Professional Documents
Culture Documents
Viral Conditions That Present As Fever Cough Malaise-1
Uploaded by
SyrelleOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Viral Conditions That Present As Fever Cough Malaise-1
Uploaded by
SyrelleCopyright:
Available Formats
VIRAL CONDITIONS THAT PRESENT AS FEVER, COUGH, AND MALAISE
VIRAL Human Respiratory Syncytial
Rhinovirus Infection Coronavirus Infection Parainfluenza Virus Infection Adenovirus Infection Influenza Virus Infection
CONDITIONS Virus (HRSV) Infection
Etiology Rhinovirus Coronavirus Human Respiratory Syncytial Virus Parainfluenza Virus Adenovirus Influenza virus
(HRSV)
Family Picornaviridae Family Coronaviridae Family Paramyxoviridae Family Adenoviridae Family Orthomyxoviridae
Small (15 to 30 nm) 100-160 nm in diameter Family Paramyxoviridae Genera: Genus Mastadenovirus (51 Influenza A, B, C viruses
Nonenveloped, single- Pleomorphic, single-stranded Genus Pneumovirus a. Respirovirus serotypes) constitute 3 separate genera
stranded RNA virus RNA virus ~ 150 to 350 nm b. Rubulavirus
3 genetic species: Crownlike appearance Enveloped, single-stranded RNA 70-80 nm in diameter Designation of influenza viruses
a. HRV-A produced by the club-shaped virus 150-200 nm in diameter is based on the anntigenic
b. HRV-B projections that stud the viral So named due to its replication in Linear double-stranded DNA characteristics of the:
c. HRV-C envelope vitro that leads to the fusion of Enveloped, single-stranded RNA Codes for structural and non- a. Nucleoprotein (NP)
neighboring cells into large virus structural polypeptides b. Matrix (M) protein antigens
Acid-labile; almost completely Three antigenic and genetic multinucleated syncytia Codes 6 structural and several
inactivated at pH ≤ 3 groups accessory proteins Influenza A
Grow preferentially at 33°- a. HCoV-229E (group 1) Codes 11 virus-specific proteins Characteristic morpholology: - Subtyped on the basis of
34°C (temp of human nasal b. HCoV-OC43 (group 2) Viral RNA is contained in a helical Viral RNA is enclosed in a helical a. Icosahedral shell with 20 the surface hemagglutinin
passages) rather than at 37°C c. SARS-CoV (distantly nucleocapsid surrounded by a nucleocapsid equilateral triangular (H) and neuraminidase (N)
(temp of the lower respiratory related member of group lipid envelope bearing 2 faces and 12 vertices antigens
tract) 2) glycoproteins Envelope is studded with 2 - Individual strains are
glycoproteins: b. Protein coat (capsid) designated accdg to the
Of the 102 recognized Human coronaviruses 2 glycoproteins: a. Glycoprotein with both hexon subunits – site of origin, isolate
serotypes of rhinovirus - Difficult to cultivate in vitro a. G protein hemagglutinin and with group-specific number, yr of isolation,
a. 91 use intercellular - Some strains grow only in by which the virus neuraminidase activity and type-specific and subtype
adhesion molecule 1 human tracheal organ attaches to cells b. Glycoprotein with fusion antigenic - Has 16 distinct H subtypes
(ICAM-1) as a cellular cultures rather than in activity determinants and 9 distinct N subtypes
receptor; “major” receptor tissue culture b. F (fusion) protein - H1-3 and N1-2 –
group facilitates entry of the 5 serotypes (1,2, 3, 4A and 4B) penton subunits at associated with epidemics
b. 10 use the LDL receptor; SARS-CoV virus into the cell by - Share certain antigens with each vertex – contain in humans
“minor” receptor group - an exception; ready fusing host and viral other members of group-specific
c. 1 uses decay- growth in African green membranes Paramyxoviridae family, antigens Influenza B and C
accelerating factor monkey kidney (Vero E6) including mumps and - Similarly designated, but H
cells Single antigenic type with 2 Newcastle disease viruses a fiber with a knob at and N do not receive
distinct subgroups (A and B) and the end projects from subtype designations due
multiple subtypes within each each penton – to less intratypic variations
subgroup contains type-specific in their antigens
and some group-
Antigenic diversity is reflected by specific antigens Influenza A and B
differences in the G protein - Major human pathogens
F protein highly conserved Six subgroups (A-F) on the - Morphologically similar
basis of the homology of DNA - Virions irregularly shaped
Both antigenic groups can genomes and other properties spherical particles
circulate simultaneously in - 80-120 nm in diameter
outbreaks; there are typically The replicative cycle of - Lipid envelop with H and N
alternating patterns in which 1 adenovirus may result in: glycoproteins
subgroup predominates over 1- to a. Lytic infection of cells
2-yr periods b. Establishment of a latent - Genomes consists of 8
infection (primarily single-stranded RNA
lymphoid cell segments, which code for
involvement) structural and non-
structural proteins
String`13 – Level III Block I Module 3 Case 6 (Fever, Cough, Malaise) 1 of 8
VIRAL Human Respiratory Syncytial
Rhinovirus Infection Coronavirus Infection Parainfluenza Virus Infection Adenovirus Infection Influenza Virus Infection
CONDITIONS Virus (HRSV) Infection
Epidemiology Prominent cause of common Present throughout the world Major respiratory pathogen of Distributed throughout the world Most frequently affect infants Influenza A
cold young children and children Most extensive and severe
Detected in up to 50% of Serum antibodies are acquired Infection is acquired in early outbreaks of influenza are
common cold-like illnesses by early in life and increase in Foremost cause of lower childhood Occur throughout the year but caused by influenza A viruses
tissue culture and PCR prevalence with advancing age respiratory disease in infants - By age 5, most children have most common from fall to antigenic shifts (major
techniques - >80% of adult populations antibodies to serotypes 1, 2, spring antigenic variation)
have antibodies as Infection seen throughout the 3 antigenic drifts (minor
Rates of infection: measured by ELISA world Nearly 100% of adults have antigenic variation)
- Higher among infants Types 1 and 2 serum antibody to multiple Pandemic and interpandemic
and young children Account for 10-35% of Annual epidemics occur in late - Cause epidemics during the serotypes indicating that
- Decrease with increasing common colds, depending on fall, winter, or spring; last up to 5 fall infection is common in children Influenza B
age the season months - Often occurring in an Causes outbreaks that are less
rarely encountered in the alternate-year pattern Most common isolates from extensive
Occur throughout the year Prevalent in late fall, winter, summer children Associated with less severe
- Seasonal peaks in early and early spring Type 3 - Types 1,2,3,5 disease than those caused by
fall and spring in - times when rhinovirus Rates of illness - Detected during all seasons influenza A virus
temperate climates infections less common - Highest among infants (1-6 of the year Acute respiratory disease in Its hemagglutinin and
months of age); peak 2-3 - Epidemics occurred annually military recruits in winter and neuraminidase undergo less
Most often introduced into SARS months of age in the spring spring frequent and less extensive
families by preschool or - Occurred in 2002-2003 - Types 4, 7 variation
grade-school children <6 yrs - Outbreak apparently In older children and adults, Rank second to HRSV as causes - Types 3, 14, 21 Outbreaks seen most frequently
old began in Southern China reinfection with HRSV is frequent of lower respiratory tract illness in in schools and military camps;
- 90% of cases occurred in but disease is milder than in young children occasionally in institutions for
Worldwide in distribution China and HK infancy the elderly
- Horseshoe bat natural Type 1 Reye’s syndrome – most
By adulthood, nearly all reservoir of SARS-CoV - Most frequent cause of croup serious complication
individuals have neutralizing in children
antibodies to multiple Influenza C
serotypes, although the Type 2 Relatively minor cause of
prevalence of antibody to any - Generally less severe disease in humans
one serotype varies widely disease Associated with common cold-
like symptoms and occasionally
Multiple serotypes circulate Type 3 with LRT illness
simultaneously - Important cause of The widespread prevalence of
no single serotype or group bronchiolitis and pneumonia serum antibody to this virus
of serotypes has been more in infants indicates that asymptomatic
prevalent than the others - Frequently causes illness infection may be common
during the 1st month of life,
when passively acquired Most prominent high risk
maternal antibody is still conditions associated with
present (unlike types 1, 2) influenza
a. Chronic cardiac and
pulmonary diseases
b. Old age
Mode of direct contact with infected both large and small aerosols close contact with contaminated person-to-person contact inhalation of aerosolized virus aerosols (cough and sneezes)
Transmission secretions (respiratory fecal-oral route fingers or fomites large droplets inoculation of virus into hand-to-hand contact
droplets) self-inoculation of the conjunctiva conjunctival sacs fomite transmission
self-inoculation of the or anterior nares fecal-oral route
conjunctival or nasal mucosa coarse aerosols (coughing and
sneezing)
String`13 – Level III Block I Module 3 Case 6 (Fever, Cough, Malaise) 2 of 8
VIRAL Human Respiratory Syncytial
Rhinovirus Infection Coronavirus Infection Parainfluenza Virus Infection Adenovirus Infection Influenza Virus Infection
CONDITIONS Virus (HRSV) Infection
Clinical Incubation period Incubation period Incubation period Incubation period Children Incubation period
Manifestations - 1-2 days - 2-7 days - 4-6 days - 3-6 days (in experimental clinical syndromes: - 18-72 hours; depending on
- (range: 1-14 days) infections) a. acute URTI + prominent the size of the viral
Usually begins with rhinorrhea HRSV infection leads to a wide - May be shorter for naturally rhinitis – most common inoculums
and sneezing + nasal SARS usually begins as a spectrum of respiratory illnesses occurring disease in children
congestion systemic illness marked by: b. LRT disease Illness characterized by:
a. Fever In infants, 25-40% of infections occurs most frequently among (bronchiolitis, pneumonia) a. Abrupt onset of systemic
Sore throat b. Malasise result in lower respiratory tract children, in whom initial infection symptoms
frequent c. Headache (LRT) involvement: with serotype 1, 2, or 3 is Pharyngoconjunctival fever headache (generalized
initial complaint (in some d. Myalgia a. Pneumonia associated with an acute febrile - types 3 and 7 or frontal)
cases) b. Bronchiolitis illness (in 50-80% of cases) - A characteristic acute feverishness (38°-41°C)
Followed in 1-2 days by: c. Tracheobronchitis febrile illness of children chills
Systemic signs and symptoms a. Non-productive cough young children that occurs in outbreaks, myalgia (most common
are mild or absent b. Dyspnea infants children may present with: most often in summer in legs and lumbosacral
a. Malaise Usually begins most frequently a. coryza camps area)
b. Headache Approx. 25% of patients have with: b. sore throat - Lasts for 1-2 weeks malaise
diarrhea a. Rhinorrhea c. hoarseness - Resolves spontaneously
Fever – unusual b. Low grade fever d. cough (may or may not be b. Respiratory tract signs
CXR: variety of infiltrates: c. Mild systemic symptoms + croupy) a. Bilateral conjunctivitis (cough and sore throat)
Generally lasts for 4-9 days a. Patchy areas of cough + wheezing (bulbar and palpebral cough may last for ≥
consolidation – most In severe croup conjunctivae – granular 1wk
Resolves spontaneously, frequently in peripheral Recover gradually over 1-2 wks - Fever persists appearance) + substernal discomfort
without sequelae and lower lung fields - With worsening coryza and b. Low-grade fever
complications related to Severe cases: sore throat (frequently present for the c. Ocular signs and
obstruction of the Eustachian b. Interstitial infiltrates – can a. Tachypnea - Brassy or barking cough may 1st 3-5 days) symptoms
tube or sinus ostia (otitis progress to diffuse b. Dyspnea progress to frank stridor c. Rhinitis pain on motion of the
media or acute sinusitis) can involvement c. Frank hypoxia d. Sore throat eyes
develop d. Cyanosis Most children recover over the e. Cervical adenopathy photophobia
Severe cases: e. Apnea next 1 or 2 days (although burning of the eyes
Immunosuppressed patients - Respiratory function may progressive airway obstruction Febrile pharyngitis with or
(BM transplant recipients) worsen during the 2nd wk f. PE: diffuse wheezing, and hypoxia ensue occasionally) without conjunctivitis d. PE: flushed; skin hot and
severe and fatal pneumonias of illness progress to rhonchi, rales dry; diaphoresis; mottled
frank adult respiratory If bronchiolitis or pneumonia Whooping cough with or extremities
distress syndrome + g. CXR: hyperexpansion, develops, these may occur: without Bordetella pertussis
multiorgan dysfunction peribronchial thickening, and a. Progressive cough + e. Pharynx – unremarkable;
variable infiltrates (diffuse wheezing adults injection of mucous
- Risk factors: interstitial infiltrates b. Tachypnea Acute respiratory disease membranes and postnasal
a. Age >50 yrs old segmental or lobar c. Intercostal retractions - Types 4 and 7 discharge apparent in
b. Co-morbidities consolidation d. Sputum production increases - Most frequently reported some cases
(CVD, diabetes, modestly in military recruits
hepatitis) Risk factors: (illness severe in:) f. Mild cervical LAD
c. Pregnant women a. Children born prematurely e. PE: nasopharyngeal a. Prominent sore throat
b. Those with congenital discharge and oropharyngeal b. Gradual onset of fever
- SARS-CoV infection cardiac disease injection + rhonchi, wheezes, (39°C) on the 2nd or 3rd Indicative of pulmonary
appears to be milder in c. Bronchopulmonary dysplasia or coarse breath sounds day of illness complications
children than in adults d. Nephrotic syndrome f. CXR: air trapping and c. Cough a. Frank dyspnea
e. Immunosuppression occasionally interstitial d. Coryza b. Hyperpnea
infiltrates e. Regional LAD c. Cyanosis
f. PE: pharyngeal edema, d. Diffuse rales
injection, tonsillar e. Signs of consolidation
enlargement with or
without exudate
String`13 – Level III Block I Module 3 Case 6 (Fever, Cough, Malaise) 3 of 8
Clinical features of common adults Older children and adults g. CXR: patchy infiltrates (if Uncomplicated influenza
colds: coronavirus vs. Most common symptoms Parainfluenza infections milder pneumonia has - Resolves over 2-5 days
rhinovirus a. Common cold developed) - Most patients largely
b. Rhinorrhea Present frequently as: recovered in 1wk
mean incubation period of c. Sore throat a. Common cold; or Acute diarrheal illness - Cough may persist 1-2
colds induced by coronavirus d. Cough b. Hoarseness (with or without - Types 40 and 41 wks longer
(3 days) – longer than that of cough)
rhinovirus infection Occasionally associated with Hemorrhagic cystitis COMPLICATIONS:
moderate systemic symptoms: LRT involvement – uncommon - Types 11 and 21 - Occur most frequently in:
Duration of illness (mean, 6- a. Malaise a. Patients >65 yrs old
7 days) – shorter than that of b. Headache Epidemic keratoconjunctivitis b. Those with certain
rhinovirus infection c. Fever Severe, prolonged, and even fatal - Types 8, 19, 37 chronic disorders
parainfluenza infection has been - Associated with c. Pregnancy (2nd or 3rd
amount of nasal discharges HRSV has been reported to cause reported in children and adults contaminated common trimester)
greater in coronavirus LRT disease with fever, including with severe immunosuppression, sources (ophthalmic d. Children < 5 yrs old
severe pneumonia in the elderly including hematopoietic stem cell solutions, roller towels)
Coronavirus other than SARS- (particularly in nursing-home and solid-organ transplant - Include:
CoV recovered occasionally residents, among whom its impact recipients Disseminated disease and a. Primary influenza
from: can rival that of influenza pneumonia in viral pneumonia
a. Infants with pneumonia immunosuppressed patients b. Secondary bacterial
b. Military recruits with LRT HRSV pneumonia (solid-organ or hematopoietic pneumonia
disease - can be a significant cause of stem cell transplants) c. Mixed viral and
morbidity and death among bacterial pneumonia
Have been associated patients undergoing stem cell d. Worsening of chronic
with worsening of chronic and solid organ bronchitis
bronchitis transplantation e. Asthma
- case fatality rate 20-80% f. Croup (in children)
2 novel coronaviruses isolated g. Sinusitis
from patients with acute sinusitis, otitis media, and h. Otitis media
respiratory illness worsening obstructive and i. Reye’s syndrome
a. HCoV-NL63 (group 1) reactive airway disease – j. Myositis,
b. HCoV0HKU1 (group 2) associated with HRSV infection rhabdomyolysis,
myoglobinuria
k. CNS: encephalitis,
transverse myelitis,
Guillain-Barré
syndrome
l. TSS
VIRAL Human Respiratory Syncytial
Rhinovirus Infection Coronavirus Infection Parainfluenza Virus Infection Adenovirus Infection Influenza Virus Infection
CONDITIONS Virus (HRSV) Infection
Diagnosis PCR RT-PCR RT-PCR PCR Rapid viral diagnosis RT-PCR
- More sensitive than - Rapid diagnosis of SARS- - More specific and sensitive - Highly specific and sensitive a. Immunofluorescence/ - Rapid test detecting viral
tissue culture CoV particularly in adults ELISA of nasopharyngeal antigens
- Detects rhinovirus RNA - More sensitive than tissue Tissue culture aspirates, conjunctival or - Most sensitive and specific
culture Tissue culture - Viral growth detected by respiratory secretions, in vitro test
Tissue culture - Respiratory tract and either hemagglutination or urine, stool - Detects pandemic A/H1N1
- Rarely undertaken due to plasma (early in illness) ELISA or immunofluorescence cytopathic effect b. PCR virus (2009-2010)
benign, self-limited - Stool and urine (later) - Rapid viral diagnostic c. Nucleic acid hybridization
nature of illness technique ELISA or immunofluorescence Tissue culture/ chick embryos
Tissue culture - From nasopharyngeal - Rapid viral diagnosis Definitive diagnosis - Isolation of virus within 48-
Serum antibody test - Inoculation into vero E6 washes, aspirates, - ID of parainfluenza antigens a. Detection of virus in tissue 72 hours after inoculation
- Impractical due to many tissue culture cells nasopharyngeal swabs (less in exfoliated cells from culture (cytopathic
String`13 – Level III Block I Module 3 Case 6 (Fever, Cough, Malaise) 4 of 8
serotypes of rhinovirus - Cytopathic effect seen satisfactory) respiratory tract changes) Acute influenza virus detected
within days - Less sensitive than tissue b. Specific ID with in throat swabs,
WBC count and ESR – not Serologic diagnosis may be made culture immunofluorescence or nasopharyngeal swabs/
helpful ELISA or immunofluorescence by: other immunologic washes, sputum
- Nearly all patients - Comparison of acute and Serologic diagnosis of acute and techniques
Specific diagnosis develop detectable convalescent-phase convalescent-phase specimens Diagnosis of acute infection
- Isolation of virus from: antibodies in 28 days specimen (ELISA, can be established by: Epidemiologic setting of: a. Hemagglutinin inhibition
a. Nasal washes after the onset of illness neutralization, complement- a. Hemagglutinin inhibition a. Acute respiratory disease b. Complement fixation
b. Nasal secretions fixation tests) b. Complement fixation in military recruits c. ELISA
- Useful in older children and c. neutralization b. Certain clinical syndromes
adults in which outbreaks of
- Less sensitive in children (<4 Specific diagnosis: characteristic illness
months of age) - Detection of parainfluenza occurs
virus in: (pharyngoconjunctival
Specific diagnosis: a. Respiratory tract fever; epidemic
- Detection of HRSV in: secretions keratoconjunctivitis)
a. respiratory secretions b. Throat swabs
b. Sputum c. Nasopharyngeal Types 40 and 41
c. Throat swab washings - Associated with diarrheal
d. Nasopharyngeal disease in children
washes - Require special tissue
culture cells for isolation
- Detected by direct ELISA
of stool
Serum antibody rise can be
demonstrated by:
a. CF or neutralization test
b. ELISA
c. Radioimmunoassay
d. Hemagglutinin inhibition
test (for adenovirus that
hemagglutinates RBCs)
VIRAL Human Respiratory Syncytial
Rhinovirus Infection Coronavirus Infection Parainfluenza Virus Infection Adenovirus Infection Influenza Virus Infection
CONDITIONS Virus (HRSV) Infection
Treatment First-line antihistamines Supportive care to maintain Upper Respiratory Tract HRSV Mild cases of croup Only symptom-based treatment For influenza A and B
NSAIDs pulmonary and other organ- infection a. Bed rest and supportive therapy (neuraminidase inhibitors)
Oral decongestant system function a. Alleviation of symptoms b. Moist air generated by a. Zanamivir
Reduction of activity - Mainstay of therapy b. Treatment similar to that for vaporizers Clinically useful antiviral b. Oseltamivir
Antibacterial agents – only if other viral infections of the therapy has not been c. Peramivir
bacterial complications (otitis Approach to the treatment of URT Severe cases established
media or sinusitis) develop common colds similar to a. Hospitalization For Influenza A
rhinovirus-induced illnesses Lower Respiratory Tract HRSV b. Close observation for (adamantane agents)
Specific antiviral therapy NOT infection development of respiratory Active in vitro against certain a. Amantadine
available NO specific therapy of a. Hydration distress adenoviruses b. Rimantadine
established efficacy for SARS b. Suctioning of secretions c. Humidified oxygen and a. Ribavirin
c. Administration of humidified intermittent racemic b. Cidofovir Side effects:
oxygen and epinephrine (if acute a. Zanamivir – exacerbate
antibronchospastic agents respiratory distress bronchospasm in
(as needed) develops) asthmatic patients
d. Severe hypoxia intubation d. Aerosolized or systemically
and ventilatory assistance administered GC – beneficial b. Oseltamivir – nausea and
String`13 – Level III Block I Module 3 Case 6 (Fever, Cough, Malaise) 5 of 8
vomiting; neuropsychiatric
Aerosolized Ribavirin No specific antiviral therapy side effects in children
- Nucleoside analogue active
in vitro against HRSV Ribavirin – active against c. Amantadine – mild CNS
- Modest beneficial effect on parainfluenza virus in vitro; side effects primarily
the resolution of LRTI anecdotal reports describe its jitterness, insomnia,
- “may be considered” for clinical use in immunosuppressed difficulty concentrating
infants who are severely ill or patients
who are at high risk for d. Rimantidine – less
complications of HRSV frequent CNS side effects
infection than amantadine
Not beneficial RIBAVIRIN
a. RSVIg – no longer available - Nucleoside analogue with
b. Palivizumab – chimeric activity against influenza A
mouse-human monoclonal and B in vitro
IgG antibody to HRSV - Variably effective against
influenza when
administered as an aerosol
- Ineffective when
administered orally
- Its efficacy as treatment
not established
Symptom-based treatment for
uncomplicated influenza with
low risk for complications
VIRAL Human Respiratory Syncytial
Rhinovirus Infection Coronavirus Infection Parainfluenza Virus Infection Adenovirus Infection Influenza Virus Infection
CONDITIONS Virus (HRSV) Infection
Prevention and Intranasal application of Strict infection-control Approved as prophylaxis for Vaccines under development Live vaccines against types 4 Inactivated (killed) vaccine
Control interferon spray practices children <2yrs old who have and 7 - 50-80% protection
- Effective prophylaxis bronchopulmonary dysplasia or - Use to control illness - LGF and mild systemic
- Assoc. with local irritation No vaccines against known cyanotic heart disease, or who among military recruits symptoms 8-24h after
of the nasal mucosa human coronaviruses were born prematurely - Live, unattenuated virus vaccination
a. RSVIg – no longer administered in enteric- - Mild redness or
Help reduce rates of available coated capsules tenderness at the
transmission b. Palivizumab vaccination site
a. Thorough hand washing - Infection of the GI tract
b. Environmental Other approaches: with types 4 and 7 does Live attenuated vaccine
decontamination a. Immunization with purified F not cause disease but - Generated by
c. Protection against and G surface glycoproteins stimulates local and reassortment between
autoinoculation of HRSV or generation of systemic antibodies that currently circulating strains
stable, live attenuated virus are protective against of influenza A and B virus
vaccines subsequent acute and a cold-adapted,
b. Barrier methods for the respiratory disease due to attenuated master strain
protection of hands and those serotypes - >90% protective in young
conjunctivae children (>6 months)
- Approved for use in
Inactivated whole-virus vaccine – healthy non-pregnant
INEFFECTIVE persons 2-49 yrs of age
Chemoprophylaxis: oseltamivir
or zanamivir (84-89%)
String`13 – Level III Block I Module 3 Case 6 (Fever, Cough, Malaise) 6 of 8
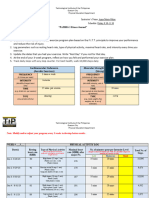
Table 186-1 Illnesses Associated with Respiratory Viruses
Frequency of Respiratory Syndromes
Virus Most Frequent Occasional Infrequent
Rhinoviruses Common cold Exacerbation of chronic bronchitis and Pneumonia in children
asthma
Coronavirusesa Common cold Exacerbation of chronic bronchitis and Pneumonia and bronchiolitis
asthma
Human respiratory Pneumonia and bronchiolitis in young Common cold in adults Pneumonia in elderly and immunosuppressed patients
syncytial virus children
Parainfluenza viruses Croup and lower respiratory tract Pharyngitis and common cold Tracheobronchitis in adults; lower respiratory tract disease in
disease in young children immunosuppressed patients
Adenoviruses Common cold and pharyngitis in Outbreaks of acute respiratory disease in Pneumonia in children; lower respiratory tract and disseminated
children military recruitsb disease in immunosuppressed patients
Influenza A viruses Influenzac Pneumonia and excess mortality in high- Pneumonia in healthy individuals
risk patients
Influenza B viruses Influenzac Rhinitis or pharyngitis alone Pneumonia
d
Enteroviruses Acute undifferentiated febrile illnesses Rhinitis or pharyngitis alone Pneumonia
Herpes simplex viruses Gingivostomatitis in children; Tracheitis and pneumonia in Disseminated infection in immunocompromised patients
pharyngotonsillitis in adults immunocompromised patients
Human Upper and lower respiratory tract Upper respiratory tract illness in adults Pneumonia in elderly and immunosuppressed patients
metapneumoviruses disease in children
a
SARS-associated coronavirus (SARS-CoV) caused epidemics of pneumonia from November 2002 to July 2003 (see text).
b
Serotypes 4 and 7.
c
Fever, cough, myalgia, malaise.
d
May or may not have a respiratory component.
String`13 – Level III Block I Module 3 Case 6 (Fever, Cough, Malaise) 7 of 8
Table 187-3 Antiviral Medications for Treatment and Prophylaxis of Influenza
Age Group (Years)
Antiviral Drug Children (≤12) 13–64 ≥65
Oseltamivir
Treatment, influenza A and B Age 1–12, dose varies by weighta 75 mg PO bid 75 mg PO bid
Prophylaxis, influenza A and B Age 1–12, dose varies by weightb 75 PO qd 75 mg PO qd
Zanamivir
Treatment, influenza A and B Age 7–12, 10 mg bid by inhalation 10 mg bid by inhalation 10 mg bid by inhalation
Prophylaxis, influenza A and B Age 5–12, 10 mg qd by inhalation 10 mg qd by inhalation 10 mg qd by inhalation
Amantadinec
Treatment, influenza A Age 1–9, 5 mg/kg in 2 divided doses, up to 150 mg/d Age ≥10, 100 mg PO bid ≤100 mg/d
Prophylaxis, influenza A Age 1–9, 5 mg/kg in 2 divided doses, up to 150 mg/d Age≥ 10, 100 mg PO bid ≤100 mg/d
Rimantadinec
Treatment, influenza A Not approved 100 mg PO bid 100–200 mg/d
Prophylaxis, influenza A Age 1–9, 5 mg/kg in 2 divided doses, up to 150 mg/d Age ≥10, 100 mg PO bid 100–200 mg/d
a
<15 kg: 30 mg bid; >15–23 kg: 45 mg bid; >23–40 kg: 60 mg bid; >40 kg: 75 mg bid. For children <1 year of age, see www.cdc.gov/h1n1flu/recommendations.htm.
b
<15 kg: 30 mg qd; >15–23 kg: 45 mg qd; >23–40 kg: 60 mg qd; >40 kg: 75 mg qd. For children <1 year of age, see www.cdc.gov/h1n1flu/recommendations.htm.
c
Amantadine and rimantadine are not currently recommended (2009–2010) because of widespread resistance in influenza A viruses. Their use may be reconsidered if viral susceptibility is reestablished.
String`13 – Level III Block I Module 3 Case 6 (Fever, Cough, Malaise) 8 of 8
You might also like
- Cap SnatchingDocument11 pagesCap SnatchingJUAN OSWALDO CONCHA CASAVERDENo ratings yet
- Coronaviruses: Structure and GenomeDocument10 pagesCoronaviruses: Structure and GenomedeviNo ratings yet
- CIA Patho 2Document7 pagesCIA Patho 2Suhas H GNo ratings yet
- Apendice B VirusDocument4 pagesApendice B VirusSaskya GuelfiNo ratings yet
- Virology:: Introduction To Virology, Its' Pathogenesis & EradicationDocument72 pagesVirology:: Introduction To Virology, Its' Pathogenesis & EradicationAndi IrgiNo ratings yet
- The VirusDocument62 pagesThe VirusAhimsa MartawigunaNo ratings yet
- Virology:: Introduction To Virology, Its' Pathogenesis & EradicationDocument73 pagesVirology:: Introduction To Virology, Its' Pathogenesis & EradicationNanda ShafiraNo ratings yet
- Viruses: Key Characteristics!Document7 pagesViruses: Key Characteristics!Melody Jane PardilloNo ratings yet
- Gene of The Month: The 2019-Ncov/Sars - Cov-2 Novel Coronavirus Spike ProteinDocument4 pagesGene of The Month: The 2019-Ncov/Sars - Cov-2 Novel Coronavirus Spike ProteinNandagopal PaneerselvamNo ratings yet
- MLT503 - L2 - General Properties of VirusesDocument51 pagesMLT503 - L2 - General Properties of VirusesMuhammad FirdausNo ratings yet
- Virus FactoriesDocument26 pagesVirus FactoriesGul AfshaNo ratings yet
- Lecture Influenza 03Document10 pagesLecture Influenza 03Muhammad Ikram RabbaniNo ratings yet
- C-Section On Pregnant Women With COVID-19 Final 17 Mei 2020Document61 pagesC-Section On Pregnant Women With COVID-19 Final 17 Mei 2020Anne ChasnyNo ratings yet
- Ann Rev of Virology IPNVDocument30 pagesAnn Rev of Virology IPNVRodolfo VelazcoNo ratings yet
- HIV, Varicella, Polio, and Hepes VirusDocument3 pagesHIV, Varicella, Polio, and Hepes VirusIrfan Adi SaputraNo ratings yet
- RNA Viruses: Segmented Double-Stranded RNA Genome Icosahedral Capsid With No EnvelopeDocument9 pagesRNA Viruses: Segmented Double-Stranded RNA Genome Icosahedral Capsid With No Envelopebaihern24No ratings yet
- Chapter 28: Virology: Poxvirus Herpes Virus Adenovirus Papovavirus Hepatitis BDocument2 pagesChapter 28: Virology: Poxvirus Herpes Virus Adenovirus Papovavirus Hepatitis BAngel FiloteoNo ratings yet
- Recovery of Infectious Bluetongue Virus From RNA: Mark Boyce and Polly RoyDocument8 pagesRecovery of Infectious Bluetongue Virus From RNA: Mark Boyce and Polly Roydrranjanabt100% (2)
- Viruses and Viral InfectionsDocument42 pagesViruses and Viral Infectionsluthfiah adzaniNo ratings yet
- 유전체학Document19 pages유전체학wiwaxia1911No ratings yet
- Quasispecies of SARS-CoV-2 Revealed by Single Nucleotide Polymorphisms (SNPS) AnalysisDocument18 pagesQuasispecies of SARS-CoV-2 Revealed by Single Nucleotide Polymorphisms (SNPS) AnalysisDanilo RosaNo ratings yet
- Microbiology: Coronavirus, Slow Viruses and Prion DiseasesDocument7 pagesMicrobiology: Coronavirus, Slow Viruses and Prion DiseasesJustin TayabanNo ratings yet
- I&V II Virology Lecture 4 of 9Document27 pagesI&V II Virology Lecture 4 of 9Alros ManteltNo ratings yet
- Biology 512 - General Virology: 10:00 - 10:50 Am, MWF 2023 Haworth HallDocument15 pagesBiology 512 - General Virology: 10:00 - 10:50 Am, MWF 2023 Haworth HallChris NguyenNo ratings yet
- THE COVID-19 Pandemic:: A SummaryDocument8 pagesTHE COVID-19 Pandemic:: A SummaryCarl Christian V. DonaireNo ratings yet
- Virology The Study of VirusesDocument45 pagesVirology The Study of Virusesdawoodabdullah56100% (2)
- Viruses and Their Global Impact: IB Plant and Microbial SciencesDocument31 pagesViruses and Their Global Impact: IB Plant and Microbial Sciencesss2945No ratings yet
- Baculovirus: A Viral Bioagent For Biological ControlDocument56 pagesBaculovirus: A Viral Bioagent For Biological ControlA PrashantNo ratings yet
- Nidoviruses - (2. Genomics and Evolution of The Nidovirales) PDFDocument14 pagesNidoviruses - (2. Genomics and Evolution of The Nidovirales) PDFluis echeverryfNo ratings yet
- Retroviruses, HIV/AIDS: March 26 - 27, 2018 SUSOM Dr. Rachel L. RobsonDocument47 pagesRetroviruses, HIV/AIDS: March 26 - 27, 2018 SUSOM Dr. Rachel L. RobsonelitelikeNo ratings yet
- Virology UG Class IV SemesterDocument109 pagesVirology UG Class IV Semestervallabhaneni rajesh100% (1)
- Final Project Bio. MolDocument25 pagesFinal Project Bio. MolJaylenneNo ratings yet
- 7.1 - Medical Virology Part 1Document29 pages7.1 - Medical Virology Part 1Kaela Beatrice Sy LatoNo ratings yet
- Rhabdoviridae - Rabies and Ephemeral FeverDocument14 pagesRhabdoviridae - Rabies and Ephemeral FeverELIJAH EUMIR CUNANANNo ratings yet
- Assignment Quiz Midterm LABESORESDocument2 pagesAssignment Quiz Midterm LABESORESJAN ELMER L. LABESORESNo ratings yet
- General Characteristics of VirusesDocument3 pagesGeneral Characteristics of VirusesLyraski BalawisNo ratings yet
- MycovDocument3 pagesMycovsyareeisyeeNo ratings yet
- Chemical Composition of VirusesDocument24 pagesChemical Composition of VirusesMohammed Yousif mzori100% (1)
- OrthomyxovirusesDocument39 pagesOrthomyxovirusesማላያላም ማላያላምNo ratings yet
- A Thermostable mRNA Vaccine Against COVID-19 Zhang Et - Al. 2020Document30 pagesA Thermostable mRNA Vaccine Against COVID-19 Zhang Et - Al. 2020SY LodhiNo ratings yet
- 5 Basic VirologyDocument71 pages5 Basic VirologyErdemNo ratings yet
- Reverse-Transcribed Sars-Cov-2 Rna Can Integrate Into The Genome of Cultured Human Cells and Can Be Expressed in Patient-Derived TissuesDocument10 pagesReverse-Transcribed Sars-Cov-2 Rna Can Integrate Into The Genome of Cultured Human Cells and Can Be Expressed in Patient-Derived Tissuesdarkangel0282No ratings yet
- Masters and Perlman 2013 in Fields Virology 1Document34 pagesMasters and Perlman 2013 in Fields Virology 1s_navroopNo ratings yet
- Properties: Myxo-TypeDocument4 pagesProperties: Myxo-Typeحسين محمد مطرود كاظمNo ratings yet
- FlaviDocument3 pagesFlaviAyioKunNo ratings yet
- A Bacterial Artificial Chromosome (Bac) - Vectored Noninfectious Replicon of Sars-Cov-2Document25 pagesA Bacterial Artificial Chromosome (Bac) - Vectored Noninfectious Replicon of Sars-Cov-2JuensNo ratings yet
- VirusDocument15 pagesVirusAaron GarciaNo ratings yet
- Virology Course 1Document33 pagesVirology Course 1Uyisabye VénusteNo ratings yet
- The Molecular Biology of Coronaviruses David Cavanaght: MichaelDocument100 pagesThe Molecular Biology of Coronaviruses David Cavanaght: MichaelAchi JackNo ratings yet
- General Characteristics of Viruses and Viral Pathogenesis 1Document37 pagesGeneral Characteristics of Viruses and Viral Pathogenesis 1Gabriella CrooksNo ratings yet
- Retroviruses: HivDocument5 pagesRetroviruses: HivArshu Shaik812No ratings yet
- 01 - General Structure and Classification of Viruses1Document38 pages01 - General Structure and Classification of Viruses1Rahul Kumar100% (1)
- Introduction To VirologyDocument39 pagesIntroduction To VirologybmackarelNo ratings yet
- Bornaviruses: ClassificationDocument7 pagesBornaviruses: ClassificationFrancisco BecerraNo ratings yet
- E 2105968118.fullDocument10 pagesE 2105968118.fullLeblancNo ratings yet
- Taxonomía: ParvoviridaeDocument2 pagesTaxonomía: ParvoviridaeRaquel Elena Martínez LópezNo ratings yet
- COVID 19 Genome Sequencing and DetectionDocument3 pagesCOVID 19 Genome Sequencing and DetectiongygyNo ratings yet
- Finals - VirologyDocument14 pagesFinals - VirologyAngela ReyesNo ratings yet
- ArenavirusDocument29 pagesArenavirusRamirez GiovarNo ratings yet
- Resume Executive Summary ExampleDocument5 pagesResume Executive Summary ExampleSathish GunasekarNo ratings yet
- Healthy Lives, Brighter Futures - The Strategy For Children and Young People's HealthDocument35 pagesHealthy Lives, Brighter Futures - The Strategy For Children and Young People's Healthdhubhat4056No ratings yet
- English: Quarter 2 - Module 1Document12 pagesEnglish: Quarter 2 - Module 1Raquel FranciscoNo ratings yet
- Speech Contest - Stunting in Indonesia2Document2 pagesSpeech Contest - Stunting in Indonesia2Hermawan ChenNo ratings yet
- Lapsus NICUDocument49 pagesLapsus NICUZukmianty SuaibNo ratings yet
- Lectures in PediatricsDocument217 pagesLectures in PediatricsPachiappan NatarajanNo ratings yet
- Nursing Care PlanDocument3 pagesNursing Care Plananon_984362No ratings yet
- Health Insurance UnderwritingDocument59 pagesHealth Insurance UnderwritingDJR DJRNo ratings yet
- Pompy and IPMA V MBT Et Al Second Amended Compalint 6-23Document60 pagesPompy and IPMA V MBT Et Al Second Amended Compalint 6-23Neil AnandNo ratings yet
- Acute StressDocument4 pagesAcute StressRafael MadureiraNo ratings yet
- Dotc Lto Form 21Document13 pagesDotc Lto Form 21CONNIE L. MEDINANo ratings yet
- 10 1016@j Nedt 2020 104440Document13 pages10 1016@j Nedt 2020 104440Florian BodnariuNo ratings yet
- Cognitive-Behavioral Therapy For ADHD in Adolescents Clinical ConsiderationsDocument11 pagesCognitive-Behavioral Therapy For ADHD in Adolescents Clinical Considerationsdmsds100% (1)
- Er - Training/: Urinary IncontinenceDocument3 pagesEr - Training/: Urinary IncontinenceLisnainiMuchlisNo ratings yet
- Thelma ImmunizationDocument51 pagesThelma Immunizationclement johnNo ratings yet
- Goal 1: Eradicate Extreme Poverty and HungerDocument15 pagesGoal 1: Eradicate Extreme Poverty and HungerChege Mbuthia Jr.No ratings yet
- Objectives: Your QuestiensDocument8 pagesObjectives: Your Questiensjoel zapanaNo ratings yet
- Corn PresentationDocument20 pagesCorn PresentationPooja ShrivastavNo ratings yet
- Lesson 3 & 4 - Types of EatingDocument33 pagesLesson 3 & 4 - Types of EatingLawrence L. Clemente100% (1)
- Elderly Skin CareDocument46 pagesElderly Skin CareRobbyNo ratings yet
- POC and Concepts Maps Week 12Document23 pagesPOC and Concepts Maps Week 12Michelle CollinsNo ratings yet
- 3 Nyc PydpDocument13 pages3 Nyc PydpYang RheaNo ratings yet
- Quiz 2Document3 pagesQuiz 2air france bargamentoNo ratings yet
- HSSE Handbook - EngDocument34 pagesHSSE Handbook - EngFabian.DNo ratings yet
- Doroga Bahrm21s1 Pe003 Fitness Journal LogDocument4 pagesDoroga Bahrm21s1 Pe003 Fitness Journal LogJeah Joyce LagrimasNo ratings yet
- Annual Operational Plan 2012 NarrativeDocument11 pagesAnnual Operational Plan 2012 NarrativeArianne A ZamoraNo ratings yet
- Apple Snail Health Problems and SolutionsDocument11 pagesApple Snail Health Problems and SolutionsDonya Quick86% (7)
- Pembukaan Survei Pendampingan Akreditasi Rsu Permata Bunda - GroboganDocument14 pagesPembukaan Survei Pendampingan Akreditasi Rsu Permata Bunda - GroboganAli MuhsonNo ratings yet
- What Are The Parts of A Nursing Diagnosis? Know How To Write An Appropriate Nursing DiagnosisDocument9 pagesWhat Are The Parts of A Nursing Diagnosis? Know How To Write An Appropriate Nursing DiagnosisNoah ClevengerNo ratings yet
- Safety of Patwardhan Technique in Deeply Engaged Head: Reeta Bansiwal, HP Anand, Meera JindalDocument4 pagesSafety of Patwardhan Technique in Deeply Engaged Head: Reeta Bansiwal, HP Anand, Meera JindalToni Marie Q. Mangubat-OpiñaNo ratings yet
- Uncontrolled Spread: Why COVID-19 Crushed Us and How We Can Defeat the Next PandemicFrom EverandUncontrolled Spread: Why COVID-19 Crushed Us and How We Can Defeat the Next PandemicNo ratings yet
- The Wisdom of Plagues: Lessons from 25 Years of Covering PandemicsFrom EverandThe Wisdom of Plagues: Lessons from 25 Years of Covering PandemicsRating: 4.5 out of 5 stars4.5/5 (6)
- Deaths of Despair and the Future of CapitalismFrom EverandDeaths of Despair and the Future of CapitalismRating: 4.5 out of 5 stars4.5/5 (30)
- The Gut-Immune Connection: How Understanding the Connection Between Food and Immunity Can Help Us Regain Our HealthFrom EverandThe Gut-Immune Connection: How Understanding the Connection Between Food and Immunity Can Help Us Regain Our HealthNo ratings yet
- Summary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisFrom EverandSummary: The Myth of Normal: Trauma, Illness, and Healing in a Toxic Culture By Gabor Maté MD & Daniel Maté: Key Takeaways, Summary & AnalysisRating: 4 out of 5 stars4/5 (9)
- Do You Believe in Magic?: The Sense and Nonsense of Alternative MedicineFrom EverandDo You Believe in Magic?: The Sense and Nonsense of Alternative MedicineNo ratings yet
- There Are No Accidents: The Deadly Rise of Injury and Disaster—Who Profits and Who Pays the PriceFrom EverandThere Are No Accidents: The Deadly Rise of Injury and Disaster—Who Profits and Who Pays the PriceRating: 4.5 out of 5 stars4.5/5 (11)
- There Are No Accidents: The Deadly Rise of Injury and Disaster—Who Profits and Who Pays the PriceFrom EverandThere Are No Accidents: The Deadly Rise of Injury and Disaster—Who Profits and Who Pays the PriceRating: 4.5 out of 5 stars4.5/5 (15)
- The Bodies of Others: The New Authoritarians, COVID-19 and The War Against the HumanFrom EverandThe Bodies of Others: The New Authoritarians, COVID-19 and The War Against the HumanRating: 4.5 out of 5 stars4.5/5 (12)
- The Wuhan Cover-Up: And the Terrifying Bioweapons Arms RaceFrom EverandThe Wuhan Cover-Up: And the Terrifying Bioweapons Arms RaceNo ratings yet
- The Price of Health: The Modern Pharmaceutical Industry and the Betrayal of a History of CareFrom EverandThe Price of Health: The Modern Pharmaceutical Industry and the Betrayal of a History of CareRating: 4.5 out of 5 stars4.5/5 (3)
- Epic Measures: One Doctor. Seven Billion Patients.From EverandEpic Measures: One Doctor. Seven Billion Patients.Rating: 4 out of 5 stars4/5 (13)
- Mama Might Be Better Off Dead: The Failure of Health Care in Urban AmericaFrom EverandMama Might Be Better Off Dead: The Failure of Health Care in Urban AmericaNo ratings yet
- Clean: Overcoming Addiction and Ending America’s Greatest TragedyFrom EverandClean: Overcoming Addiction and Ending America’s Greatest TragedyRating: 4 out of 5 stars4/5 (18)
- Summary: The Real Anthony Fauci: Bill Gates, Big Pharma, and the Global War on Democracy and Public Health by Robert F. Kennedy Jr: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Real Anthony Fauci: Bill Gates, Big Pharma, and the Global War on Democracy and Public Health by Robert F. Kennedy Jr: Key Takeaways, Summary & Analysis IncludedNo ratings yet
- COVID-19: The Victims, The Heroes, The Comlicit, and Our New NormalFrom EverandCOVID-19: The Victims, The Heroes, The Comlicit, and Our New NormalNo ratings yet
- Coronary: A True Story of Medicine Gone AwryFrom EverandCoronary: A True Story of Medicine Gone AwryRating: 5 out of 5 stars5/5 (4)
- Fatal Conveniences: The Toxic Products and Harmful Habits That Are Making You Sick—and the Simple Changes That Will Save Your HealthFrom EverandFatal Conveniences: The Toxic Products and Harmful Habits That Are Making You Sick—and the Simple Changes That Will Save Your HealthRating: 4 out of 5 stars4/5 (7)
- Inflamed: Deep Medicine and the Anatomy of InjusticeFrom EverandInflamed: Deep Medicine and the Anatomy of InjusticeRating: 5 out of 5 stars5/5 (12)
- Heat Wave: A Social Autopsy of Disaster in ChicagoFrom EverandHeat Wave: A Social Autopsy of Disaster in ChicagoRating: 4 out of 5 stars4/5 (40)
- Breaking out of the Health Care Abyss: Transformational Tips for Agents of ChangeFrom EverandBreaking out of the Health Care Abyss: Transformational Tips for Agents of ChangeNo ratings yet
- Epidemics and Society: From the Black Death to the PresentFrom EverandEpidemics and Society: From the Black Death to the PresentRating: 4.5 out of 5 stars4.5/5 (9)
- Healthy Buildings: How Indoor Spaces Drive Performance and ProductivityFrom EverandHealthy Buildings: How Indoor Spaces Drive Performance and ProductivityRating: 5 out of 5 stars5/5 (2)
- The Hair Color Mix Book: More Than 150 Recipes for Salon-Perfect Color at HomeFrom EverandThe Hair Color Mix Book: More Than 150 Recipes for Salon-Perfect Color at HomeRating: 3.5 out of 5 stars3.5/5 (7)
- Money-Driven Medicine: The Real Reason Health Care Costs So MuchFrom EverandMoney-Driven Medicine: The Real Reason Health Care Costs So MuchRating: 4.5 out of 5 stars4.5/5 (11)
- Vaccine Injuries: Documented Adverse Reactions to VaccinesFrom EverandVaccine Injuries: Documented Adverse Reactions to VaccinesRating: 2.5 out of 5 stars2.5/5 (3)