Professional Documents
Culture Documents
Readings
Uploaded by
niestephOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Readings
Uploaded by
niestephCopyright:
Available Formats
Chlamydial Infection
Is a common sexual transmitted disease that occurs in women and men, particularly in adolescents and young adults. Women are asymptomatic or present with cervicitis. Men are commonly asymptomatic but may present with urethritis. Untreated chlamydial infections can lead to epididymitis, salphingitis, pelvic inflammatory disease and eventually sterility. Mode of Transmission 1. The disease is transmitted through vaginal or rectal intercourse. 2. The disease is also transmitted through oral-genital contact with an infected person. 3. Conjunctivitis, otitis media, and pneumonia may develop to children born to mothers with chlamydial infection passed through birth canal. Clinical Manifestations 1. May be asymptomatic or have vaginal discharge may be clear mucoid to creamy discharge. 2. May have dysuria and mild pelvic disorder. 3. Cervix may be covered by thick mucopurulent discharge and be tender, erythematous, edematous, and friable. Diagnostic Evaluation 1. DNA detection test on cervical smear or urine sample (by DNA amplification method). 2. Chlamydia culture from cervical exudate. 3. Screening urinalysis in males for leukocytes; if positive result, confirmed by DNA detection test. 4. ELISA 5. Direct fluorescent anti-body test. 6. The Centers for Disease Control and Prevention (CDC) recommends annual screening for all sexually active adolescents women as well as young women, ages 20 to 24, and older women at high risk (multiple sex partners or new partner). Complications 1. Pelvic Inflammatory Disease. 2. Ectopic pregnancy or infertility secondary to untreated or recurrent pelvic inflammatory diseases. 3. Transmission to neonate born through infected birth canal. Treatment 1. Doxycycline oral for several days. 2. Azithromycin in single dose. Nursing Interventions 1. Advice abstinence from sexual intercourse until treatment has been completed. No follow-up culture is necessary to ensure cure; however, re-screening is recommended 3 to 4 months after treatment to detect reinfection, particularly in adolescents and young women. 2. Ensure that the partner is treated at the same time; recent partners should receive treatment despite lack of symptoms and negative Chlamydia result. 3. Report case to local public health department (Chlamydia is a reportable infectious disease). 4. Ensure that the patient begins treatment and will have access to prescription follow up. 5. Explain mode of transmission, complications, and the risk for other STDs. 6. Teach about all STDs and their symptoms. 7. Explain the treatment regimen to patient and advise her of adverse effects. 8. Encourage abstinence, monogamy, or safer sex methods, such as female or male condom. 9. Stress the importance of follow-up examination and testing to eradication of infection. Recurrence rates are highest in young patients.
Erythema Infectiosum (Fifth Disease
Definition Erythema infectiosum or the Fifth Disease is an infectious disorder that affects children aging 2-12 years of age. The term fifth disease was based on the classification system for childhood rashes decades ago. Generally, the five frequent childhood rashes are the following:
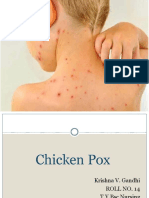
1. Measles (rubeola) 2. Chickenpox (vaicella) 3. German measles (rubella) 4. Roseola 5. Erythema Infectiosum (Parvovirus B19) Because erythema infectiosum is the fifth disease that causes rashes in children, thus, the term has been used by most people. The prevalence of the illness is more commonly seen during spring and winter period and studies show that females are often affected than males. Parvovirus B19, sometimes called as erythrovirus B19 is a part of the genus Parvoviridae. It was accidentally detected in 1975 by an Australian virologist Yvonne Cossart. Fifth Disease Related Data Causative Agent: Parvovirus B19 Incubation period: 6-14 days Mode of transmission: droplet (respiratory secretions transmitted by cough and sneeze) Period of communicability: uncertain Signs and symptoms Fifth disease produces symptoms that are benign and go away on their own. The following are most likely observed: Fever, headache, coryza, abdominal pain, sore throat and malaise on the first week. Rashes appear a week after, erupting in three sequential phases: Face Bright red rash coalesces at the cheeks forms a slapped face appearance.(Hallmarksign) Extensor surface of extremities(outer arm) Rashes are expected to scatter on the extremities (extensor surface) a day after the facial rash develops. (Extensor surfaces refers to the part of the skin that do not touch when the joints are bend) Flexor surfaces of extremities and trunk Rash invasion in these areas are observed a day after it appeared on the extensor surfaces (inner arm and leg). The eruptions will last for a week or more. Rashes start to fade from the center outward (a lace-like appearance will be observe due to this manner of disappearance) Management Home care: 1. Adequate fluid intake 2. Frequent hand washing. 3. Acetaminophen (Tylenol) is given to decrease body temperature. Aspirin (acetylsalicylic acid) is not recommended as it is related to the occurrence of Reye syndrome. Droplet precautions should be implemented if the child is hospitalized. (wearing mask,gloves, eyewear, spacing client in single room) Avoid contact to pregnant women. Parvovirus B19 is teratogenic. It causes severe anemia with congestive heart failure to the fetus. A child may resume school as soon as the rash appears. (the disease is no longer contagious at this time)
You might also like
- CDNDocument2 pagesCDNJohn Paulo MoralesNo ratings yet
- Chickenpox & ChlamydialDocument5 pagesChickenpox & ChlamydialEliezah RodriguezNo ratings yet
- Case Study in Micro-1Document50 pagesCase Study in Micro-1Angie Cabanting BañezNo ratings yet
- Viral InfectionsDocument34 pagesViral InfectionsAlaa MadmoujNo ratings yet
- 3.torch InfectionsDocument15 pages3.torch InfectionsKuleshwar SahuNo ratings yet
- Sexually Transmitted Infections and PregnancyDocument19 pagesSexually Transmitted Infections and PregnancyBeyins TiuNo ratings yet
- Communicable Diseases Affecting The Reproductive SystemDocument49 pagesCommunicable Diseases Affecting The Reproductive SystemJR Rolf NeuqeletNo ratings yet
- ScabiesDocument16 pagesScabiescarla_sarmiento4847No ratings yet
- Childhood Sicknesses1111Document17 pagesChildhood Sicknesses1111abdulrahmanbelewa96No ratings yet
- Clinical ManifestationDocument6 pagesClinical ManifestationKrystal Jane SalinasNo ratings yet
- Name: Carlo M. Yao Bachelor of Science in NursingDocument33 pagesName: Carlo M. Yao Bachelor of Science in Nursingcarlo24_briggsNo ratings yet
- Measles (Report) DocsDocument4 pagesMeasles (Report) DocsCrystal AbarrientosNo ratings yet
- Dengue 1Document6 pagesDengue 1Johannah Ruth BacolodNo ratings yet
- Viral Diseases - 06Document51 pagesViral Diseases - 06HIMANSHU SINGHNo ratings yet
- SARS-2nd ProffDocument27 pagesSARS-2nd ProffMuhammad aslamNo ratings yet
- Psoriasis: Posted: 02 Aug 2010 11:18 PM PDTDocument5 pagesPsoriasis: Posted: 02 Aug 2010 11:18 PM PDTScamb TrekNo ratings yet
- ChickenpoxDocument4 pagesChickenpoxJen Vizcarra CaminoNo ratings yet
- Measles (Rubeola) Rubeola Red Spot: Dr. Eman Khammas Alsadi Community Medicine LecturerDocument34 pagesMeasles (Rubeola) Rubeola Red Spot: Dr. Eman Khammas Alsadi Community Medicine Lecturereman khammasNo ratings yet
- Chicken-Pox Concept MapDocument4 pagesChicken-Pox Concept MapElle0% (1)
- Mayores. Chicken Pox - Concept MapDocument3 pagesMayores. Chicken Pox - Concept MapAlvic Dy KowNo ratings yet
- Synonyms Causative Agents Incubatiob Period Mode of Transmission Signs and Symptoms Period of Communicability Diagnostic Test Medical Management Nursing Management ComplicationsDocument13 pagesSynonyms Causative Agents Incubatiob Period Mode of Transmission Signs and Symptoms Period of Communicability Diagnostic Test Medical Management Nursing Management ComplicationsYnah DominiqueNo ratings yet
- LECTURE 02A German MeaslesDocument21 pagesLECTURE 02A German Measlesraxma4682No ratings yet
- Chicken PoxDocument4 pagesChicken PoxFloyd SevillaNo ratings yet
- School PrerequistesDocument65 pagesSchool Prerequistesmanaribrahim309No ratings yet
- Https://ar - scribd.com/document/391648283/OET Future Land Full Book Final Edition July 2018Document52 pagesHttps://ar - scribd.com/document/391648283/OET Future Land Full Book Final Edition July 2018Qutaiba ShdaifatNo ratings yet
- 2 - SyphilisDocument24 pages2 - SyphilisCaila LimNo ratings yet
- Signs and SymptomsDocument6 pagesSigns and SymptomsKajim SharibiNo ratings yet
- PAEDS 4 - 18.10.19 Viral InfectionDocument15 pagesPAEDS 4 - 18.10.19 Viral Infectionlotp12No ratings yet
- Chickenpox ActividadDocument6 pagesChickenpox ActividadAngie MinayaNo ratings yet
- Sexually Transmitted DiseasesDocument17 pagesSexually Transmitted DiseasesChrystele Ann Ramilo100% (1)
- CHN - Communicable DiseaseDocument117 pagesCHN - Communicable DiseaseGetom NgukirNo ratings yet
- Herpes 3, VSVDocument21 pagesHerpes 3, VSVCharles SainzNo ratings yet
- Kutis PorcelanaDocument34 pagesKutis Porcelanaapi-3743483No ratings yet
- Child Health Nursing: MumpsDocument25 pagesChild Health Nursing: MumpsmanibharathiNo ratings yet
- UntitledDocument6 pagesUntitledGenelly Anne Argañoza RamosNo ratings yet
- Chicken PoxDocument26 pagesChicken PoxKrishna GandhiNo ratings yet
- Monkeypox RA and MX 27 Mei 2022Document45 pagesMonkeypox RA and MX 27 Mei 2022alfonso de albuquerqueNo ratings yet
- Sexually Transmitted DiseasesDocument19 pagesSexually Transmitted DiseasesAhmed HajiNo ratings yet
- ChickenpoxDocument24 pagesChickenpoxPRATIK SHRESTHANo ratings yet
- Vulvovaginitis in Childhood: Cristina Vezzani, Gilda Di Paolo, Terryann Spagnuolo, and Gabriele TridentiDocument17 pagesVulvovaginitis in Childhood: Cristina Vezzani, Gilda Di Paolo, Terryann Spagnuolo, and Gabriele TridentiIvonne CabreraNo ratings yet
- Gusti Izza - English Medical ArticleDocument6 pagesGusti Izza - English Medical Articlenuna_idaNo ratings yet
- 1-Measles (Rubeola) PDFDocument37 pages1-Measles (Rubeola) PDFمصطفى رسول هاديNo ratings yet
- Medical Terms Kind of IlnessDocument11 pagesMedical Terms Kind of IlnessFani KimerliNo ratings yet
- Chickenpox: SymptomsDocument10 pagesChickenpox: SymptomsAnand SwamiNo ratings yet
- VaricellachickenpoxDocument6 pagesVaricellachickenpoxDedi SofyanNo ratings yet
- Genitourinary SystemDocument7 pagesGenitourinary SystemMary Angel VelascoNo ratings yet
- Lect 4 Viral InfectionDocument44 pagesLect 4 Viral InfectionAMIT GUPTANo ratings yet
- Meehleib, Rachelle Ayn S. Pepino, Stephanie Kate ADocument16 pagesMeehleib, Rachelle Ayn S. Pepino, Stephanie Kate ARachelle AynNo ratings yet
- Helminths (Tapeworm, Pinworm) - NavarroDocument26 pagesHelminths (Tapeworm, Pinworm) - NavarroThaddeus Dalagan NavarroNo ratings yet
- Acute Infections During PregnancyDocument63 pagesAcute Infections During PregnancyHussein AliNo ratings yet
- Rle BSN 2 (Lesson 3) (2021-2022)Document26 pagesRle BSN 2 (Lesson 3) (2021-2022)Flonamae AbiarNo ratings yet
- WCLF E1 J 66 F YPUTf 0149Document165 pagesWCLF E1 J 66 F YPUTf 0149ClintonNo ratings yet
- MEASLES and MALARIADocument19 pagesMEASLES and MALARIADoreen Claire M. WallangNo ratings yet
- Common DiseasesDocument7 pagesCommon DiseasesAlter BadonNo ratings yet
- GonorrheaDocument22 pagesGonorrheaSharah Londonio100% (1)
- Sexually Transmitted Diseases: Jasmin P. EgargueDocument33 pagesSexually Transmitted Diseases: Jasmin P. EgargueLiza AingelicaNo ratings yet
- Monkey Pox FinalDocument35 pagesMonkey Pox FinalHiren patelNo ratings yet
- ChickenpoxDocument7 pagesChickenpoxJennevy Buque100% (1)
- CHN DiseasesDocument216 pagesCHN DiseasesCzarina May TumandanNo ratings yet
- JN KDocument24 pagesJN Kcatch.amit19No ratings yet
- Pascual V PascualDocument2 pagesPascual V PascualAices SalvadorNo ratings yet
- Population Disadvantage GDI 2005Document71 pagesPopulation Disadvantage GDI 2005Incoherency100% (12)
- Open Fire Assembly GuidesDocument2 pagesOpen Fire Assembly GuidesRandall CaseNo ratings yet
- An Introduction To Historical "Lavender" Linguistics byDocument2 pagesAn Introduction To Historical "Lavender" Linguistics byapi-25885198No ratings yet
- 47 - Ong Vs CA, GR 95386, May 29, 1997Document6 pages47 - Ong Vs CA, GR 95386, May 29, 1997美咲剛No ratings yet
- Passive SentencesDocument6 pagesPassive SentencesFadiaNo ratings yet
- M.A. in Social Work Colleges in North IndiaDocument2 pagesM.A. in Social Work Colleges in North Indiasandeepkumarmsw8442No ratings yet
- 0 042010 Notes - Brandon AdamsDocument17 pages0 042010 Notes - Brandon AdamsCK in DC100% (5)
- EM 8-Position PaperDocument2 pagesEM 8-Position PaperSTEVEN MENDEZNo ratings yet
- Motion For Stay Pending Appeal and Memo in SupportDocument15 pagesMotion For Stay Pending Appeal and Memo in SupportMartin AustermuhleNo ratings yet
- Space Opera Adv - 1Document24 pagesSpace Opera Adv - 1Jacopo Jbb ColabattistaNo ratings yet
- An Example of Narrative TextDocument2 pagesAn Example of Narrative TextihdaNo ratings yet
- Enquiry ProceedingsDocument5 pagesEnquiry ProceedingsNiraj Kumar MishraNo ratings yet
- Jail (Prison Constable Merit) - 1Document419 pagesJail (Prison Constable Merit) - 1Mujeeb Ur RehmanNo ratings yet
- Article 7 Sec 4 Legarda V de CastroDocument2 pagesArticle 7 Sec 4 Legarda V de CastroJc Araojo100% (1)
- Drug Law Enforcement: Narcotics Control BureauDocument160 pagesDrug Law Enforcement: Narcotics Control BureausameerNo ratings yet
- Framework For Conflict AnalysisDocument18 pagesFramework For Conflict Analysiseliasox123No ratings yet
- EXAMINING THE ROLE OF THE 50/50 GROUP Thesis From FredlineDocument209 pagesEXAMINING THE ROLE OF THE 50/50 GROUP Thesis From FredlineBrima GeorgeNo ratings yet
- 4 G.R. No. 171673 Banahaw vs. PacanaDocument8 pages4 G.R. No. 171673 Banahaw vs. Pacanaaags_06No ratings yet
- Digital Devils - Player AgreementDocument3 pagesDigital Devils - Player AgreementRizaNo ratings yet
- Nuestra Senora de La Inmaculada Concepcion y Del Triunfo de La Cruz de MigpangiDocument2 pagesNuestra Senora de La Inmaculada Concepcion y Del Triunfo de La Cruz de MigpangilhemnavalNo ratings yet
- Prime Marine Service vs. NLRC DDocument3 pagesPrime Marine Service vs. NLRC DCzar Ian AgbayaniNo ratings yet
- SIRD MizoramDocument2 pagesSIRD MizoramRaju MacharlaNo ratings yet
- Recognition of Foreign Divorce in The PhilippinesDocument9 pagesRecognition of Foreign Divorce in The PhilippinesRaffy Pangilinan0% (1)
- Report of The African Court On Human and Peoples Rights in The Protection of Human Rights in Africa FinalDocument10 pagesReport of The African Court On Human and Peoples Rights in The Protection of Human Rights in Africa FinalRANDAN SADIQNo ratings yet
- International Express Travel v. CADocument3 pagesInternational Express Travel v. CACherry ChaoNo ratings yet
- Holocaust Era Assets Conference Proceedings 2009Document653 pagesHolocaust Era Assets Conference Proceedings 2009bekowiczNo ratings yet
- Gogol, Eugene - Toward A Dialectic of Philosophy and OrganizationDocument409 pagesGogol, Eugene - Toward A Dialectic of Philosophy and Organizationzvonomir100% (1)
- Airport Activities VocabularyDocument3 pagesAirport Activities VocabularyTY FlamencoSNo ratings yet