Professional Documents
Culture Documents
Arterial Pressure Allows Monitoring The Changes In.98440
Uploaded by
Jihad MallatOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Arterial Pressure Allows Monitoring The Changes In.98440
Uploaded by
Jihad MallatCopyright:
Available Formats
Arterial pressure allows monitoring the changes in cardiac output
induced by volume expansion but not by norepinephrine*
Xavier Monnet, MD, PhD; Alexia Letierce, PhD; Olfa Hamzaoui, MD; Denis Chemla, MD, PhD;
Nadia Anguel, MD; David Osman, MD; Christian Richard, MD; Jean-Louis Teboul, MD, PhD
Objective: To evaluate to which extent the systemic arterial in pulse pressure of >17% allowed detecting a fluid-induced
pulse pressure could be used as a surrogate of cardiac output for increase in cardiac output of >15% with a sensitivity of 65[56 –
assessing the effects of a fluid challenge and of norepinephrine. 72]% and a specificity of 85[76 –92]%. The area under the receiver
Design: Observational study. operating characteristic curves for the fluid-induced changes in
Setting: Medical intensive care unit. mean arterial pressure and in diastolic arterial pressure was
Patients: Patients with an acute circulatory failure who received significantly lower than for pulse pressure. In group 2, the intro-
a fluid challenge (228 patients, group 1) or in whom norepinephrine duction/increase of norepinephrine significantly increased car-
was introduced or increased (145 patients, group 2). diac output by 14% ! 18%. The changes in cardiac output
Interventions: We measured the systolic, diastolic, and mean induced by the introduction/increase in the dose of norepineph-
arterial pressure, pulse pressure, and the transpulmonary ther- rine were correlated with the changes in pulse pressure and
modilution cardiac output before and after the therapeutic inter- systolic arterial pressure (r # .21 and .29, respectively, p # .001)
ventions. but to a significantly lesser extent than in group 1.
Main Results: In group 1, the fluid challenge significantly Conclusions: Pulse pressure and systolic arterial pressure
increased cardiac output by 24% ! 25%. It significantly increased could be used for detecting the fluid-induced changes in cardiac
cardiac output by >15% ("35% ! 27%) in 142 patients (“re- output, in spite of a significant proportion of false-negative cases.
sponders”). The fluid-induced changes in cardiac output were By contrast, the changes in pulse pressure and systolic arterial
correlated with the changes in pulse pressure (r # .56, p < pressure were unable to detect the changes in cardiac output
.0001), systolic arterial pressure (r # .55, p < .0001), diastolic induced by norepinephrine. (Crit Care Med 2011; 39:000 – 000)
arterial pressure (r # .37, p < .0001), and mean arterial pressure KEY WORDS: fluid challenge; volume expansion; norepinephrine;
(r # .52, p < .0001). At multivariate analysis, changes in pulse vasopressors; arterial pressure; cardiac output; arterial compli-
pressure were significantly related to changes in stroke volume ance; pulse wave amplification
(multiple r # .52) and to age (r # .12). A fluid-induced increase
I n patients with an acute circula- measure cardiac output in patients with tionship between PP and stroke volume is
tory failure, the question whether ventricular failure or persistent shock de- affected by two physiologic phenomena: the
cardiac output should be moni- spite adequate fluid resuscitation (1). Al- arterial compliance and, if PP is measured
tored or not is still a matter of though these recommendations are not at the peripheral level, the pulse wave am-
debate. Recent guidelines recommend to supported by a high level of evidence, plification phenomenon (3). Since vaso-
they suggest that a “basic” hemodynamic pressors might alter both arterial compli-
monitoring based on the sole arterial ance and pulse wave amplification to a
pressure might be sufficient for monitor- larger extent than volume expansion, the
*See also p. 000.
From the Service de Réanimation médicale (XM, ing initial fluid resuscitation but insuffi- ability of PP to reflect the changes in stroke
OH, NA, DO, CR, J-LT) and Unité de Recherche clinique cient for monitoring later resuscitation volume (and cardiac output) might be bet-
(AL), Hôpital de Bicêtre, AP-HP, Le Kremlin-Bicêtre; with fluid and vasopressors (1). ter for fluid therapy than for vasopressors,
Faculté de Médecine Paris-Sud (XM, OH, DC, NA, DO, but this has never been demonstrated.
Since it tends to maintain arterial pres-
CR, J-LT), Univ Paris-Sud, Le Kremlin-Bicêtre; and Thus, in the present study, we inves-
Service de Physiologie (DC), Hôpital Antoine Béclère, sure stable while cardiac output varies, the
AP-HP, Clamart, France. sympathetic regulation might preclude us- tigated to what extent PP could be used
Supplemental digital content is available for this ar- ing arterial pressure for monitoring the for indicating absolute values and treat-
ticle. Direct URL citations appear in the printed text and
treatment-induced changes of cardiac out- ment-induced changes of cardiac output
are provided in the HTML and PDF versions of this article in a large population of patients with an
on the journal’s Web site (http://www.ccmjournal.com). put. However, among the different values of
Dr. Monnet and Dr. Teboul consulted for Pulsion. arterial pressure, the pulse pressure (PP, acute circulatory failure treated with
The remaining authors have not disclosed any poten- i.e., the difference between systolic [SAP] fluid and norepinephrine.
tial conflicts of interest.
and diastolic [DAP] arterial pressure) is
For information regarding this article, E-mail: METHODS
xavier.monnet@bct.aphp.fr physiologically related to stroke volume
Copyright © 2011 by the Society of Critical Care (2). It might thus be able to reflect the Patients. This study was approved by our
Medicine and Lippincott Williams & Wilkins changes in cardiac output induced by dif- institutional review board. A deferred consent
DOI: 10.1097/CCM.0b013e31820edcf0 ferent treatments. Nevertheless, the rela- was asked from the patient’s surrogate as soon
Crit Care Med 2011 Vol. 39, No. 6 1
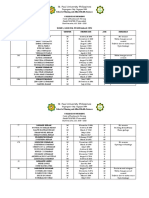
Table 1. Patients characteristics at baseline also used some other definitions of the fluid
responsiveness: an increase in cardiac output
Patients With of "10%, an increase in stroke volume of
Patients Receiving an Introduction/ "15%, and an increase in stroke volume of
Volume Expansion Increase of NE "10%.
Characteristic (n ! 228) (n ! 145)
Statistical Analysis. All continuous vari-
ables except the dose of norepinephrine were
Gender (no of patients, F/M) 95/133 58/87
normally distributed at Kolmogorov-Smirnov
Age (mean " SD, years) 63 " 13 63 " 12
Simplified acute physiology score II (mean " SD) 52 " 11 43 " 18 test. Results are expressed as mean " SD, as
Type of shock (no of patients, %) median (25%–75% interquartile range) or as
Septic 193 (85) 145 (100) mean (95% confidence interval), as appropri-
Hypovolemic 14 (6) 0 (0) ate. Comparisons of variables between before
Post cardiac arrest 8 (4) 0 (0) vs. after fluid administration were assessed by
Drug poisoning 7 (3) 0 (0) using a paired Student’s t test. Comparisons
Other 6 (2) 0 (0) between responders vs. nonresponders were
Patients receiving NE at baseline (no. of patients, %) 212 (93) 86 (59) assessed by using a two-sample Student’s t test
NE dose at baseline (median &25%–75% 0.5 &0.3–1.1' 0.5 &0.2–0.7'
or a Mann-Whitney U test, as appropriate. Cor-
interquartile', #g/kg/min)
relations were assessed by the Pearson coeffi-
Acute respiratory distress syndrome (no. of patients, %) 137 (61) 73 (50)
cient and correlation coefficients were com-
There was no statistical difference between groups. pared between group 1 and group 2 using the
NE, norepinephrine. Fisher transformation (8). The correlation
analysis was also performed in the four quar-
tiles of age of the total population. A stepwise
regression analysis was performed to look for
as possible. As he/she recovered conscious- itoring kit (Pulsion Medical Systems, Munich,
independent variables related to the changes
ness, a deferred consent was asked from the Germany) and invasive arterial pressure was
in PP (in %). A p value of $.20 was necessary
patient. If the patient or his/her next of kin measured by the PiCCO-Plus or PiCCO-2 de-
for a variable to enter regression analysis.
refused to consent, patient’s data were not vice. Before all pressure measurements, the
Elsewhere, a p value of $.05 was considered
entered into analysis. arterial line was carefully flushed and zeroed
statistically significant. In group 1, receiver
We included patients (1) if they presented to atmospheric pressure. For the measure-
operating characteristic (ROC) curves (with
an acute circulatory failure defined by the ment of cardiac output, the values of three
95% confidence intervals) were constructed
presence of at least one of the following crite- thermodilution measurements were averaged.
for testing the ability of the fluid-induced
ria: 1) SAP !90 mm Hg (or fall of SAP "50 The PiCCO-Plus and the PiCCO-2 devices both
changes in SAP, DAP, MAP, and PP to predict
mm Hg in patients previously known as hy- measure cardiac output and arterial pressure fluid responsiveness. The areas under the ROC
pertensive), 2) urinary flow !0.5 mL/kg/min in a similar way. curves were compared using a Hanley-McNeil
for more than 2 hrs, 3) tachycardia "100 Study Design. Before fluid infusion in test (9). Since the two groups of patients could
beats/min, or 4) presence of skin mottling and group 1 and before the introduction/increase have different arterial pressures at baseline, we
(2) if a fluid challenge was administered in the dose of norepinephrine in group 2, a also analyzed the data in a subpopulation of
(group 1, n ! 228 patients) or if norepineph- transpulmonary thermodilution was per- each groups with matched baseline MAP (for
rine was introduced or its dose was increased formed and the values of cardiac output, detailed methods, see Supplemental Digital
(group 2, n ! 145 patients, different from stroke volume, global end-diastolic volume, Content 1, http://links.lww.com/CCM/A228).
and extravascular lung water (all obtained The statistical analysis was performed by using
patients of group 1), as ordered by the attend-
from transpulmonary thermodilution), the the Statview5.0 software (Abacus Concepts,
ing physician. The decision to administer fluid
values of SAP, DAP, mean arterial pressure Berkeley, CA) and the MedCalc8.1.0.0 software
and to introduce/increase the dose of norepi-
(MAP), and PP were recorded. (Mariakerke, Belgium).
nephrine was based on standard care criteria
In group 1, a 500-mL saline bolus was
(e.g., positive fluid responsiveness indicators
infused over 20 min. In this group, norepi-
for fluid, low arterial pressure for vasopres-
nephrine was administered at baseline (in 228 RESULTS
sors). Patients’ characteristics at baseline are
patients) and its dose was unchanged during Effects of the Therapeutic Interven-
listed in Table 1. Twenty-two patients were not
fluid infusion. In group 2, norepinephrine was tions on Hemodynamic Variables. In
ventilated. Among the overall 353 patients
introduced (in 59 patients) at a dose of 0.24
who were intubated, 70 were ventilated in the group 1 (n ! 228 patients), volume ex-
(0.13– 0.48) #g/kg/min or its dose was in-
pressure support mode. Among the 283 re- pansion increased cardiac output by 24%
creased (in 86 patients) from 0.48 (0.24 – 0.71)
maining patients, all of whom were ventilated " 25% (p $ .05). It significantly in-
#g/kg/min to 0.62 (0.43–1.07) #g/kg/min.
in the assist control mode, 223 exhibited some creased cardiac output of "15% (%35%
The values of cardiac output, stroke vol-
spontaneous triggering of the ventilator. In
ume, global end-diastolic volume, and ex-
" 27%) in 142 patients (“responders”)
patients ventilated in the assist-control mode, (Table 2). In the 86 remaining patients of
travascular lung water, the values of SAP,
tidal volume was 6.5% " 2.1% mL/kg. group 1 (“nonresponders”), volume ex-
DAP, MAP, and PP were also obtained after the
Measurements. All patients had an internal pansion significantly increased cardiac
therapeutic intervention, i.e., immediately af-
jugular vein catheter and a thermistor-tipped output by 7% " 5% (Table 2). In the
arterial catheter (PV2015L20N, Pulsion Medi- ter fluid infusion in group 1 and 5 min after
the stabilization of MAP in group 2. Since whole group 1, volume expansion in-
cal Systems, Munich, Germany) in the femoral
predicting fluid responsiveness is an impor- creased SAP, DAP, MAP, and PP by 15%
artery that was connected to a PiCCO-Plus or
a PiCCO-2 device (Pulsion Medical Systems, tant issue in critically ill patients, we separated " 19%, 9% " 16%, 13% " 17%, and
Munich, Germany) for measuring cardiac out- patients in group 1 between “fluid responders” 21% " 29%, respectively (Table 2). The
put through transpulmonary thermodilution. and “fluid nonresponders.” A positive fluid re- magnitude of these changes was signifi-
The femoral arterial catheter was connected to sponse was defined by a treatment-induced cantly larger in responder than in nonre-
the pressure sensor PV8215 by a PV8215 mon- increase in cardiac output of "15% (4 –7). We sponder patients (Table 2).
2 Crit Care Med 2011 Vol. 39, No. 6
Table 2. Hemodynamic variables in patients receiving volume expansion (n ! 228) first quartile of age (from 36 to 53 yrs,
n ! 59), r ! .48 (p ! .0001) for the
Before Volume After Volume
second quartile of age (from 54 to 62
Variable Category Expansion Expansion
yrs, n ! 50), r ! .54 (p $ .0001) for the
Heart rate (mean "SD, beats/min) Nonresponders 92 " 23 90 " 22a third quartile of age (from 63 to 74 yrs,
Responders 98 " 22 96 " 21a,b n ! 70), r ! .68 (p $ .0001) for the
Systolic arterial pressure (mean " SD, mm Hg) Nonresponders 107 " 24 115 " 26a fourth quartile of age (from 75 to 88
Responders 109 " 21 129 " 23a,b yrs, n ! 49).
Diastolic arterial pressure (mean " SD, mm Hg) Nonresponders 52 " 13 55 " 13a
Responders 53 " 13 59 " 13a,b
In group 2, the changes (in %) in
Mean arterial pressure (mean " SD, mm Hg) Nonresponders 71 " 16 75 " 16a cardiac output induced by the introduc-
Responders 71 " 14 82 " 16a,b tion/increase in dose of norepinephrine
Pulse arterial pressure (mean " SD, mm Hg) Nonresponders 56 " 19 60 " 20a were correlated with the changes (in %)
Responders 56 " 18 70 " 18a,b in PP (r ! .21, p ! .001, Fig. 2), SAP (r !
Global end-diastolic volume (mean " SD, mL/m2) Nonresponders 703 " 185 808 " 280a
Responders 649 " 203b 766 " 264a,b .29, p ! .004), and MAP (r ! .21, p !
Extravascular lung water (mean " SD, mL/kg Nonresponders 11 " 5 11 " 5 .01) but not in DAP (r ! .13, p ! .12).
predicted body weight) All these correlations were significantly
Responders 10 " 6 10 " 5 lower than in group 1 (p ! .0001, .003,
Cardiac index (mean " SD, L/min/m2) Nonresponders 3.2 " 1.0 3.4 " 1.1a and .0007 for the changes in PP, SAP,
Responders 2.7 " 0.9b 3.5 " 1.1b
and MAP, respectively). The changes (in
“Responders” refers to patients in whom volume expansion increased cardiac index by "15% (n ! %) in stroke volume induced by the
86). “Nonresponders” refers to the other patients (n ! 142). introduction/increase in dose of norepi-
a
p $ .05 vs. before volume expansion (comparisons in rows); bp $ .05 vs. nonresponders nephrine were correlated with the
(comparisons in columns). changes (in %) in PP (r ! .17, p ! .04),
SAP (r ! .18, p ! .003), and MAP (r !
Table 3. Hemodynamic variables in patients with an introduction/increase of norepinephrine .17, p ! .04) but not in DAP (r ! (.01,
(n ! 145) p ! .92). All these correlations were
significantly lower than in group 1 (p !
Before Introduction/ After Introduction/ .0007, .007, and .02 for the changes in
Increase of Increase of
PP, SAP, and MAP, respectively). Multi-
Variable Norepinephrine Norepinephrine
variate analysis indicated that the
Heart rate (mean " SD, beats/min) 97 " 22 96 " 21 changes in PP (in %) were related to the
Systolic arterial pressure (mean " SD, mm Hg) 83 " 14 120 " 21a changes (in %) in stroke volume (r !
Diastolic arterial pressure (mean " SD, mm Hg) 39 " 7 52 " 9a .17) but not to age.
Mean arterial pressure (mean " SD, mm Hg) 54 " 8 75 " 10a Ability of the Changes in Arterial
Pulse arterial pressure (mean " SD, mm Hg) 45 " 14 67 " 22a
Global end-diastolic volume (mean " SD, mL/m2) 692 " 137 735 " 154a
Pressure to Detect Fluid Responsiveness
Extravascular lung water (mean " SD, mL/kg 10 " 4 10 " 5 in Group 1. The ability of the changes in
predicted body weight) the different values of arterial pressure to
Cardiac index (mean " SD, L/min/m2) 3.1 " 1.0 3.5 " 1.1a detect a fluid-induced increase in cardiac
a
output of "15% in group 1 is described
p $ .05 vs. before introduction/increase in NE (comparisons in rows). in Table 4 and Figure 2. The fluid-
induced changes in PP and in SAP exhi-
bited the best diagnostic values, with
In group 2 (n ! 145 patients), the ume were correlated with the changes similar areas under the ROC curves. A
introduction/increase in dose of norepi- (in %) in PP (r ! .49, p $ .0001), SAP fluid-induced increase in PP of "17%
nephrine increased cardiac output by (r ! .44, p $ .0001), DAP (r ! .25, p ! allowed detecting a fluid-induced in-
14% " 18% (p $ .05) (Table 3). In the .0002), and MAP (r ! .39, p $ .0001). crease in cardiac output of "15% with a
whole group 2, the introduction/ There was not statistical difference be- sensitivity of 65% (95% confidence inter-
increase in the dose of norepinephrine tween the r coefficients found for the val: 56%–72%) and a specificity of 85%
significantly increased SAP, DAP, MAP, correlation between changes in cardiac (95% confidence interval: 76%–92%),
and PP by 46% " 30%, 9% " 16%, output and change in PP on the one i.e., with 6% and 22% of false-positive
38% " 24%, and 41% " 23%, respec- side and for the correlation between and false-negative cases, respectively. The
tively (Table 3). changes in cardiac output and changes area under the ROC curves for the fluid-
Relationship Between the Changes in in SAP on the other side. Multivariate induced changes in MAP and for the flu-
Arterial Pressure and the Changes analysis indicated that the changes in id-induced changes in DAP was signifi-
in Cardiac Output and Stroke Volume. In PP (in %) were significantly related to cantly lower than for the fluid-induced
group 1, the fluid-induced changes (in the changes in stroke volume (r ! .52) changes in PP (Table 4). The areas under
%) in cardiac output were correlated and to age (r ! .12). When the popula- the ROC curve describing the ability of
with the changes (in %) in PP (r ! .56, tion was divided in 4 quartiles of age, the fluid-induced changes in PP to detect
p $ .0001) (Fig. 1), SAP (r ! .55, p $ the changes (in %) in PP were related to a fluid-induced increase in cardiac output
.0001), DAP (r ! .37, p $ .0001), and the changes (in %) in stroke volume for of "15% were not different among pa-
MAP (r ! .52, p $ .0001). The fluid- all quartiles with different coefficients tients belonging to the first, the second,
induced changes (in %) in stroke vol- of correlation: r ! .40 (p ! .002) for the the third, and the fourth age quartiles
Crit Care Med 2011 Vol. 39, No. 6 3
A B DISCUSSION
*
This study suggests that PP and SAP
r = 0.56 r = 0.21
300
n = 228
300
n = 145 could be used for detecting the changes
by the introduction/increase in NE
in cardiac output induced by a fluid chal-
Changes in PP (in %) induced
Changes in PP (in %) induced
250 250
lenge, in spite of a significant proportion
by the fluid challenge
200 200
of false-negative cases in which PP and
150 150
SAP did not change while cardiac output
100 100 increased. By contrast, the changes in PP
50 50 and SAP were unable to detect the
0 0
changes in cardiac output induced by the
norepinephrine.
-50 -50
-50 0 50 100 150 200 250 300 -50 0 50 100 150 200 250 300 When taking care of patients with cir-
Changes in CO (in %) induced Changes in CO (in %) induced culatory shock, the question is frequently
by the fluid challenge by the introduction/increase in NE pending whether cardiac output must be
Figure 1. Correlation between the changes in arterial pulse pressure (PP, in % change from baseline) monitored or if a basic monitoring with
and cardiac output (CO, in % change from baseline) induced by a fluid challenge (A, n ! 228 pairs of the sole arterial pressure will be suffi-
measurements) and by the introduction or increase in dose of norepinephrine. (B, n ! 145 pairs of cient. International guidelines recom-
measurements). *p ! .0001 vs. r in A. mend monitoring cardiac output in pa-
tients with shock refractory to initial
100 fluid therapy (1), but this is not sup-
ported by a substantial scientific back-
ground. The goal of the present study was
80 to provide some physiologic basis to this
guideline.
In the first place, our study indicates
Sensitivity (%)
60
that the different values of arterial pres-
sure are not equivalent for monitoring
the treatment-induced changes in stroke
40
Diagnostic ability of
volume or cardiac output. Physiologi-
the fluid-induced changes (in %) in: PP cally, the changes in MAP are dissociated
20 SAP
from the changes in cardiac output due
to the sympathetic modulation of the ar-
MAP
terial tone, which tends to maintain MAP
0
DAP constant while cardiac output varies (10).
0 20 40 60 80 100 According to this physiologic paradigm,
100-Specificity (%) we found that the changes in MAP were
Figure 2. Receiving Operating Characteristics curves describing the ability of the fluid-induced unable to reflect the changes in cardiac
changes (in %) in arterial pulse (PP) and systolic (SAP), diastolic (DAP), and mean (MAP) arterial output induced either by fluid infusion or
pressure to detect a fluid-induced increase in cardiac index of "15%. by the introduction or increase in norepi-
nephrine. In particular, the introduction/
increase in norepinephrine augmented
(0.81 " 0.05, 0.78 " 0.07, 0.78 " 0.05, Influence of Baseline Arterial Pres- MAP to a large extent, but this was re-
and 0.80 " 0.06, respectively). Similar sure. The analysis of the subsets of groups lated to arterial vasoconstriction and not
results were obtained when using dif- 1 and 2 matched for baseline MAP showed correlated with a simultaneous change in
ferent definitions of fluid responsive- similar results than in the whole popula- stroke volume or cardiac output.
ness (see Supplemental Digital Content tion (see Supplemental Digital Content, Another physiologic paradigm is that,
1, http://links.lww.com/CCM/A228). http://links.lww.com/CCM/A228). in contrast with MAP, PP is directly re-
Table 4. Diagnostic ability of the fluid-induced changes in arterial pressures values to detect a fluid-induced increase in cardiac index of "15% in patients
receiving fluid infusion (group 1)
Area Under the Positive Negative
Receiver Operating p vs. Best Cutoff Predictive Predictive Youden
Variable Characteristic Curve .500 Value Sensitivity Specificity Value Value Index
Changes in arterial pulse pressure 0.784 " 0.03 .0001 17% 65 &56–72' 85 &76–92' 88 &80–93' 59 &50–68' 0.50
Changes in systolic arterial pressure 0.757 " 0.03 .0001 8% 74 &66–81' 67 &57–77' 79 &71–85' 61 &51–71' 0.41
Changes in mean arterial pressure 0.692 " 0.04a .001 13% 46 &38–55' 84 &74–91' 82 &72–90' 49 &40–57' 0.30
Changes in diastolic arterial pressure 0.598 " 0.04a .01 11% 67 &29–45' 83 &73–90' 78 &66–87' 44 &37–52' 0.50
n ! 228, mean " SD or mean &95% confidence interval'.
a
p $ .05 vs. changes in arterial pulse pressure.
4 Crit Care Med 2011 Vol. 39, No. 6
lated to stroke volume (2). In theory, PP diac output was poor. This indicates that by norepinephrine than by volume expan-
might thus be a better candidate for mon- changes of mechanical properties of the sion (17).
itoring the changes in cardiac output at arterial system induced by norepineph- To summarize, the changes in PP or
the bedside (3). However, PP is also in- rine, including arterial compliance and SAP but not in MAP could help for de-
versely correlated with arterial compli- pulse wave amplification, were so marked tecting the hemodynamic effects of a
ance, which might differ among patients that PP could not be used for tracking fluid challenge. If PP increased "17%
and might change over time in a same trends in cardiac output. Nevertheless, an during the fluid challenge, one may sup-
patient (11). Furthermore, the propor- important limitation of our study was pose with acceptable confidence that car-
tionality between PP and stroke volume is that we did not precisely investigate arte- diac output increased "15%. By contrast,
physiologically expected at the aortic rial compliance and the pulse wave am- if PP did not increase "17% during the
level but not at the peripheral arterial due plification phenomenon. fluid challenge, one could not ascertain
to the pulse wave amplification phenom- As a clinical application, the present that cardiac output did not improve. The
enon (2). In the present study, we quan- study clarifies in which manner clinicians changes in PP or SAP could not be used
tified the extent to which these two phys- should use arterial pressure for monitor- for monitoring the effects of norepineph-
iologic issues preclude to use the changes ing therapy during circulatory failure, rine on cardiac output.
in PP for detecting the changes in stroke with very different attitudes regarding
volume and cardiac output. fluid and vasopressors. The results sug- ACKNOWLEDGMENTS
In group 1, the fluid-induced changes gest that when PP increases "17% with
in PP were significantly correlated with We are greatly indebted to Prof. Lau-
fluid administration, the clinician can be
the fluid-induced changes in cardiac out- rence Meyer, from the Department of
reasonably confident that a patient is
put. These results are in line with those Epidemiology and Public Health of
fluid responsive (6% of false-positive
of previous small human studies in which Bicêtre Hospital, for her help in statis-
cases only). By contrast, if PP does not
a decrease in PP paralleled the decrease tical analysis.
increase "17%, the high number of
in stroke volume induced by graded low false-negative cases (22%) precludes
body negative pressure (12) or compres- drawing any reasonable conclusion con- REFERENCES
sion of the right atrium (13). In our cerning fluid responsiveness. This issue 1. Antonelli M, Levy M, Andrews PJ, et al: He-
study, the correlation with the fluid-
might be particularly relevant when per- modynamic monitoring in shock and impli-
induced changes in PP was not better for
forming repetitive fluid challenges, a pro- cations for management. International Con-
the fluid-induced changes in stroke vol- sensus Conference, Paris, France, 27–28
cedure that has been recently revisited
ume than for the fluid-induced changes April 2006. Intensive Care Med 2007; 33:
(14). Underestimating the response of
in cardiac output, since heart rate was 575–590
cardiac output to fluid boluses might
not decreased to a large extent by volume 2. Chemla D, Hébert JL, Coirault C, et al:
clearly lead to fluid under-resuscitation.
expansion in our study population. In Total arterial compliance estimated by
Concerning the monitoring of norepi- stroke volume-to-aortic pulse pressure ra-
turn, the changes in PP exhibited a good
nephrine administration, PP cannot be tio in humans. Am J Physiol 1998; 274:
diagnostic accuracy for detecting fluid re-
sponsiveness. This indicates that PP was used for assessing the effects that norepi- H500 –H505
an acceptable surrogate of cardiac output nephrine can exert on stroke volume (15, 3. Lamia B, Chemla D, Richard C, et al: Clinical
16). However, despite our results might review: Interpretation of arterial pressure
for assessing the effects of fluid therapy. wave in shock states. Crit Care 2005;
Since DAP was only slightly modified by change routine practice, their clinical
relevance is highly limited by the fact 9:601– 606
volume expansion, SAP (i.e., the sum of 4. Michard F, Boussat S, Chemla D, et al: Rela-
DAP and PP) exhibited a similar diagnos- that this study was not designed for evi-
tion between respiratory changes in arterial
tic accuracy. dencing any different impact of arterial pulse pressure and fluid responsiveness in
Although the fluid-induced changes in pressure vs. cardiac output monitoring septic patients with acute circulatory failure.
PP and SAP and in cardiac output were on outcome. This issue should be inves- Am J Respir Crit Care Med 2000; 162:
significantly correlated, these correla- tigated in further studies. 134 –138
tions were not excellent (r ! .56 and .55, Some monitoring devices use the 5. Monnet X, Osman D, Ridel C, et al: Predict-
physiologic relationship between the am- ing volume responsiveness by using the end-
respectively). This might be related to the
plitude of the arterial curve and stroke expiratory occlusion in mechanically venti-
physiologic issues of arterial compliance lated intensive care unit patients. Crit Care
and pulse wave amplification phenome- volume for estimating cardiac output
Med 2009; 37:951–956
non (10). According to this hypothesis, from an arterial line. For this purpose, 6. Monnet X, Rienzo M, Osman D, et al: Esoph-
we found that the coefficient of correla- these devices estimate arterial compl- ageal Doppler monitoring predicts fluid re-
tion between changes in PP and in stroke iance and vasomotor tone from a complex sponsiveness in critically ill ventilated pa-
volume induced by the fluid challenge analysis of the arterial pressure curve tients. Intensive Care Med 2005; 31:
was lower in the youngest patients, in and, for some of these systems, with help 1195–1201
whom the arterial compliance was as- of an external calibration (17). In accor- 7. Monnet X, Rienzo M, Osman D, et al: Passive
dance with our results, the fact that leg raising predicts fluid responsiveness in
sumed to be higher and the pulse wave
the critically ill. Crit Care Med 2006; 34:
amplification lower than in the oldest. changes in arterial compliance and/or va-
1402–1407
In group 2, it is not surprising that somotor tone are more marked with nor- 8. Fisher RA: Statistical Methods for Research
norepinephrine increased DAP and MAP, epinephrine than with fluid therapy Workers. Fourteenth Edition. Edinburgh,
which are related to the arterial tone (3). might explain why some systems have London, UK, Oliver & Boyd, 1970
By contrast, an interesting finding was greater difficulty to reliably estimate the 9. Hanley JA, McNeil BJ: A method of compar-
that the relationship between PP and car- changes in cardiac output when induced ing the areas under receiver operating char-
Crit Care Med 2011 Vol. 39, No. 6 5
acteristic curves derived from the same central hypovolemia. J Trauma 2006; 61: septic patients with life-threatening hypoten-
cases. Radiology 1983; 148:839 – 843 629 – 634 sion. Crit Care 2010; 14:R142
10. Nichols W, O’Rourke M: Contours of pressure 13. Marquez J, McCurry K, Severyn DA, et al: 16. Monnet X, Jabot J, Maizel J, et al: Norepi-
and flow waves in arteries. In: Blood Flow in Ability of pulse power, esophageal Doppler, nephrine increases cardiac preload and re-
Arteries. Nichols W, O’Rourke MS (Eds). London, and arterial pulse pressure to estimate rapid duces preload dependency assessed by pas-
UK, Oxford University Press; 1998, pp 170–200 changes in stroke volume in humans. Crit sive leg raising in septic shock patients Crit
11. O’Rourke B: Evidence for mitochondrial K% Care Med 2008; 36:3001–3007 Care Med 2011; In Press
channels and their role in cardioprotection. 14. Vincent JL, Weil MH: Fluid challenge re- 17. Monnet X, Anguel N, Naudin B, et al: Arterial
Circ Res 2004; 94:420 – 432 visited. Crit Care Med 2006; 34:1333–1337 pressure-based cardiac output in septic pa-
12. Convertino VA, Cooke WH, Holcomb JB: Ar- 15. Hamzaoui O, Georger JF, Monnet X, et al: tients: Different accuracy of pulse contour
terial pulse pressure and its association with Early administration of norepinephrine in- and uncalibrated pressure waveform devices.
reduced stroke volume during progressive creases cardiac preload and cardiac output in Crit Care 2010; 14:R109
6 Crit Care Med 2011 Vol. 39, No. 6
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (345)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- APPROVED PP-US-2817 v1 HPI Algorithms PresentationDocument19 pagesAPPROVED PP-US-2817 v1 HPI Algorithms PresentationNat SNo ratings yet
- ACC ECG 2.fullDocument8 pagesACC ECG 2.fullRajendra ChavanNo ratings yet
- Unit Three: The Heart: Chapter 9: Cardiac Muscle The Heart As A Pump and Function of The Heart ValvesDocument36 pagesUnit Three: The Heart: Chapter 9: Cardiac Muscle The Heart As A Pump and Function of The Heart ValvesEbaa Moh'd ZayadnehNo ratings yet
- CvsDocument35 pagesCvsVISS11No ratings yet
- Nursing Care Plan For HypertentionDocument2 pagesNursing Care Plan For HypertentionLunnet Begg100% (1)
- Cardiac Arrythmias in The ED Menbeu Edited From AnaDocument106 pagesCardiac Arrythmias in The ED Menbeu Edited From AnaTemesgen Geleta100% (1)
- Daftar Poster CaseDocument6 pagesDaftar Poster Casebagusputrabali13No ratings yet
- Chapter18 TheCardiovascularSystem TheHeartDocument7 pagesChapter18 TheCardiovascularSystem TheHeartChelsea CunninghamNo ratings yet
- St. Paul University Philippines: School of Nursing and Allied Health SciencesDocument12 pagesSt. Paul University Philippines: School of Nursing and Allied Health SciencesKarina MadriagaNo ratings yet
- Cape Exercise LabDocument2 pagesCape Exercise Labanisa aliNo ratings yet
- White Coat HypertensionDocument7 pagesWhite Coat HypertensionarfikNo ratings yet
- Membaca Ekg Untuk PemulaDocument15 pagesMembaca Ekg Untuk PemulaChristopher NjotokusgitoNo ratings yet
- The Assessment of Blood Pressure in Atrial FibrillationDocument4 pagesThe Assessment of Blood Pressure in Atrial FibrillationThatikala AbhilashNo ratings yet
- E Cart MedicationsDocument12 pagesE Cart Medicationsbalong1219No ratings yet
- Valvular Heart Diseases: Cardiology, Med Ii - 3Rd YearDocument11 pagesValvular Heart Diseases: Cardiology, Med Ii - 3Rd YearMiguel Cuevas DolotNo ratings yet
- ACLS Study Guide NewDocument35 pagesACLS Study Guide NewNIRANJANA SHALININo ratings yet
- Cardiovascular Review QuestionsDocument48 pagesCardiovascular Review Questionsgnikap_deleon0% (1)
- Basic ECG Interpretation MWDocument211 pagesBasic ECG Interpretation MWLorelie AsisNo ratings yet
- Kinns The Medical Assistant An Applied Learning Approach 13Th Edition Proctor Test Bank Full Chapter PDFDocument49 pagesKinns The Medical Assistant An Applied Learning Approach 13Th Edition Proctor Test Bank Full Chapter PDFsiliquavexinglygmnfo100% (10)
- Checklist CPR 2018 PDFDocument2 pagesChecklist CPR 2018 PDFCarissa Tirtania100% (3)
- Hypertension: Signs and SymptomsDocument7 pagesHypertension: Signs and SymptomsAdinia NugrahiniNo ratings yet
- ECG WorldDocument139 pagesECG WorldsatyaNo ratings yet
- Medical Surgical Nursing - Cardiovascular System DisordersDocument11 pagesMedical Surgical Nursing - Cardiovascular System DisordersSofia LiNo ratings yet
- DCLT?Document5 pagesDCLT?My selfNo ratings yet
- Cardiac Implantable Electronic DevicesDocument49 pagesCardiac Implantable Electronic DevicespriyathasanNo ratings yet
- Dr. G.N. Prabhu Associate Professor Cardiothoracic Surgery SRM MCH & RCDocument60 pagesDr. G.N. Prabhu Associate Professor Cardiothoracic Surgery SRM MCH & RCNithya SekarNo ratings yet
- SA Exit Block (Andrea Romandini)Document10 pagesSA Exit Block (Andrea Romandini)Swempi Melchiadi AbollaNo ratings yet
- Daftar Pustaka: Medical Students and Faculty - Edisi Keempat - Baltimore-PhiladelpiaDocument2 pagesDaftar Pustaka: Medical Students and Faculty - Edisi Keempat - Baltimore-PhiladelpiaSylvia PertiwiNo ratings yet
- Name: Patient ID: Incident ID: 2582 Device: Device Configuration: Software Revision: LP12 21X LP1230214429 2G04Krokg3Ggbj 3011371-090Document1 pageName: Patient ID: Incident ID: 2582 Device: Device Configuration: Software Revision: LP12 21X LP1230214429 2G04Krokg3Ggbj 3011371-090Anonymous h9utL1tiNo ratings yet
- Assessing Heart and Neck Vessel Heart Heart Chambers: (Tricuspid & Bicuspid)Document7 pagesAssessing Heart and Neck Vessel Heart Heart Chambers: (Tricuspid & Bicuspid)Dan Floyd FernandezNo ratings yet