Professional Documents
Culture Documents
Proximal Aortic Re Operations in Patients With
Uploaded by
Juan Carlos OzanCopyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Proximal Aortic Re Operations in Patients With
Uploaded by
Juan Carlos OzanCopyright:
Available Formats
Proximal aortic reoperations in patients with composite valve grafts
Scott A. LeMaire, Daniel J. DiBardino, Cüneyt Köksoy and Joseph S. Coselli
Ann Thorac Surg 2002;74:1777-1780
The online version of this article, along with updated information and services, is
located on the World Wide Web at:
http://ats.ctsnetjournals.org/cgi/content/full/74/5/S1777
The Annals of Thoracic Surgery is the official journal of The Society of Thoracic Surgeons and the
Southern Thoracic Surgical Association. Copyright © 2002 by The Society of Thoracic Surgeons.
Print ISSN: 0003-4975; eISSN: 1552-6259.
Downloaded from ats.ctsnetjournals.org by on June 6, 2010
Proximal Aortic Reoperations in Patients With
Composite Valve Grafts
Scott A. LeMaire, MD, Daniel J. DiBardino, MD, Cüneyt Köksoy, MD, and
Joseph S. Coselli, MD
The Michael E. DeBakey Department of Surgery, Division of Cardiothoracic Surgery, Baylor College of Medicine, and the
Methodist DeBakey Heart Center, Houston, Texas
Background. The purpose of this study was to examine ing 2 of the 7 patients who had infected CVGs (29%). All
our experience with proximal aortic reoperations in pa- 4 patients who had infected CVGs replaced with aortic
tients with composite valve grafts (CVGs) and assess root homografts survived. Complications included vocal
postoperative survival and morbidity. cord paralysis (n ⴝ 4, 12%), bleeding requiring reopera-
Methods. Since 1991, 33 patients with CVGs underwent tion (n ⴝ 3, 9%) and stroke (n ⴝ 2, 6%). Actuarial 3-year
reoperation for one or more of the following indications: survival was 74.4% ⴞ 7.9%.
aneurysms distal to the CVG (n ⴝ 20, 61%), false aneu- Conclusions. Reoperations in patients with CVGs re-
rysms (n ⴝ 13, 39%) and graft infection (n ⴝ 7, 21%). main challenging procedures with high associated mor-
Operations included false aneurysm repair (n ⴝ 13, 39%), bidity and mortality, especially in the setting of graft
graft replacement of distal ascending aortic or transverse infection. The results of homograft aortic root re-
aortic arch aneurysm (n ⴝ 20, 61%) and aortic root replacement for infected CVGs are encouraging.
re-replacement with a new CVG (n ⴝ 6, 18%) or ho-
mograft (n ⴝ 4, 12%). (Ann Thorac Surg 2002;74:S1777– 80)
Results. Operative mortality was 15% (n ⴝ 5), includ- © 2002 by The Society of Thoracic Surgeons
D ata from several centers have established that pri-
mary aortic root replacement can be performed
with low morbidity and mortality [1– 6]. In the wake of
Twenty patients (61%) presented with a recurrent an-
eurysm distal to the previously placed CVG; this was the
most common indication for reoperation. One of these
these excellent results an increasing number of these patients underwent an emergency operation for rupture.
patients are returning with a variety of indications for Two patients had acute dissection and 12 had chronic
reoperation [7–9]. Patients requiring reoperation on the dissection. In 19 patients the graft repair extended into
proximal aorta after previous composite valve graft the transverse aortic arch. Graft extension was performed
(CVG) placement represent a challenging subset [10]. as the sole operation in 13 patients and combined with
The purpose of this retrospective review was to examine other procedures in 7 patients; 5 of these underwent
our experience with proximal aortic reoperations in pa- concomitant pseudoaneurysm repair and 2 underwent
tients who have undergone previous CVG placement. placement of a new CVG for perivalvular pseudoaneu-
rysm or bioprosthetic aortic valve insufficiency.
Seven patients (21%) presented with infected CVGs,
Patients and Methods
proven by either preoperative blood culture (n ⫽ 6) or
Since 1991, 33 patients with previously placed CVGs intraoperative mediastinal fluid culture (n ⫽ 1). One
presented for reoperation. During the same period, the patient underwent only pseudoaneurysm repair and
senior author (J.S.C.) performed aortic root replacement omental coverage of the infected graft. Two patients
with CVGs in 124 patients, only 1 of whom returned for underwent CVG resection and replacement with a new
reoperation; the remaining 32 patients had their original CVG; a pedicled omental flap was placed around the new
CVG placed elsewhere. The average age at reoperation graft in 1. Since mid-1994 we have used homografts for all
was 46 ⫾ 14 years. Twenty-seven patients (82%) were patients with infected CVGs. Four patients underwent
men and 6 (18%) were women. Seventeen patients (52%) CVG resection and replacement with a homograft aortic
had Marfan’s syndrome. The average time interval be- root; omentum was placed around the homograft in 1
tween the initial operation and presentation was 81 ⫾ 71 patient. One of these patients had also undergone bev-
months (range, 3 to 252). In many cases there were eled polyester graft replacement of the proximal trans-
multiple simultaneous indications for reoperation. verse aortic arch during the initial operation; his reop-
eration included resection of all prosthetic material and
Presented at the Aortic Surgery Symposium VIII, May 2–3, 2002, New replacement with homograft aortic root and arch.
York, NY. Pseudoaneurysms were present in 13 patients (39%,
Address reprint requests to Dr LeMaire, 6560 Fannin St, Suite 1100, Table 1) and were usually associated with other pathol-
Houston, TX 77030; e-mail: slemaire@bcm.tmc.edu. ogy. Only 1 pseudoaneurysm (perivalvular) was related
© 2002 by The Society of Thoracic Surgeons 0003-4975/02/$22.00
Published by Elsevier Science Inc PII S0003-4975(02)04152-8
Downloaded from ats.ctsnetjournals.org by on June 6, 2010
S1778 AORTIC SURGERY SYMPOSIUM VIII LEMAIRE ET AL Ann Thorac Surg
PROXIMAL AORTIC REOPERATIONS 2002;74:S1777– 80
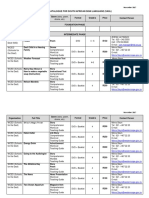
Table 1. Location and Type of Repair of 14 Pseudoaneurysms was placed to the left main coronary artery ostium.
in 13 Patients With Composite Valve Grafts Nine patients not requiring re-replacement of the aortic
Pseudoaneurysm No. of
root also underwent coronary artery procedures includ-
Location Type of Repair Patients ing pseudoaneurysm repair (Table 1) and coronary
revascularization.
Perivalvular Replacement with new CVG 4 Mean cardiopulmonary bypass and aortic clamp times
Primary repair 2* were 147 ⫾ 63 minutes and 108 ⫾ 49 minutes, respec-
Distal aortic Extended graft repair of aorta 3* tively. Hypothermic circulatory arrest was used in 25
anastomosis
patients (76%) to enable either aortic arch repair or safe
RCA attachment site Dacron interposition graft to 2
RCA (10 mm) sternal reentry. The mean circulatory arrest time was 49
Patch closure and SVG to 1 ⫾ 29 minutes. Seven patients received retrograde cere-
RCA bral perfusion during circulatory arrest. Operative trans-
LMCA attachment Dacron interposition graft to 2 fusion requirements were 10 ⫾ 6 U packed red blood
site LMCA (8 and 10 mm) cells, 31 ⫾ 22 U platelets, 16 ⫾ 17 U fresh frozen plasma,
and 27 ⫾ 18 U cryoprecipitate.
* One patient had simultaneous repair of perivalvular and distal aortic
anastomotic pseudoaneurysms.
CVG ⫽ composite valve graft; LMCA ⫽ left main coronary artery; Results
RCA ⫽ right coronary artery; SVG ⫽ saphenous vein graft.
There were no intraoperative deaths. There were 5 oper-
ative deaths (15%). All deaths occurred during the initial
hospitalization and 3 occurred within 30 days. The indi-
to graft infection. One patient with a perivalvular pseu- cations for operation in these 5 patients were CVG
doaneurysm and prosthetic aortic valve insufficiency infection (n ⫽ 2), recurrent aneurysm of the ascending
underwent placement of a new CVG. One patient had a aorta and aortic arch (2, including 1 rupture) and false
perivalvular pseudoaneurysm-to-right atrial fistula that aneurysm (n ⫽ 1). Both patients who had an infected
was closed at the time of pseudoaneurysm repair. CVG removed and replaced with a new CVG died.
Pseudoaneurysms were the sole indication for reopera- Causes of death included multiple organ failure (n ⫽ 2),
tion in only 4 patients (12%); 3 underwent repair alone stroke (n ⫽ 1), heart failure (n ⫽ 1), and pulmonary
and 1 underwent placement of a new CVG. embolism (n ⫽ 1).
A variety of coronary artery procedures were per- There were no postoperative complications in 42% of
formed depending on the presence of previously placed patients (n ⫽ 14). Two patients had strokes (6%), one of
coronary grafts, the presence of coronary occlusive dis- which was fatal. Both strokes occurred in patients who
ease, and the procedure chosen for aortic reconstruction. required hypothermic circulatory arrest. Nine patients
Overall, 58% of patients (n ⫽ 19) required at least one (27%) required more than 48 hours of ventilatory sup-
coronary artery intervention. Of 10 patients who under- port. Two patients required a tracheostomy; both were
went aortic root re-replacement (Table 2), 8 required successfully weaned from the ventilator and discharged
either a Cabrol interposition graft or saphenous vein home. Left vocal cord paralysis occurred in 4 patients
grafts to maintain coronary circulation. Cabrol grafts (12%). Three of these patients had undergone graft re-
were used when adequate coronary mobilization was placement of the transverse aortic arch during reopera-
not possible, ie, when there was extensive fibrosis or a tion and 1 had an infected CVG with a perivalvular
large coronary pseudoaneurysm. One patient required a pseudoaneurysm. Three patients (9%) required reopera-
Cabrol reattachment of the left coronary artery (hemi- tion for postoperative bleeding. Wound infection oc-
Cabrol) and a vein bypass graft to the right coronary curred in 3 patients (9%) and required a subsequent
artery. In 1 patient with a preexisting saphenous vein operation for wound debridement in 2 cases; only 1 of
bypass to the right coronary, the right coronary ostium these patients had initially presented with an infected
was oversewn and an interposition saphenous vein graft CVG. One patient developed atrioventricular block, but
did not require pacemaker placement.
Of 28 patients surviving to discharge, long-term fol-
Table 2. Coronary Artery Procedures in 10 Patients low-up was available for 24 patients (86%) and included
Requiring Redo Aortic Root Replacement data up to 9 years postoperatively (mean follow-up, 4.7 ⫾
2.5 years). There were 5 late deaths yielding a 79%
Method of Root No. of
Re-replacement Coronary Artery Procedure Patients survival rate among these 24 patients. Actuarial 3-year
survival was 74.4% ⫾ 7.9% (Fig 1). The patient who
Composite valve graft Open button anastomoses 1 underwent a pedicled omental wrap of the existing
Saphenous vein grafts 2* infected CVG was discharged on oral antibiotics and
Cabrol graft 4* remains active and healthy 8 years after discharge. Three
Homograft aortic root Open button anastomoses 1 patients who received homografts were discharged with
Saphenous vein grafts 3 intravenous antibiotics and tunneled central venous
* One patient underwent “hemi-Cabrol” reattachment of the left main lines. Three of the 4 patients with homografts remain
coronary artery and saphenous vein bypass to the right coronary artery. alive and well with no further complications an average
Downloaded from ats.ctsnetjournals.org by on June 6, 2010
Ann Thorac Surg AORTIC SURGERY SYMPOSIUM VIII LEMAIRE ET AL S1779
2002;74:S1777– 80 PROXIMAL AORTIC REOPERATIONS
Fig 1. Kaplan-Meier curve demonstrating
actuarial survival after proximal aortic re-
operation in 33 patients with composite
valve grafts. Values are reported with stan-
dard deviations.
of 6 years after discharge. The patient who presented nique used. Lifelong surveillance with echocardiography
with an infected CVG and beveled hemiarch graft died of and computed tomography scanning is required to as-
a myocardial infarction 5 months after discharge. Two of sess the integrity of the valve mechanism, the develop-
the 13 patients who underwent pseudoaneurysm repair ment of pseudoaneurysms, and dilatation of the distal
developed new pseudoaneurysms. One patient had un- aorta.
dergone repair of a left main coronary pseudoaneurysm As we have reported previously [14], CVG infection
and presented 4 years later with a new pseudoaneurysm remains a catastrophic complication. Prosthetic endocar-
involving the distal aortic anastomosis; this was repaired ditis is the most common complication after CVG place-
elsewhere by graft extension into the proximal hemiarch. ment and carries a mortality that exceeds 50% [2]. Al-
The other patient had undergone repair of a pseudoan- though simply wrapping the infected graft with a
eurysm at the distal aortic anastomosis by graft extension pedicled omental flap and administering long-term in-
into the proximal hemiarch and concomitant coronary travenous antibiotics was successful in 1 patient, replace-
artery bypass; 5 years later he developed a pseudoaneu- ment of the infected CVG with a homograft aortic root
rysm involving the vein grafts but was lost to follow-up provided encouraging early and midterm results. After
before treatment. homograft placement, we recommend a 6-week course of
intravenous antibiotics through a tunneled central ve-
nous catheter. Importantly, the risk of CVG infection
Comment
continues long after the initial operation. In our series 4
The most common indication for reoperation in this of the 7 patients (57%) with graft infection presented
series was aneurysm recurrence just distal to the previ- more than 3 years after CVG placement. We believe that
ously placed graft [11]. Although more judicious inspec- this justifies an aggressive approach to antibiotic prophy-
tion and aggressive resection of the proximal aorta at the laxis whenever patients with CVGs require invasive
original operation may reduce the incidence of recur- procedures that produce bacteremia such as bronchos-
rence, we recognize that limiting the initial repair (espe- copy, colonoscopy, and dental procedures; regardless of
cially under emergency circumstances) is often prudent. the length of time since CVG placement, we recommend
When feasible, brief periods of hypothermic circulatory periprocedural administration of intravenous broad-
arrest allow assessment of the aortic arch and may alter spectrum antibiotics.
the extent of reconstruction. Cooley and Livesay [12]
have referred to this as the open distal anastomosis
technique and have long recommended its use to more References
clearly identify the need for extended resection in pa- 1. Svensson LG, Crawford ES, Hess KR, Coselli JS, Safi HJ.
tients with aortic dissection. Composite valve graft replacement of the proximal aorta:
The open button technique of coronary artery reattach- comparison of techniques in 348 patients. Ann Thorac Surg
1992;54:427–39.
ment during CVG insertion has decreased the incidence
2. Gott VL, Gillinov AM, Pyeritz RE, et al. Aortic root replace-
of coronary artery pseudoaneurysm [3]. Similarly, using ment: risk factor analysis of a seventeen-year experience.
interrupted sutures rather than a continuous suture line J Thorac Cardiovasc Surg 1995;109:536 –45.
at the annular anastomosis may reduce the risk of peri- 3. Kouchoukos NT, Wareing TH, Murphy SF, Perillo JB. Six-
valvular pseudoaneurysm [13]. The variety of the 14 teen-year experience with aortic root replacement: results of
172 operations. Ann Surg 1991;214:308 –20.
pseudoaneurysms in this series, however, serves as a 4. Lewis CTP, Cooley DA, Murphy MC, Talledo O, Vega D.
reminder that patients with CVGs are at risk for the Surgical repair of aortic root aneurysms in 280 patients. Ann
development of pseudoaneurysms regardless of the tech- Thorac Surg 1992;53:38 –46.
Downloaded from ats.ctsnetjournals.org by on June 6, 2010
S1780 AORTIC SURGERY SYMPOSIUM VIII LEMAIRE ET AL Ann Thorac Surg
PROXIMAL AORTIC REOPERATIONS 2002;74:S1777– 80
5. Hilgenberg AD, Akins CW, Logan DL, et al. Composite 10. Raanani E, David TE, Dellgren G, Armstrong S, Ivanov J,
aortic root replacement with direct coronary implantation. Feindel CM. Redo aortic root replacment: experience with 31
Ann Thorac Surg 1996;62:1090 –5. patients. Ann Thorac Surg 2001;71:1460 –3.
6. Dossche KM, Schepens MA, Morshuis WJ, et al. A 23-year 11. Crawford ES, Crawford JL, Safi HJ, Coselli JS. Redo opera-
experience with composite valve graft replacement of the tions for recurrent aneurysmal disease of the ascending
aorta and transverse aortic arch. Ann Thorac Surg 1985;40:
aortic root. Ann Thorac Surg 1999;67:1070 –7.
439 –55.
7. Dougenis D, Daily BB, Kouchoukos NT. Reoperation on the
12. Cooley DA, Livesay JJ. Technique of “open” distal anasto-
aortic root and ascending aorta. Ann Thorac Surg 1997;64: mosis for ascending and transverse arch resection. Cardio-
986 –92. vasc Dis (Bull Tex Heart Inst) 1981;8:421–6.
8. Hahn C, Tam SKC, Vlahakis GJ, et al. Repeat aortic root 13. Grey DP, Ott DA, Cooley DA. Surgical treatment of aneu-
replacement. Ann Thorac Surg 1998;66:88 –98. rysms of the ascending aorta with aortic insufficiency. J Tho-
9. Luciani GB, Casali G, Faggian G, Mazzucco A. Predicting rac Cardiovasc Surg 1983;86:864 –77.
outcome after reoperative procedures on the aortic root and 14. Coselli JS, Köksoy C, LeMaire SA. Management of thoracic
ascending aorta. Eur J Cardio-thorac Surg 2000;17:602–7. aortic graft infections. Ann Thorac Surg 1999;67:1990–3.
Downloaded from ats.ctsnetjournals.org by on June 6, 2010
Proximal aortic reoperations in patients with composite valve grafts
Scott A. LeMaire, Daniel J. DiBardino, Cüneyt Köksoy and Joseph S. Coselli
Ann Thorac Surg 2002;74:1777-1780
Updated Information including high-resolution figures, can be found at:
& Services http://ats.ctsnetjournals.org/cgi/content/full/74/5/S1777
References This article cites 14 articles, 12 of which you can access for free at:
http://ats.ctsnetjournals.org/cgi/content/full/74/5/S1777#BIBL
Citations This article has been cited by 8 HighWire-hosted articles:
http://ats.ctsnetjournals.org/cgi/content/full/74/5/S1777#otherarticl
es
Subspecialty Collections This article, along with others on similar topics, appears in the
following collection(s):
Great vessels
http://ats.ctsnetjournals.org/cgi/collection/great_vessels
Permissions & Licensing Requests about reproducing this article in parts (figures, tables) or
in its entirety should be submitted to:
http://www.us.elsevierhealth.com/Licensing/permissions.jsp or
email: healthpermissions@elsevier.com.
Reprints For information about ordering reprints, please email:
reprints@elsevier.com
Downloaded from ats.ctsnetjournals.org by on June 6, 2010
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Developmental Screening Tools: Michelle M. Macias, MD D-PIP Training Workshop June 16, 2006Document39 pagesDevelopmental Screening Tools: Michelle M. Macias, MD D-PIP Training Workshop June 16, 2006psy22No ratings yet
- Can Celebrities Be Good Role Models For UsDocument2 pagesCan Celebrities Be Good Role Models For UsSamira MusayevaNo ratings yet
- Hypertensive Disorder in PregnancyDocument7 pagesHypertensive Disorder in PregnancyBiscuits and milkNo ratings yet
- GHGK SDocument48 pagesGHGK SAnonymous Syr2mlNo ratings yet
- NHP Original 1985 PDFDocument4 pagesNHP Original 1985 PDFAndrei IordanNo ratings yet
- Time Management StrategiesDocument3 pagesTime Management Strategiesأحمد عبدالمحسنNo ratings yet
- CCMA Consent Form - BlankDocument2 pagesCCMA Consent Form - BlankChristina Blignault50% (2)
- New IB Diploma Psychology Topic PostersDocument8 pagesNew IB Diploma Psychology Topic PostersRajat Palaswadikar100% (1)
- The Trade Effluents (Prescribed Processes and Substances) Regulations 1992Document2 pagesThe Trade Effluents (Prescribed Processes and Substances) Regulations 1992Lúcio FernandesNo ratings yet
- INGREDIENTSDocument17 pagesINGREDIENTSPaulo BacayNo ratings yet
- Garrison, NancyDocument139 pagesGarrison, NancyBrunoNo ratings yet
- S9 Q4 M1 Transport and Excretion and Respiration and Energy Exchange QuizDocument3 pagesS9 Q4 M1 Transport and Excretion and Respiration and Energy Exchange QuizJermae DizonNo ratings yet
- Mil PRF 680Document14 pagesMil PRF 680Wisdom SamuelNo ratings yet
- Nqs NQSDocument270 pagesNqs NQSManpreet KaurNo ratings yet
- Bathing Your Baby: When Should Newborns Get Their First Bath?Document5 pagesBathing Your Baby: When Should Newborns Get Their First Bath?Glads D. Ferrer-JimlanoNo ratings yet
- MSDS Bleach PDFDocument5 pagesMSDS Bleach PDFAlfonso Alejandro Loayza RodriguezNo ratings yet
- التقييم التغذويDocument4 pagesالتقييم التغذويMai GaberNo ratings yet
- P9 Lecture Child Abuse PDFDocument53 pagesP9 Lecture Child Abuse PDFVira PebrianaNo ratings yet
- Radiation PhysicsDocument307 pagesRadiation PhysicsHarley Alejo MNo ratings yet
- New Patient Medical Form: in One SentenceDocument1 pageNew Patient Medical Form: in One SentenceAzra BarliNo ratings yet
- About MADocument14 pagesAbout MADd DdNo ratings yet
- DBE South African Sign Language National Catalogue 2018Document7 pagesDBE South African Sign Language National Catalogue 2018Anonymous ozd4aLKhNo ratings yet
- Rimso 50Document1 pageRimso 50monloviNo ratings yet
- The ConsulDocument4 pagesThe ConsulPrince Adesina HaastrupNo ratings yet
- MNT CancerDocument62 pagesMNT CancerSaufi ZakariaNo ratings yet
- Nove Farmakološke Strategije U Lečenju Nesitnoćelijskog Karcinoma PlućaDocument8 pagesNove Farmakološke Strategije U Lečenju Nesitnoćelijskog Karcinoma PlućaMomcilo Moca DjurovicNo ratings yet
- Grief & Loss - pptx-1Document66 pagesGrief & Loss - pptx-1pinkyNo ratings yet
- Kangaroo Mother Care Rooming in UpdatedDocument44 pagesKangaroo Mother Care Rooming in UpdatedStar DustNo ratings yet
- Chapter 6 Test Skeletal SystemDocument49 pagesChapter 6 Test Skeletal SystemAlexandra CampeanuNo ratings yet
- HR Director VPHR CHRO Employee Relations in San Diego CA Resume Milton GreenDocument2 pagesHR Director VPHR CHRO Employee Relations in San Diego CA Resume Milton GreenMiltonGreenNo ratings yet