Professional Documents
Culture Documents
Severe of Stenosis Unfavor: Carotid A Stenosis Carotid Angioplasty + Stenting
Uploaded by
URo KkuOriginal Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Severe of Stenosis Unfavor: Carotid A Stenosis Carotid Angioplasty + Stenting
Uploaded by
URo KkuCopyright:
Available Formats
Arterial disease short note by S.
Wichien (SNG KKU)
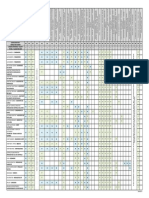
Carotid A stenosis Severe of stenosis Mild<50% Mod 50-69% Severe 70-99% Clinical 1.Ocular symptom -Amaurosis fugux :transient monocular blindness :hollenhorst plaque in retina vv :choles emboli 2.Sensory/motor deficit 3.Hi cortical fxn--speech Tx 1.symp carotid stenosis (2nd stroke prevention) Med = ASA, clopidogrel Sx=carotid endarterectomy 1.severe dz--sig than drug alone 2.mod dz--favor than drug alone 3.mild stenosis--no benefit Optimal time -early (<2wk of stroke) : hi mortality 2.asymptomatic carotid stenosis (1stroke prevention) Severe ds (>80%) -sx or endovascular revas :benefit Carotid endarterctomy vs Angioplasty+stent hi-risk pt 1.anatomy factor -hi bifurcate >C2 -low common carotid ,below clavicle -contralat carotid occlusion -restenosis prior endarterctomy -previous neck radiation -contralat laryngeal n palsy -tracheostomy 2.physiology factor ->80yr -LV<30% -NYHA 3-4 -recent MI -severe COPD -ESRD on HD -signi CHF Carotid angioplasty + stenting Unfavor -extensive calcify -long segment >2cm -severe tortuosity -carotid a occlusion Preop--clopidogrel 3d Technic -retrograde transfemoral approach 1.distal embolic protection device-EPD 2.+/-pre dilatation balloon 3.stent 4.post dilatation balloon 5.retrieve EPD C/p -acute carotid stent thrombosis--rare -carotid a dissection Carotid endarterctomy Intraop cerebral mornitoring -awake--rxn command -GA--intraop electroencephalogram or Transcranial power doppler Poor collateral flow -intra arterial carotid shunting Technique -hyperextend+turn to contralat side -incision--oblique ant of SCM -dissect bifurcate--facial v,CN12 :bradycardia---stimulate carotid body :inject 1%xylocain to CB :reverse by atropine iv -heparin 1mg/kg before clamp -vascular clamp 1-ICA 2-ECA,CCA -longitudinal arteriotomy in distal CCA -may temporary shunt--CCA-ICA -patch closed :saphenous vein, PTFE -declamp--ECA --> ICA Eversion technic -transect ICA--remove plaque -no need patch closure -clear visual distal zone C/p Acute iipsilat stroke -emboli(common) -prolong cerebral ischemia -thrombosis Ix--carotid duplex Tx--re explor in acute occlusion Bleeding/hematoma Aw compromise CN palsy--traction inj
Arterial disease short note by S.Wichien (SNG KKU)
Carotid artery stenosis (non atherosclerosis) 1.carotid coil,kink -excess elongate of ICA -women > man -cerebral hypoperfusion :sudden head rotation :flex,extension 2.fibromuscular dysplasia -FMD -medium size artery -focal stenosis/multiple lesion with intervening aneurysmal outpouching 3.carotid a dissection Risk--CNT dz -ehler danlos, marfan, alpha1 antitrypsin def Traumatic dissection -hyperextend neck in blunt -penetrating inj Iatrogenic -catheter -balloon angioplasty Clinical Typical -uni neck pain -headache -ilsilat horner synd -cerebral ischemia Tx 1 Tx of symp pt -med--heparin/warfarin, ASA Intervention --endovascular -recurrent TIA,stroke -fail med 4.carotid a aneurysm -pulsatile neck mass -emboli--neuro symptom -rupture/thrombosis--rare Mycotic aneurysm -syphilis--in the past -s.aures--peritonsillar abscess Tx--endovascular 5.carotid body tumor -3rd brachial arch,neural creast -CB--bifurcate of CCA in adventitia -n=glossopharyngeal -a=ext carotid a -5% = malignancy Shamblin class 1-<5cm,free vv involved 2-intima involve,not encase 3-intramural,encase Tx--sx resection 6.carotid trauma cute carotid a thrombosis -asymptom--anticoagulant -cerebral ischemia--revascularized Carotid a dissection -thromboembolism event -distal ICA--petrous part ICA Pseudoaneurysm -sx -selective coil embolization or covered stent
Arterial disease short note by S.Wichien (SNG KKU)
Aneurysm -dilate of a. greater than 1.5x its normal diameter Classification Shape 1.fusiform -spindle -diffuse dilate 2.saccular Wall constitutent 1.true aneurysm 2.pseudoaneurysm/false aneurysm Etiology 1.dissecting aneurysm 2.mycotic 3.traumatic-catheter,trauma AAA -sx mortal<5% -if >5.5 cm :risk of rupture > mortality Etiology/pathology -progressive loss of elastin -increase metalloprotease activity -sex -link and autosomal recessive -smoking Clinical manifestation -major=asymptomatic -incidental finding:x-ray,u/s,CT -new onset low back pain/abdo pain
-pain from stretching retroperitoneal
-aortocaval/aortoduodenal fistula -lower ext embolization -ureteric obstruction PE -pulsatile mass -femoral/distal pulse -carotid bruit Testing 1.ultrasound -screening modality of choice -follow up 2.CT -gold std for pre-op -thin cut(3mm) c contrast -CTA 3.angiography -more accurate -access renal a,horseshoe kidney, mesenteric ischemia,lower ext claudi 4.MR Preop-evaluation 1.symptom 2.hx of pelvic sx/ XR :in retroperitoneal exposure 3.claudication--iliac occlusive dz 4.LE bypass/femoral procedure 5.CKD, contrast allergy
Mycotic aneurysm 1.stap 2.samonella 3.mycobacterium,pasteurella,candida cause -result of infected emboli :aortic,mitral valve -direct extension of area of infection -higher rupture Tx -PTFE resist infection than dacron -may use ATB impregnated dacron :rifampicin -ATB--3-6mo 1.In-situ reconstruction 2.Extra-anatomical approach -Axillo-bifemoral bypass -stap.aureus,pseudo
Arterial disease short note by S.Wichien (SNG KKU)
AAA EVAR Aortic endografting -smaller procedure -not require ICU -2d hospitalization -1-2 wk to normal -10% require additional intervention -in hi risk,have anatomy suitable, benefit in avoiding laparotomy Benefit -minimal invasive -severe pulmo ds -GI c/p C/p -endoleak--ruptured <0.8% -stent graft iliac limb dysfxn :graft kink :progress of atherosclerotic Tx-thrombolysis, graft thombectomy -graft separation/dislocation -rupture--1-1.5%/yr Tx-open conversion vs endovas.stent Anatomy eligibility Neck length >15mm Neck diameter >18 <32mm Neck angle <60 Neck mural calci<50% circumf Neck lumi throm <50% circumf CIA dia 8-20mm CIA length >20mm EIA dia >7mm Aortic endografting -bilat transverse oblique incision (just below inguinal L) :some--complete percu access -transfemoral access :guidewire -iv heparin 80 u/kg -delivery catheter $ device--L1-2 :1device--rt femoral a :contralat iliac limb--lt femoral a -aortogram :locate renal a :1device--deploy below renal a -contralat iliac limb--deploy -complete angiogram Surveillance--CT scan -1st mo -q 6mo*2yr -q 1 yr Complication -illiac a. inj :rupture,dissection,limb occlusion -renal failure from dye toxicity -endoleak Endoleak classification-20-30% T1-attachment site leak <5% -poor pt selection/ inadequate repair -80%--spon seal in 6 mo T2-lumbar/IMA endoleak 20-30% -most common -50%--spon seal T3-junctional leak -if intraop/early post op :inadequate overlap 2 stent -if late period :fabric tear/ jxn separation Tx--prompt repair T4-transgraft -endograft fabric/ porosity leak Endotension--5% -aneurysm grow up but no leak 2intervention--10-15%/yr -migration -endoleak T2--embolization -open sx conversion
Arterial disease short note by S.Wichien (SNG KKU)
AAA sx Traditional open repair -require 1-day ICU -5-7d hospitalization -2mo to normal -long term complication 5-10% Benefit 1.no recur/delay ruptured 2.assess colon Risk 1.cardiac c/p--MI,arrhythmia -most common morbid -2-6% 2.renal failure -periop hypoT -suprarenal clamp 3.atheromatous embolization No femoral p. -poor anastomosis -graft kinking -clamp inj to iliac a. Present femoral p. -distal emboli 4.ischemic colitis -can check by insert catheter into IMA stump and measure back p., if >40mmhg indicate adequate collateral flow and safe ligate of IMA 5.prosthesis graft infection -1-4% 6.spinal cord ischemia -sacrifice lumbar a.to SC Pre-op -risk f.for open aneurysm repair include MI in 6mo co revascularized, CHF,angina,FEV1<1L,cr>2 Sx 1.open approach -midline abdo incision or lt retroperitoneal approach -retract T.colon superiorly -retract small bowel to rt -expose mesentery -incise peritoneum over aorta from iliac bifurcation,up to lt renal v. -IMV can be safely divided and ligated -distal extent of dissection is determined by extent of aneurysmal involvement of iliac a. -heparin 100 u/kg,3 min later illiac a. are clamped,followed by aorta -open aneurysm longitudinally -back bleeding lumbar vv are oversewn c silk 2-0 -graft is sewn end to end c prolene3-0 -graft flushed c heparinized saline -check femoral p. -check sigmoid colon,if not,would exploration of IMA,reimplant to graft -anticoag is reversed by protamine s. -re-approximate aneurysm sac c polyglactin 2-0 -closed retroperito c polyglactin 2-0 Post-op -f/u 1,6 mo then yearly -CT 3yr to look pseudoaneurysm Complication of prosthetic repair -anastomotic aneurysm :distal anastomosis is common -graft infection -graft thrombosis -aortoenteric fistula :<1%,graft erode to duodenum :massive GI bleeding
Arterial disease short note by S.Wichien (SNG KKU)
PAAA -para-anastomotic aortic aneurysm -0.2-15% -mean interval 8-10 yr True PAAA -inadequate resection -continue degen of vv False PAAA -defect in a.,suture,graft -suture material,type of anastomosis mismatch graft,infect -excessive tension on graft Clinical -asymp--major detect late -abdp.pain,back pain,claudication -pulsatile masd -25%--false aneurysm of femoral a. Surveillance -CT/1yr--4yr after repair AAA,rupture -sudden onset -severe abdo/back pain -mortality 70-77% 1/2-not reach hospital 1/2-sx mortal 50% Rx
-emergent repair -avoid aggressive resuscitation and
infuse fluid or blood only to keep pt stable -HTN accelerate additional bleeding -SBP 70 mmhg c cerebrated pt is tolerate while preparation are made to go to OR OR -prep and draped skin c awake pt -when GA=long midline incision -infrarenal or supraceliac control Supraceliac control -incise lesser omentum -exposure aorta at the diaphragm -blunt dissection c finger -finger insert on neck of aorta and post spine -avoid lt renal v. -when neck isolate,coarctation clamp is placed at supraceliac control -open aorta -control illiac vv -declamping aware intractable hyopT -check colon,feet Complication -venous inj -ureter inj -duodenum inj -multi organs fail
Arterial disease short note by S.Wichien (SNG KKU)
Mesenteric a disease ->60yr, woman 3x Cause -atherosclerotic vascu ds--most com other -mesenteric arteritis -radiation arteritis -cholesterol emboli -polyarteritis nodosa -lupus eryth, kawasaki -fibromuscular dysplasia -heavy smoke,young women+OC (intimal hyperpla of a.) Blood supply to intestine (chronic MI--2/3 of vv involved) 1.celiac a (CA) 2.sup mesenteric a (SMA)--most com 3.inf mesenteric a (IMA) CA-SMA anastomosis -sup/inf pancreaticodudodenal a SMA-IMA anastomosis -Drummon arce -Riolan arce Clinical Acute -abdo pain out of proportion to clinical finding in acute type -sudden onset of abdominal cramp in pt c cardiac/atherosclerosis dz -bloody diarrhea from ischemia -bowel emptying from intes spasm -fever-n/v-abdo distention Chronic -postpandrial abdo.pain, food fearwt loss -abdo angina Non-occlusive -old age c CHF,AMI c cardio shock, hypovolemic, hemorrhagic shock, sepsis,digitalis, pancreatitis, vasoconstrictor (epi) -abdo pain (70%of case) :severe pain :vary in locate,character,intensive lnvest -CBC:hemoconcen,leukocytosis -met acidosis -hyperK,azotemia in late stage -film abdomen(exclude other cause) :finding-adynamic ileus, gasless -duplex u/s--use after sx recon -CTA,MRA Definite dx--gold std :biplanar mesen arteriography :time consuming dx 1.emboli -lodge in SMA at origin of middle colic a (meniscus sign) 2.thrombosis -most proximal SMA -taper off 1-2 cm from it origin Therapeutic role in 2. -transcath thrombolytic tx -little role--require definite sx tx -difficult assess bowel viable 3.chronic occlusion -collateral vv 4.non occlusive -segmental mesen vasospasm -diffuse spasm of intes arcade -normal appear SMA trunk Therapeutic role in 4. -catheter at SMA orifice -vasodilator : papaverine
-meandering mesenteric a
:unnamed retroperi collat vv GI Hormone vasodilate -NO,glucagon,VIP Vasocons -vasopressin Type of mesenteric a occlusive dz 1.acute mesen ishemia A.acute embolic -origin from cardiac--AF/MI B.acute thrombotic -typical origin of MA 2.chronic mesen ischemia A.long atherosclerotic process -2/3 of three main MA B.CA compression synd -median arcuate lig synd -extrinsic compression 3.nonocclusive mesen ischemia -low flow state -normal mesen artery -criticism ill pt + vasopressor Aortic operation -OR--ligate IMA -aortic dissection include MA
Arterial disease short note by S.Wichien (SNG KKU)
Endovascular Tx Acute mesenteric ischemia -cath directed thrombolytic tx -urokinase/recombinant tissue PA -within 12 hr of onset -may lead to delay open revas -should select pt Chronic mesenteric ischemia -balloon dilate/stent placement -hi med comorbid, recurrent dz anastomosis stricture (previous sx) Stent placement -calcify ostial stenosis -hi grade eccentric stenosis -chronic occlusion -sig residual stenosis >30% -dissect after angioplasty -restenosis after PTA Non occlusive MI -selective mesen a catheterization follow by infusion of vasodilator (tolazoline,papaverine) :papaverine 30-60 mg/h -concomitant iv heparin :prevent thrombosis in canulate vv -beware hypoT--cath migrate to aorta -if have sign of continue bowel ische (rebound tender/involunguarding)-Sx -Sx should kept warm :prevent further intes vasoconstrict Clinical results of endovascular -inf success rate -low MM--suit in hi risk pt Surgical repair 1.acute embolic MI -fluid resus/anticoag--heparin/ATB 1goal of sx -restore a.perfusion + remove emboli Procedure -midline incision -lift transverse colon/SMB to RUQ -approach SMA :root of SMB mesentery :beneath pancrease :across jxn of 3rd-4th duodenum -proximal control -transverse arteriotomy -balloon embolectomy catheter -assess intestinal viability :intraoperative iv fluorescin injection +inspection with Wood lamp :Doppler assess of antimesen intes -2nd look procedure +/- in 24-48 hr :reassess bowel viability 2.acute thrombotic MI -usually involve atheroscler vv -typical at prox CA,SMA -requir recons procedure to distal SMA to bypass proximal occlusive lesion saphenous v -graft material of choice -avoid prothetic graft--infection Antegrade bypass--supraceliac aorta Retrograde bypass--infrarenal/iliac artery supraceliac infradiphragmatic aorta -less chance kinking -no atherosclerotic lesion 3.chronic MI -goal--revascu mesen circu + prevent develop bowel infarction -typical--multiple mesen a involve Transaortic endarterectomy -ostial lesion of CA MSA -lateral aortotomy Mesen a bypass -lesion 1-2 cm distal to mesen origin 4.celiac a compression synd Goal -release lig structure compress CA -correct persistent stricture--bypass Extrinsic compress -endovascular--fail/recur -should open sx
Arterial disease short note by S.Wichien (SNG KKU)
Acute limb ischemia doppler sensory weak A V 1 no no audible audible 2a minimal no inaudible audible 2b more mild-mod inaudible audible rest pain,intrinsic muscle 3 profound anes+paralysis inaudible skin bleb 1-viable 2-threatened 2a-marginal 2b-immediate--immediate revascu 3-irreversible Embolism source -heart--most com--AF,MI -aortic a eurysm -paradoxical emboli--patent F.ovale Thrombosis -risk f of atherosclerotic -hypercoagulable stage Tx Medical Tx -if no C/I,should heparin -hypercoagulable w/u if suspicious -prevent propagation of clot -iv fluid -retained foley catheter -cr Endovascular Tx 1.Thrombolysis -1st line in class 1,2a Advantage -reduce endothelial trauma -can small br -gradual thrombolyzedec reperfu.S Absolute CI -CVA(+TIA) in 2m -active bleeding diathesis -<10d GIB -neuro sx/IC trauma 3mo C/p -hemorrhage stroke 1-2% 2.percu.mechanical thrombectomy -class 2b -CI for thrombolysis -use djunct c thrombolysis Surgical Tx 1.Embolectomy -prep abdomen,contralat groin, entire lower ext in field -groin vertical incision -expose CFA and bifurcation -transverse arteriotomy -Fogarty balloon embolectomy cathter -complete angiogram -close artery,fully anticoagulant -Post-op:echo,CTdescend/abdo aorta to seek source of emboli -post revascularized syndrome :hypoT,hyperK,myoglobinuria,RF 2.Preexisting PVD -embolectomy can't pass occlusion -angiogram--for extent of occlude, search inflow/distal outflow :to decide thrombolysis vs bypass 2 option 1.bypass graft thrombectomy -good distal vv -good saphenous v graft 2.catheter-based lytic therapy -t-PA,urokinase -lysis time 12-36hr -once clot dissolved,underlying stenosis are tx c balloon angioplasty, stenting,by pass C/P of revascularization -reperfusion synd -compartment synd--ant comp -ischemic neuropathy -m.necrosis -recurrent thrombosis Recurrent thrombosis -recurrent embolization -inadequate removal -a.inj from thrombectomy cath -m.edema precluding distal flow -hypercoag state -technical problems c graft, arteriotomy closure
Arterial disease short note by S.Wichien (SNG KKU)
Chronic limb ischemia (>2wk) Vascular claudication -walk--cramping,tight pain Disbling claudication -claudication <50-100 m -dec of distance Critical limb -ischemic rest pain -toe p.<30,ankle p.<50 mmhg Rutherford class Grade cat 0 0 asymp,normal stress test 1 1 mild claudication 2 mod claudication 3 severe claudication 2 4 ischemic rest pain 5 minor tissue loss 3 6 major tissue loss extending above TM level TASCII (of femoropopliteal occlusion) A--endovascular Tx -single stenosis <=10cm -single occlude <=5cm B -multi steno/occlude c <=5cm/each -single stenosis <=15cm (not infrageniculate popli a) -absent conti tibial vv for distal bypass -single popliteal stenosis C -multi stenosis/occlude >=15cm -recur after 2 endovascular D--open sx -occlude >20cm, involved popliteal -occlude popliteal+prox trifurcation Site -distal SFA--most common (entrap by adductor hiatus) ABI Rt ABI Higher rt S.P.dorsalis,post tibial/ Higher rt/lt S.P.brachial lt ABI Higher lt S.P.dorsalis,post tibial/ Higher rt/lt S.P.brachial >1 =normal <0.9 = PAD 0.5-0.7 =claudication 0.3-0.5 =rest pain <0.3 =gangrene
Arterial disease short note by S.Wichien (SNG KKU)
Chronic AO endovascular Technical -access site=CFA -traverse lesion with guidewire -under fluoroscope -heparin--prevent pericath thrombosis :80-100 u/kg bolus :1000 u/hr Tx--angioplasty,stent,stent graft, anthrectomy -ASA, plavix 6 wk (if stent) 1.percu translumi balloon angioplasty -severe pain--vv rupture/dissect limit in -longer lesion -infrapopliteal 2.subintimal angioplasty -long segment, heavy calcify, fail intraluminal approach -create subintimal dissection 1,2 c/p -dissection,rupture,emboli,pseudoA restenosis,hematoma,vasospasm, Chronic AO Sx 1.Endarterectomy -use in CFA,PFA -no role in SFA--restenosis -open longitudinal--excised atheroma 2.bypass grafting A.SFA,normal PA>4cm,1 vv to foot -AK femoropopliteal bypass graft -PTFE/saphenous VG B.PA involved -outflow--BK-PA,ATA,PTA,peronel a Patency -length of bypass--long=dec patency -quality of recipient a -extent of run off -quality of conduit--VG (not PTFE infrapopliteaL) 2 technic 1.reversed SVG 2.in situ SVG C/p VG thrombosis -15% in 18mo -duplex scan q 3mo--graft velocity :>300cm/s or <45cm/s -stenosis >50%--should repair Tx -angioplasty/stent -short segment venous interposition Limb swelling Wound infection -prosthesis graft infec--excised 3.amputation -class 3 -critical limb in non ambulate :knee contracture,stroke
3.stent placement IC -residual stenosis s/p PTA >30% -dissection/perforate s/p PTA Self expanding stent Ballon expanding stent DES--drug eluting stent -dec restenosis 4.Stent graft Unsupport stent graft--PTFE Support stent graft--metallic skeletal -more inflam--risk graft thrombosis 3,4 c/p -stent fracture/deformity -cover collateral vv-5.Athrectomy device Laser athrectomy C/p -same PTA
Arterial disease short note by S.Wichien (SNG KKU)
Aortoiliac occlusion Collateral a 1.SMA--IMA--hemorrhoid a--int iliac 2.lumbar a--sup gluteal--int iliac 3.lumbar a--deep circum a--CFA 4.subclavian--sup epigas--inf epi --ext illiac (winslow pw) Classification T1.distal aorta+CIA--5-10% -rare limb threatened symp--collat -leriche syndrome -microembolize--trash foot T2.diffuse abdo aorta+CIA--25% -CIA--above inguinal ligament T3.diffuse above-below inguinal--65% -DM,HT,CVA,ACS -present advanced ischemia -require revascularize TASCll TypeA--very good in endovascu -uni/bilat CIA stenosis -uni/bilat EIA stenosis (<=3cm) TypeB--prefer endovascular -infrarenal aorta stenosis (<=3cm) -uni CIA occlusion -EIA stenosis (3-10cm) not to CFA -uni EIA occlusion TypeC--prefer sx -bilat CIA occlusion -bilat EIA stenosis(3-10cm) not to CFA -uni EIA stenosis to CFA -uni EIA occlusion involve IIA,CFA -heavy calcify uni EIA occlusion TypeD--sx -infrarenal occlusion -diffuse ds--aorta,both iliac -diffuse multi steno-uni CIA,EIA,CFA -uni occlusion CIA+EIA -bilat occlusion EIA -iliac stenosis in AAA :not endograft---should open Aortoilliac endovascular Focal aortic stenosis -self expanding stent or balloon expandable stent -balloon size 12-18 mm -distal aorta+bilat prox iliac lesion :kissing stent--bilat prox iliac stent C/p -back/abdo.pain--impending rupture :stent grant Occlusive of aortic bifurcate -kissing balloon Technique :2 angioplasty balloon :across ostia of CIA -require kissing stent Illiac artery disease PTA -isolate iliac stenosis <4cm Primary stenting -longer iliac lesion -all TASC II C/D -recur stenosis after previous PTA -lesion prone distal emboli after PTA :calcify/ulcerate plaque :plaque w spon dissection Selective stenting -PTA-->inadequate-->stent C/p 1.distal embolization--2-10% Tx -percu cath aspiration -sx embolec--large lesion 2.pseudoaneurysm --0.5% -at puncture site Percu thrombin injection u/s guide ->2cm -c/p--rupture Tx--occlusive balloon--coverd stent -faild--sx
Arterial disease short note by S.Wichien (SNG KKU)
Aortoilliac Sx 1.Aortobifem bypass -80%--relief symptom -10-15%--require outflow recons Approach 1.Long midline 2.Retroperitoneal -lt frank incision -previous abdo sx -less GI disturb,dec 3rd space loss Proximal anastomosis 1.end to end -aortic aneurysm 2.end to side -large aberrant renal a unusual large IMA :poor back flow -occlude bilat EIA :no retrograde flow--not end to end Disadvantage -distal embolization -aortoenteric fistula--difficult coverage Distal anastomosis -retroperitonium to groin -end to side anastomosis -aware declamp hypoT 5.Femorofemoral bypass -unilat occlusion CIA/EIA -rest pain, tissue loss, intractable clau -5yr patency--60-70% -inferior to aortofemoral bypass -not clamp aorta--in multi-comorbid -donor site dz--may steal synd 6.Obturator bypass Can't groin area -groin sepsis--prior prosthesis graft -groin tumor/radiation Procedure -tunnel--anteromedial to distal SFA -awarw obturator a/n -mobilized vascularized m flap cover 7.Thoracofemoral bypass IC 1.multiple prior sx c fail intrarenal aortic recons 2.infected aortic prosthesis Procedure -Lt thoracotomy tunnel 1.lt thorax--post lt kidney--lt inguinal li 2.rt limb--retzius space C/p Early -graft thrombosis--1-3% -retroperi bleeding -groin hematoma -declamped shock -bowel ischemia--2% -embolization -ED -lymph leak/chylous ascites -paraplegia Late -graft thrombosis--most com late c/p -graft infection--1% -anastomosis pseudoaneurysm--sx -aortoenteric fistula -aortourinary fistula
Rule -if PFA can 4mm probe or no.3 fogarty can pass 20 cm =adequate outflow/ not revas
2.Aortic endarterctomy -rarely perform :difficult, hi-EBL/sex dysfxn -pt risk of graft infection -hi early thrombosis/late failure 3.Axillofemoral bypass (+femorofemoral crossover) -extraanatomical bypass -hi comorbid pt -patency < aortobifem -axillary a--below clavicle -CFA bifurcate -6-8 mm PTFE graft -5yr patency--30-80% 4.Iliofemoral bypass -unilat occlusion distal CIA/EIA
Arterial disease short note by S.Wichien (SNG KKU)
Graft Autogenous vein -superior to prosthesis -ipsil/contralat GSV,SSV,arm vein Cryopreserved graft -cadaveric -expensive -more failure -freeze--endo.lost--early thrombosis -role in remove infect prosthesis graft + no VG Human umbilical v -less use than PTFE Prosthetic conduit -AK bypass+no VG--PTFE or dacron Compartment syndrome -prolong ischemia follow by reperfuse -capillary leak fluid into interstitial space in muscle which nondistend fascia -most : anterior compartment in leg Compartment Anterior -ext m.,tibialis ant,EDL,EHL, peroneus tertius -ant tibial a/v -deep peroneal n. Lateral -peroneus longus/brevis -sup peroneal n. Deep posterior -deep flexor m,FDL,tibialis post,FHL, popliteus -post tibial a/v,peroneal a/v
Celiac a compression synd -extrinsic compress/impingement -by median arcuate ligament -chronic MI -young female 20-40 yr -abdo symptom ; non specific -pain localize in upper abdomen
-tibial n.
Superficial posterior -superficial flexor m,soleus, gastrocnemius,plantaris Clinical -excessive pain -pain on passive stretching -sensory loss due to n.compression -numbness in web space of 1st-2nd toe : deep peroneal n.comp. Measure -insert arterial line into compartment -Pressures greater than 45 mmHg usually require operative intervention. Pressures between 30 and 45 mmHg should be carefully evaluated and watched closely.
precipitate by meal
-Rx = release ligament structure+ correct any persist stricture by bypass grafting
Buerger ds -thromboangitis obliteran -cause--unknown -non atherosclerotic -small/medium a,v,n -upper/lower ext -20-50 yr,male,smoke -migratory superficial phlebitis Ix Angiography--4 limb -ds confine distal circu -infrapop/distal BA -segmental/skip lesion -extensive collateral--corkscrew Tx -smoking cessation -sx--minimal role--no target vv
You might also like
- Prophylactic ETT 6yr Fail IV 2: Primary Survey 1.airway 3.circulationDocument17 pagesProphylactic ETT 6yr Fail IV 2: Primary Survey 1.airway 3.circulationURo KkuNo ratings yet
- Possible Sign of Superfi V.abnor: 2 Primary FXNDocument7 pagesPossible Sign of Superfi V.abnor: 2 Primary FXNURo KkuNo ratings yet
- Weed12.jpg: Ikue Nakayama PGY-3Document46 pagesWeed12.jpg: Ikue Nakayama PGY-3skaruthuNo ratings yet
- Reflec in SXDocument2 pagesReflec in SXURo KkuNo ratings yet
- Aortic Disease and ProceduresDocument58 pagesAortic Disease and ProceduresJ_SteinbergNo ratings yet
- Surgery Reviosn NotesDocument41 pagesSurgery Reviosn Noteshy7tn100% (1)
- Congenital Heart Disease (CHD) : Lecture For C-I StudentsDocument89 pagesCongenital Heart Disease (CHD) : Lecture For C-I StudentsGomathi ShankarNo ratings yet
- Acute Arterial OcclusionDocument44 pagesAcute Arterial OcclusionAlbertus Maria Henry SantosoNo ratings yet
- 07 The Valvular PatientDocument83 pages07 The Valvular PatientDanielaNo ratings yet
- I ST - Vascular SurgeryDocument117 pagesI ST - Vascular SurgeryMohammad_Islam8767% (3)
- Congenital Heart Disease (CHD) : Kussia Ayano (MD)Document54 pagesCongenital Heart Disease (CHD) : Kussia Ayano (MD)Yemata HailuNo ratings yet
- Dr. Amanj Kamal Mohammed F.I.C.M.S. Cardiovascular SurgeryDocument47 pagesDr. Amanj Kamal Mohammed F.I.C.M.S. Cardiovascular SurgerydrelvNo ratings yet
- VESAP Study Guide 2Document8 pagesVESAP Study Guide 2jhk0428No ratings yet
- Liver TraumaDocument27 pagesLiver Traumamuhammad haryatman-No ratings yet
- Anatomy: - 4 Glands ( 4 Gland 3%) PhysiologicDocument6 pagesAnatomy: - 4 Glands ( 4 Gland 3%) PhysiologicURo KkuNo ratings yet
- Echographie Cardiaque AnglaisDocument1 pageEchographie Cardiaque AnglaiswkoussahNo ratings yet
- 58-63 DallAra JIC 2020 Feb WMDocument6 pages58-63 DallAra JIC 2020 Feb WMJose Manuel Ornelas-AguirreNo ratings yet
- Neuroimaging of Stroke (Early Signs On CT and MRI)Document48 pagesNeuroimaging of Stroke (Early Signs On CT and MRI)erickoteNo ratings yet
- Test 39 Qid: 2300: Medicine - Pulmonary & Critical CareDocument7 pagesTest 39 Qid: 2300: Medicine - Pulmonary & Critical Carekabal321No ratings yet
- Classification of Cardiac Malformations: Daniel Bernstein's (Clinical + Physiopathological)Document28 pagesClassification of Cardiac Malformations: Daniel Bernstein's (Clinical + Physiopathological)Sandyka AleNo ratings yet
- Acute Appendicitis: Incidence SignsDocument4 pagesAcute Appendicitis: Incidence SignsWichien SiriNo ratings yet
- 2 StrokeDocument82 pages2 StrokeNikhilNo ratings yet
- Aortic Aneurysm: Imu LectureDocument73 pagesAortic Aneurysm: Imu LectureCeline HerreraNo ratings yet
- Moya Moya DiseaseDocument87 pagesMoya Moya DiseaseDilip Kumar MNo ratings yet
- 2-Ammar Notes (Surgery)Document16 pages2-Ammar Notes (Surgery)anmar alkhudhriNo ratings yet
- Bailey S1Document17 pagesBailey S1hazama kurroNo ratings yet
- Rutherford CH96 - Unusual Conditions of The Carotid ArteryDocument3 pagesRutherford CH96 - Unusual Conditions of The Carotid Arteryomamah.almousaNo ratings yet
- Amboss:CardioDocument18 pagesAmboss:CardioNicole Juliette CCNo ratings yet
- Jurnal Coronary Artery FistulaDocument3 pagesJurnal Coronary Artery FistulaRistinyaUnuyNo ratings yet
- Endopeptidase: Carbo ProteinDocument12 pagesEndopeptidase: Carbo ProteinURo KkuNo ratings yet
- Carotid and Vertebral Ultrasonography - Dr. DanielDocument74 pagesCarotid and Vertebral Ultrasonography - Dr. DanielSuci Rahayu Evasha100% (1)
- Bipolar Blindness in MappingDocument5 pagesBipolar Blindness in MappingTanah PantaiNo ratings yet
- LiverDocument27 pagesLiverAndi Arwan AgusnawanNo ratings yet
- 04c4spleen ReviewDocument24 pages04c4spleen ReviewMadhavan KhannaNo ratings yet
- Liver Trauma: Mohamed. Hashim Milhim Year Medstudent An-Najah National UnivDocument27 pagesLiver Trauma: Mohamed. Hashim Milhim Year Medstudent An-Najah National Univsatya.drNo ratings yet
- TBB Giant CellDocument2 pagesTBB Giant CellRestiNo ratings yet
- Abdominal Aortic Aneurysm 1Document44 pagesAbdominal Aortic Aneurysm 1Kendy Rizky Hadyan100% (1)
- Congenital Heart Disease (CHD)Document89 pagesCongenital Heart Disease (CHD)jefferyNo ratings yet
- Iatrogenic Acute Aortic Dissection During PPCIDocument4 pagesIatrogenic Acute Aortic Dissection During PPCISajjad HussainNo ratings yet
- All About Leg UlcerDocument51 pagesAll About Leg Ulcersyifa_mustika100% (1)
- 3.trauma Vaskular Richard SDocument79 pages3.trauma Vaskular Richard SAdang SunandarNo ratings yet
- Peds Study GuideDocument73 pagesPeds Study GuideYvonne Huang100% (1)
- UMS20 Medical 20 Short 20 and 20 Long 20 Cases 20 Record 20 Second 20 EditiDocument132 pagesUMS20 Medical 20 Short 20 and 20 Long 20 Cases 20 Record 20 Second 20 EditiUchiha AnzarNo ratings yet
- May 2022 MRCS Part A Recalls - 1Document11 pagesMay 2022 MRCS Part A Recalls - 1JU WSDNo ratings yet
- Acute Stroke ManagementDocument51 pagesAcute Stroke Managementmae sarohNo ratings yet
- Adrenal Cortex: Embryo Cushing SyndDocument7 pagesAdrenal Cortex: Embryo Cushing SyndWichien SiriNo ratings yet
- Letters: Safety of Angioplasty For Intracranial Artery ReferencesDocument5 pagesLetters: Safety of Angioplasty For Intracranial Artery Referencesaula nisafitriNo ratings yet
- Clinical Cases: Ischaemic Heart DiseaseDocument4 pagesClinical Cases: Ischaemic Heart DiseaseLADY JOWAHER ALLASNo ratings yet
- Extracranial Cerrebrovascular DiseaseDocument10 pagesExtracranial Cerrebrovascular DiseaseAbrar SabawiNo ratings yet
- Adobe Scan 12 Aug 2023Document2 pagesAdobe Scan 12 Aug 2023Gowtham LNo ratings yet
- Sindromul Coronarian Acut: UMF VB Timisoara Departamentul VI Medicina Interna de AmbulatorDocument78 pagesSindromul Coronarian Acut: UMF VB Timisoara Departamentul VI Medicina Interna de AmbulatorIulia CeveiNo ratings yet
- Anatomy (Length: Duodenum 2.submucosaDocument12 pagesAnatomy (Length: Duodenum 2.submucosaURo KkuNo ratings yet
- Dural Avf - Classification and Management PDFDocument144 pagesDural Avf - Classification and Management PDFAciNo ratings yet
- Assignment ON: TOPIC: PTCA (Percutaneous Transluminous Coronary Angioplasty)Document7 pagesAssignment ON: TOPIC: PTCA (Percutaneous Transluminous Coronary Angioplasty)soniya josephNo ratings yet
- Aneurysms & Aortic DissectionDocument36 pagesAneurysms & Aortic Dissectionr100% (1)
- Aydarous Vascular AnathesiaDocument30 pagesAydarous Vascular Anathesiagulf jobs100% (1)
- New Approaches to Aortic Diseases from Valve to Abdominal BifurcationFrom EverandNew Approaches to Aortic Diseases from Valve to Abdominal BifurcationNo ratings yet
- Atlas of Coronary Intravascular Optical Coherence TomographyFrom EverandAtlas of Coronary Intravascular Optical Coherence TomographyNo ratings yet
- Abdominal PainDocument76 pagesAbdominal PainURo KkuNo ratings yet
- Case Discussion: Stab Injury L Frank CHFDocument27 pagesCase Discussion: Stab Injury L Frank CHFURo KkuNo ratings yet
- Ruptured DiverticulitisDocument18 pagesRuptured DiverticulitisURo KkuNo ratings yet
- Mesenteric AdenitisDocument28 pagesMesenteric AdenitisURo KkuNo ratings yet
- Perirenal HematomaDocument23 pagesPerirenal HematomaURo KkuNo ratings yet
- แบบฝึกหัด Essay 4.1Document1 pageแบบฝึกหัด Essay 4.1URo KkuNo ratings yet
- Urologic Imaging For Externist PDFDocument55 pagesUrologic Imaging For Externist PDFURo KkuNo ratings yet
- Malignant Renal TumorDocument17 pagesMalignant Renal TumorURo KkuNo ratings yet
- Hepatoblastoma ReseachDocument32 pagesHepatoblastoma ReseachURo KkuNo ratings yet
- GEP NETsDocument3 pagesGEP NETsURo KkuNo ratings yet
- Renal Trauma BluntDocument40 pagesRenal Trauma BluntURo KkuNo ratings yet
- Histology: GIST Short Note by by S.Wichien (SNG KKU)Document3 pagesHistology: GIST Short Note by by S.Wichien (SNG KKU)URo KkuNo ratings yet
- LRP PresentationDocument21 pagesLRP PresentationURo KkuNo ratings yet
- แบบฝึกหัด Essay 3Document1 pageแบบฝึกหัด Essay 3URo KkuNo ratings yet
- Parietal Cell: Angle of His Angularis IncisuraDocument13 pagesParietal Cell: Angle of His Angularis IncisuraURo Kku100% (1)
- แบบฝึกหัด Essay 3Document1 pageแบบฝึกหัด Essay 3URo KkuNo ratings yet
- Endopeptidase: Carbo ProteinDocument12 pagesEndopeptidase: Carbo ProteinURo KkuNo ratings yet
- UrologyDocument10 pagesUrologyURo KkuNo ratings yet
- Anatomy (Length: Duodenum 2.submucosaDocument12 pagesAnatomy (Length: Duodenum 2.submucosaURo KkuNo ratings yet
- Anatomy: - 4 Glands ( 4 Gland 3%) PhysiologicDocument6 pagesAnatomy: - 4 Glands ( 4 Gland 3%) PhysiologicURo KkuNo ratings yet
- HerniaDocument5 pagesHerniaURo KkuNo ratings yet
- SpleenDocument3 pagesSpleenURo KkuNo ratings yet
- ColorectalDocument26 pagesColorectalURo KkuNo ratings yet
- BreastDocument13 pagesBreastURo KkuNo ratings yet
- LiverDocument13 pagesLiverURo KkuNo ratings yet
- Acute PancreatitisDocument36 pagesAcute PancreatitisURo KkuNo ratings yet
- 2012 Conference NewsfgfghsfghsfghDocument3 pages2012 Conference NewsfgfghsfghsfghabdNo ratings yet
- White Cataract What To AssesDocument2 pagesWhite Cataract What To Assesalif andraNo ratings yet
- DILG Opinion-Sanggunian Employees Disbursements, Sign Checks & Travel OrderDocument2 pagesDILG Opinion-Sanggunian Employees Disbursements, Sign Checks & Travel OrderCrizalde de DiosNo ratings yet
- Bugatti Type 57SCDocument10 pagesBugatti Type 57SCjorge Angel Lope100% (1)
- SAP HCM Case StudyDocument17 pagesSAP HCM Case StudyRafidaFatimatuzzahraNo ratings yet
- Assignment 1 Brief: ScenarioDocument4 pagesAssignment 1 Brief: ScenarioChâu TrầnNo ratings yet
- Atoll 1400Document2 pagesAtoll 1400David M. SeoaneNo ratings yet
- Technology ForecastingDocument38 pagesTechnology ForecastingSourabh TandonNo ratings yet
- Sheet (8) Synchronous Machine Problem (1) :: SolutionDocument5 pagesSheet (8) Synchronous Machine Problem (1) :: Solutionمكاريوس عيادNo ratings yet
- Coefficient of Restitution - Center of MassDocument3 pagesCoefficient of Restitution - Center of MassMannyCesNo ratings yet
- A Tall Order - Cooling Dubai's Burj Khalifa: FeatureDocument2 pagesA Tall Order - Cooling Dubai's Burj Khalifa: FeatureMohsin KhanNo ratings yet
- Types of Intermolecular ForcesDocument34 pagesTypes of Intermolecular ForcesRuschan JaraNo ratings yet
- Adsorption ExperimentDocument5 pagesAdsorption ExperimentNauman KhalidNo ratings yet
- Necromunda CatalogDocument35 pagesNecromunda Catalogzafnequin8494100% (1)
- 04 Membrane Structure NotesDocument22 pages04 Membrane Structure NotesWesley ChinNo ratings yet
- Volvo Catalog Part2Document360 pagesVolvo Catalog Part2Denis Konovalov71% (7)
- Ducati WiringDocument7 pagesDucati WiringRyan LeisNo ratings yet
- Family Factors: Its Effect On The Academic Performance of The Grade 6 Pupils of East Bayugan Central Elementary SchoolDocument11 pagesFamily Factors: Its Effect On The Academic Performance of The Grade 6 Pupils of East Bayugan Central Elementary SchoolGrace Joy AsorNo ratings yet
- PMDG 737NGX Tutorial 2 PDFDocument148 pagesPMDG 737NGX Tutorial 2 PDFMatt HenryNo ratings yet
- Net Pert: Cable QualifierDocument4 pagesNet Pert: Cable QualifierAndrés Felipe Fandiño MNo ratings yet
- Offshore Training Matriz Matriz de Treinamentos OffshoreDocument2 pagesOffshore Training Matriz Matriz de Treinamentos OffshorecamiladiasmanoelNo ratings yet
- Ocr A Level History Russia CourseworkDocument7 pagesOcr A Level History Russia Courseworkbcrqhr1n100% (1)
- Honeywell Rondostat Hr20 SpesificationDocument2 pagesHoneywell Rondostat Hr20 Spesificationfrox123No ratings yet
- 4D Beijing (Muslim) CHINA MATTA Fair PackageDocument1 page4D Beijing (Muslim) CHINA MATTA Fair PackageSedunia TravelNo ratings yet
- MARTELINO Vs Alejandro DigestDocument1 pageMARTELINO Vs Alejandro Digestheirarchy100% (2)
- ISSA2013Ed CabinStores v100 Часть10Document2 pagesISSA2013Ed CabinStores v100 Часть10AlexanderNo ratings yet
- Purification of Dilactide by Melt CrystallizationDocument4 pagesPurification of Dilactide by Melt CrystallizationRaj SolankiNo ratings yet
- PPT-QC AcDocument34 pagesPPT-QC AcAmlan Chakrabarti Calcutta UniversityNo ratings yet
- Beng (Hons) Telecommunications: Cohort: Btel/10B/Ft & Btel/09/FtDocument9 pagesBeng (Hons) Telecommunications: Cohort: Btel/10B/Ft & Btel/09/FtMarcelo BaptistaNo ratings yet
- CP3 - June2019 2Document5 pagesCP3 - June2019 2Sifei ZhangNo ratings yet