Professional Documents
Culture Documents
Ebn - Mad
Uploaded by
Emkhei Gonzales0 ratings0% found this document useful (0 votes)
54 views2 pagesCognitive behavioural therapy improved psychiatric symptoms in drug refractory schizophrenia. Only the CBT group continued to improve after the treatment ended. Patients showed no evidence of poorer adherence to medication.
Original Description:
Original Title
EBN- MAD
Copyright
© Attribution Non-Commercial (BY-NC)
Available Formats
PDF, TXT or read online from Scribd
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCognitive behavioural therapy improved psychiatric symptoms in drug refractory schizophrenia. Only the CBT group continued to improve after the treatment ended. Patients showed no evidence of poorer adherence to medication.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as PDF, TXT or read online from Scribd
0 ratings0% found this document useful (0 votes)
54 views2 pagesEbn - Mad
Uploaded by
Emkhei GonzalesCognitive behavioural therapy improved psychiatric symptoms in drug refractory schizophrenia. Only the CBT group continued to improve after the treatment ended. Patients showed no evidence of poorer adherence to medication.
Copyright:
Attribution Non-Commercial (BY-NC)
Available Formats
Download as PDF, TXT or read online from Scribd
You are on page 1of 2
Downloaded from ebn.bmj.com on April 16, 2011 - Published by group.bmj.
com
Cognitive behavioural therapy improved psychiatric
symptoms in drug refractory schizophrenia
Sensky T, Turkington D, Kingdon D, et al. A randomized controlled trial of cognitive-behavioral therapy for persistent
symptoms in schizophrenia resistant to medication. Arch Gen Psychiatry 2000 Feb;57:165–72.
QUESTION: Is cognitive behavioural therapy (CBT) more effective than a befriending
intervention for reducing psychiatric symptoms in drug refractory schizophrenia?
Design with ≥ 50% improvement in CPRS schizophrenia change
Randomised (allocation concealed), blinded (outcome scores (p = 0.06) (table). Groups did not differ for patients
assessors), controlled trial with 9 months of follow up with ≥ 50% improvement in MADRS or SANS scores.
after treatment.
Conclusion
Setting Cognitive behavioural therapy led to greater improve-
5 clinical services in the UK (Newcastle, Cleveland, Dur- ment in psychiatric symptoms at 9 months follow up
ham, and 2 in west London). than did a non-specific befriending intervention in
patients with drug refractory schizophrenia.
Patients
90 patients who were 16–60 years of age (mean age 39 y,
COMMENTARY
59% men, 89% white), met ICD-10 research and DSM-IV
criteria for schizophrenia, and had symptoms causing dis- A recent Cochrane review on the use of CBT for schizophre-
tress or dysfunction for ≥ 6 months despite adequate nia showed promising findings but recommended further
doses of antipsychotic drugs. Follow up was 100% for all large, methodologically rigorous trials.1 In their well designed
outcomes except for scores on the Scale for Assessment and controlled study, Sensky et al compare the role of CBT
of Negative Symptoms (SANS), which had 98% follow up. and befriending for drug resistant schizophrenia. Although
both groups showed improvements immediately after treat-
ment, only the CBT group continued to improve after the
Intervention treatment ended. Clinical improvements were greater for
Patients were allocated to CBT (n = 46) or befriending CBT than for befriending in all 4 outcome measures at 9
(n = 44). Both interventions were done by the same expe- months of follow up. At the beginning of the study, patients
rienced nurses. CBT involved attaining a collaborative showed no evidence of poorer adherence to medication, and
understanding of the development of symptoms and by the end of the study, the results could not be accounted for
working towards reducing distress and disability. The pro- by changes in antipsychotic medication.
vision of CBT was guided by a manual and regular super- Strengths of this study are randomised treatment alloca-
vision. Befriending involved sessions focused on neutral tion, blinded outcome assessors, audiotaped sessions to
ensure that the nurses delivered the assigned intervention,
topics (ie, hobbies, sports, and current affairs). Sessions
medication monitoring for all patients, and an adequate
were approximately 45 minutes/week for the first 2 follow up period accounting for all participants. Weaknesses
months with reduced frequency for the next 7 months are possible contamination by therapists conducting both
(mean total of 19 sessions). Patients in both groups were interventions, insufficient detail about the severity of patient
on antipsychotic medication throughout the study period. psychosis, inadequate social profiles (eg, socioeconomic
status) of participants to determine representativeness of
Main outcome measures study patients to all those with drug resistant symptoms, and
an absence of measures such as relapse and readmission rates.
Sources of funding: Scores on the Comprehensive Psychiatric Rating Scale
The positive findings suggest greater internalised ability
Wellcome Trust and (CPRS) (total and schizophrenia change scores), the
Hounslow and and skill acquisition by patients in the CBT group to control
Montgomery-Åsberg Depression Rating Scale (MADRS), or cope with their persistent symptoms at follow up, whereas
Spelthorne Community
and Mental Health and the SANS. those in the befriending group lost their initial gains once
National Health Service direct contact with the therapist ended. Given that up to 50%
Trust. of patients with schizophrenia are non-responsive to antipsy-
Main results
Analysis was by intention to treat. After treatment, chotic agents, effective psychological interventions, such as
For correspondence:
Dr T Sensky, Division of improvement was similar in each group. At 9 months fol- CBT, are viable alternatives or adjuncts to medication. The
Neurosciences and cost of specialised CBT training has not been accounted for in
Psychological Medicine,
low up, patients in the CBT group had greater improve-
this investigation and is recommended for future research. It
Imperial College School ment on all outcomes than did those in the befriending appears that CBT by trained and experienced therapists is
of Medicine, West group. More patients in the CBT group than in the effective for patients who are drug resistant and who do not
Middlesex University befriending group had ≥ 50% improvement in CPRS
Hospital, Isleworth, experience severe symptoms that would interfere with the
Middlesex TW7 6AF, total scores (p = 0.02); a trend existed toward more requirements of this intervention. Future research should
UK. t.skensky@ic.ac.uk patients in the CBT group than in the befriending group more clearly describe those patients who may benefit.
Jeannette LeGris, RN, MHSc
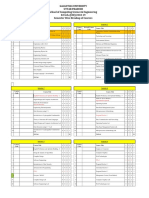
Cognitive behavioural therapy (CBT) v befriending in drug refractory schizophrenia* Clinical Nurse Specialist, Psychiatry
Outcomes at 9 months CBT Befriending RBI (95% CI) NNT (CI) Assistant Professor, School of Nursing
McMaster University
>50% improvement in CPRS Hamilton, Ontario, Canada
total scores 63% 39% 63% (8 to 157) 5 (3 to 28)
>50% improvement in CPRS 1 Jones C, Cormac I, Mota J, et al. Cognitive behaviour therapy
schizophrenia change scores 70% 50% 39% (−1 to 102) Not significant for schizophrenia (Cochrane Review, latest version 28 Jan
*CPRS=Comprehensive Psychiatric Rating Scale. Other abbreviations defined in glossary; RBI, NNT, and CI cal- 2000). In: Cochrane Library. Oxford: Update Software.
culated from data in article.
116 Volume 3 October 2000 EBN Treatment
Downloaded from ebn.bmj.com on April 16, 2011 - Published by group.bmj.com
Cognitive behavioural therapy improved
psychiatric symptoms in drug refractory
schizophrenia
BMJ Publishing Group Ltd and RCN Publishing Company Ltd
Evid Based Nurs 2000 3: 116
doi: 10.1136/ebn.3.4.116
Updated information and services can be found at:
http://ebn.bmj.com/content/3/4/116.full.html
These include:
References This article cites 1 articles, 1 of which can be accessed free at:
http://ebn.bmj.com/content/3/4/116.full.html#ref-list-1
Email alerting Receive free email alerts when new articles cite this article. Sign up in the
service box at the top right corner of the online article.
Topic Articles on similar topics can be found in the following collections
Collections
Interventional cardiology (7292 articles)
Drugs: psychiatry (1776 articles)
Psychotic disorders (incl schizophrenia) (2460 articles)
Notes
To request permissions go to:
http://group.bmj.com/group/rights-licensing/permissions
To order reprints go to:
http://journals.bmj.com/cgi/reprintform
To subscribe to BMJ go to:
http://group.bmj.com/subscribe/
You might also like
- Theories of AgingDocument4 pagesTheories of AgingEmkhei Gonzales100% (2)
- Theories of AgingDocument4 pagesTheories of AgingEmkhei Gonzales100% (2)
- CoxaDocument9 pagesCoxaEmkhei GonzalesNo ratings yet
- Patho OtotoxicityDocument2 pagesPatho OtotoxicityEmkhei GonzalesNo ratings yet
- Assessment Diagnosis Analysis Planning Intervention Rationale EvaluationDocument13 pagesAssessment Diagnosis Analysis Planning Intervention Rationale EvaluationEmkhei GonzalesNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Mooring Pattern Study For Q-Flex Type LNG Carriers Scheduled For Berthing at Ege Gaz Aliaga LNG TerminalDocument6 pagesThe Mooring Pattern Study For Q-Flex Type LNG Carriers Scheduled For Berthing at Ege Gaz Aliaga LNG TerminalMahad Abdi100% (1)
- Toolbox TalkDocument14 pagesToolbox Talkcall_mustafas2361No ratings yet
- I. Learning Objectives / Learning Outcomes: Esson LANDocument3 pagesI. Learning Objectives / Learning Outcomes: Esson LANWilliams M. Gamarra ArateaNo ratings yet
- The Checkmate Patterns Manual: The Ultimate Guide To Winning in ChessDocument30 pagesThe Checkmate Patterns Manual: The Ultimate Guide To Winning in ChessDusen VanNo ratings yet
- Industrial ExperienceDocument30 pagesIndustrial ExperienceThe GridLockNo ratings yet
- Simon Ardhi Yudanto UpdateDocument3 pagesSimon Ardhi Yudanto UpdateojksunarmanNo ratings yet
- 3D Printing & Embedded ElectronicsDocument7 pages3D Printing & Embedded ElectronicsSantiago PatitucciNo ratings yet
- Invisible CitiesDocument14 pagesInvisible Citiesvelveteeny0% (1)
- SG110CX: Multi-MPPT String Inverter For SystemDocument2 pagesSG110CX: Multi-MPPT String Inverter For SystemKatherine SmithNo ratings yet
- Highlights ASME Guides Preheat PWHT IDocument4 pagesHighlights ASME Guides Preheat PWHT IArul Edwin Vijay VincentNo ratings yet
- Module 6 Metal Properties and Destructive TestingDocument46 pagesModule 6 Metal Properties and Destructive TestingMiki Jaksic100% (6)
- Culture 2007 2013 Projects Overview 2018-03-18Document133 pagesCulture 2007 2013 Projects Overview 2018-03-18PontesDeboraNo ratings yet
- SP-Chapter 14 PresentationDocument83 pagesSP-Chapter 14 PresentationLoiDa FloresNo ratings yet
- KPI AssignmentDocument7 pagesKPI AssignmentErfan Ahmed100% (1)
- Johnson & Johnson Equity Research ReportDocument13 pagesJohnson & Johnson Equity Research ReportPraveen R V100% (3)
- Design of Reinforced Cement Concrete ElementsDocument14 pagesDesign of Reinforced Cement Concrete ElementsSudeesh M SNo ratings yet
- Crypto Wall Crypto Snipershot OB Strategy - Day Trade SwingDocument29 pagesCrypto Wall Crypto Snipershot OB Strategy - Day Trade SwingArete JinseiNo ratings yet
- Generation III Sonic Feeder Control System Manual 20576Document32 pagesGeneration III Sonic Feeder Control System Manual 20576julianmataNo ratings yet
- Claim of FactDocument11 pagesClaim of FactXeb UlritzNo ratings yet
- Alfa Week 1Document13 pagesAlfa Week 1Cikgu kannaNo ratings yet
- World War II D-Day Invasion by SlidesgoDocument55 pagesWorld War II D-Day Invasion by SlidesgoPreston SandsNo ratings yet
- CHARACTER FORMATION 1 PrelimDocument15 pagesCHARACTER FORMATION 1 PrelimAiza Minalabag100% (1)
- Galgotias University Uttar Pradesh School of Computing Science & Engineering B.Tech. (CSE) 2018-19 Semester Wise Breakup of CoursesDocument2 pagesGalgotias University Uttar Pradesh School of Computing Science & Engineering B.Tech. (CSE) 2018-19 Semester Wise Breakup of CoursesRohit Singh BhatiNo ratings yet
- A P P E N D I X Powers of Ten and Scientific NotationDocument5 pagesA P P E N D I X Powers of Ten and Scientific NotationAnthony BensonNo ratings yet
- Mcdaniel Tanilla Civilian Resume Complete v1Document3 pagesMcdaniel Tanilla Civilian Resume Complete v1api-246751844No ratings yet
- A.meaning and Scope of Education FinalDocument22 pagesA.meaning and Scope of Education FinalMelody CamcamNo ratings yet
- Institutional Group Agencies For EducationDocument22 pagesInstitutional Group Agencies For EducationGlory Aroma100% (1)
- Literature Review Template DownloadDocument4 pagesLiterature Review Template Downloadaflsigfek100% (1)
- Based On PSA 700 Revised - The Independent Auditor's Report On A Complete Set of General Purpose Financial StatementsDocument12 pagesBased On PSA 700 Revised - The Independent Auditor's Report On A Complete Set of General Purpose Financial Statementsbobo kaNo ratings yet
- Department of Education: Template No. 1 Teacher'S Report On The Results of The Regional Mid-Year AssessmentDocument3 pagesDepartment of Education: Template No. 1 Teacher'S Report On The Results of The Regional Mid-Year Assessmentkathrine cadalsoNo ratings yet