Professional Documents
Culture Documents
023 Evaluation of The Sysmex UF-100 Automated
Uploaded by
blanket_thOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
023 Evaluation of The Sysmex UF-100 Automated
Uploaded by
blanket_thCopyright:
Available Formats
Clinical Chemistry 44:1 9295 (1998)
Hematology
Evaluation of the Sysmex UF-100 automated urinalysis analyzer
Jonathan Ben-Ezra,* Linda Bork, and Richard A. McPherson
Urinalysis is a high-volume procedure that currently requires significant labor to examine microscopic sediment. We evaluated the Sysmex UF-100 automated urinalysis analyzer for performing this task. Instrument accuracy was assessed by comparing continuous counts of microscopic elements from the UF-100 with ranges of cells (per low-power field or high-power field) from manual microscopy performed on centrifuged urines. Counts showed good agreement between methods (gamma statistic: 0.880 0.970) for all microscopic elements in 252 urine samples. Within-run imprecision of cell counts expressed as CV (mean cell count/ L) was for erythrocytes (RBC) 31% (5), 18% (50), 2.4% (800); for leukocytes (WBC) 14% (10), 11% (100), 8.5% (400); for squamous epithelial cells (SEC) 18% (5), 12% (30), 7.0% (100); for casts 45% (1), 17% (4); for bacteria 212% (entire range of 40 2500). Between-run imprecision on qualitycontrol cell suspensions expressed as CV (mean cell count/ L) was for RBC 6.1% (50), 2.7% (256); for WBC 26.9% (54), 4.9% (228). Cells counted on dilution were 99.1% of expected for RBC, 102.0% for WBC, and 121.8% for bacteria. Carryover was <0.04% for RBC, <0.03% for WBC, <0.14% for SEC, <0.29% for bacteria. We conclude that the UF-100 can automatically perform reliable quantitative microscopic urinalysis in batches without operator interaction. The microscopic analysis of urine sediment provides essential information to clinicians about disease states in patients. Unfortunately, it lacks precision and has wide interobserver variability [1 4]. Moreover, it is a very labor-intensive procedure, adding greatly to the cost of providing laboratory services [5]. In the attempt to automate the process of microscopic urinalysis, image-based analysis systems have been developed [1, 3, 4, 6, 7]. However, even though these image-based automated systems offer increased speed of throughput and precision, there is still the need for an operator to visually inspect images of cells and casts as the sample is processed by the instrument; this severely limits their usefulness in terms of freeing technician time to perform other tasks within the laboratory. Therefore, the need for a truly walkaway microscopic urine analyzer is great. To this end, we evaluated the UF-100 (Sysmex Corp.) automated urine analyzer, a flow cytometer-based walkaway instrument that performs automated microscopic urinalysis.
Materials and Methods sysmex uf-100
The Sysmex UF-100 is an automated analyzer that performs a microscopic urinalysis by flow cytometry. In brief, after identifying the specimen by its bar code, the UF-100 aspirates 800 L of urine and performs the analysis. Cells, bacteria, and casts are measured by electrical impedance for volume, forward light-scatter for size, and by fluorescent dye for nuclear and cytoplasmic characteristics. The cells and formed elements are categorized in multidimensional space on the basis of their size, shape, volume, and staining characteristics. The results are displayed in scattergrams on a screen, and a hard copy of the results may be obtained. Problematic specimens are identified for manual microscopic urinalysis. Although the instrument does not have chemical analysis capabilities, it can be electronically linked to an automated strip-reader to generate an integrated report; in this study, all urine samples were analyzed chemically on a different instrument (data not shown).
materials and methods
We studied 252 freshly collected urine samples submitted for diagnostic urinalysis to our laboratory in a tertiarycare university hospital. After the routine diagnostic microscopic urinalysis was performed, the samples were analyzed the same day on the UF-100 analyzer; the use of such discarded material has been approved by our institutions IRB panel. To reduce interobserver variability, the same technologist performed all the microscopic urinaly-
Department of Pathology, Virginia Commonwealth University/Medical College of Virginia, Richmond, VA. *Address correspondence to this author at: Department of Pathology, Medical College of Virginia, P.O. Box 980250, Richmond, VA 23298-0250. Fax 804-828-2812; e-mail JBENEZRA@HSC.VCU.EDU. Received June 9, 1997; revision accepted August 25, 1997.
92
Clinical Chemistry 44, No. 1, 1998
93
ses with the same microscope, using the KOVA system (Hycor Biomedical) [8]. The areas of a low-power field (LPF) and high-power field (HPF) were determined with a measured scale to be able to correlate the cells or particles seen in a microscopic field (usually measured as cells or particles/LPF or HPF) with the quantitative results of the UF-100, which are provided in units of cells (or particles)/ L.1 Between-run quality-control samples consisted of suspensions of particles, provided by the manufacturer, in the sizes of bacteria, erythrocytes (RBCs), leukocytes (WBCs), and squamous epithelial cells (SECs). Within-run imprecision was determined by analyzing specimens with various concentrations of RBCs, WBCs, SECs, and bacteria 1220 times (usually 20) each on the UF-100 analyzer. Linearity was determined by analyzing in triplicate specimens and their dilutions of 1:2, 1:4, 1:5, 1:10, 1:20, and 1:40; the slope, intercept, and proportion of measured value to expected value were determined with EP-Evaluator (Rhoads). Carryover analysis was performed by analyzing the specimen in triplicate, followed by three blank specimens; the percent carryover was determined by the formula: Carryover (blank 1 blank 3)/(specimen 3 blank 3)
tive results (5 RBC/HPF 26 RBC/ L), the two methods differed significantly (McNemar test, P 0.00001). As can be seen from the Table, the UF-100 identified more RBCs in the samples than did microscopic urinalysis; this is most likely due to incomplete pelleting of the sediment for manual urinalysis, as well as the nonstandardization of cell resuspension after centrifugation. For the WBC data (Table 2), the gamma was 0.970. Analyzing the data by clinical positive vs negative results (5 WBC/HPF 26 WBC/ L), we again found significant differences between methods (P 0.00001). For the SEC data (Table 3), the gamma was 0.880. With results categorized by clinical positive vs negative (5 SECs/LPF 1.95 SECs/ L), the methods differed (McNemar test, P 0.00001). Samples in which the UF-100 overcalled epithelial cells contained casts and Trichomonas organisms. The protein in these samples most likely caused WBCs to aggregate, resulting in a possibly falsely high SEC count. The UF-100 detected many types of casts, including hyaline, granular, and cellular casts. For these data (Table 4), the gamma was 0.880. Analyzing the data by clinical positive vs negative results (1 cast/LPF 0.39 casts/ L), we found significant differences between the two methods (McNemar test, P 0.00001).
Statistical analysis, including the gamma statistic [9] for measuring correlation and the McNemar test for measuring change in the distribution of two dichotomous variables by the 2 test, was performed by using SPSS for Windows. Gamma is a measure of association between two variables measured on an ordinal level, and can be thought of as the probability that a random pair of observations is concordant minus the probability that the pair is discordant, assuming the absence of ties. Gamma is symmetric and ranges between 0 and 1.
Table 2. Comparison of automated and manual WBC counts.
Automated (UF-100), cells/ L Manual, cells/HPF 05 520 2050 >50
262 105262 26105 026
9 52 101
5 37 9 2
8 5
24
Results comparison with manual results
For RBC data (Table 1), the gamma statistic was 0.963. When we analyzed the data as clinical positive vs nega-
Table 3. Comparison of automated and manual SEC counts.
Automated (UF-100), cells/ L Manual, cells/LPF 05 520 2050 50100 >100
Table 1. Comparison of automated and manual RBC counts.
Automated (UF-100), cells/ L Manual, cells/HPF 05 520 2050 50100 >100
39 19.539 7.819.5 1.957.8 01.95 11
3 1 3 20 19
9 14 50 27 3
13 22 6 1
15 8 1
38 1 1
524 262524 105262 26105 026
1 1 5 36 162
2 7 4
1 9 2 1
3 1 1
Table 4. Comparison of automated and manual cast counts.
Automated (UF-100), cells/ L Manual, cells/LPF 01 15 510 1020 >100
1 Nonstandard abbreviations: LPF, low-power field; HPF, high-power field; RBC, erythrocyte; WBC, leukocyte; and SEC, squamous epithelial cell.
7.8 3.907.8 1.953.90 0.391.95 00.39
4 5 51 131
4 9 9 2
6 3 3 1
1 3
7 1 2 2
94
Ben-Ezra et al.: UF-100 urine analyzer
precision
Within-run CVs for the RBC analysis are shown in Table 5. The CV ranged from 33% for low numbers of RBCs (5 RBCs/ L) to 3% at RBC concentrations 660/ L. Between-run precision was 6% at a measured mean of 50 RBC/ L and 2.7% at a measured mean RBC of 256/ L. Within-run precision for the WBC analysis is shown in Table 5. The CV ranged from 24% for low numbers of WBCs (4 WBCs/ L) to 6% at a WBC count of 853/ L. Between-run precision was 27% at 54 WBC/ L and 4.9% at a WBC of 228/ L. Within-run precision ranged from 24% at 3.42 SECs/ L to 2.9% at 180 SECs/LPF. Between-run precision was 9.1% at 22 SECs/LPF and 7.5% at 88 SECs/LPF. Within-run precision for casts varied from 75% for samples with 0.42 casts/ L to 17% for samples with 4.6 casts/ L. The within-run CVs for bacterial counts (Table 5) was 212% over the concentration of bacteria tested. Betweenrun CV was 29% at 54 bacteria/ L, 37% at 60 bacteria/ L, and 26% at 146 bacteria/ L.
any of the samples, demonstrating that the carryover was not systematic.
Discussion
Manual analysis of urine sediment, although clinically useful, is fraught with methodological problems. At least 11 different factors may contribute to imprecision in manual urinalysis [1], ranging from centrifugation to the different interpretation of a cell or cast in a urine sediment by different technologists [2]. In addition, the process is time consuming, requiring approximately 6 min of technologist time per specimen [5]. To this end, there have been attempts to automate the process, thereby improving accuracy, precision, and throughput. The Yellow IRIS urinalysis instrument has automated the microscopic evaluation of urine sediment. Several studies have demonstrated that it has increased precision over routine manual urinalysis, and that it can detect more abnormalities than conventional microscopy [1, 3, 4, 6, 7]. However, a technologist must be physically present at the instrument to characterize events, and some technologist interpretation of images is required, thus leading to imprecision and inaccuracy. The UF-100 instrument analyzes urine cells and particles on the basis of flow cytometric principles, analogous to the manner by which modern hematology analyzers perform complete blood and differential cell counts. The UF-100 analyzer in this study detected more RBCs, WBCs, and SECs than did manual microscopy; similar findings have also been reported for the Yellow IRIS [1]. This probably represents true detection of cells not identified by manual microscopy, since routine urinalysis has centrifugation, decantation, and resuspension steps that are either incomplete or lead to cellular loss and lysis. Nonetheless, agreement between the manual and UF-100 methods for these cellular elements was excellent (gamma 0.88 0.97). Samples in which the UF-100 overcalled epithelial cells contained casts and Trichomonas organisms. The protein in these samples possibly caused WBCs to clump, resulting in a possibly falsely high SEC count. Detection of casts with the UF-100 was less robust than was the detection of cellular elements; this has also been seen with the Yellow IRIS [6], and may be due to differences in the volume of urine sample analyzed. We chose not to evaluate accuracy of bacteria detection, since the gold standard, quantifying bacterial counts in culture, measures something qualitatively different, live bacteria, from what the UF-100 urine analyzer measures, live and dead bacterial particles. This is a limitation of all automated urinalysis analyzers [10]. Nonetheless, the UF-100 flags the presence of casts, crystals, and bacteria, alerting the laboratory to their presence and the need to characterize them further under the microscope. Automated urinalysis performed by the UF-100 displayed good precision for analyzing cellular elements, bacteria, and casts; the CVs were much less than those
linearity
Dilutions of urine samples were made as described in Materials and Methods. For casts, dilutions of 1:2 and 1:4 were made from a sample with 18 casts/ L, and the specimens were analyzed in triplicate. For samples with RBC concentrations of 3864 to 15 956 cells/ L, the measured values were 87105% of expected. For three samples with WBC concentrations of 5698 to 5735 cells/ L, values were 92112% of expected. For bacteria (two samples), results were 111% (at 1809 cells/ L) and 133% (4433 cells/ L) of expected, and for casts (one sample) 106%.
carryover
Carryover studies were performed on four urine samples of various RBC, WBC, SEC, cast, and bacterial counts. Carryover ranged from 0.13% to 0.04% for RBC of 13 to 2404 cells/ L, 0.62% to 0.03% for WBC counts of 12 to 855 cells/ L, 1.6% to 0.14% for SEC of 3.0 to 72 cells/ L, 0.00% to 0.44% for 0.26 to 28 casts/ L, and 0.23% to 0.29% for bacterial counts of 277 to 2744 cells/ L. These results show that no substantial carryover was detected in
Table 5. Imprecision of results of UF-100 analyzer.
Mean cell count/ L CV range, %
RBC
WBC
Bacteria
510 1060 200875 520 70200 200900 3555 200600 10002500
2533 1338 1.47.7 1124 716 2.322 3.912 1.86.7 3.77.7
Clinical Chemistry 44, No. 1, 1998
95
reported historically for manual urinalysis [1, 3, 4], and are comparable with those seen with other automated instruments. Moreover, the assays were linear over clinically useful ranges, and no carryover was found with the UF-100 analyzer for the analytes measured. Comparison of the UF-100 with manual microscopy, the gold standard, is somewhat difficult, since this standard is somewhat tarnished by several methodological steps that lead to imprecision and inaccuracy [1, 2]. Our studies show that the UF-100 urine analyzers results are comparable with those of manual microscopy and published reports of the performance of the Yellow IRIS urine analyzer. In addition, counts of cellular elements with the UF-100 are comparable with those obtained on unspun urines analyzed under the microscope with a hemocytometer (manuscript in preparation). We conclude that the UF-100 can perform accurate and precise quantification of microscopic elements in urine with little or no operator interaction.
References
1. Carlson DE, Statland BE. Automated urinalysis. Clin Lab Med 1988;8:449 61. 2. Winkel P, Statland BE, Jorgenson J. Urine microscopy: an illdefined method examined by a multifactorial technique. Clin Chem 1974;20:436 9. 3. Roe CE, Carlson DA, Daigneault RW, Statland BE. Evaluation of the Yellow IRIS. An automated method for urinalysis. Am J Clin Pathol 1986;86:6615. 4. Deindorfer FH, Gangwer JR, Laird CW, Ringold RR. The Yellow IRIS urinalysis workstationthe first commercial application of automated intelligent microscopy. Clin Chem 1985;31:14919. 5. Manual for laboratory workload recording method. Skokie, IL: College of American Pathologists, 1984:140. 6. Elin RJ, Hosseini JM, Kestner J, Rawe M, Ruddel M, Nishi HH. Comparison of automated and manual methods for urinalysis. Am J Clin Pathol 1986;86:7317. 7. Wargotz ES, Hyde JE, Karcher DS, Hitlan J-P, Wilkinson DS. Urine sediment analysis by the Yellow IRIS automated urinalysis workstation. Am J Clin Pathol 1987;88:746 8. 8. McGinley M, Wong LL, McBride JH, Rodgerson DO. Comparison of various methods for the enumeration of blood cells in urine. J Clin Lab Anal 1992;6:359 61. 9. Goodman LA, Kruskal WH. Measures of association for crossclassification. J Am Stat Assoc 1954;49:732 64. 10. Poropatich CO, Mendoza SM, Hitlan JJ, Wilkinson DS. Inconsistent detection of bacteriuria with the Yellow IRIS automated urinalysis workstation. Lab Med 1988;19:499 501.
We acknowledge the assistance of the Sysmex Corporation, which provided technical assistance, control material, and a stipend for evaluation of the UF-100 urine analyzer.
You might also like
- 2014 Body Code Client Information PDFDocument7 pages2014 Body Code Client Information PDFkrug100% (1)
- Use of Fresh Blood For Quality Control: Erythrocyte Sedimentation RateDocument6 pagesUse of Fresh Blood For Quality Control: Erythrocyte Sedimentation RateTriana AmaliaNo ratings yet
- The Chemical ImbalanceDocument70 pagesThe Chemical ImbalancebredabredaNo ratings yet
- HOHF Witch of The Wilderlands VsubhaDocument30 pagesHOHF Witch of The Wilderlands VsubhaDom100% (1)
- Leadership Development PlanDocument5 pagesLeadership Development Planapi-262531856No ratings yet
- Portfolio Template for Diploma in Occupational MedicineDocument11 pagesPortfolio Template for Diploma in Occupational MedicineChengyuan ZhangNo ratings yet
- Analytical Method Validation of Clopidogrel Tablets BR HPLCDocument48 pagesAnalytical Method Validation of Clopidogrel Tablets BR HPLCAman ThakurNo ratings yet
- Automated Urine Sediment AnalyzerDocument5 pagesAutomated Urine Sediment AnalyzerCarolinaAngelaNo ratings yet
- Letter To The Editor: Comparison Between Automated and Microscopic Analysis in Body Fluids CytologyDocument3 pagesLetter To The Editor: Comparison Between Automated and Microscopic Analysis in Body Fluids CytologybalkisNo ratings yet
- Safely Reducing Manual Urine Microscopy Analyses by Combining Urine Flow Cytometer and Strip ResultsDocument7 pagesSafely Reducing Manual Urine Microscopy Analyses by Combining Urine Flow Cytometer and Strip ResultsFearless AngelNo ratings yet
- 420-Article Text-1407-1-10-20130601Document5 pages420-Article Text-1407-1-10-20130601Laboratorium RS BELLANo ratings yet
- Optimization of Laboratory Workflow in Clinical Hematology Laboratory With Reduced Manual Slide Review: Comparison Between Sysmex XE-2100 and ABX Pentra DX120Document8 pagesOptimization of Laboratory Workflow in Clinical Hematology Laboratory With Reduced Manual Slide Review: Comparison Between Sysmex XE-2100 and ABX Pentra DX120Marice Ferrufino SchmidtNo ratings yet
- Diagnosis of Bacteriuria and Leukocyturia by Automated Flow Cytometry Compared With Urine CultureDocument7 pagesDiagnosis of Bacteriuria and Leukocyturia by Automated Flow Cytometry Compared With Urine CultureAriHendraWijayantiNo ratings yet
- Platelet Counting by The Coulter LH 750, Sysmex XE 2100Document7 pagesPlatelet Counting by The Coulter LH 750, Sysmex XE 2100blanket_thNo ratings yet
- Control Charts in Clinical LabsDocument8 pagesControl Charts in Clinical LabsLuisNo ratings yet
- Veterinary Clinical PathologyDocument15 pagesVeterinary Clinical Pathologypand00raNo ratings yet
- 10 0000@www Jrheum Org@32@5@828Document5 pages10 0000@www Jrheum Org@32@5@828Yasser AlghrafyNo ratings yet
- Comprehensive Comparison of Five Top Hematology AnalyzersDocument15 pagesComprehensive Comparison of Five Top Hematology Analyzersmy accountNo ratings yet
- Science: Assessment of The Reliability of The Sysmex XE-5000 Analyzer To Detect Platelet ClumpsDocument6 pagesScience: Assessment of The Reliability of The Sysmex XE-5000 Analyzer To Detect Platelet ClumpsnivmastNo ratings yet
- Lmy 030Document7 pagesLmy 030Tuan NguyenNo ratings yet
- Evaluation of The Performance of Sysmex XN-3100 Automated Hematology Analyzer Regarding The Sysmex XE-2100 and Microscopic ExaminationDocument9 pagesEvaluation of The Performance of Sysmex XN-3100 Automated Hematology Analyzer Regarding The Sysmex XE-2100 and Microscopic ExaminationbalkisNo ratings yet
- Clinical Chemistry and Laboratory Medicine (CCLM) Comparison of five a.._Document10 pagesClinical Chemistry and Laboratory Medicine (CCLM) Comparison of five a.._Rafat ElshemiNo ratings yet
- Evaluation of Urinalysis Parameters To Predict Urinary-Tract InfectionDocument3 pagesEvaluation of Urinalysis Parameters To Predict Urinary-Tract InfectionIsfahan MasulotNo ratings yet
- Clinical Biochemistry: E. Schapkaitz, S. RaburabuDocument7 pagesClinical Biochemistry: E. Schapkaitz, S. RaburabuMunawwar SaukaniNo ratings yet
- Sismex ManualDocument11 pagesSismex ManualDigo SomengNo ratings yet
- Performance Evaluation of The Body Fluid Mode On The Platform Sysmex XE-5000 Series Automated Hematology AnalyzerDocument9 pagesPerformance Evaluation of The Body Fluid Mode On The Platform Sysmex XE-5000 Series Automated Hematology AnalyzerbalkisNo ratings yet
- Utility - of - Scatterplot - Patterns - of - Automated - Hematology Analysers 2020Document6 pagesUtility - of - Scatterplot - Patterns - of - Automated - Hematology Analysers 2020tufis02No ratings yet
- Performance of new automated urine analyser UF-5000 vs manual methodDocument29 pagesPerformance of new automated urine analyser UF-5000 vs manual methodrild278111No ratings yet
- Comparison Between Manual Procedure and Automated For Determinant of Wbcs and PCV in Maternity and Labor Hospital in Karbala CityDocument3 pagesComparison Between Manual Procedure and Automated For Determinant of Wbcs and PCV in Maternity and Labor Hospital in Karbala Cityyousrazeidan1979No ratings yet
- Body Fluid Cell Counts by Automated MethodsDocument11 pagesBody Fluid Cell Counts by Automated MethodsntnquynhproNo ratings yet
- Evaluation of The Abbott CELL-DYN 4000 HematologyDocument10 pagesEvaluation of The Abbott CELL-DYN 4000 Hematologypasamuco473No ratings yet
- 2 Ijmpsapr20172Document6 pages2 Ijmpsapr20172TJPRC PublicationsNo ratings yet
- Evaluation of RDW-CV RDW-SD Math 1sd 2013Document8 pagesEvaluation of RDW-CV RDW-SD Math 1sd 2013Gregorio De Las CasasNo ratings yet
- Ok 1Document6 pagesOk 1cydolusNo ratings yet
- Briggs 2009Document13 pagesBriggs 2009anggaririnNo ratings yet
- Validacion de AgaDocument7 pagesValidacion de AgaSATURNONo ratings yet
- CQ HematoDocument8 pagesCQ HematoRizky Pratama NurhakimNo ratings yet
- 661 FullDocument2 pages661 FullTommy DamanikNo ratings yet
- Immature GranulocytesDocument10 pagesImmature Granulocytespieterinpretoria391No ratings yet
- Simple Operation, Easy As 1-2-3: Vetscan Hm5 Less Time, Less Sample, More Accuracy, More ReproducibilityDocument6 pagesSimple Operation, Easy As 1-2-3: Vetscan Hm5 Less Time, Less Sample, More Accuracy, More ReproducibilityglenniesamuelNo ratings yet
- 005 Performance Evaluation of The Sysmex XT-2000iDocument9 pages005 Performance Evaluation of The Sysmex XT-2000iblanket_thNo ratings yet
- Plateletcrit, Mean Platelet Volume, Platelet Distribution Width: Its Expected Values and Correlation With Parallel Red Blood Cell ParametersDocument4 pagesPlateletcrit, Mean Platelet Volume, Platelet Distribution Width: Its Expected Values and Correlation With Parallel Red Blood Cell ParametersSoumik SahaNo ratings yet
- Reference Value Evaluation of Urine Sediment in Indonesian Adult Population Using Automated Urine AnalyzerDocument7 pagesReference Value Evaluation of Urine Sediment in Indonesian Adult Population Using Automated Urine AnalyzerptfajarindahlestariNo ratings yet
- Semiquantitative, Fully Automated Urine Test Strip AnalysisDocument7 pagesSemiquantitative, Fully Automated Urine Test Strip AnalysisDewi PradnyaNo ratings yet
- Evaluation and Comparison of The New Mindray BC-6200 Hematology Analyzer With ADVIA 2120iDocument8 pagesEvaluation and Comparison of The New Mindray BC-6200 Hematology Analyzer With ADVIA 2120iGABRIELA HERRERANo ratings yet
- Automated Blood Cell AnalysisDocument5 pagesAutomated Blood Cell AnalysiswerfsdsfNo ratings yet
- RetikulositDocument4 pagesRetikulositFajar Tea JieNo ratings yet
- Jurnal Malaria TesDocument5 pagesJurnal Malaria TesMaya RustamNo ratings yet
- Labmed40 0227Document5 pagesLabmed40 0227Airell Takinan DumangengNo ratings yet
- UF 1000i Urine Flow CytometerDocument5 pagesUF 1000i Urine Flow CytometerHeinny FunezNo ratings yet
- Performance Evaluation of The Sysmex XP-300 in An Oncology Setting: Evaluation and Comparison of Hematological Parameters With The Sysmex XN-3000Document7 pagesPerformance Evaluation of The Sysmex XP-300 in An Oncology Setting: Evaluation and Comparison of Hematological Parameters With The Sysmex XN-3000Yojan Leo Irakurri PuenteNo ratings yet
- Estimating platelet counts: auto analyzer vs smear methodsDocument7 pagesEstimating platelet counts: auto analyzer vs smear methodsLaboratorium RS BELLANo ratings yet
- Reticulocyte Counting in ThalasemiaDocument6 pagesReticulocyte Counting in ThalasemiaSutjipto WijonoNo ratings yet
- Five-Part Hematology AnalyzerDocument78 pagesFive-Part Hematology Analyzerswaraj sharmaNo ratings yet
- New QuantitiesDocument6 pagesNew Quantities20100117 Bùi Thùy VyNo ratings yet
- Evaluation and Performance Characteristics of The Coagulation System ACL TOP Analyzer - HemosIL ReagentsDocument10 pagesEvaluation and Performance Characteristics of The Coagulation System ACL TOP Analyzer - HemosIL ReagentsEsther Jara GarcíaNo ratings yet
- White Paper CPD Sepsis AJCP 2005Document5 pagesWhite Paper CPD Sepsis AJCP 2005jtmchughNo ratings yet
- Platelet Estimation by Manual and AutomationDocument4 pagesPlatelet Estimation by Manual and AutomationKamran DawoodNo ratings yet
- An_Artificial_Intelligence-Assisted_Diagnostic_PlaDocument11 pagesAn_Artificial_Intelligence-Assisted_Diagnostic_Plahanrong912No ratings yet
- Study 2Document7 pagesStudy 2Suyash BagdeNo ratings yet
- Chapter 11 Clinical Laboratory InstrumentationDocument19 pagesChapter 11 Clinical Laboratory InstrumentationAnonymous 58LGc3No ratings yet
- 09 Platelet Count by Peripheral Smear and Automated Cell Counter PDFDocument4 pages09 Platelet Count by Peripheral Smear and Automated Cell Counter PDFanggaririnNo ratings yet
- Tropmed 82 412Document3 pagesTropmed 82 412OlpinNo ratings yet
- Manavi 2021Document5 pagesManavi 2021Diesnatalisfkunand67No ratings yet
- Estudo Hepasfera Versus BeadDocument6 pagesEstudo Hepasfera Versus BeadAlexandre Campos Moraes AmatoNo ratings yet
- 027 Use of The Haemopoietic Progenitor Cell Count of The SysmexDocument7 pages027 Use of The Haemopoietic Progenitor Cell Count of The Sysmexblanket_thNo ratings yet
- 019 Age-Dependent Reference Ranges For AutomatedDocument7 pages019 Age-Dependent Reference Ranges For Automatedblanket_thNo ratings yet
- 020 Evaluation of The Sysmex XT-2000iV Hematology Instrument ForDocument31 pages020 Evaluation of The Sysmex XT-2000iV Hematology Instrument Forblanket_thNo ratings yet
- 024 Evaluation of The Sysmex UF-1000i For The DiagnosisDocument6 pages024 Evaluation of The Sysmex UF-1000i For The Diagnosisblanket_thNo ratings yet
- 025 Automated UrinalysisDocument6 pages025 Automated Urinalysisblanket_thNo ratings yet
- 028 Improved Performance of The AutomatedDocument6 pages028 Improved Performance of The Automatedblanket_thNo ratings yet
- 026 Evaluation of The Sysmex UF-100 Urine Cell AnalyzerDocument4 pages026 Evaluation of The Sysmex UF-100 Urine Cell Analyzerblanket_thNo ratings yet
- 022 Leucocyte Differentiation With The XT-SeriesDocument6 pages022 Leucocyte Differentiation With The XT-Seriesblanket_thNo ratings yet
- 013 Estimated Platelet and Differential LeucocyteDocument8 pages013 Estimated Platelet and Differential Leucocyteblanket_thNo ratings yet
- 017 The New Hematology Analyzer Sysmex XE-2100Document6 pages017 The New Hematology Analyzer Sysmex XE-2100blanket_thNo ratings yet
- 022 Leucocyte Differentiation With The XT-SeriesDocument6 pages022 Leucocyte Differentiation With The XT-Seriesblanket_thNo ratings yet
- 012 Analysis of Reticulocyte Parameters On The Sysmex XEDocument8 pages012 Analysis of Reticulocyte Parameters On The Sysmex XEblanket_thNo ratings yet
- 016 A Method For Optimizing and Validating InstitutionDocument6 pages016 A Method For Optimizing and Validating Institutionblanket_thNo ratings yet
- 018 An Evaluation of The Performance of Sysmex XE-2100 inDocument7 pages018 An Evaluation of The Performance of Sysmex XE-2100 inblanket_thNo ratings yet
- 015 Performance of An Automated Immature GranulocyteDocument7 pages015 Performance of An Automated Immature Granulocyteblanket_thNo ratings yet
- 009the Automated Nucleated Red Cell Count On The Sysmex XE-2100Document5 pages009the Automated Nucleated Red Cell Count On The Sysmex XE-2100blanket_thNo ratings yet
- 014 Immature Granulocyte Measurement Using The SysmexDocument5 pages014 Immature Granulocyte Measurement Using The Sysmexblanket_thNo ratings yet
- Precision and Accuracy of The Leukocyte DifferentialDocument14 pagesPrecision and Accuracy of The Leukocyte Differentialblanket_thNo ratings yet
- Precision and Accuracy of The Leukocyte DifferentialDocument14 pagesPrecision and Accuracy of The Leukocyte Differentialblanket_thNo ratings yet
- 011 Evaluation of The Automated Immature Granulocyte CountDocument1 page011 Evaluation of The Automated Immature Granulocyte Countblanket_thNo ratings yet
- 010new Red Cell Parameters On The Sysmex XeDocument1 page010new Red Cell Parameters On The Sysmex Xeblanket_thNo ratings yet
- 002performance Evaluation of The Sysmex XE-2100™Document7 pages002performance Evaluation of The Sysmex XE-2100™blanket_thNo ratings yet
- 005 Performance Evaluation of The Sysmex XT-2000iDocument9 pages005 Performance Evaluation of The Sysmex XT-2000iblanket_thNo ratings yet
- 008the Technology of ReagentsDocument7 pages008the Technology of Reagentsblanket_thNo ratings yet
- Platelet Counting by The Coulter LH 750, Sysmex XE 2100Document7 pagesPlatelet Counting by The Coulter LH 750, Sysmex XE 2100blanket_thNo ratings yet
- 006the New Reticulocyte Parameter (RET-Y) of The SysmexDocument7 pages006the New Reticulocyte Parameter (RET-Y) of The Sysmexblanket_thNo ratings yet
- 004 Evaluation of Two Sysmex XE-2100 AnalyzersDocument7 pages004 Evaluation of Two Sysmex XE-2100 Analyzersblanket_thNo ratings yet
- 001 Potential Utility of The New Sysmex XE 5000Document6 pages001 Potential Utility of The New Sysmex XE 5000blanket_thNo ratings yet
- CCMP 2020 Batch Cardiovascular MCQsDocument2 pagesCCMP 2020 Batch Cardiovascular MCQsharshad patelNo ratings yet
- ParoxetineDocument12 pagesParoxetinemarwa ammarNo ratings yet
- Pivas 2018Document46 pagesPivas 2018Denny PaatNo ratings yet
- Pulmonary EmbolismDocument93 pagesPulmonary EmbolismRakesh PanchalNo ratings yet
- Click Here Click Here To View Optimized Website For Mobile DevicesDocument4 pagesClick Here Click Here To View Optimized Website For Mobile DevicesFirman SalamNo ratings yet
- Clabsi TeamDocument20 pagesClabsi Teamapi-344209032100% (1)
- ResumeDocument7 pagesResumeRonald Fuéntes EndómaNo ratings yet
- How To Avoid Medication ErrorsDocument2 pagesHow To Avoid Medication ErrorsLorenn AdarnaNo ratings yet
- Diatermo MB 122 and MB 160 Mono-Bipolar: Cautery & ElectrosurgeryDocument13 pagesDiatermo MB 122 and MB 160 Mono-Bipolar: Cautery & ElectrosurgeryDani Daniela100% (1)
- Chapter 3 PsychDocument12 pagesChapter 3 Psychred_gyrl9282No ratings yet
- DR Wong Teck WeeipadDocument2 pagesDR Wong Teck Weeipadtwwong68No ratings yet
- Depression in Today - BioDocument5 pagesDepression in Today - Bioapi-272648963No ratings yet
- Unit 2Document4 pagesUnit 2api-296199660No ratings yet
- Legumes - AnOverview PDFDocument6 pagesLegumes - AnOverview PDFMayuri JagtapNo ratings yet
- Audit of Barangay Health Centers in PhilippinesDocument26 pagesAudit of Barangay Health Centers in PhilippineskenvysNo ratings yet
- v1 High Sensitivity C-Reactive Protein HSCDocument2 pagesv1 High Sensitivity C-Reactive Protein HSCKhendy SugihartoNo ratings yet
- Medical Certificate Guidelines June 2012Document3 pagesMedical Certificate Guidelines June 2012wudthipanNo ratings yet
- Novo NordiskDocument2 pagesNovo NordiskSpotlightNo ratings yet
- RAV Admission Notice for Ayurveda CoursesDocument4 pagesRAV Admission Notice for Ayurveda CoursesBhargav KalalNo ratings yet
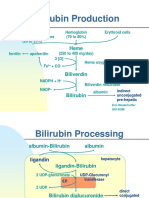
- Bilirubin Production: Hemoglobin (70 To 80%) Erythroid Cells Heme Proteins Myoglobin, Cytochromes (20 To 25%)Document5 pagesBilirubin Production: Hemoglobin (70 To 80%) Erythroid Cells Heme Proteins Myoglobin, Cytochromes (20 To 25%)Daffa Samudera Nakz DoeratipNo ratings yet
- Pre Employment Occupational Health FormDocument7 pagesPre Employment Occupational Health Formlinks2309No ratings yet
- Hypertension: Hozan Jaza MSC Clinical Pharmacy College of Pharmacy 10/12/2020Document81 pagesHypertension: Hozan Jaza MSC Clinical Pharmacy College of Pharmacy 10/12/2020Alan K MhamadNo ratings yet
- Diagnostic Imaging Equipment & Consumables Laser PrintersDocument5 pagesDiagnostic Imaging Equipment & Consumables Laser Printersnanu_gomezNo ratings yet
- Academica Science Journal PSYCHOLOGICA - No 2Document3 pagesAcademica Science Journal PSYCHOLOGICA - No 2Ciotea ValentinNo ratings yet