Professional Documents
Culture Documents
High Risk Mild Head Injury
Uploaded by
May JPOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
High Risk Mild Head Injury
Uploaded by
May JPCopyright:
Available Formats
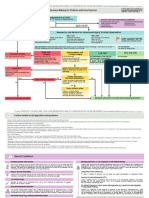
Initial Management of Adult Mild Head Injury
Initial GCS 14-15 on arrival following blunt trauma. Stabilise ABCDE’s then assess risk factors.
Low risk Mild Head Injury High risk Mild Head Injury
All of ... Any of ...
1 GCS 15 at 2 hours post injury. 1 Persistent GCS <15 at 2 hours post injury.
1 No focal neurological deficit. 1 Deterioration in GCS.
1 No clinical suspicion of skull fracture. ::1 1 Focal neurological deficit.
1 Brief loss of consciousness (<5 mins). 1 Clinical suspicion of skull fracture. ::1
1 Brief anterograde / retrograde amnesia (<30 mins). 1 Prolonged loss of consciousness (>5 mins).
1 No post traumatic seizure. 1 Prolonged anterograde / retrograde amnesia (>30 mins).
1 Mild nausea or single episode of vomiting. 1 Post traumatic seizure. ::2
1 Mild headache. 1 Persistent abnormal alertness / behaviour / cognition.
1 No known coagulopathy. 1 Persistent vomiting (2 or more occasions).
1 Age <65 years. 1 Persistent severe headache.
1 Isolated head injury without dangerous mechanism. 1 Known coagulopathy (eg warfarin / alcoholic).
1 No drug or alcohol ingestion. 1 Age >65 years. ::3
1 No known neurosurgery / neurological impairment. 1 Multi-system trauma. ::4
1 Dangerous mechanism. ::5
1 Clinically obvious drug or alcohol intoxication. ::6
Clinical observation until at least 1 Known neurosurgery / neurological impairment. ::7
four hours post time of injury. 1 Delayed presentation or representation. ::8
Abnormal alertness / behaviour / cognition. Indication for early CT scan and
Clinically deteriorates or not improving. prolonged clinical observation.
Normal during Normal CT Normal CT Abnormal CT scan. CT scan unavailable.
observation scan. Clinical scan. Clinical
period. symptoms symptoms NOT
improving at improving at Consider urgent transfer for CT scanning if:
4 hours post 4 hours post 1 Persistent GCS <15 at 2 hours post injury.
1 Deterioration in GCS.
time of injury. time of injury.
1 Focal neurological deficit.
1 Clinical suspicion of skull fracture.
1 Persistent abnormal mental status, vomiting or
severe headache at 4 hours post time of injury.
Clinically safe for discharge for home observation if: Admit for prolonged hospital observation and
1 Normal alertness / behaviour / cognition. consult regional neurosurgical service regarding
1 Clinically improving after observation.
further management and disposition.
1 Normal CT scan or no indication for CT scan.
1 Clinical judgment required if elderly and /
Note – Clinical judgement required
or known coagulopathy due to increased risk ::1 Clinical suspicion of skull fracture includes – history of focal blunt assault
NSW Institute of Trauma and Injury Management © January 2007 SHPN: (TI) 070032
of delayed subdural haematoma. or injury; large scalp lacerations or haematomas; signs of base of skull fracture
– haemotympanum / CSF leak / raccoon eyes / Battles sign.
::2 Post traumatic seizures – prolonged, focal or delayed seizures are significant risk
factors for intracranial injury but brief generalised seizures immediately following
Socially safe for discharge for home observation if: head injury are less concerning.
::3 Age >65yrs – elderly patients have increased risk of significant intracranial injury;
1 Responsible person available to take home and observe.
routine CT scanning unless totally asymptomatic patient with no other risk factors.
1 Able to return if deteriorates.
::4 Multi-system trauma – beware patients with unstable vital signs or distracting
1 Discharge advice is understood. injuries, as significant head injuries are easily missed.
::5 Dangerous mechanisms include MVA ejection / rollover; pedestrians / cyclists hit
by vehicle; falls >own height or five stairs; falls from horses / cycles etc; focal blunt
trauma, eg bat / ball / club.
Discharge for home observation ::6 Clinically obvious drug or alcohol intoxication with altered mental status is an indication
for CT scanning but drug or alcohol ingestion with normal mental status is not.
and provide written discharge advice.
::7 Known neurosurgery/neurological impairment – conditions such as hydrocephalus
with shunt or AVM or tumour or cognitive impairment from any cause make clinical
assessment less reliable and may increase risk of intracranial injury.
::8 Delayed presentation or representation – consider both intracranial injury
and post concussion symptoms and have a low threshold for CT scanning.
You might also like
- Head Injury 22Document0 pagesHead Injury 22Permata Ayu KamilaNo ratings yet
- Closed Head Injury CPG 2nd Ed Algorithm 2Document1 pageClosed Head Injury CPG 2nd Ed Algorithm 2Nick PaulNo ratings yet
- Head Injury EciDocument29 pagesHead Injury EciYullytia Galaksi MharyatiNo ratings yet
- Head Injury GoulburnDocument47 pagesHead Injury GoulburnSyarifah Maisyura100% (1)
- Initial Treatment For Closed Head Injuries PDFDocument1 pageInitial Treatment For Closed Head Injuries PDFdiaga081No ratings yet
- Head Trauma: Types of Resulting Brain InjuryDocument6 pagesHead Trauma: Types of Resulting Brain InjuryAnjali ParajuliNo ratings yet
- Update: Management of Head InjuriesDocument38 pagesUpdate: Management of Head InjuriesWilly OematanNo ratings yet
- Update: Management of Head InjuriesDocument38 pagesUpdate: Management of Head InjuriesRoby Aditya SuryaNo ratings yet
- Trauma KepalaDocument43 pagesTrauma KepalaAray Al-AfiqahNo ratings yet
- Case Study SDHDocument34 pagesCase Study SDHLisa Daniel HouselNo ratings yet
- Head InjuryDocument39 pagesHead InjuryYonathan asnakeNo ratings yet
- Head InjuryDocument34 pagesHead Injuryrxmskdkd33No ratings yet
- Cedera Kepala Dan Otak: Dr. Isnaniah, Sp. S Bagian Saraf Fkik UntadDocument91 pagesCedera Kepala Dan Otak: Dr. Isnaniah, Sp. S Bagian Saraf Fkik UntadSiwa MerthadinataNo ratings yet
- Acute Stroke Management by Carlos L Chua PDFDocument61 pagesAcute Stroke Management by Carlos L Chua PDFHynne Jhea EchavezNo ratings yet
- STROKE Mimic and Chameleons EDDocument34 pagesSTROKE Mimic and Chameleons EDMohammad LouayNo ratings yet
- Head Trauma (Head Injury) : Thitinan LimchoopornwikulDocument42 pagesHead Trauma (Head Injury) : Thitinan LimchoopornwikulPasut ChangeNo ratings yet
- Head InjuriesDocument7 pagesHead Injuriesapi-3822433100% (1)
- Management of Head Injuries (Open and ClosedDocument48 pagesManagement of Head Injuries (Open and ClosedAsmahan AliNo ratings yet
- Neurological 5Document39 pagesNeurological 5ta CNo ratings yet
- Kuliah Head Injury MakasarDocument113 pagesKuliah Head Injury MakasarJerrod WilsonNo ratings yet
- PREDICTALGORITHM v1 1 29.01.21Document2 pagesPREDICTALGORITHM v1 1 29.01.21selvi zhafirahNo ratings yet
- Head InjuryDocument50 pagesHead InjuryThiagarajah RaviNo ratings yet
- Traumatic Brain InjuryDocument88 pagesTraumatic Brain Injurympm8471No ratings yet
- Acute Monocular Vision LossDocument9 pagesAcute Monocular Vision LossRoberto López MataNo ratings yet
- Cerebral Concussion (Mini Case Study)Document8 pagesCerebral Concussion (Mini Case Study)Airalyn Chavez AlaroNo ratings yet
- AISDocument40 pagesAISMohamed AbdoNo ratings yet
- CBT Neurosurgery - TutorDocument24 pagesCBT Neurosurgery - Tutoramoody95No ratings yet
- Management of Mild Traumatic Brain InjuryDocument9 pagesManagement of Mild Traumatic Brain InjuryYaseerNo ratings yet
- Brain ScintigraphyDocument24 pagesBrain ScintigraphyDustin Miranda100% (1)
- CNUR 204 - Unit Ten - Neurological DisordersDocument18 pagesCNUR 204 - Unit Ten - Neurological DisordersAbby PohlNo ratings yet
- Traumatic Brain InjuryDocument39 pagesTraumatic Brain InjuryMORGAN LAMBERTNo ratings yet
- Semana 10 TECDocument42 pagesSemana 10 TECJenny Lopez BocangelNo ratings yet
- Head Injury 1Document22 pagesHead Injury 1ahmedfarghaly909090No ratings yet
- Traumatic Brain Injury: 2. Prophylactic HypothermiaDocument77 pagesTraumatic Brain Injury: 2. Prophylactic HypothermiaNinaNo ratings yet
- Craniocerebral Traumatology TBIDocument22 pagesCraniocerebral Traumatology TBIconfuisosNo ratings yet
- Module 56 - Group 4Document27 pagesModule 56 - Group 4Katherine May F. LloritoNo ratings yet
- Traumatic Brain Injury (TBI)Document48 pagesTraumatic Brain Injury (TBI)Alaa OmarNo ratings yet
- Head Trauma: Drs. Afnan Abdirahman MBBS Elrazi University General Surgery Resident (UOH/IMU)Document30 pagesHead Trauma: Drs. Afnan Abdirahman MBBS Elrazi University General Surgery Resident (UOH/IMU)DrRahma Ali HeissNo ratings yet
- Head Traumas: Anthony Safi Mediii Neurosurgery RotationDocument17 pagesHead Traumas: Anthony Safi Mediii Neurosurgery RotationAnthony safiNo ratings yet
- Head Injury: Which Patients Need Imaging? Which Test Is Best?Document5 pagesHead Injury: Which Patients Need Imaging? Which Test Is Best?crushnaNo ratings yet
- Trauma Kepala Handy 2020Document45 pagesTrauma Kepala Handy 2020NandatholoeNo ratings yet
- General Surgery Trauma (Head and Thorax)Document24 pagesGeneral Surgery Trauma (Head and Thorax)Noora AlmuailiNo ratings yet
- Traumatic Brain Injury (TBI) : Epidural Hematoma Subdural HematomaDocument62 pagesTraumatic Brain Injury (TBI) : Epidural Hematoma Subdural HematomaRey AlwiwikhNo ratings yet
- Algoritma TBIDocument3 pagesAlgoritma TBIravenskaNo ratings yet
- Head Injuries 2Document4 pagesHead Injuries 2canndy202No ratings yet
- Cerebral ConcussionDocument4 pagesCerebral Concussionnur_shakirin0% (1)
- Neurological EmergenciesDocument11 pagesNeurological Emergenciespunit lakraNo ratings yet
- First Seizure-RCEMDocument2 pagesFirst Seizure-RCEMalsadiqbr5No ratings yet
- Medical-Surgical Nursing: Primary Brain TumorDocument20 pagesMedical-Surgical Nursing: Primary Brain TumorYejiNo ratings yet
- HEAD INJURY (Trauma Kepala) DR - AgusDocument53 pagesHEAD INJURY (Trauma Kepala) DR - AgusSetyo RahmanNo ratings yet
- NeurologyDocument37 pagesNeurologyDevangkumar PatelNo ratings yet
- Head InjuryDocument30 pagesHead InjuryAngel MakinNo ratings yet
- 9 5神經系統Document59 pages9 5神經系統陳姿螢No ratings yet
- Daf Ter Noo NDocument45 pagesDaf Ter Noo NpolaggariNo ratings yet
- Tbi 100121072336 Phpapp02Document74 pagesTbi 100121072336 Phpapp02Luther ThengNo ratings yet
- Head Injury 2022.Document45 pagesHead Injury 2022.Alia QNo ratings yet
- Head Trauma: Kelompok 2: Andry Wongso Rhiza M.I.S Terri S. S PriscillaDocument22 pagesHead Trauma: Kelompok 2: Andry Wongso Rhiza M.I.S Terri S. S PriscillaJenadi BinartoNo ratings yet
- Managing - Patients - With - Severe - Traumatic - Brain WITH HIGHLIGHTSDocument8 pagesManaging - Patients - With - Severe - Traumatic - Brain WITH HIGHLIGHTSTre OfficialNo ratings yet
- Management of Head Injury in Primary CareDocument77 pagesManagement of Head Injury in Primary CareChidi MbatuegwuNo ratings yet
- Primary and Secondary SurveyDocument10 pagesPrimary and Secondary SurveyBernadeth Meily100% (1)
- G01-Initial Assessment and Management of The Multiply Injured PatientDocument48 pagesG01-Initial Assessment and Management of The Multiply Injured Patientkosmynin86No ratings yet
- Estioko FractureDocument10 pagesEstioko FractureJewell EstiokoNo ratings yet
- Wound CareDocument30 pagesWound Carerumaisha100% (2)
- Fracture ClassificationDocument50 pagesFracture ClassificationsrhubanbabuNo ratings yet
- Traumatic Brain Injury and Cerebral ResuscitationDocument56 pagesTraumatic Brain Injury and Cerebral ResuscitationsyahirNo ratings yet
- By. Kaimuddin Disampaikan Pada Pelatihan BTCLS Batam, 21 September 2012Document15 pagesBy. Kaimuddin Disampaikan Pada Pelatihan BTCLS Batam, 21 September 2012Lusy Angriani ManurungNo ratings yet
- Introduction To Basic Life SupportDocument20 pagesIntroduction To Basic Life SupportJyle Mareinette ManiagoNo ratings yet
- Penetrating Abdominal Trauma in The Era of Selective Conservatism: A Prospective Cohort Study in A Level 1 Trauma CenterDocument9 pagesPenetrating Abdominal Trauma in The Era of Selective Conservatism: A Prospective Cohort Study in A Level 1 Trauma CenterDewi HenssaNo ratings yet
- Injury ManagementDocument20 pagesInjury Managementnizam_skabbNo ratings yet
- ArticlesDocument4 pagesArticleschris7982No ratings yet
- Fraktur Dan DislokasiDocument77 pagesFraktur Dan DislokasiRicky Jawwa0% (1)
- Musculoskeletal TraumaDocument68 pagesMusculoskeletal TraumaRismayanti HairilNo ratings yet
- Clinical Skill Handout Forensic Medicine and MedicolegalDocument20 pagesClinical Skill Handout Forensic Medicine and MedicolegalCici MutiaNo ratings yet
- Acetabular Fractures UW Emergency RadiologyDocument1 pageAcetabular Fractures UW Emergency RadiologyDr.upendra goudNo ratings yet
- Check List For AmbulanceDocument2 pagesCheck List For AmbulanceEka B100% (1)
- CPR Test and AnswersDocument2 pagesCPR Test and AnswersjoesphsteelNo ratings yet
- Hemorrhagic Shock Classification in Pediatric TraumaDocument1 pageHemorrhagic Shock Classification in Pediatric TraumaPrisia AnantamaNo ratings yet
- Avulsion and Degloving InjuryDocument12 pagesAvulsion and Degloving InjuryandicaNo ratings yet
- PPTDocument29 pagesPPTAkosh BB100% (1)
- Abdominal TraumaDocument47 pagesAbdominal TraumaWidya Rahayu100% (1)
- Acute and Chronic WoundDocument18 pagesAcute and Chronic WoundNawal FarooqNo ratings yet
- Fracture of The Talus and Calcaneus NickDocument43 pagesFracture of The Talus and Calcaneus NickTan Zhi HongNo ratings yet
- 5607TNCC-Abdominal TraumaDocument65 pages5607TNCC-Abdominal Traumabagus100% (1)
- Defibrillator - HeartStart - PhilipsDocument72 pagesDefibrillator - HeartStart - PhilipseryNo ratings yet
- PHTLS 9Document2 pagesPHTLS 9Luis Alexander0% (2)
- Daftar PustakaDocument2 pagesDaftar PustakaputriNo ratings yet
- Airway ManagementDocument4 pagesAirway Managementpaveethrah100% (1)
- Advanced Trauma and Surgery PDFDocument455 pagesAdvanced Trauma and Surgery PDFyuliandiazhadi100% (1)
- First Aid BookletDocument37 pagesFirst Aid BookletLeNo ratings yet