Professional Documents
Culture Documents
Exam 1reference Sheet
Uploaded by
Andrea NortonOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Exam 1reference Sheet
Uploaded by
Andrea NortonCopyright:
Available Formats
Ass: 5-10 sec ABC’s: 1˚-color, LOC& position, neck/chest, subj.c/o,rhythm&pressure,IV,pulse,skin,caprefill,edema,analysis 2˚-auscultate,pupil,LE,abd,back,VS,hx,pul asses.
ABG: acidosis handled well, alk tolerated poorly Compensatory Mech: Buffer systems: weakens strong acids/bases
paCO2- 35-45 ↑ acid reflect of alveolar ventilation –rate&depth Pulmonary Sys: 1-3 min: eliminates/retains CO2
pH- 7.35-7.45 acd ↓ alk ↑ blood-measures free H+ ions. fatal: 6.8,7.8 Renal Sys: 24-48 hrs: elimn/retains HCO3, elim acids- (chronic)
HCO3- 22-26 alk ↑ met/renal part. Base Excess: only reflects balance/not problem pH WNL=complete compens. pH outside= partial compens.
PaO2 & SaO2:oxygenation of bld. OK:60-100 & >92%- Resp acid=hypovent/CO2 ↑ tx:ventilate! Met acid= acc of acids- anion gap
PaO2: parenchymal fxn, O2 avail->tissue; nl: 80-100 <60yrs; drops 1 q year; 65yo= Resp alk= hypervent/CO2 ↓ tx: under acidosis(high) ex Lactic Acidosis vs loss
75 , 80yo=60 -aff by paCO2, pH, temp SaO2: nl: >95% OK >92% lying cause. i.e. anxiety of bases non anion gap acidosis ex diarh
nl paO2/fiO2: = >300 tells shape of lungs (vent/CPAP); <300 ALI, <200 ARDS Shift to L: ˆpH, ˇDPG, ˇtemp bound Na-(Cl +HCO3)= 8-16 nl- non anion
resp failure= paO2<55-60 paCO2 25-35 saO2 <90% tx- airway, lowest FIO2, cause Shift to R: ˇpH, ˆDPG inc the abi of Tx : cause, NaHCO3 or Lactate
impaired O2 perfusion, lung vent, ↓ pulm circu, inspired oxy, blood O2 RBCs to release oxy,ˆtemp dissolved Met alk=usu loss of acids ex:↓K/ ↑bases
ex: antacids tx: cause, KCl-, NH3Cl
CV ↓CO=↓HR ↓SV ↓PL ↑AL ↓ CNT Afterload: force ejection Contractility: inotropy Norepi-alpha
Preload: stretch created by volume in vent just must oppose – WKLOAD! EF- echo/cath nl: 57-73% <50%bad Epi-beta and alpha
before they contract- LVEDV&RVEDVnl: 2-8 mmHg Nl: 800-1400 dynes/sec/cm <35% worse Alpha- peripheral vessels/stim
tx= low: fluids/vasopressor high:diuretics, vaso- ↓ AL=↑CNT ↑AL=↓ CNT -SV ratio to EDV: % ejected vasoconstriction
dilator,UF (SBP= DBP + PP) RV AL: pulm vas res CO= SV x HR: Beta1: myocardium
RV Preload: RVEDP: RAP or CVP PVR-100-250 -C.O./C.I: 4-8L/min C.I./BSA: 2.5-4.5L Stim: ˆino/chrono/dromo/automat,
LV Preload: LVEDP: LAP or PAOP/PAWP/PCWP LV AL: systemic SVR -Stroke Work Index LVSWI/RVSWI coronary vasodilation
nl: 6-12 mHg MAP- actual perfusion pressure tx= low: same preload Nl: 50-62 g-m/m2 most sensitive indic Beta2: peri vessels/bronchioles
{(2x DBP) + SBP}/3 high: vasodilator/ tx agg f ↑CO= ↑HR ↑SV =↑PL ↓ AL ↑ CNT Stim: vasodilat/bronchodilat
(PP=SBP-DBP)
Transducer maintenance leveling/zeroing phlebostatic axis (4th ICS/ ½ AP diameter 1 cm above= 0.73 mmHg decrease/ 1 inch+ 1.87 mm Hg dec
Fast-flush Square Wave Test: Right Dominant Circulation: R coronary
NL: 1-2 osc <.12 sec arteryRA(SA/AV node) + RV +inferior LV—Posterior
Overdamped: no ringing-blunted/ no osc below baseline descending artery PDA
false low SBP/false high DBP air bubbles, compliant L main coronary arteryLcircumflexLA+lateral wall—L
tubing, low/open connections, low fluid level in flush bag anterior descending LADanterior wall of RV, apical wall
Underdamped: mult osc above & below baseline Left Dominant Circulation: PDA fed by circumflex
artificially spiked false high SBP/fals e low DBP artery- L circumflex LA+lateral wall+anterior wall of
small air bubbles, tubing too long, defective transducer RV+apical wall+inferior wall
PAC: CO/CI, preload, contractility/afterload©, 02 delivery & consumption PCWP/PAOP/PAWP: nl: 6-12
RAP=CVP: 2-8 mm Hg/ 8-10 cm H2O R side preload PCWP=LAP=LVEDP=LV prload
RV=20-30/0-8 mmHg sys-RV ejection diast-RVEDP same as (RAP) High: ↑volume, ↓contract, mitral
PAP= pulmRVartery pressure-
PA 20-30/8-15 mmHg PAP mean- 10-20 mmHg sys- RVejet regurg or stenosis
RA PCW
diastHIGH pulm HTN, pul Dx, hypervolemia LOW hypovolemia Low: hypvolemia, RV failure
PAS= pulm artery sys- 20-30 RV ejection PAD= PCWP if NL condition w/o
Distal: PA Proximal: RA Balloon: wedging
PAD= pulm artery diast (mean)-10 20 PA vasc tone meds/pulm issues
Thermistor: for C.O. VIP fluid port
CVC: preload, contractility/afterload©,02 delivery & consumpt* CVC Complication: electrical, infection,
-indicator: circulatory vol, venous return, RV compliance circ impairment: hemorrhage- disconnect, dislodge, open stopcock
High- inc preload, inc volume, failure of ventricle air embolism: 1)mill wheel murmur (churning) d/t R vent outflow 2) gasp reflex d/t hypoxemia tx:
Low- low preload, hypvolemic, dec venous return d/t vasodilators L lateral trendelenberg- air to apex where it can be aspirated/reabsorb
A-Line SC/IJ: BP, CO/CI*,contractility/afterload©, Allen test hydrothorax: loss of breath sounds- catheter in pleural space
ADHF: dyspnea,fatigue, fluid retention ADHF TX: #1 Preload: IV Diuretics, IV Vasodilator( NTG, Nesiritide (BNP),
Sys HF: ↓contraction, ↓ ejection, EF<40% Dias HF: ↓vent filling, ↓relaxation; EJ nl nitroprusside -S/E not for liver), Slow Ultrafiltration #2 Afterload #3 Inotropes-
No NSAIDs & TZDs:Actos & Avandia d/t fluid retention Milirone: potent Dobutamine: beta drug of choice inc contract & vasodilation,
BNP: >100pg/ml: hf, 100-500 tx with IV diuretics, add nesiritide if >500 admit tx asap dopamine- dose specific >10 mcg vasoconstriction thus inc. AL.
confirmed pul congest, borderline hemodynamic instability, imp. Renal fx., Pulm edema: + pressure O2 CPAP,preload&afterload reduction, intotropes
--Cong/↓Perf @ rest C&D, PCW ↓, CI ↓= inotrop. C&W, PCW ↑=vasodilator Cardio shock (inad. Tissue perf): C.I. <2.2 tx: maintain O2 vent, preload&afterload
tx: OXY-(CPAP, intubation prn), PRELOAD, AFTERLOAD, INOTROPES-contract reduction, introtropics necessary, IABP/mech assist
ACS: dyspnea, nausea, cold sweats, sense of doom, fatigue SV= nl: 60-100ml Guidelines STEMI: same as UA/STEMI MS:2-4,8prn but Revascularize:
Unstable angina: nonocclusive, no cell injury, T wave inversion BB: blks adrenaline PCI or Thrombolytics is preferred intervention.
and/or ST depression, Cardiac Enz: NL ACEI: blocks ACE Tx Goals (ACS): 1. Inc. coronary blood supply-restore blood flow
NSTEMI: nonocclusive, ishc->partial thickness nontransmural ARB: blks agioten II Anti-plt therapy: ASA, Anti-thrombin Agents, Nitrates, STEMI:
necrosis, t wave inversion and/or ST depress, cardiac enz: high MCC: blks release of ALD revascularize via PCI/thrombolytics 2. Dec. Myocardial O2 demand-limit
Guidelines UA/NSTEMI: d/c NSAIDS, O2, ASA 162- Alpha blker: blk NEPI infarct size –Dec workload-Beta-Blockers, pain relief, nitrates. Goal: PCI:
325mg,NTG SL/spray q5minx3-IVdrip till sx relief, MS, BB, Cablk: ↓HR ↓bp ↓o2 dem w/ in 12hrs &Door-Balloon <90 min-unless: inexperienced ctr, or >1hr
Plavix, Antithrombin, GPllb/lla inhibitor, ACEI-only if HTN/DM, Cardiac Enzymes: delay > than expected time to thrombolytics; Thrombolytic Tx: w/in 12hrs
Angiography/ Revascularization. Myoglob & Door Drug <30 mi-only if sx dur </= 3hrs & expected time to balloon
STEMI: Injury: occlusive, transmural/full thickness cell necrosis, Troponin 1,T >1hr than expected time to thrombolytics.
ST elev. (MI in prog), cardiac enz: high, AMI= ST elevation w/ Q CKMB
wave
ARF: inadequate gas exchange/ hypoxemia- ↓paO2, ↑ pCO2 Shunt: ARDS:Acute, ALI/ARDS p/F <=300/200,bilat diffuse infiltrates,PCWP<18,refract
alveoli blocked, cap perf. Ǿ respond to O2 need CPAP VQ MM: alv semi hypoxemia Mgmt: ventilator low vol 6-8 ok hypercapnia pCO2 >80, PEEP,
blocked,responds to O2 Dead space: vent/ Ǿperf. Mgmt: O2>90%, IRV,maintain C.O. but keep dry, proning ↑PaO2 >10 or ↑ p/f >20% w/in 2 hrs=
bronchdil,steroids,sed,neuroblock,analge.Pose good lung down, plan activity/ responder.
rest,hydrate to loose secretion, pul-exer:C/DB hold 3secs x10/hr. ADHF:
Congestion @ rest, Low perf @ rest: Cold & wet, PCW ↑, CI ↓ = Vasodilator
(NTG)
ФCongestion @ rest, Low perf @ rest: Cold & dry, PCW ↓/nl, CI ↓= Inotropes
You might also like
- Perfusion for Congenital Heart Surgery: Notes on Cardiopulmonary Bypass for a Complex Patient PopulationFrom EverandPerfusion for Congenital Heart Surgery: Notes on Cardiopulmonary Bypass for a Complex Patient PopulationRating: 5 out of 5 stars5/5 (2)
- DMDudzinski EKG Algorithm4Document1 pageDMDudzinski EKG Algorithm4nate simmons100% (1)
- Lecture Notes On CardiologyDocument31 pagesLecture Notes On CardiologyambiskuysNo ratings yet
- RHC in PH FinalDocument36 pagesRHC in PH FinalKirti KadianNo ratings yet
- CCC Nurs 235 - Pediatric & Maternity NursingFinal Study GuideDocument13 pagesCCC Nurs 235 - Pediatric & Maternity NursingFinal Study GuideHeidi HeffelfingerNo ratings yet
- Cardiovascular Sequence, October 2000: A Wave in Atrial PressureDocument5 pagesCardiovascular Sequence, October 2000: A Wave in Atrial PressureMohamed KhattabNo ratings yet
- FA 2020 - Cardio Sterling Curve PDFDocument15 pagesFA 2020 - Cardio Sterling Curve PDFDrbee10No ratings yet
- CCRN CardiacDocument39 pagesCCRN CardiacMike100% (5)
- Clinical Congenital Heart Disease: Prof M S Ranjit MD DCH Senior Consultant Paed. Cardiologist ChennaiDocument78 pagesClinical Congenital Heart Disease: Prof M S Ranjit MD DCH Senior Consultant Paed. Cardiologist ChennaiAnişoara FrunzeNo ratings yet
- Congenital Heart Diseases ReviewDocument2 pagesCongenital Heart Diseases ReviewQworldNo ratings yet
- Downloadfile 28Document31 pagesDownloadfile 28Chowdhury Mohammed Tawhid TasneefNo ratings yet
- Ebook Hupperts Notes Pathophysiology and Clinical Pearls For Internal Medicine PDF Full Chapter PDFDocument67 pagesEbook Hupperts Notes Pathophysiology and Clinical Pearls For Internal Medicine PDF Full Chapter PDFmartha.delancey633100% (26)
- CCRN-PCCN-CMC Review Cardiac Part 3Document18 pagesCCRN-PCCN-CMC Review Cardiac Part 3Giovanni MictilNo ratings yet
- FP-C ReviewDocument71 pagesFP-C ReviewJamesNo ratings yet
- ABA OSCE ReviewDocument25 pagesABA OSCE ReviewJohn Smith100% (1)
- Hupperts Notes Pathophysiology and Clinical Pearls For Internal Medicine Laura Huppert Full ChapterDocument67 pagesHupperts Notes Pathophysiology and Clinical Pearls For Internal Medicine Laura Huppert Full Chapterannette.reese953100% (6)
- Httpsboardsandbeyoend Image.s3.Us East 1.amazonaws - compublicdocumentsStep1SlidesCardiologySlides2021 FullSize 3 PDFDocument1,036 pagesHttpsboardsandbeyoend Image.s3.Us East 1.amazonaws - compublicdocumentsStep1SlidesCardiologySlides2021 FullSize 3 PDFcnikhila93No ratings yet
- CARDIODocument10 pagesCARDIOMarcel TabucolNo ratings yet
- High Yield Surgery Shelf Exam Review CompleteDocument10 pagesHigh Yield Surgery Shelf Exam Review CompleteAmir Ali100% (1)
- Hemodynamic Failure March 2016Document61 pagesHemodynamic Failure March 2016Adriana VillarrealNo ratings yet
- Review of HD Monitoring: DR Ghaleb Almekhlafi MD, SFCCM, EdicDocument105 pagesReview of HD Monitoring: DR Ghaleb Almekhlafi MD, SFCCM, EdicGHALEB A. Almekhlafi100% (1)
- Notes To RewriteDocument6 pagesNotes To RewriteEunice Angela FulguerasNo ratings yet
- Clin Med For PAsDocument32 pagesClin Med For PAsMaryNguyen100% (2)
- Swan Ganz FinalDocument36 pagesSwan Ganz FinalDanial HassanNo ratings yet
- Septic Shock: Mixed Venous Oxygen Saturation IncreasedDocument1 pageSeptic Shock: Mixed Venous Oxygen Saturation IncreasedAsfand Yar KakarNo ratings yet
- Ankle Brachial Index, RandomDocument4 pagesAnkle Brachial Index, Randomkabal321No ratings yet
- Physiology Slides UsmleDocument46 pagesPhysiology Slides Usmlejustseas100% (1)
- Hemodynamic MonitoringDocument33 pagesHemodynamic MonitoringISICLE GTNo ratings yet
- Shock States Topic DiscussionDocument3 pagesShock States Topic Discussionapi-648891519No ratings yet
- Hemodinamik Dasar Invasive 2Document27 pagesHemodinamik Dasar Invasive 2Tkv UhamkaNo ratings yet
- LVEDP TableDocument3 pagesLVEDP TablehollyuNo ratings yet
- Cardiovascular System ConditionsDocument4 pagesCardiovascular System ConditionsNinjaNo ratings yet
- Cardiology-3 HFDocument17 pagesCardiology-3 HFMahmoud RamadanNo ratings yet
- 6 CVS RegulationDocument55 pages6 CVS RegulationDisha SuvarnaNo ratings yet
- Medsurg NursingDocument3 pagesMedsurg NursingGeraldine TeneclanNo ratings yet
- System and Disease III ComprehensiveDocument46 pagesSystem and Disease III Comprehensivenasr234No ratings yet
- Pulmonary Artery Catheters and Hemodynamic MonitoringDocument32 pagesPulmonary Artery Catheters and Hemodynamic Monitoringjpsahni100% (1)
- Stenotic Lesions AaDocument7 pagesStenotic Lesions Aaprem kotiNo ratings yet
- Copy Monitoring HemodinamicDocument23 pagesCopy Monitoring HemodinamicwarmanlicyNo ratings yet
- EKG Interpretation NursingDocument14 pagesEKG Interpretation NursingTanya ViarsNo ratings yet
- PcicardDocument2 pagesPcicardWahdat100% (1)
- Hemodynamic MonitoringDocument41 pagesHemodynamic MonitoringSuresh KumarNo ratings yet
- MS4 Exam 2Document27 pagesMS4 Exam 2JessNo ratings yet
- ECG at A GlanceDocument53 pagesECG at A GlancePetrus TjiangNo ratings yet
- Ntiarrhythmic X: Use Mechanism of Action Toxicities NotesDocument3 pagesNtiarrhythmic X: Use Mechanism of Action Toxicities NotesthescarletpimpernelsNo ratings yet
- Cardiology CardiovascularExaminationDocument5 pagesCardiology CardiovascularExaminationSalifyanji SimpambaNo ratings yet
- Path of Blood FlowDocument10 pagesPath of Blood Flowkiki188No ratings yet
- Code Mnagment Repaired FEB 1 2017Document22 pagesCode Mnagment Repaired FEB 1 2017Mr. Tauqeer Ahmed Faculty Member FUCNNo ratings yet
- ECG Interpretation and Dysrhythmias: Karen L. O'Brien MSN, RN JAN 07Document60 pagesECG Interpretation and Dysrhythmias: Karen L. O'Brien MSN, RN JAN 07ampogison08No ratings yet
- 04-Role of Echo in Pulm Hypertion N EmbolismDocument57 pages04-Role of Echo in Pulm Hypertion N EmbolismSiska Istanah Wong SintingNo ratings yet
- Cardiac Study GuideDocument3 pagesCardiac Study GuideLindsay BirnbrichNo ratings yet
- NCLEX Cram SheetDocument6 pagesNCLEX Cram Sheetaishwariyapokharel55No ratings yet
- Blood Pressure Regulation MechanismsDocument68 pagesBlood Pressure Regulation MechanismsPhysiology by Dr RaghuveerNo ratings yet
- Hemodynamic MonitoringDocument111 pagesHemodynamic MonitoringVenkatesan AnnamalaiNo ratings yet
- Rosenberg Circulatory Assist DevicesDocument61 pagesRosenberg Circulatory Assist DevicesMilisha Albro100% (1)
- Cardio Pulmonary Final FrontierDocument10 pagesCardio Pulmonary Final Frontierdina sharafNo ratings yet
- Anatomy: Cardiac Symptoms Cardiac Examination ECG and X RayDocument27 pagesAnatomy: Cardiac Symptoms Cardiac Examination ECG and X RayEmey AlahmadNo ratings yet
- Cardiovascular SystemDocument24 pagesCardiovascular SystemCandice100% (1)
- Swan Gantz Catherter and The Meaning of Its ReadingsDocument67 pagesSwan Gantz Catherter and The Meaning of Its ReadingsNouman Hameed100% (1)
- BOC Clinical Chemistry ReviewDocument6 pagesBOC Clinical Chemistry ReviewBloody MarieNo ratings yet
- Introduction To ElectrolytesDocument13 pagesIntroduction To ElectrolytesMaam ShaNo ratings yet
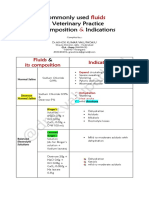
- Common IV Fluids at Composition & IndicationsDocument2 pagesCommon IV Fluids at Composition & IndicationsNilesh SuryawanshiNo ratings yet
- NCM 109 Finals NotesDocument21 pagesNCM 109 Finals NotesERIKA BOOTS CABALUNANo ratings yet
- Medical Surgical Nursing Cardio Vascular System ClassDocument15 pagesMedical Surgical Nursing Cardio Vascular System Classvallal100% (2)
- Lactic Acidosis and The Role of Sodium Bicarbonate: A Narrative Opinion Running Head: Lactic Acidosis and Sodium BicarbonateDocument38 pagesLactic Acidosis and The Role of Sodium Bicarbonate: A Narrative Opinion Running Head: Lactic Acidosis and Sodium BicarbonatentnquynhproNo ratings yet
- Chemistry: 25 Minutes 30 QuestionsDocument22 pagesChemistry: 25 Minutes 30 QuestionsAlex OlivarNo ratings yet
- NCLEX Study Notes 20080924Document61 pagesNCLEX Study Notes 20080924Shan Shan He100% (6)
- Abg Quiz in Class With Answers 1Document3 pagesAbg Quiz in Class With Answers 1Janae TaylorNo ratings yet
- Comp ReDocument9 pagesComp ReleninisanurseNo ratings yet
- NCM 112Document24 pagesNCM 112Amoroso, Marian Corneth D.No ratings yet
- 5 6231171839033344436Document454 pages5 6231171839033344436Amit KumarNo ratings yet
- Associations USMLEDocument99 pagesAssociations USMLEnu.bombinaNo ratings yet
- Acid Base ImbalancesDocument7 pagesAcid Base ImbalancesNicholas TagleNo ratings yet
- Fluid, Electrolyte, and Acid-BaseDocument6 pagesFluid, Electrolyte, and Acid-BaseRaquel MonsalveNo ratings yet
- Salicylates Tca ToxicityDocument54 pagesSalicylates Tca Toxicityapi-298936498No ratings yet
- All FormulasDocument3 pagesAll FormulasKevin Apeles100% (1)
- Acid-Base Balance: Graciela Lou F. Mana-Ay, RN, ManDocument68 pagesAcid-Base Balance: Graciela Lou F. Mana-Ay, RN, ManKeshia Joyce LimNo ratings yet
- Metabolic Encephalopaty PDFDocument46 pagesMetabolic Encephalopaty PDFRez QNo ratings yet
- DocxDocument99 pagesDocxVanessa AbboudNo ratings yet
- Medical Surgical Nursing ReviewDocument16 pagesMedical Surgical Nursing ReviewArda LynNo ratings yet
- Mcqs Fcps Feb 2018 Evening ShiftDocument20 pagesMcqs Fcps Feb 2018 Evening ShiftDrAttaullah ArbaniNo ratings yet
- Fundamentals of NursingDocument13 pagesFundamentals of NursingGiselle Chloe Baluya icoNo ratings yet
- Aspirin OverdoseDocument3 pagesAspirin OverdoseSaputra BismaNo ratings yet
- Interpretation of The Abnormal Laboratory Test .2Document11 pagesInterpretation of The Abnormal Laboratory Test .2Justine DumaguinNo ratings yet
- MK Combined PDFDocument93 pagesMK Combined PDFAnkit ChoudharyNo ratings yet
- Old Free 120 - Answers & Explanations (SP)Document63 pagesOld Free 120 - Answers & Explanations (SP)abdulahad mohamedNo ratings yet
- ShockDocument177 pagesShockISMAIL100% (1)
- Me Pediatrics Ntruhs Previous Question Papers Chapter WiseDocument9 pagesMe Pediatrics Ntruhs Previous Question Papers Chapter WiseNarendra AnnaladasuNo ratings yet
- Concept Map FinalDocument5 pagesConcept Map Finalapi-545001894No ratings yet