenediamine tetraacetate for
ACTH, cortisol, vasopressin, oxytocin, estradiol, and progesterone as- during the exercise test [F(7,56) ⫽ 12.2; P ⬍ 0.0001]. In ad-
says and into tubes containing heparin and fluoride for lactate and dition, there was a significant interaction of ACTH response
glucose measurements. Chilled tubes were stored on ice until plasma with cycle phase [F(7,56 ⫽ 13.85; P ⬍ 0.0001], with the ACTH
was separated by centrifugation at 4 C (within 30 min). Plasma for response enhanced in the luteal phase.
ACTH, vasopressin, and cortisol determinations was stored frozen at
A significant increase in vasopressin during the exercise
⫺80 C until assayed, whereas plasma for lactate, glucose, estrogen, and
progesterone determinations was refrigerated and assayed on the day test was also found [F(7,56) ⫽ 5.8; P ⬍ 0.0001] along with a
of the exercise test. significant menstrual cycle phase interaction [F(7,56) ⫽ 3.0;
Biochemical assays
TABLE 1. Basal hormone in the early follicular and midluteal
Plasma lactate and glucose concentrations were determined in du- phases
plicate (analyzer model 27, YSI, Inc., Yellow Springs, OH). The intra- and
interassay coefficients of variation (CVs) for lactate and glucose were less Variable Early follicular Midluteal
than 5%. ACTH, vasopressin, and cortisol were assayed in three batches,
ACTH (pmol/L) 2.78 ⫾ 0.57 2.66 ⫾ 0.96
with follicular and luteal samples from individual subjects run in the
Cortisol (nmol/L) 521 ⫾ 25 552 ⫾ 50
same batch to minimize effects due to interassay variation. All oxytocin
Vasopressin (pmol/L) 0.80 ⫾ 0.13 0.73 ⫾ 0.11
samples were run in one assay. Commercial RIA kits were used to
Oxytocin (pmol/L) 1.66 ⫾ 0.10 1.95 ⫾ 0.45
measure ACTH (immunoradiometric assay, Nichols Institute Diagnos-
Glucose (mmol/L) 5.0 ⫾ 0.3 5.2 ⫾ 0.3
tics, San Juan Capistrano, CA) and cortisol (Coat-a-Count, Diagnostic
Lactate (mmol/L) 1.0 ⫾ 0.1 0.9 ⫾ 0.1
Products, Los Angeles, CA). The limits of detection for these kits in our
Estradiol (pmol/L) 242 ⫾ 48 580 ⫾ 48a
laboratory are 0.55 pmol/L for ACTH and 27 nmd/L for cortisol. The
Progesterone (nmol/L) 2.86 ⫾ 1.27 47.7 ⫾ 5.09a
intraassay CV averaged 5% for cortisol and ACTH, and the interassay
CV was 12% for ACTH and 8% for cortisol. Arginine vasopressin and Values are the means ⫾ SEM.
oxytocin RIAs were performed as previously described (13, 14) with a a
P ⬍ 0.01.
Downloaded from jcem.endojournals.org by on July 26, 2009
ENHANCED MIDLUTEAL ARGININE VASOPRESSIN AND ACTH RELEASE 2527
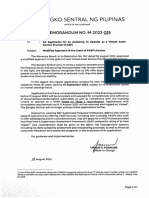
FIG. 1. Hormonal and metabolic re-
sponses to 20 min of graded treadmill
exercise in the early follicular and mid-
luteal phases of the menstrual cycle.
ACTH, vasopressin, and glucose re-
sponses were significantly increased in
the midluteal phase by ANOVA. *, Sig-
nificant differences (P ⬍ 0.05) by post
hoc contrasts at single time points.
P ⬍ 0.01]. As noted for ACTH, the vasopressin response was also was no main effect of cycle phase on cortisol levels
enhanced in the luteal phase. [F(1,8) ⫽ 1.2; P ⫽ 0.29].
As expected, a significant change in plasma glucose oc- In contrast to the other metabolic and hormonal param-
curred during the exercise [F(6,48) ⫽ 6.0; P ⬍ 0.0001]. As eters, there was no effect of exercise on plasma oxytocin
noted for ACTH and vasopressin, there was a significant [F(7,42) ⫽ 0.617; P ⫽ 0.74]. Moreover, oxytocin secretion was
interaction of glucose response to exercise and cycle phase not affected by cycle phase [F(1,6) ⫽ 0.016; P ⫽ 0.90], and
[F(6,48) ⫽ 2.5; P ⬍ 0.04], with exercise-induced glucose levels there was no interaction between the oxytocin response to the
being higher in the luteal phase. exercise test and cycle phase [F(7,42) ⫽ 0.954; P ⫽ 0.48].
There was only a trend toward an effect of exercise on A significant positive correlation was found between basal
plasma cortisol release during the exercise test [F(7,56) ⫽ 2.2; plasma progesterone and the AUC for both ACTH (r ⫽ 0.54)
P ⬍ 0.06], and no interaction between the cortisol response and cortisol (r ⫽ 0.56) in the luteal phase. Basal estradiol
to exercise and cycle phase [F(7,56) ⫽ 1.1; P ⫽ 0.40]. There levels correlated positively with AUC for ACTH (r ⫽ 0.80),
Downloaded from jcem.endojournals.org by on July 26, 2009
2528 ALTEMUS ET AL. JCE & M • 2001
Vol. 86 • No. 6
cortisol (r ⫽ 0.55), and glucose (r ⫽ 0.75) in the follicular However, several other exercise studies found no difference
phase and the AUC for cortisol (r ⫽ 0.50) and glucose (r ⫽ in glucose levels across the menstrual cycle (19, 26). Impair-
0.82) in the luteal phase. ment of glucose uptake and increases in fasting glucose in the
luteal phase have been described in two studies that more
directly focused on glucose regulation across the menstrual
Discussion
cycle (27, 28). Increased glucose responsivity noted in the
We found increased ACTH, vasopressin, and glucose re- luteal phase in our current study may be a consequence of
sponses to treadmill exercise in the midluteal compared with increased vasopressin and cortisol responses in the luteal
the early follicular phase of the menstrual cycle. The results phase, as both of these hormones mobilize glucose. The lack
of this study are compatible with those of a few human of cycle phase differences in glucose response in other studies
studies of HPA axis responsivity across the menstrual cycle, may result from less robust cycle-related differences in hor-
including two studies that found increased cortisol response mones that mobilize glucose.
to psychological stress in the luteal phase (15, 16), another The failure of exercise to stimulate oxytocin release in
study that reported increased cortisol response to prolonged healthy women is consistent with the findings of other ex-
(90-min) submaximal exercise in the luteal phase (17), and a ercise and psychological stress studies (12, 29, 30). On the
fourth study that found a significant rise in cortisol after 30 other hand, massage (31) and breast stimulation in the luteal
min of submaximal exercise stress only the in midluteal phase (32) have been shown to provoke oxytocin release in
phase of the cycle (18). However, many stress studies have women. The lack of oxytocin response to exercise in women
not found menstrual cycle-related differences in HPA axis stands in contrast to the oxytocin release in rats that occurs
responsivity, including studies using intense (19) and mod- in response to a wide variety of physiological stressors (33).
erate physical exercise (20, 21), endotoxin infusion stress (22), This species difference parallels observations that oxytocin
or psychological stressors (23, 24). The lack of a menstrual increases plasma ACTH release in rats (33) and inhibits
cycle effect on ACTH secretion in an earlier exercise stress plasma ACTH release in humans (34, 35).
study from our laboratory (21) and in an exercise study from Menstrual cycle-related changes in several different reg-
another laboratory (20), both using lower intensity exercise, ulatory elements of the HPA axis may contribute to the
suggests that cycle phase differences in ACTH secretion are increased HPA axis responsivity in the luteal phase. Perhaps
evident only during high intensity exercise. Our use of nar-
most important, gonadal steroids appear to regulate glu-
row windows for timing of tests, our choice of testing times
cocorticoid receptor activity in the limbic-hypothalamic-
to maximize differences in gonadal steroid levels, measure-
pituitary-adrenal axis and are likely to thereby modulate
ment of ACTH and vasopressin secretion in addition to cor-
feedback sensitivity of the HPA axis. In a prior study using
tisol secretion, and use of a relatively severe stress stimulus
the same sampling windows across the menstrual cycle, we
may have increased our ability to detect these cycle-related
found decreased lymphocyte glucocorticoid receptor mRNA
differences. Our finding of increased HPA axis responsivity
expression in the midluteal compared with the early follic-
in the luteal phase parallels our previous report of enhanced
ular phase. Reduced glucocorticoid receptor mRNA expres-
HPA axis responses to exercise in nonlactating postpartum
women compared with lactating women who are in a state sion in the luteal phase was accompanied by reduced sen-
of relative gonadal steroid suppression (12). sitivity to dexamethasone suppression of plasma cortisol (7).
The less robust cycle-related difference in cortisol secretion Animal studies are consistent with these observations, show-
in response to the exercise testing is surprising in light of the ing increases in HPA axis feedback sensitivity after ovari-
enhanced ACTH and vasopressin responses in the luteal ectomy (36). Enhanced plasma vasopressin release in the
phase, both of which stimulate cortisol secretion, and in light midluteal phase may also contribute to the enhanced ACTH
of reports that adrenal sensitivity to ACTH is enhanced in the response found in the midluteal phase by stimulating pitu-
luteal phase (16, 25). This discrepancy most likely is due to itary vasopressin receptors (37, 38). In addition, catechol-
the circadian fall in cortisol, which continued through the amine activity is enhanced in the luteal phase (39, 40) and
early morning testing. The circadian fall completely ob- may contribute to enhanced HPA axis responsivity. Central
scured any rise in plasma cortisol in response to the exercise serotonergic activity also may fluctuate across the menstrual
test in half of the subjects. In contrast, cortisol responses were cycle and contribute to changes in HPA axis regulation
larger and more distinct in an exercise study that was per- (41– 43).
formed in postpartum women in our laboratory using the Because of the naturalistic design of this study, it was not
same protocol but at midday, when ambient cortisol levels possible to definitely sort out the differential effects of spe-
are lower (12). cific gonadal steroids on HPA axis responsivity. Both estra-
The physiological mechanism that produces the increase diol and progesterone levels correlated positively with at
in glucose level at baseline and throughout testing during the least some components of HPA axis responsivity. Although
luteal phase is unclear. An earlier study from our laboratory correlations between estradiol and HPA axis responses were
using moderate intensity exercise during the follicular and seen in both the follicular and luteal phases of the cycle,
luteal phases of the cycle also demonstrated higher glucose progesterone levels all were close to the detection limit of the
levels during the luteal phase (21). Another study noted the assay in the follicular phase; this prevented any meaningful
typical drop in glucose in response to submaximal exercise associations with hormonal responses. Further studies using
only in the luteal phase (17); this finding also suggests that specific estrogen and progesterone receptor antagonists or
glucose responses to stress are enhanced in the luteal phase. single hormone replacement strategies in postmenopausal
Downloaded from jcem.endojournals.org by on July 26, 2009
ENHANCED MIDLUTEAL ARGININE VASOPRESSIN AND ACTH RELEASE 2529
women should help to clarify the roles of individual gonadal exercise in lactating women suggest that relatively low levels
steroid hormones in regulation of the HPA axis in humans. of gonadal steroids in premenopausal women may reduce
Numerous studies of ovariectomized rats have found a the effects of stress on the HPA axis.
stimulatory effect of estradiol on HPA axis responsivity (44,
45) and an inhibitory effect of estradiol on HPA axis feedback
sensitivity (44, 46), but effects of progesterone on HPA axis References
regulation are less clear (44, 45, 47– 49). Studies in ovariec- 1. Schulkin J, Gold PW, McEwen BS. 1998 Induction of corticotropin-releasing
hormone gene expression by glucocorticoids: implication for understanding
tomized primates have shown that ACTH and cortisol re- the states of fear and anxiety and allostatic load. Psychoneuroendocrinology.
sponses to interleukin-1 challenge were enhanced during 23:219 –243.
replacement of late follicular compared with early follicular 2. Munck A, Guyre PM, Holbrook NJ. 1984 Physiological functions of glucocor-
ticoids in stress and their relations to pharmacological actions. Endocr Rev.
levels of estradiol (50, 51). The effects of estrogen on HPA axis 5:25– 44.
responsivity in humans have been mixed, with increased 3. Brown M, Fisher L. 1986 Glucocorticoid suppression of the sympathetic ner-
HPA axis responsivity after 1 day of estradiol treatment in vous system and adrenal medulla. Life Sci. 39:1003–1012.
4. Chrousos GP, Gold PW. 1992 The concepts of stress and stress system dis-
men (52), reduced responsivity after 6 – 8 weeks of estrogen orders. Overview of physical and behavioral homeostasis. JAMA.
treatment in postmenopausal women (53, 54), and no effect 267:1244 –1252.
5. Pepin MC, Beaulieu S, Barden N. 1989 Antidepressants regulate glucocorti-
on HPA responses to stress after longer term treatment (55). coid receptor messenger RNA concentrations in primary neuronal cultures.
Also, a recent study in men showed that 24-h administration Mol Brain Res. 6:77– 83.
of exogenous estrogen significantly enhanced HPA axis re- 6. Kitayama I, Janson AM, Cintra A, et al. 1988 Effects of chronic imipramine
treatment on glucocorticoid receptor immunoreactivity in various regions of
sponses to interview stress. These effects of estrogen and the rat brain: evidence for selective increases of glucocorticoid receptor im-
progesterone on HPA axis regulation may be mediated by munoreactivity in the locus coeruleus and in 5-hydroxytryptamine nerve cell
the effects of these gonadal steroids on glucocorticoid re- groups of the rostral ventromedial medulla. J Neural Transm. 73:191–203.
7. Altemus M, Redwine L, Leong YM, et al. 1997 Reduced sensitivity to glu-
ceptor feedback sensitivity. Preclinical data indicate that pro- cocorticoid feedback and reduced glucocorticoid receptor mRNA expression
gesterone serves as an antagonist at glucocorticoid receptors in the luteal phase of the menstrual cycle. Neuropsychopharmacology.
17:100 –109.
(56, 57) and that short-term estrogen treatment in ovariec- 8. Luger A, Deuster P, Kyle SB, et al. 1987 Acute hypothalamic-pituitary-adrenal
tomized rats can down-regulate glucocorticoid receptors in responses to the stress of treadmill exercise. N Engl J Med. 316:1309 –1315.
the hippocampus, hypothalamus, and pituitary (47, 58 – 60). 9. Deuster PA, Chrousos GP, Luger A, et al. 1989 Hormonal and metabolic
responses of untrained, moderately trained, and highly trained men to three
Preclinical data also indicate that estrogen may enhance the exercise intensities. Metabolism. 38:141–148.
magnocellular release of vasopressin. In rats ovariectomy 10. Spitzer RL, Williams JB, Gibbon M, First MB. 1994 Structured clinical in-
prevented the release of vasopressin into the systemic cir- terview for DSM-IV: patient edition. New York: New York State Psychiatric
Institute, Biometrics Research Department.
culation in response to salt loading and also attenuated the 11. Rubinow Dl, Roy-Byrne P, Hoban MC, Gold PW, Post RM. 1984 Prospective
induction of vasopressin mRNA expression in the magno- assessment of menstrually related mood disorders. Am J Psychiatry.
141:684 – 686.
cellular cells of the supraoptic and paraventricular nuclei of 12. Altemus M, Deuster P, Galliven E, Carter S, Gold PW. 1995 Suppression of
the hypothalamus (61). In addition, arginine vasopressin hypothalamic-pituitary adrenal axis responses to stress in lactating women.
mRNA in the magnocellular division of the paraventricular J Clin Endocrinol Metab. 80:2954 –2959.
13. Altemus M, Pigott T, Kalogeras KT, et al. 1992 Abnormalities in the regulation
nucleus was increased in ovariectomized rats in response to of vasopressin and corticotropin releasing factor secretion in obsessive-
estrogen treatment (59). compulsive disorder. Arch Gen Psychiatry. 49:9 –20.
Changes in HPA axis and plasma vasopressin responsivity 14. Demitrack MA, Lesem MD, Listwak SJ, Brandt HA, Jimerson DC, Gold PW.
1990 CSF oxytocin in anorexia nervosa and bulimia nervosa: clinical and
across the menstrual cycle may be linked to fluctuations in pathophysiologic considerations. Am J Psychiatry. 147:882– 886.
mood and somatic symptoms. Multiple studies in nonclinical 15. Marinari KT, Leshner AI, Doyle MP. 1976 Menstrual cycle status and adre-
nocortical reactivity to psychological stress. Psychoneuroendocrinology. 1:213.
populations have documented increases in irritability, anx- 16. Kirschbaum C, Kudielka BM, Gaab J, Schommer NC, Hellhammer DH. 1999
iety, and depression symptoms in the mid- and late luteal Impact of gender, menstrual cycle phase, and oral contraceptives on the ac-
phases of the menstrual cycle (23, 62, 63). In addition, 3– 8% tivity of the hypothalamic-pituitary-adrenal axis. Pscyhosomat Med.
61:154 –162.
of women are particularly sensitive to menstrual cycle hor- 17. Lavoie JM, Dionne N, Helie R, Brisson GR. 1987 Menstrual cycle phase
monal changes and experience severe mood worsening in the dissociation of blood glucose homeostasis during exercise. J Appl Physiol.
luteal phase, with significant impairment of social and oc- 62:1084 –1089.
18. Kanaley JA, Boileau RA, Bahr JM, Misner JE, Nelson RA. 1992 Cortisol levels
cupational functioning (11, 63– 65). Suppression of HPA axis during prolonged exercise: the influence of menstrual phase and menstrual
activation during the follicular phase of the menstrual cycle status. Int J Sports Med. 13:332–336.
19. Bonen A, Haynes FJ, Watson-Wright W, et al. 1983 Effects of menstrual cycle
may be a reflection at least in part of suppression of central on metabolic responses to exercise. J Appl Physiol. 55:1506 –1513.
neuropeptides that drive the axis, particularly CRH and 20. DeSouza MJ, Maguire MS, Maresh CM, Kraemer WJ, Rubin KR, Loucks AB.
vasopressin. These peptides have arousal-producing, anxio- 1991 Adrenal activation and prolactin response to exercise in eumenorrheic
and amenorrheic runners. J Appl Physiol. 70:2378 –2387.
genic effects and have been argued to play an important role 21. Galliven EA, Singh A, Michelson D, Bina S, Gold PW, Deuster PA. 1997
in the generation of depression and anxiety disorder symp- Hormonal and metabolic responses to exercise across time of day and men-
toms (66). In addition, increased vasopressin responsivity in strual cycle phase. J Appl Physiol. 83:1822–1831.
22. Xiao E, Xia-Zhang L, Ferin M. 1999 Stress and the menstrual cycle: short- and
the midluteal phase of the menstrual cycle may contribute to long-term response to a five-day endotoxin challenge during the luteal phase
subjective sensations of fluid retention premenstrually. in the rhesus monkey. J Clin Endocrinol Metab. 84:623– 626.
23. Collins A, Eneroth P, Landgren B. 1985 Psychoneuroendocrine stress re-
In summary, this study demonstrates suppression of HPA sponses and mood as related to the menstrual cycle. Psychosom Med.
axis and plasma vasopressin reactivity to exercise stress in 47:512–527.
the early follicular compared with the midluteal phase of the 24. Ablanalp JM, Livingston L, Rose RM, Sandwich D. 1977 Cortisol and growth
hormone responses to psychological stress during the menstrual cycle. Psy-
menstrual cycle. These findings in combination with prior chosom Med. 39:158 –177.
findings of reduced HPA axis and vasopressin responses to 25. Kruyt N, Rolland R. 1982 Cortisol, 17␣-OH-progesterone, and androgen re-
Downloaded from jcem.endojournals.org by on July 26, 2009
2530 ALTEMUS ET AL. JCE & M • 2001
Vol. 86 • No. 6
sponse to a standardized ACTH-stimulation in different stages of the normal cocorticoid receptor messenger ribonucleic acid in rat brain. Endocrinology.
menstrual cycle. Acta Endocrinol (Copenh). 100:427– 433. 129:2166 –2174.
26. Nicklas BJ, Hackney AC, Sharp RL. 1989 The menstrual cycle and exercise 48. Burgess LH, Handa RJ. 1993 Estrogen-induced alterations in the regulation of
performance, muscle glycogen, and substrate responses. Int J Sports Med. mineralocorticoid and glucocorticoid receptor messenger RNA expression in
10:264 –269. the female rat anterior pituitary gland and brain. Mol Cell Neurosci. 4:191–198.
27. Diamond MP, Simonson DC, DeFronzo RA. 1989 Menstrual cyclicity has a 49. Handa RJ, Nunley KM, Lorens SA, Louie JP, McGivern RF, Bollnow MR.
profound effect on glucose homeostasis. Fertil Steril. 52:204 –208. 1994 Androgen regulation of adrenocorticotropin and corticosterone secretion
28. Jarrett RJ, Graver HJ. 1968 Changes in oral glucose tolerance during the in the male rat following novelty and foot shock stressors. Physiol Behav.
menstruation cycle. Br Med J. 2:528. 55:117–124.
29. Altemus M, Redwine LS, Leong YM, Porges SW, Carter CS. Responses to 50. Xia-Zhang L, Xiao E, Ferin M. 1995 A 5-day estradiol therapy, in amounts
laboratory psychosocial stress in postpartum women. Psychosom Med. In reproducing concentrations of the early-mid follicular phase, prevents the
press. activation of the hypothalamo-pituitary-adrenal axis by interleukin-1␣ in the
30. Sanders G, Freilicher J, Lightman SL. 1990 Psychological stress of exposure ovariectomized rhesus monkey. J Neuroendocrinology. 7:387–392.
to uncontrollable noise increases plasma oxytocin in high emotionality women. 51. Xiao E, Xia L, Shanen D, Khabele D, Ferin M. 1994 Stimulatory effects of
Psychoneuroendocrinology. 15:47–58. interleukin-induced activation of the hypothalamo-pituitary-adrenal axis on
31. Turner RA, Altemus M, Enos T, Cooper B, McGuinness T. 1999 Exploring the gonadotropin secretion in ovariectomized monkeys replaced with estradiol.
biological basis of attachment:Relationships among oxytocin, prolactin and Endocrinology. 135:2093–2098.
interpersonal traits in healthy women. Psychiatry. 62:97–113. 52. Kirschbaum C, Schommer N, Federenco I, et al. 1996 Short-term estradiol
32. Amico J, Finely BE. 1986 Breast stimulation in cycling women, pregnant treatment enhances pituitary-adrenal axis and sympathetic responses to psy-
women and a woman with induced lactation: pattern of release of oxytocin, chosocial stress in healthy young men. J Clin Endocrinol Metab. 81:3639 –3643.
prolactin and luteinizing hormone. Clin Endrocrinol (Oxf). 25:97–106. 53. Lindheim SR, Legro RS, Bernstein L, et al. 1992 Behavioral stress responses
33. Samson WK, Mogg RJ. 1990 Oxytocin as part of stress responses. Curr Top in premenopausal and postmenopausal women and the effects of estrogen.
Neuroendocrinol. 10:33– 60. Am J Obstet Gynecol. 167:1831–1836.
34. Izzo A, Rotondi M, Perone C, et al. 1999 Inhibitory effect of exogenous 54. Komesaroff PA, Esler MD, Sudhir K. 1999 Estrogen supplementation atten-
oxytocin on ACTH and cortisol secretion during labour. Clin Exp Obstet uates glucocorticoid and catecholamine responses to mental stress in peri-
Gynecol. 26:221–224. menopausal women. J Clin Endocrinol Metab. 84:606 – 610.
35. Chiodera P, Coiro V. 1987 Oxytocin reduces metyrapone-induced ACTH 55. Burleson MH, Malarkey WB, Cacioppo JT, et al. 1998 Postmenopausal hor-
mone replacement: effects on autonomic, neuroendocrine, and immune reac-
secretion in human subjects. Brain Res. 420:178 – 81.
tivity to brief psychological stressors. Psychosomat Med. 60:17–25.
36. Young EA. 1996 Sex differences in response to exogenous corticosterone. Mol
56. Svec F, Yeakley J, Harrison RW. 1980 Progesterone enhances glucocorticoid
Psychiatry. 1:313–319.
dissociation from the AT-20 cell glucocorticoid receptor. Endocrinology.
37. Antoni FA. 1993 Vasopressinergic control of pituitary adrenocorticotropin
107:566 –572.
secretion comes of age. Front Neuroendocrinol. 14:76 –122.
57. AbouSamra AB, Loras B, Pugeat M, Tourniare J, Bertrand J. 1984 Demon-
38. Perraudin V, Delarue C, Lefebvre H, Contesse V, Kuhn JM, Vaudry H. 1993
stration of an antiglucocorticoid action of progesterone on the corticosterone
Vasopressin stimulates cortisol secretion from human adrenocortical tissue
inhibition of -endorphin release by rat anterior pituitary in primary culture.
through activation of V1 receptors. J Clin Endocrinol Metab. 76:1522–1528. Endocrinology. 115:1471–1476.
39. Goldstein DS, Levinson P, Keiser HR. 1983 Plasma and urinary cat- 58. Peiffer A, Barden N. 1987 Estrogen-induced decrease of glucocorticoid re-
echolamines during the human ovulatory cycle. Am J Obstet Gynecol. ceptor messenger ribonucleic acid concentration in rat anterior pituitary gland.
146:824 – 829. Mol Endocrinol. 1:435– 440.
40. Girdler SS, Straneva CAPPA, Leserman J, Stanwyck CL, Benjamin S, Light 59. Patchev V, Hayashi S, Orikasa C, Almeida O. 1995 Implications of estrogen-
KC. 1998 Dysregulation of cardiovascular and neuroendocrine responses to dependent brain organization for gender difference in hypothalamic-pituitary-
stress in premenstrual dysphoric disorder. Psychiatry Res. 81:163–178. adrenal regulation. FASEB J. 9:419 – 423.
41. Bancroft J, Cook A, Davidson D, Bennie J, Goodwin G. 1991 Blunting of 60. Carey MP, Deterd CH, Koning Jd, Helmerhorst F, Kloet ERd. 1995 The
neuroendocrine responses to infusion of l-tryptophan in women with peri- influence of ovarian steroids on hypothalamic-pituitary-adrenal regulation in
menstrual mood change. Psychol Med. 21:305–312. the female rat. J Endocrinol. 144:311–321.
42. Su TP, Schmidt PJ, Danaceau M, Murphy DL, Rubinow DR. 1997 Effect of 61. Crowley RS, Amico JA. 1993 Gonadal steroid modulation of oxytocin and
menstrual cycle phase on neuroendocrine and behavioral responses to the vasopressin gene expression in the hypothalamus of the osmotically stimu-
serotonin agonist m-chlorophenylpeperazine in women with premenstrual lated rat. Endocrinology. 133:2711–2718.
syndrome and controls. J Clin Endocrinol Metab. 82:1220 –1228. 62. Johnson SR. 1987 The epidemiology and social impact of premenstrual symp-
43. O’Keane V, O’Hanlon M, Webb M, Dinan T. 1991 d-Fenfluramine/prolactin toms. J Clin Obstet Gynecol. 30:367–376.
response throughout the menstrual cycle: evidence for an oestrogen-induced 63. Andersch B, Wendestam C, Ohman LHR. 1986 Premenstrual complaints. I.
alteration. Clin Endocrinol (Oxf). 34:289 –292. Prevalence of premenstrual symptoms in a Swedish urban population. J Psy-
44. Burgess LH, Handa RJ. 1992 Chronic estrogen-induced alterations in adre- chosomat Obstet Gynaecol. 5:39 – 49.
nocorticotropin and corticosterone secretion, and glucocorticoid receptor- 64. Rivera-Tovar AD, Frank E. 1990 Late luteal phase dysphoric disorder in young
mediated functions in female rats. Endocrinology. 131:1261–1269. women. Am J Psychiatry. 147:1634 –1636.
45. Viau V, Meaney MJ. 1991 Variations in the hypothalamic-pituitary-adrenal 65. Ramcharan S, Love EJ, Fick GH, Goldfien A. 1992 The epidemiology of
response to stress during the estrous cycle in the rat. Endocrinology. premenstrual symtoms in a population based sample of 2650 urban women:
129:2503–2511. attributable risk and risk factors. J Clin Epidemiol. 45:377–392.
46. Ferrini M, Lima A, DeNicola AF. 1995 Estradiol abolishes autologous down 66. Gold PW, Goodwin FK, Chrousos GP. 1988 Clinical and biochemical man-
regulation of glucocorticoid receptors in brain. Life Sci. 57:2403–2412. ifestations of depression. Relation to the neurobiology of stress. N Engl J Med.
47. Peiffer A, Lapointe B, Barden N. 1991 Hormonal regulation of type II glu- 319:413– 420.
Downloaded from jcem.endojournals.org by on July 26, 2009
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- A High-Bias, Low-Variance Introduction To Machine Learning For Physicists PDFDocument117 pagesA High-Bias, Low-Variance Introduction To Machine Learning For Physicists PDFVaughan PngNo ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Blackkkklansman 2018 PDFDocument125 pagesBlackkkklansman 2018 PDFCamu TalmonNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Sex Determination and Gonadal Development in MammalsDocument29 pagesSex Determination and Gonadal Development in MammalsK K LoachNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- Regulation of Sexual DimorphismDocument34 pagesRegulation of Sexual DimorphismK K LoachNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Get Out 2017Document100 pagesGet Out 2017ZarathurstraNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Biosinteza Polnih HormonaDocument7 pagesBiosinteza Polnih HormonaK K LoachNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Modulation of AldDocument11 pagesModulation of AldK K LoachNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Patchev, Implications of Estrogen-Djıpendent Brain OrganizationDocument5 pagesPatchev, Implications of Estrogen-Djıpendent Brain OrganizationK K LoachNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Review Estradiol and The Developing BrainDocument35 pagesReview Estradiol and The Developing BrainK K LoachNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- Links - Sistemska Hemija I PolimeriDocument1 pageLinks - Sistemska Hemija I PolimeriK K LoachNo ratings yet
- A Two Population Model For The Stock Market Problem: Christos H. SkiadasDocument7 pagesA Two Population Model For The Stock Market Problem: Christos H. SkiadasK K LoachNo ratings yet
- Systems Chemistry and PolymersDocument22 pagesSystems Chemistry and PolymersK K LoachNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Liebhafsky1932 PDFDocument15 pagesLiebhafsky1932 PDFK K LoachNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Haight, Jones 1987 Kinetics and Mechanism of The Iodine-Azide ReactionDocument3 pagesHaight, Jones 1987 Kinetics and Mechanism of The Iodine-Azide ReactionK K LoachNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Jodijf Jsgpogjop GSPJG (P/ Fisjgopjpogj. Mpidgpsomg P NFSDF Opsgm (SGM (FSD (GM DGMDocument1 pageJodijf Jsgpogjop GSPJG (P/ Fisjgopjpogj. Mpidgpsomg P NFSDF Opsgm (SGM (FSD (GM DGMK K LoachNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Jodij 2010Document1 pageJodij 2010K K LoachNo ratings yet
- Sezgin and Schwille - 2011 - Fluorescence Techniques To Study Lipid Dynamics NewDocument33 pagesSezgin and Schwille - 2011 - Fluorescence Techniques To Study Lipid Dynamics NewK K LoachNo ratings yet
- Motivate! 2 End-Of-Term Test Standard: Units 1-3Document6 pagesMotivate! 2 End-Of-Term Test Standard: Units 1-3Oum Vibol SatyaNo ratings yet
- Final Exam, Business EnglishDocument5 pagesFinal Exam, Business EnglishsubtleserpentNo ratings yet
- Modern Dental Assisting 11Th Edition Bird Test Bank Full Chapter PDFDocument37 pagesModern Dental Assisting 11Th Edition Bird Test Bank Full Chapter PDFRichardThompsonpcbd100% (9)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- People V Gona Phil 54 Phil 605Document1 pagePeople V Gona Phil 54 Phil 605Carly GraceNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Initial Data Base (Narrative)Document11 pagesInitial Data Base (Narrative)LEBADISOS KATE PRINCESSNo ratings yet
- Day 3Document18 pagesDay 3SamNo ratings yet
- AMA Manual 10th Edition PDFDocument1,014 pagesAMA Manual 10th Edition PDFKannan Fangs S100% (2)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Lecture Notes - Sedimentation TankDocument45 pagesLecture Notes - Sedimentation TankJomer Levi PortuguezNo ratings yet
- A Game of Thrones: George RR MartinDocument6 pagesA Game of Thrones: George RR MartinRavi ShankarNo ratings yet
- Concept of Intestate SuccessionDocument9 pagesConcept of Intestate SuccessionBodhiratan BartheNo ratings yet
- Dy Keng vs. International LaborDocument9 pagesDy Keng vs. International LaborDani McstNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Classical Music Forms ExplainedDocument11 pagesClassical Music Forms Explainedcorinna_harrison100% (1)
- Factors of Cloud ComputingDocument19 pagesFactors of Cloud ComputingAdarsh TiwariNo ratings yet
- Respiration NotesDocument2 pagesRespiration NotesBriana TaylorNo ratings yet
- Service Manual Pioneer CDJ 2000-2 (RRV4163) (2010)Document28 pagesService Manual Pioneer CDJ 2000-2 (RRV4163) (2010)GiancaNo ratings yet
- The Big Banana by Roberto QuesadaDocument257 pagesThe Big Banana by Roberto QuesadaArte Público Press100% (2)
- DDAL05-02 The Black RoadDocument45 pagesDDAL05-02 The Black Roadlpokm100% (1)
- Boeing 7E7 - UV6426-XLS-ENGDocument85 pagesBoeing 7E7 - UV6426-XLS-ENGjk kumarNo ratings yet
- Thompson Industrial Products Inc Is A DiversifiedDocument4 pagesThompson Industrial Products Inc Is A DiversifiedKailash KumarNo ratings yet
- 5.3.2 Generation of Dislocations: Dislocations in The First Place!Document2 pages5.3.2 Generation of Dislocations: Dislocations in The First Place!Shakira ParveenNo ratings yet
- Buckling of Thin Metal Shells 58Document1 pageBuckling of Thin Metal Shells 58pawkomNo ratings yet
- Hempel's Curing Agent 95040 PDFDocument12 pagesHempel's Curing Agent 95040 PDFeternalkhut0% (1)
- Cub Cadet 1650 PDFDocument46 pagesCub Cadet 1650 PDFkbrckac33% (3)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Alvin - Goldman - and - Dennis - Whitcomb (Eds) - Social - Epistemology - Essential - Readings - 2011 PDFDocument368 pagesAlvin - Goldman - and - Dennis - Whitcomb (Eds) - Social - Epistemology - Essential - Readings - 2011 PDFOvejaNegra100% (2)
- Subsurface Sewage DisposalDocument174 pagesSubsurface Sewage DisposalSanthi KrishnaNo ratings yet
- Doña PerfectaDocument317 pagesDoña PerfectadracbullNo ratings yet
- Fish Culture Y4Document136 pagesFish Culture Y4KèlǐsītǎnKǎPáng100% (1)
- BSP Memorandum No. M-2022-035Document1 pageBSP Memorandum No. M-2022-035Gleim Brean EranNo ratings yet
- TIA Portal v11 - HMI ConnectionDocument4 pagesTIA Portal v11 - HMI ConnectionasdasdasdasdasdasdasadaNo ratings yet
- History of Filipino Mural (Filipino Americans: A Glorious History, A Golden Legacy)Document9 pagesHistory of Filipino Mural (Filipino Americans: A Glorious History, A Golden Legacy)Eliseo Art Arambulo SilvaNo ratings yet
- LIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionFrom EverandLIT: Life Ignition Tools: Use Nature's Playbook to Energize Your Brain, Spark Ideas, and Ignite ActionRating: 4 out of 5 stars4/5 (402)
- The Power of Now: A Guide to Spiritual EnlightenmentFrom EverandThe Power of Now: A Guide to Spiritual EnlightenmentRating: 4.5 out of 5 stars4.5/5 (4120)