Professional Documents
Culture Documents
Mordida Abierta Anterior 1
Uploaded by
Javier SanzOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Mordida Abierta Anterior 1
Uploaded by
Javier SanzCopyright:
Available Formats
Available online at www.sciencedirect.
com
British Journal of Oral and Maxillofacial Surgery 48 (2010) 352355
Closure of the anterior open bite using mandibular sagittal split osteotomy
B. Bisase , P. Johnson, M. Stacey
Royal Surrey County Hospital, Egerton Road, Guildford, Surrey, GU2 7XX, United Kingdom Accepted 21 August 2009 Available online 16 September 2009
Abstract Anterior open bite is a common problem in orthognathic practice that confers functional and aesthetic handicaps on affected patients. Its management varies, and it is one of the most challenging disorders to treat. The orthodontic and surgical approach to the treatment of skeletal anterior open bite is still debated, and the results are controversial. The relapse rate is high with all the techniques in current use. The cause of relapse is multifactorial and one of the main factors is the type of osteotomy used. Over the last 30 years preference has moved from mandibular sagittal split osteotomy (MSSO) alone, to maxillary procedures only, or to bimaxillary operations, with maxillary procedures alone being thought to confer the best stability and predictability. The aim of this study was to evaluate the results of correction of anterior open bite with the MSSO immediately after operation, and 1 year postoperatively. 2009 The British Association of Oral and Maxillofacial Surgeons. Published by Elsevier Ltd. All rights reserved.
Keywords: Anterior open bite; Mandibular sagittal split osteotomy; Closure
Introduction Anterior open bite varies, and is one of the most challenging dentofacial deciencies to treat. The joint orthodontic and orthognathic surgical approach is controversial and results can be unpredictable.1 Relapse is multifactorial and can involve skeletal and dentoalveolar components. Orthodontic treatment involves extrusion of incisors or intrusion of molars. Dental stability after vertical orthodontic mechanics is unpredictable and is likely to relapse. Recent reports of intrusion of molars using skeletal anchorage are more encouraging, but to date reported series are small.2 One of the main causes of skeletal relapse may be the type of osteotomy. The type of skeletal xation may also have some inuence. Rigid internal xation confers more stability than intraosseous wire techniques.35 Other factors
Corresponding author at: 39 Greenhill Gardens, Merrow, Guildford, GU4 7HH, United Kingdom. Tel.: +44 7957312298. E-mail addresses: bbisase@doctors.org.uk (B. Bisase), paul.johnson200@ukonline.co.uk (P. Johnson).
include neuromuscular inuences on the repositioned jaws.6 Early attempts to close an anterior open bite with mandibular procedures were mainly segmental,7 but were soon superseded by posterior impaction of the maxilla at Le Fort I level as this was thought to be more stable.810 Proft et al. classied maxillary impaction as a highly stable movement.11 However, Lo and Shapiro examined the stability of maxillary operations after correction of anterior open bite and found that 25% of 40 patients had no incisal overlap 5 years and 10 months postoperatively.12 Recently, interest has been rekindled in re-establishing a place for mandibular surgery alone.6,13 Anticlockwise rotation of the mandible to close an anterior open bite offers certain advantages. In a class II case where mandibular advancement is also required it is possible to limit intervention to a single jaw, thereby avoiding the increased morbidity associated with a bimaxillary procedure. In addition, the possible adverse aesthetic effects of a maxillary procedure with posterior impaction can be avoided. In cases with retrogenia, anticlockwise rotation of the mandible results in increased prominence of the chin. A genioplasty may thereby be avoided. Oliveira and Bloomquist13 cited an
0266-4356/$ see front matter 2009 The British Association of Oral and Maxillofacial Surgeons. Published by Elsevier Ltd. All rights reserved.
doi:10.1016/j.bjoms.2009.08.018
B. Bisase et al. / British Journal of Oral and Maxillofacial Surgery 48 (2010) 352355
353
initial study carried out by Horwitz et al. In a preliminary evaluation of the long-term stability of mandibular sagittal split osteotomies (MSSO) to close anterior open bites. They found that after 4 years and 6 months only 2/20 cases studied had relapsed to a point where there was no incisor overlap. To date there are limited data, but what there are, are encouraging. The purpose of this study was to evaluate our results of correction of anterior open bite using the MSSO with rigid internal xation immediately postoperatively and 1 year later.
Patients and methods We made a retrospective review of records of 12 adult patients consecutively treated for anterior skeletal open bite with MSSO. All procedures were done by a single surgeon using Hunsuck and Dalpont modications. The inclusion criteria for analysis were: complete clinical records for a minimum of 1 year (including lateral cephalometry and study models); and rigid internal bicortical screw xation on each side. Data collected included patients age, sex, and preoperative malocclusion pattern including the degree of anterior open bite. The procedure, specic pattern of xation, and any immediate complications were also recorded. Exclusion criteria were: patients who sucked their thumbs when this was regarded as the cause of the anterior open bite; patients in whom the tongue was thought to be a contributory factor because of its size; and conditions that affected the temporomandibular joint (TMJ). Data were recorded from preoperative and postoperative records. These included clinical documentation and cephalometry immediately postoperatively, at the rst follow-up appointment (12 weeks), and at 1 year.
Twelve cases met the criteria, of which 4 were male and 8 were female, and mean age at operation 19 (range 1525) years. Patients presented with skeletal tendencies towards class II in 8/12 cases and towards class III in 2. The mean maxillomandibular angle was 37.6 with a range of 3047 . Vertical anterior open bite was 2 mm in 5/12, 4 mm in 5/12, and 5 mm in 2. Eleven of the 12 cases were xed with 3 mm 2.0 mm titanium bicortical positional screws on each side, and 1 with 4 screws on one side and 5 on the other using the same system. This case required removal of wisdom teeth at the same time. All 12 cases had class I incisal relations (overbite 12 mm) at the end of the operation, and at the rst surgical review(12 weeks postoperatively). At 1 year, 10/12 presented with a stable class I incisal relation similar to the immediate postoperative measurements. Two of the 12 cases presented with an edge-to-edge incisor relation. There was no relapse of anterior open bite, and no cases of condylar resorption at 1 year. Although there are too few patients in each group for statistical analysis of the correlation of the maxillomandibular angle and relapse of anterior open bite, it is noteworthy that the cases with higher angles (4347 , cases 1, 6 and 8, Table 1) each had a relapse of 1 mm at 1 year.
Discussion The main indication for treatment of an anterior open bite by posterior maxillary impaction is the presence of posterior maxillary vertical maxillary excess, which is common. About a third of patients who present with orthognathic concerns have vertical maxillary excess. It is also reported that about 60% of patients with it also have an open bite, or a tendency to an open bite.14 It follows that many patients who are operated on to correct anterior open bites may require maxillary surgery. Where the vertical and anteriorposterior position of the maxilla is within reasonable limits there is less of an indication to operate on the maxilla, except when it is thought to be the most stable technique to close an ante-
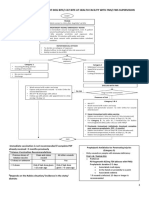
Results (Table 1) Fifteen patients were identied, but 3 were excluded because records were incomplete (n = 2) and one had possible ongoing condylar resorption that had been suspected preoperatively.
Table 1 Results. Case no. Skeletal pattern III III II II II II I I II II II II Maxillomandibular angle ( ) 47 33 32 35 42 43 33 44 34 30 40 39 Anterior open bite (mm) 5 4 2 2 4 4 2 5 4 2 2 4
Fixation screws (2.0) L/R 3/3 3/3 3/3 3/3 3/3 3/3 3/3 3/3 4/5 3/3 3/3 3/3
Overbite after operation (mm) Immediately 1 1 2 1 2 1 1 2 1 2 1 2 At 12 weeks 1 1 2 1 2 1 1 2 1 2 1 2 At 12 months 0 1 1 1 2 0 1 1 1 2 1 1
1 2 3 4 5 6 7 8 9 10 11 12
354
B. Bisase et al. / British Journal of Oral and Maxillofacial Surgery 48 (2010) 352355
rior open bite. Although many studies have reported better stability with a maxillary procedure, the patients are heterogeneous and include those with appreciable vertical maxillary discrepancies.15,16 Few compare or report on cases where the maxilla was in a favourable position without a posterior vertical maxillary extension. The height of the mandibular ramus and the clinical state of the condyles are factors only recently emphasised as useful contributors to aiding the decision about the choice of procedure.6 Patients with a short mandibular ramus, normal condyles, no sign of ongoing resorption, and a well positioned maxilla (no posterior maxillary excess) would lend themselves to an MSSO alone as the procedure of choice. There have been few publications about mandibular surgery alone, with the few studies published including sample sizes of only 1530.13,17 This may reect the limited number of cases that are appropriate for such a procedure, or may reect the blanket treatment selected by many, based on the heterogeneous case-mix previously analysed, which suggests universally more stability with maxillary surgery. The former explanation is exemplied by the small number of cases in our series, as only a few met the inclusion criteria. Our results suggest that in selected cases mandibular surgery alone is appropriate and allows a stable result. Studies that describe or compare mandibular anticlockwise rotational movements alone do not clarify the technique of sagittal split osteotomy, and whether this was conventional or modied. In particular, with reference to the posterior extension of the cut in the medial ramus, ensuring a split that allows part of the medial pterygoid to remain attached to the proximal segment and to stripping of the pterygomasseteric sling, medial pterygoid, and stylomandibular ligament from the distal segment.6 These manoeuvres during a modied medial ramus osteotomy (short split technique)8 reduce the risk that the medial pterygoid muscle may contribute to forces that encourage relapse when closing an anterior open bite with the mandible. Other factors thought to contribute to relapse (but to a lesser degree) are the stretching of nonmuscular soft tissue and neuromuscular activity. Both factors are thought to adapt early postoperatively rather than cause relapse. Various studies have suggested that rigid xation confers greater stability than other methods in the closure of anterior open bite.18 Most of these data, however, relate to xation with wire compared with mini-plates. It has been suggested that rigid xation using positional screws in the closure of an anterior open bite may confer better surgical stability than semirigid mini-plates, and was therefore the preferred method used by the surgeon in this series.13,15,18,19 Although maxillary osteotomy is done regularly with few complications, morbidity still exists and can be lifethreatening, in particular bleeding. In practice some patients who need closure of an anterior open bite may also require an increased prominence of the chin. This would necessitate advancement genioplasty if the correction of the anterior open bite was to be achieved by maxillary surgery only. Anticlock-
wise rotation of the mandible has the aesthetic advantage of addressing this decit, and avoids the risks and morbidity associated to advancement genioplasty as an additional procedure. Bimaxillary surgery, although advocated in the closure of anterior open bite, may present a higher risk of morbidity than either maxillary or mandibular surgery alone. Published evidence has recognised the risks of relapse with this procedure11,16 and means that care must be taken in calculating the denite need for double jaw surgery to optimise risk/benet for the patient. We suggest that patients who meet similar inclusion and exclusion criteria to those that we studied should be considered for correction by mandibular surgery alone to minimise such risks. Although there are few published reports, a growing numbers of surgeons are attempting and reporting this technique to close anterior open bite.6,13,17 The limitations in this study included the difculty of obtaining complete information about the degree of orthodontic preoperative decompensation, in particular worsening the overbite, and also limitations related to sample size and short follow-up (which should ideally be 2 and 5 years). These aspects will be addressed in a future prospective study.
Conclusion Our results suggest that the results following the closure of anterior open bites by mandibular anti-clockwise rotation are at least as stable as AOBs closed by maxillary impaction. We suggest that consideration should be given to the use of a mandibular procedure alone in the presence of certain conditions such as the existence of a normal maxilla, in Class II cases where mandibular advancement is also required and the presence of retrogenia where mandibular rotation can obviate the need for a genioplasty.
References
1. Denison TF, Kokich VG, Shapiro PA. Stability of maxillary surgery in openbite versus nonopenbite malocclusions. Angle Orthod 1989;59:510. 2. Erverdi N, Keles A, Nanda R. The use of skeletal anchorage in open-bite treatment: aacephalometic evaluation. Angle Orthod 2004;74: 38190. 3. Brammer J, Finn R, Bell WH, Sinn D, Reisch J, Dana K. Stability after bimaxillary surgery to correct vertical maxillary excess and mandibular deciency. J Oral Surg 1980;38:66470. 4. Hiranaka DK, Kelly JP. Stability of simultaneous orthognathic surgery on the maxilla and mandible: a computer-assisted cephalometric study. Int J Adult Orthodon Orthognath Surg 1987;2:193213. 5. Hoppenreijs TJ, Freihofer HP, Stoelinga PJ, Tuinzing DB, vant Hof MA, van der Linden FP, et al. Skeletal and dento-alveolar stability of Le Fort I intrusion osteotomies and bimaxillary osteotomies in anterior open bite deformities. A retrospective three-centre study. Int J Oral Maxillofac Surg 1997;26:16175. 6. Reyneke JP, Ferretti C. Anterior open bite correction by Le Fort I or bilateral sagittal split osteotomy. Oral Maxillofac Surg Clin North Am 2007;19:3218.
B. Bisase et al. / British Journal of Oral and Maxillofacial Surgery 48 (2010) 352355 7. Kloosterman J. Koeles osteotomy: a follow-up study. J Maxillofac Surg 1985;13:5963. 8. Epker BN, Fish L. Surgical-orthodontic correction of open-bite deformity. Am J Orthod 1977;71:27899. 9. Schmidt LP, Sailer H. Long-term results of surgical-orthodontic treatment of open bite deformity by a Le-Fort-I osteotomy. Swiss Dent 1991;12:27(29):312. 10. Swinnen K, Politis C, Willems G, De Bruyne I, Fieuws S, Heidbuchel K, et al. Skeletal and dento-alveolar stability after surgical-orthodontic treatment of anterior open bite: a retrospective study. Eur J Orthod 2001;23:54757. 11. Proft W, Turvey T, Phillips C. The hierarchy of stability and predictability in orthognathic surgery with rigid xation: an update and extension. Head Face Med 2007;3:21. 12. Lo F, Shapiro P. Effect of presurgical incisor extrusion on stability of anterior open-bite malocclusion treated with orthognathic surgery. Int J Adult Orthod Orthognath Surg 1998;13:2334. 13. Oliveira JA, Bloomquist DS. The stability of the use of bilateral sagittal split osteotomy in the closure of anterior open bite. Int J Adult Orthodon Orthognath Surg 1997;12:1018.
355
14. Reyneke JP, editor. Essentials of orthognathic surgery. Chicago: Quintessence; 2003. p. 2145. 15. Hoppenreijs TJ, Freihofer HP, Stoelinga PJ, Tuinzing DB. Stability of orthodontic-maxillofacial surgical treatment of anterior open bite deformities. Ned Tijdschr Tandheelkd 2001;108:1738. 16. Proft WR, Bailey LJ, Phillips C, Turvey TA. Long-term stability of surgical open-bite correction by Le Fort I osteotomy. Angle Orthod 2000;70:1127. 17. Reitzik M, Barer PG, Wainwright WM, Lim B. The surgical treatment of skeletal anterior open-bite deformities with rigid internal xation in the mandible. Am J Orthod Dentofacial Orthop 1990;97: 527. 18. Blomqvist JE, Ahlborg G, Isaksson S, Svartz K. A comparison of skeletal stability after mandibular advancement and use of two rigid internal xation techniques. J Oral Maxillofac Surg 1997;55: 56875. 19. Forssell K, Turvey TA, Phillips C, Proft WR. Superior repositioning of the maxilla combined with mandibular advancement: mandibular RIF improves stability. Am J Orthod Dentofacial Orthop 1992;102: 34250.
You might also like
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Patient Centered Pharmacology Tindall William N Sedrak Mona M Boltri John M SRG PDFDocument575 pagesPatient Centered Pharmacology Tindall William N Sedrak Mona M Boltri John M SRG PDFTedpwer100% (3)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- New Patient History FormDocument6 pagesNew Patient History Formعبدالله الكافNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Ridge Split Technique Using Piezosurgery - A Case ReportDocument6 pagesRidge Split Technique Using Piezosurgery - A Case ReportInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- Osteopathic Considerations in Systemic Dysfunction (2nd Ed)Document296 pagesOsteopathic Considerations in Systemic Dysfunction (2nd Ed)Natan Babek100% (1)
- Hospital DocumentsDocument17 pagesHospital DocumentsRaviraj PisheNo ratings yet
- Physiotherapy Guide for Respiratory & Cardiac Issues in Adults & ChildrenDocument1 pagePhysiotherapy Guide for Respiratory & Cardiac Issues in Adults & ChildrenAndrei Briceag100% (1)
- Biochemical Biomarkers in Alzheimer's DiseaseDocument150 pagesBiochemical Biomarkers in Alzheimer's DiseaseInternational Medical PublisherNo ratings yet
- Stress Ulcer Prophylaxis GuidelinesDocument4 pagesStress Ulcer Prophylaxis GuidelinesAzi Rifki NasutionNo ratings yet
- Detailed Lesson Plan in Mapeh 8 JoanneDocument9 pagesDetailed Lesson Plan in Mapeh 8 JoanneLANI JOY TABAMONo ratings yet
- Sas 3Document3 pagesSas 3Dummy AccountNo ratings yet
- Surgical Versus Medical Treatment of Drug-Resistant Epilepsy: A Systematic Review and Meta-AnalysisDocument10 pagesSurgical Versus Medical Treatment of Drug-Resistant Epilepsy: A Systematic Review and Meta-AnalysisSebastianNo ratings yet
- SIR Epidemic Model Explained: Susceptible, Infected, Recovered PopulationsDocument16 pagesSIR Epidemic Model Explained: Susceptible, Infected, Recovered Populationsmirast91No ratings yet
- Clinical Alert A Quick Reference To Adverse Clinical EventsDocument272 pagesClinical Alert A Quick Reference To Adverse Clinical EventsOmasNers100% (1)
- BMS 533 Case Study Factors and ConsequencesDocument14 pagesBMS 533 Case Study Factors and ConsequencesAhmad Nur AqmalNo ratings yet
- The Health Bank (THB) Connected Care Program A Pilot Study of Remote Monitoring For The Management of Chronic Conditions Focusing On DiabetesDocument5 pagesThe Health Bank (THB) Connected Care Program A Pilot Study of Remote Monitoring For The Management of Chronic Conditions Focusing On DiabetesInternational Journal of Innovative Science and Research TechnologyNo ratings yet
- ENGLISH SPM Section C 2Document4 pagesENGLISH SPM Section C 2Mohamad NuraizatNo ratings yet
- 1-The Etiology of Orthodontic ProblemsDocument47 pages1-The Etiology of Orthodontic ProblemsEzza RiezaNo ratings yet
- LIS 141 Report - Medical TermsDocument14 pagesLIS 141 Report - Medical TermsR.B. DavilaNo ratings yet
- Malaria PDFDocument28 pagesMalaria PDFKABERA RENENo ratings yet
- Chapter 11 Hospital Pharmacy Notes Complete Notes by Noteskarts Acc To ER20Document2 pagesChapter 11 Hospital Pharmacy Notes Complete Notes by Noteskarts Acc To ER20Mobeen AhmedNo ratings yet
- ScheduleDocument52 pagesSchedulerohitNo ratings yet
- Impact of Topical Steroids on Acanthamoeba Keratitis OutcomesDocument8 pagesImpact of Topical Steroids on Acanthamoeba Keratitis OutcomesDiana BaagilNo ratings yet
- HS 2212 Wa U5Document4 pagesHS 2212 Wa U5bnvjNo ratings yet
- Compensation Fy2018sDocument218 pagesCompensation Fy2018sJesse YoungbloodNo ratings yet
- Rincian Kewenangan Klinis Dokter Spesialis Anak: Congenital DisordersDocument6 pagesRincian Kewenangan Klinis Dokter Spesialis Anak: Congenital DisordersIMELDA ARCANNo ratings yet
- Protocol Posters SC CHCDocument16 pagesProtocol Posters SC CHCSandeep ShettyNo ratings yet
- Missing Women Revisited by Amartya SenDocument2 pagesMissing Women Revisited by Amartya SenDebashish BoseNo ratings yet
- MANAGING DOG/CAT BITES AT HEALTH FACILITYDocument5 pagesMANAGING DOG/CAT BITES AT HEALTH FACILITYleo89azman100% (1)
- Informed Consent - Laser Hair RemovalDocument4 pagesInformed Consent - Laser Hair RemovalAshraf AboNo ratings yet
- Uri Flush 3 Liquid Stones ProblemDocument4 pagesUri Flush 3 Liquid Stones ProblemSourabh KoshtaNo ratings yet