Professional Documents
Culture Documents
Medical Billing Specialist
Uploaded by
api-77992927Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Medical Billing Specialist
Uploaded by
api-77992927Copyright:
Available Formats
Mina D.
Jones
1812 Woodcrest Walk
Lithonia, Ga. 30058
404-207-3303
mja5c83e@westpost.net
OBJECTIVE:
Over 20 years experience as a medical management specialist with proficiencies i
n the following areas: Medical billing and coding,extensive follow-up research,
Medicare/Medicaid regulations,
Managed Care and Commercial Insurances, Customer Service and Front Office/Back O
ffice and interpersonal and communication skills. PC proficient Premis, Medical
Manager, Amazing Charts,Web Portal Medicaid, Medicare and Navinet,Blue Cross,etc
. Ability to organize time and detail-oriented. Extensive use of medical termino
logy, icd9/cpt coding. Software: Medical Manager, Centricity,Medisoft, Premis, p
osting payments,charges and adjustments, aged accounts, submissions of claims el
ectronically.
WORK EXPERIENCE:
LifeCycle Midwife Associates, June 2010-August 2010 Medical Biller
Responsible for all billing duties, including denials, inputting charges, rebill
ing, extensive
Follow-up on aged accounts and current, rebilling of claims, and uploading claim
s to clearinghouse.
Primary Family Care, PC. December 2009- April 2010 Medical Biller
Responsible for all commercial and managed care billing of pediatric claims, res
ubmission of claims, file rejections, posting of payments daily from Blue Cross,
Aetna, Cigna and United Healthcare as well as other managed care carriers and c
ommercial carriers. Corrections of diagnosis and procedure code errors, extensiv
e followup on all claims via web portal usage and calling of insurance carriers.
Inputting charges,payments,followup of aged accounts.
Atlanta Obstetrics and Family Care,P.C. March 2009-Sept. 2009 Medical Office Ass
istant
Handled all facets of the front desk, greeting patients, registering new patient
s, collecting copayments and past balances, answering calls from patients, docto
rs, hospitals, etc.,referrals to specialists, assisting in back office with vita
l signs of patients, requesting reports and consultations from hospitals and con
sultants.
Equivision, Inc., Atlanta, Ga. October 2003-Jan. 2009 MedicalBiller Analysis cor
respondence and Eobs to insure timely claim process, denial of services, co-paym
ents and additional information needed for processing. Extensive follow-up and r
esearch of rejected and denials of claims, calling insurance carriers on a daily
basis to resolve claim issues and receive payments, working on aged reports on
older claims, all facets of medical billing.
EDUCATION:
Ribault High School, Jacksonville, Fla. 1976, Florida A&M University,1981.
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Health Problem Family Nusing Problem Goals of Care Objectives of CareDocument8 pagesHealth Problem Family Nusing Problem Goals of Care Objectives of CareMyrshaida IbrahimNo ratings yet
- In Holland V Hodgson The ObjectDocument5 pagesIn Holland V Hodgson The ObjectSuvigya TripathiNo ratings yet
- Ethics - FinalsDocument18 pagesEthics - Finalsannie lalangNo ratings yet
- City Living: Centro de Lenguas ExtranjerasDocument2 pagesCity Living: Centro de Lenguas Extranjerascolombia RodriguezNo ratings yet
- ADDICTED (The Novel) Book 1 - The Original English TranslationDocument1,788 pagesADDICTED (The Novel) Book 1 - The Original English TranslationMónica M. Giraldo100% (7)
- Final Draft Investment Proposal For ReviewDocument7 pagesFinal Draft Investment Proposal For ReviewMerwinNo ratings yet
- Book - IMO Model Course 7.04 - IMO - 2012Document228 pagesBook - IMO Model Course 7.04 - IMO - 2012Singgih Satrio Wibowo100% (4)
- Logical Remarks On The Semantic Approach PDFDocument34 pagesLogical Remarks On The Semantic Approach PDFFelipe SantosNo ratings yet
- Assignment 1 TVM, Bonds StockDocument2 pagesAssignment 1 TVM, Bonds StockMuhammad Ali SamarNo ratings yet
- If He Asked YouDocument10 pagesIf He Asked YouLourdes MartinsNo ratings yet
- Edu 536 - Task A2 - pld5Document3 pagesEdu 536 - Task A2 - pld5api-281740174No ratings yet
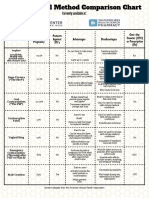
- Birth Control Comparison Chart 2018Document1 pageBirth Control Comparison Chart 2018Eric SandesNo ratings yet
- MNT-Notes Pt. 2Document58 pagesMNT-Notes Pt. 2leemon.mary.alipao8695No ratings yet
- Rules of SyllogismDocument6 pagesRules of Syllogismassume5No ratings yet
- I. Title: "REPAINTING: Streetlight Caution Signs"Document5 pagesI. Title: "REPAINTING: Streetlight Caution Signs"Ziegfred AlmonteNo ratings yet
- Sepulveda v. de Las CasasDocument2 pagesSepulveda v. de Las CasasNova GaveNo ratings yet
- Karaf-Usermanual-2 2 2Document147 pagesKaraf-Usermanual-2 2 2aaaeeeiiioooNo ratings yet
- Glgq1g10 Sci Las Set 4 ColoredDocument4 pagesGlgq1g10 Sci Las Set 4 ColoredPogi AkoNo ratings yet
- Finlatics Investment Banking Experience ProgramDocument4 pagesFinlatics Investment Banking Experience ProgramSameer BheriNo ratings yet
- SjshagavDocument6 pagesSjshagavindah ayu lestariNo ratings yet
- XS2 Pharma 0512 103 UK U-NiDocument2 pagesXS2 Pharma 0512 103 UK U-NiMilan MilovanovicNo ratings yet
- Building Social CapitalDocument17 pagesBuilding Social CapitalMuhammad RonyNo ratings yet
- Songs of KabirDocument342 pagesSongs of KabirSant MatNo ratings yet
- 10 Proven GPAT Preparation Tips To Top PDFDocument7 pages10 Proven GPAT Preparation Tips To Top PDFALINo ratings yet
- Commercial LawDocument61 pagesCommercial LawthebfilesNo ratings yet
- How To Access Proquest: Off-CampusDocument9 pagesHow To Access Proquest: Off-CampusZav D. NiroNo ratings yet
- Business Intelligence in RetailDocument21 pagesBusiness Intelligence in RetailGaurav Kumar100% (1)
- Anesthesia Considerations in Microlaryngoscopy or Direct LaryngosDocument6 pagesAnesthesia Considerations in Microlaryngoscopy or Direct LaryngosRubén Darío HerediaNo ratings yet
- 2 - The British Legal SystemDocument4 pages2 - The British Legal SystemSTAN GABRIELA ELENANo ratings yet
- Formulating A PICOT QuestionDocument4 pagesFormulating A PICOT QuestionKarl RobleNo ratings yet