Professional Documents
Culture Documents
Nursing Care Plan For Fracture PN303
Uploaded by
Fryam BellsOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Nursing Care Plan For Fracture PN303
Uploaded by
Fryam BellsCopyright:
Available Formats
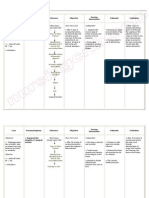
Nursing Care Plan for Fracture
Nursing Diagnosis Pain, acute related to Muscle spasms Movement of bone fragments, edema, and injury to the soft tissue Cues Reports of pain Distraction; selffocusing/narr owed focus; facial mask of pain Goals Verbalize relief of pain Display relaxed manner; able to participate in activities, sleep/rest appropriately. Intervention Independent 1. Maintain immobilization of affected part by means of bed rest, cast, splint, traction. 2. Elevate and support injured extremity. 3. Avoid use of plastic sheets/pillows under limbs in cast. 4. Elevate bed covers; keep linens off toes. 5. Evaluate/document reports of pain/discomfort, noting location and characteristics, including intensity (010 scale), relieving and aggravating factors. Note nonverbal pain cues (changes in vital signs and emotions/behavior). 6. Listen to reports of family member/SO regarding patients pain. 7. Encourage patient to discuss problems related to injury. 8. Provide alternative comfort measures, e.g., massage, back rub, position changes. 9. Provide emotional support and encourage use of stress management techniques, e.g., progressive relaxation, deep-breathing exercises, visualization/guided imagery; provide Therapeutic Touch. 10. Identify diversional activities appropriate for patient age, physical abilities, and personal preferences.
Traction/immobil Guarding, ity device protective behavior; Stress, Anxiety alteration in muscle tone; autonomic responses
Dependent 1. Apply cold/ice pack first 24 72 hr and as necessary. 2. Administer medications as indicated: narcotic and nonnarcotic analgesics, e.g., morphine, meperidine (Demerol), hydrocodone (Vicodin); injectable and oral nonsteroidal antiinflammatory drugs (NSAIDs), e.g., ketorolac (Toradol), ibuprofen (Motrin); and/or muscle relaxants, e.g., cyclobenzaprine (Flexeril), carisoprodol (Soma), diazepam (Valium). Administer analgesics around the clock for 35 days. 3. Explain procedures before beginning them. Medicate before care activities. Let patient know it is important to request medication before pain becomes severe. Independent 1. Assess degree of immobility produced by injury/treatment and note patients perception of immobility. 2. Reposition periodically and encourage coughing/deep breathing exercises. 3. Encourage increased fluid intake to 20003000 mL/day (within cardiac tolerance), including acid/ash juices. 4. Encourage participation in diversional/recreational activities. 5. Maintain stimulating
Mobility, impaired physical May be related to Neuromuscular skeletal impairment; pain/discomfort; restrictive therapies (limb immobilization) Psychological immobility
Inability to move purposefully within the physical environment, imposed restrictions Reluctance to attempt movement;
Regain/maintain mobility at the highest possible level. Maintain position of function. Increase strength/functio n of affected and
limited ROM
compensatory body parts.
Decreased muscle Demonstrate strength/cont techniques that rol enable resumption of activities.
environment, e.g., radio, TV, newspapers, personal possessions/pictures, clock, calendar, visits from family/friends. Instruct patient in/assist with active/passive ROM exercises of affected and unaffected extremities. 6. Encourage use of isometric exercises starting with the unaffected limb. 7. Provide footboard, wrist splints, trochanter/hand rolls as appropriate. 8. Place in supine position periodically if possible, when traction is used to stabilize lower limb fractures. 9. Instruct in/encourage use of trapeze and post position for lower limb fractures. 10. Assist with/encourage selfcare activities (e.g., bathing, shaving). 11. Provide/assist with mobility by means of wheelchair, walker, crutches, canes as soon as possible. Instruct in safe use of mobility aids. 12. Monitor blood pressure (BP) with resumption of activity. Note reports of dizziness. Collaborative 13. Consult with physical/occupational therapist and/or rehabilitation specialist. Independent 1. Examine the skin for open wounds, foreign bodies, rashes, bleeding, discoloration, duskiness, blanching.
Impaired skin/tissue integrity r/t : Puncture injury; compound
Reports of itching, pain, numbness, pressure in
Verbalize relief of discomfort. Demonstrate
fracture; surgical affected/surr repair; insertion ounding area of traction pins, wires, screws Disruption of skin surface; Altered invasion of sensation, body circulation; structures; accumulation of destruction excretions/secre of skin tions layers/tissue s Physical immobilization
behaviors/techni ques to prevent skin breakdown/facili tate healing as indicated.
Achieve timely wound/lesion healing if present.
2. Massage skin and bony prominences. Keep the bed linens dry and free of wrinkles. Place water pads/other padding under elbows/heels as indicated. 3. Reposition frequently. Encourage use of trapeze if possible. 4. Assess position of splint ring of traction device.
Cast Care: Wet (NIC) 1. Plaster cast application and skin care: Cleanse skin with soap and water. Rub gently with alcohol and/or dust with small amount of a zinc or stearate powder; 2. Cut a length of stockinette to cover the area and extend several inches beyond the cast; 3. Use palm of hand to apply, hold, or move cast and support on pillows after application; Independent 1. Trim excess plaster from edges of cast as soon as casting is completed; 2. Promote cast drying by removing bed linen, exposing to circulating air; 3. Observe for potential pressure areas, especially at the edges of and under the splint/cast; 4. Pad (petal) the edges of the cast with waterproof tape; 5. Cleanse excess plaster from skin while still wet, if possible;
6. Protect cast and skin in perineal area. Provide frequent perineal care; 7. Instruct patient/SO to avoid inserting objects inside casts; 8. Massage the skin around the cast edges; 9. Turn frequently to include the uninvolved side, back, and prone positions (as tolerated) with patients feet over the end of the mattress. Traction/Immobilization Care (NIC) Skin traction application and skin care: 1. Cleanse the skin with warm, soapy water; 2. Apply tincture of benzoin; 3. Apply commercial skin traction tapes (or make some with strips of moleskin/adhesive tape) lengthwise on opposite sides of the affected limb; 4. Extend the tapes beyond the length of the limb; 5. Place protective padding under the leg and over bony prominences; 6. Wrap the limb circumference, including tapes and padding, with elastic bandages, being careful to wrap snugly but not too tightly; 7. Palpate taped tissues daily and document any tenderness or pain; 8. Remove skin traction every 24 hr, per protocol; inspect and give skin care.
Skeletal traction/fixation application and skin care: y Bend wire ends or cover ends of wires/pins with rubber or cork protectors or needle caps; y Pad slings/frame with sheepskin, foam. Pressure Management (NIC) Collaborative Provide foam mattress, sheepskins, flotation pads, or air mattress as indicated. Monovalve, bivalve, or cut a window in the cast, per protocol. Peripheral Neurovascular, dysfunction, risk for Risk factors may include Reduction/interr uption of blood flow Direct vascular injury, tissue trauma, excessive edema, thrombus formation Hypovolemia Independent Maintain tissue perfusion as evidenced by palpable pulses, skin warm/dry, normal sensation, usual sensorium, stable vital signs, and adequate urinary output for individual situation. 1. Remove jewelry from affected limb. 2. Evaluate presence/quality of peripheral pulse distal to injury via palpation/Doppler. Compare with uninjured limb. 3. Assess capillary return, skin color, and warmth distal to the fracture. 4. Assess entire length of injured extremity for swelling/edema formation. Measure injured extremity and compare with uninjured extremity. Note appearance/spread of hematoma. 5. Note reports of pain extreme for type of injury or increasing pain on passive movement of extremity, development of paresthesia,
muscle tension/tenderness with erythema, and change in pulse quality distal to injury. Do not elevate extremity. Report symptoms to physician at once. 6. Encourage patient to routinely exercise digits/joints distal to injury. Ambulate as soon as possible. Collaborative Apply ice bags around fracture site for short periods of time on an intermittent basis for 2472 hr. Infection, risk for Risk factors may include Inadequate primary defenses: broken skin, traumatized tissues; environmental exposure Invasive procedures, skeletal traction Independent Achieve timely wound healing, be free of purulent drainage or erythema, and be afebrile. 1. Inspect the skin for preexisting irritation or breaks in continuity. 2. Assess pin sites/skin areas, noting reports of increased pain/burning sensation or presence of edema, erythema, foul odor, or drainage. 3. Provide sterile pin/wound care according to protocol, and exercise meticulous handwashing. 4. Observe wounds for formation of bullae, crepitation, bronze discoloration of skin, frothy/fruity-smelling drainage. 5. Assess muscle tone, reflexes, and ability to speak. 6. Monitor vital signs. Note presence of chills, fever, malaise, changes in mentation. 7. Investigate abrupt onset of
pain/limitation of movement with localized edema/erythema in injured extremity. Collaborative Monitor laboratory/diagnostic studies, e.g.: Complete blood count (CBC); ESR; Cultures and sensitivity of wound/serum/bone; Radioisotope scans. Administer medications as indicated, e.g.: IV/topical antibiotics; Tetanus toxoid. Gas Exchange, risk for impaired Risk factors may include: Altered blood flow; blood/fat emboli Alveolar/capillar y membrane changes: interstitial, pulmonary edema, congestion Independent Maintain adequate respiratory function, as evidenced by absence of dyspnea/cyanos is; respiratory rate and arterial blood gases (ABGs) within patients normal range. 1. Monitor respiratory rate and effort. Note stridor, use of accessory muscles, retractions, development of central cyanosis. 2. Auscultate breath sounds, noting development of unequal, hyperresonant sounds; also note presence of crackles/ rhonchi/wheezes and inspiratory crowing or croupy sounds. 3. Instruct and assist with deep-breathing and coughing. Reposition frequently. 4. Note increasing restlessness, confusion, lethargy, stupor. Collaborative Assist with incentive spirometry. Administer supplemental oxygen if indicated. Monitor laboratory studies e.g ABG
Knowledge, deficient [Learning Need] regarding condition, prognosis, treatment, selfcare, and discharge needs May be related to Lack of exposure/recall Information misinterpretation /unfamiliarity with information resources
Knowledge: Treatment Regimen (NOC) Verbalize understanding of condition, prognosis, and potential complications. Correctly perform necessary procedures and explain reasons for actions.
Teaching: Disease Process (NIC) Independent 1. Review pathology, prognosis, and future expectations. 2. Discuss dietary needs. 3. Discuss individual drug regimen as appropriate. 4. Reinforce methods of mobility and ambulation as instructed by physical therapist when indicated. 5. List activities patient can perform independently and those that require assistance. 6. Identify available community services, e.g., rehabilitation teams, home nursing/homemaker services. 7. Encourage patient to continue active exercises for the joints above and below the fracture. 8. Discuss importance of clinical and therapy followup appointments. 9. Review proper pin/wound care. 10. Recommend cleaning external fixator regularly. Teaching Disease Process: 1. Identifysigns/symptoms requiring medical evaluation, e.g., severe pain, fever/chills, foul odors; changes in sensation, swelling, burning, numbness, tingling, skin discoloration, paralysis, white/cool toes or fingertips; warm spots, soft areas,
cracks in cast. 2. Demonstrate use of plastic bags to cover plaster cast during wet weather or while bathing. 3. Clean soiled cast with a slightly dampened cloth and some scouring powder. 4. Emphasize importance of not adjusting clamps/nuts of external fixator. 5. Demonstrate use of plastic bags to cover plaster cast during wet weather or while bathing. Clean soiled cast with a slightly dampened cloth and some scouring powder. 6. Emphasize importance of not adjusting clamps/nuts of external fixator.
You might also like
- Assessing and Preventing Pressure UlcersDocument8 pagesAssessing and Preventing Pressure UlcersTamil VillardoNo ratings yet
- Fracture Nursing Care PlansDocument14 pagesFracture Nursing Care PlansjamieboyRN88% (17)
- NCP FractureDocument3 pagesNCP FractureDino V EscalonaNo ratings yet
- Impaired Physical MobilityDocument2 pagesImpaired Physical MobilityHanya Bint PotawanNo ratings yet
- FractureDocument1 pageFractureReechie TeasoonNo ratings yet
- NCP LocDocument2 pagesNCP LocMel RodolfoNo ratings yet
- Nursing Care Plan Impaire Physical MobilityDocument2 pagesNursing Care Plan Impaire Physical Mobilityderic90% (10)
- NCP Acute Pain RT CancerDocument3 pagesNCP Acute Pain RT CancerCharissa Magistrado De LeonNo ratings yet
- NCP FractureDocument2 pagesNCP Fracturemawel50% (2)
- Nursing Care Plan For Hip Fracture Assessment Diagnosis Rationale Goal & Objectives Interventions Rationale EvaluationDocument1 pageNursing Care Plan For Hip Fracture Assessment Diagnosis Rationale Goal & Objectives Interventions Rationale EvaluationJaylord Verazon100% (1)
- NCP FractureDocument1 pageNCP FractureJonathan Bermundo Barba0% (1)
- Nursing Care Plan - Impaired Physical MobilityDocument2 pagesNursing Care Plan - Impaired Physical MobilitySusan Croce57% (7)
- Massive AscitesDocument12 pagesMassive Ascitesranitidin100% (1)
- Impaired Verbal CommunicationDocument6 pagesImpaired Verbal CommunicationLaura Sansonetti100% (1)
- Nursing Care Plan for Skin IntegrityDocument3 pagesNursing Care Plan for Skin IntegrityCrystal Joy Misa100% (1)
- NCP pAlPITATIONSDocument3 pagesNCP pAlPITATIONSHazel PalomaresNo ratings yet
- Body Weakness NCPDocument1 pageBody Weakness NCPtwicetrashNo ratings yet
- NCP CholangitisDocument4 pagesNCP CholangitisJanica C. BayauaNo ratings yet
- Impaired Physical Mobility...Document3 pagesImpaired Physical Mobility...Christy BerryNo ratings yet
- NCP HemothoraxDocument3 pagesNCP HemothoraxMichael John F. NatividadNo ratings yet
- Activity IntoleranceDocument2 pagesActivity IntolerancedohbleNo ratings yet
- NCP OsteoarthritisDocument4 pagesNCP OsteoarthritisKyle Margaret Flores100% (1)
- NCP 2 and Soapie 1Document5 pagesNCP 2 and Soapie 1narsD100% (1)
- Nursing Care Plan For "Fractures"Document21 pagesNursing Care Plan For "Fractures"jhonroks97% (34)
- CP Intestinal Obstruction Nursing Care PlanDocument7 pagesCP Intestinal Obstruction Nursing Care PlanShiella Heart MalanaNo ratings yet
- Impaired Skin IntegrityDocument4 pagesImpaired Skin IntegrityMarjorie Jofel Cerrudo PaciaNo ratings yet
- Sexual history and STI examDocument2 pagesSexual history and STI examLizaEllaga67% (3)
- Case Scenario: Prostate CancerDocument5 pagesCase Scenario: Prostate Cancer24 PAULINO ALDRIN MUJARNo ratings yet
- Fistula NCPDocument1 pageFistula NCPHasna LisnaNo ratings yet
- A Renal Failure (NCP)Document2 pagesA Renal Failure (NCP)Julie Aranda Hapin100% (1)
- Hemorrhoidectomy Case StudyDocument19 pagesHemorrhoidectomy Case StudyJoyJoy Tabada CalunsagNo ratings yet
- Multiple Sclerosis Nursing Care PlanDocument4 pagesMultiple Sclerosis Nursing Care PlanCHRISTIE MONTANONo ratings yet
- Ineffective Breathing PatternDocument185 pagesIneffective Breathing PatternSusi LambiyantiNo ratings yet
- NCP PancreatitisDocument2 pagesNCP PancreatitisJeanelle GenerosoNo ratings yet
- 4 Amputation Nursing Care Plans - Nurseslabs-1 PDFDocument12 pages4 Amputation Nursing Care Plans - Nurseslabs-1 PDFsaidi MwanamongaNo ratings yet
- Case Group Work #2 CHAPTER 6 Learning Exercise 6.4 L&M 03-03-2021 SituationDocument3 pagesCase Group Work #2 CHAPTER 6 Learning Exercise 6.4 L&M 03-03-2021 SituationZunnel CortesNo ratings yet
- Hypospadia CompletedDocument92 pagesHypospadia Completedgideon A. owusu100% (1)
- NCP GbsDocument2 pagesNCP GbsJaylord VerazonNo ratings yet
- Complications of Plaster Cast PATIENT LEAFLETDocument6 pagesComplications of Plaster Cast PATIENT LEAFLETRadiyan MeidhiyantoNo ratings yet
- Drugs - Icu (Group)Document7 pagesDrugs - Icu (Group)Patricia LuceroNo ratings yet
- Post-Throidectomy Nursing Care PlanDocument2 pagesPost-Throidectomy Nursing Care PlanCyrus De AsisNo ratings yet
- Teaching Plan for Chronic Kidney Disease PatientDocument5 pagesTeaching Plan for Chronic Kidney Disease PatientYhan-yhan Rodriguez Khou100% (1)
- Nursing Care Plan for Skin InfectionDocument6 pagesNursing Care Plan for Skin Infectionالأغا محمد زكارنةNo ratings yet
- Nursing Care Plan of Pressure UlcersDocument1 pageNursing Care Plan of Pressure UlcersCyrus De Asis46% (13)
- Thyroidectomy Nursing Care PlanDocument2 pagesThyroidectomy Nursing Care PlanRnspeakcom100% (1)
- Preoperative Teaching EssentialsDocument11 pagesPreoperative Teaching EssentialsDani ThomasNo ratings yet
- Nursing Care PlanDocument13 pagesNursing Care PlanRen DolosaNo ratings yet
- Constipation NCPDocument2 pagesConstipation NCPKaren Pili100% (1)
- NCP GrandcaseDocument5 pagesNCP GrandcaseSaima BataloNo ratings yet
- Nursing Care Plan for Immobility and Pain ManagementDocument3 pagesNursing Care Plan for Immobility and Pain ManagementClariss Alota100% (2)
- NCP-Impaired Physical MobilityDocument3 pagesNCP-Impaired Physical MobilityRene John FranciscoNo ratings yet
- 1 Acute Pain NCPDocument2 pages1 Acute Pain NCPFilipinas BelzaNo ratings yet
- Nursing Care Plan Orthopedic Philipine CenterDocument4 pagesNursing Care Plan Orthopedic Philipine CenterAnonymous NZTQVgjaNo ratings yet
- Fracture NCPDocument3 pagesFracture NCPCandy Paraiso AgustinNo ratings yet
- Caring for a Cast: Monitoring for ComplicationsDocument39 pagesCaring for a Cast: Monitoring for ComplicationsGrape JuiceNo ratings yet
- Pressure Sores: AssessmentDocument7 pagesPressure Sores: AssessmentXyzelle Kim Monteilo OrtizNo ratings yet
- Pressure SoreDocument31 pagesPressure SoreElfayad HamadNo ratings yet
- 1.what Are The Risk Factors Contributing To Pressure Area Breakdown/ulcers?Document6 pages1.what Are The Risk Factors Contributing To Pressure Area Breakdown/ulcers?Paula FeierNo ratings yet
- Promote Activity Mobility and Exercise and Comfort Rest and SleepDocument14 pagesPromote Activity Mobility and Exercise and Comfort Rest and SleepCamille MaterumNo ratings yet
- Reconstruction Post Burn Injury RehabDocument23 pagesReconstruction Post Burn Injury RehabPraja KabyanataraNo ratings yet
- Conformity Influence by Ann Pryam Bagongon :0)Document4 pagesConformity Influence by Ann Pryam Bagongon :0)Fryam BellsNo ratings yet
- Karen HorneyDocument12 pagesKaren HorneyFryam Bells100% (11)
- PneumoniaDocument18 pagesPneumoniaFryam Bells100% (1)
- Addisons Disease MSN ReportDocument16 pagesAddisons Disease MSN ReportFryam BellsNo ratings yet
- PN303 Brief Psychotic DisorderDocument8 pagesPN303 Brief Psychotic DisorderFryam BellsNo ratings yet
- MSN 303fracture by Ann Pryam BagongonDocument22 pagesMSN 303fracture by Ann Pryam BagongonFryam BellsNo ratings yet
- Schizophrenia PN302Document23 pagesSchizophrenia PN302Fryam BellsNo ratings yet
- Types of Bone Fractures and Clinical ManifestationsDocument10 pagesTypes of Bone Fractures and Clinical ManifestationsFryam BellsNo ratings yet
- Liver Cirrhosis My Fisrt CP in MRH :-)Document32 pagesLiver Cirrhosis My Fisrt CP in MRH :-)Fryam BellsNo ratings yet
- Biochemistry QuizDocument28 pagesBiochemistry Quizsanjviews100% (3)
- 1.4 The Lymphatic System: Prepared By: Ling Mei TengDocument15 pages1.4 The Lymphatic System: Prepared By: Ling Mei TengJuliet LingNo ratings yet
- Anatomy and Physiology-REVIEWER-Practical ExamDocument12 pagesAnatomy and Physiology-REVIEWER-Practical ExamDeity Ann ReuterezNo ratings yet
- Top Knife - Cutted - Top PDFDocument238 pagesTop Knife - Cutted - Top PDFIvanKazaiev100% (1)
- Bfhi-Session-5-How Breastfeeding WorksDocument16 pagesBfhi-Session-5-How Breastfeeding Worksreema arshadNo ratings yet
- The Integumentary SystemDocument11 pagesThe Integumentary SystemHamdy Pagilit DimaporoNo ratings yet
- T2DMDocument24 pagesT2DMXyra BadangayonNo ratings yet
- Anesthesia For The Pet Practitioner (2011 3rd Edition)Document216 pagesAnesthesia For The Pet Practitioner (2011 3rd Edition)Amela Dolittle Halilbašić100% (5)
- Ujian Sumatif 1 Biologi 2023Document12 pagesUjian Sumatif 1 Biologi 2023Siti Nor AishahNo ratings yet
- Meridians and Points PDFDocument35 pagesMeridians and Points PDFHamdon Hamad100% (9)
- CHAPTER SUMMARY-opiod AnalgesicDocument9 pagesCHAPTER SUMMARY-opiod AnalgesicNuttiya WerawattanachaiNo ratings yet
- Uji Aktivitas Antioksidan Ekstrak Etanol 70% Bunga Telang (Clitoria TernateaL) Dari Daerah Sleman Dengan Metode DPPHDocument7 pagesUji Aktivitas Antioksidan Ekstrak Etanol 70% Bunga Telang (Clitoria TernateaL) Dari Daerah Sleman Dengan Metode DPPHAnastasia FebruestiNo ratings yet
- Chapter 3 Science Form 4Document30 pagesChapter 3 Science Form 4Shafie BuyaminNo ratings yet
- Cell Cycle Lesson PlanDocument4 pagesCell Cycle Lesson PlanJustine Pama94% (17)
- Comprehensive Review of Temporal Lobe EpilepsyDocument36 pagesComprehensive Review of Temporal Lobe Epilepsyyohanes0gadiNo ratings yet
- Sri Padmavathi Medical College Hospital: APPLICATIONS Are INVITED For The Following Post - 2013-14Document3 pagesSri Padmavathi Medical College Hospital: APPLICATIONS Are INVITED For The Following Post - 2013-14Birupakshya RoutNo ratings yet
- Chlorhexidine - An Antiseptic in PeriodonticsDocument4 pagesChlorhexidine - An Antiseptic in PeriodonticsInternational Organization of Scientific Research (IOSR)No ratings yet
- Lecture 8 - 30.12.2022Document17 pagesLecture 8 - 30.12.2022Adnan Mohammad Adnan HailatNo ratings yet
- Pharmacology Nursing ReviewDocument19 pagesPharmacology Nursing Reviewp_dawg50% (2)
- Electrolyte Imbalance 1Document3 pagesElectrolyte Imbalance 1Marius Clifford BilledoNo ratings yet
- Nutritional Management of High Output Enterocutaneous FistulaDocument2 pagesNutritional Management of High Output Enterocutaneous FistulaAfra AmiraNo ratings yet
- Overview of Complications Occurring in The Post-Anesthesia Care UnitDocument14 pagesOverview of Complications Occurring in The Post-Anesthesia Care UnitShahabuddin ShaikhNo ratings yet
- Amino Acid Sequences Reveal Evolutionary RelationshipsDocument6 pagesAmino Acid Sequences Reveal Evolutionary RelationshipsAbby Gail DigalNo ratings yet
- Nicotrol InhalerDocument19 pagesNicotrol InhalerdebysiskaNo ratings yet
- CorneaDocument41 pagesCorneaNikhil KorripatiNo ratings yet
- Branches of ZoologyDocument3 pagesBranches of ZoologyVivek Morya100% (1)
- January 2016 (IAL) QP - Unit 1 Edexcel Biology A-LevelDocument24 pagesJanuary 2016 (IAL) QP - Unit 1 Edexcel Biology A-LevelkirthikaNo ratings yet
- Poster 10 NLS 01 01 ENG V20100927 PDFDocument1 pagePoster 10 NLS 01 01 ENG V20100927 PDFAndy XiaoNo ratings yet
- How Can We Use Neurotransmitters in Emotion and Reward System To Study DepressionDocument22 pagesHow Can We Use Neurotransmitters in Emotion and Reward System To Study DepressionGlobal Research and Development ServicesNo ratings yet
- q3 Sci10 Unit1 Feedback MechanismsDocument125 pagesq3 Sci10 Unit1 Feedback MechanismsIvann EboraNo ratings yet