Professional Documents
Culture Documents
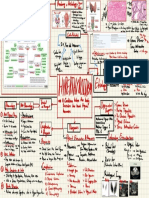
Circulatory
Uploaded by
Nida NidiOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Circulatory
Uploaded by
Nida NidiCopyright:
Available Formats
Dr.
Vince Scialli BSC 1086
REV. 12/22/06
BLOOD VESSELS ~ OVERVIEW
Blood vessels are the plumbing for the body Blood vessels are NOT rigid . . . they are dynamic structures Pulsate Constrict ~ vasoconstriction Relax ~ vasodilation
Proliferate ~ grow & invade ~ collateral circulation Blood vessels are a closed delivery system Start at left heart: End at right heart: Aorta > Arteries ~ carry O2 blood Veins > Vena Cava ~ carry CO2 blood
BLOOD VESSEL TYPES
ARTERIES > Large Arteries > Small Arteries > Arterioles Carry oxygenated blood away from heart ~ high O2 Branch Out ~ from big to small VEINS < Large Veins < Small Veins < Venules (small to large) Carry unoxygenated blood toward heart ~ high CO2 Merge together from small to big CAPILLARIES ~ contact tissue through capillary walls Only one cell layer thick for diffusion ~ endothelium Exchange O2 & CO2 between blood & tissue ~ O2/CO2
Blood Vessels & Circulation ~ Chapter 21~7/13/2011 1
Dr. Vince Scialli BSC 1086
BLOOD VESSEL WALL STRUCTURE Arteries & Veins ~ Three distinct layers
1.
Tunica intima ~ tunica interna ~ inside layer
Lines lumen of vessels ~ opening Endothelium ~ simple squamous & elastic tissue Continuous with endocardium Veins have flaps or valves that prevent back flow
2.
Tunica media ~ middle smooth muscle & elastic layer
Thick in arteries Thin in veins
Innervated by Sympathetic NS ONLY Adrenergic Stimulation > Vasoconstriction BP Cholinergic Stimulation > Vasodilation BP
Vasa Vasorum ~ blood vessels supplying wall of other blood vessels 3. Tunica externa ~ outside layer ~ collegen & elastic fibers Thin in arteries Thick in veins
Capillaries ~ composed of epithelial cells only ~ single layer
Tunica Interna ONLY
Blood Vessels & Circulation ~ Chapter 21~7/13/2011 2
Dr. Vince Scialli BSC 1086
CIRCULATORY PATHWAYS
ARTERIES ~ ARTERIAL SYSTEM Systemic arteries always carry oxygenated blood ~ O2 Pulmonary arteries always carry unoxygenated blood ~ CO2 Arterial walls thicker than veins Artery walls DO NOT contain valves ~ Veins contain valves Arteries vasoconstrict ~ Veins collapse BOTH Arteries & Veins can relax ~ vasodilate
Types of Arteries
1.
ELASTIC ARTERIES ~ AORTA & main branches
Called Conducting Arteries . . . Close to heart Thick Tunica Externa with some elastic fibers Conduct blood from heart to smaller arteries Elasticity allows expansion & contraction as blood volumes change NOT much resistance ~ due to large diameter DO NOT Vasoconstrict ~ due to thick externa walls Maintain constant blood flow ~ conducting
Blood Vessels & Circulation ~ Chapter 21~7/13/2011
Dr. Vince Scialli BSC 1086
2.
MUSCULAR ARTERIES ~ MOST of arterial system
Called Distributing Arteries ~ MOST COMMON Deliver blood to organs & skeletal muscle Small Diameter ~ more resistance > greater pressure Thick tunica media with less elastic tissue More vasoconstriction than larger elastic arteries Make up pressure points Can be pressed against bones to stop bleeding
3.
ARTERIOLES ~ smallest arteries
Resistance Vessels ~ increase/decrease resistance Deliver blood into capillary beds in tissue Very small diameter ~ Greatest resistance DILATION > decreases resistance > increases blood flow into capillaries ----> Lowers Blood Pressure CONSTRICTION > increases resistance > decreases flow into Capillaries ----> Increases Blood Pressure
Most important in regulating B.P. & flow to tissues !!!
Blood Vessels & Circulation ~ Chapter 21~7/13/2011
Dr. Vince Scialli BSC 1086
ARTERY STRUCTURE ABNORMALATIES Atheriosclerosis ~ thickening & hardening of artery walls
Plaque ~ cholesterol, low density lipoproteins ~ LDL Coronary Artery Disease ~ Cerebral Strokes ~ Thrombus
Aneurysm ~ bulge ~ thin weakened artery wall
Can be very dangerous if in brain or in large artery Can result in catastrophic blow out ~ fatal bleeding
Aortic Aneurysm ~ Fatal bleeding Brain Aneurysm ~ stroke due to hemorrhage
COMMON if associated with high blood pressure
CAPILLARIES
Microscopic in size ~ smallest of all blood vessels Diameter is slightly larger than diameter of a single RBC Very thinned wall ~ tunica interna only ~ endothelium only MOST body tissue has a rich capillary supply Exceptions: Tendons & Ligaments ~ DON T BLEED
Blood Vessels & Circulation ~ Chapter 21~7/13/2011
Dr. Vince Scialli BSC 1086
Capillaries allow exchange of O2/CO2, nutrients, & hormones between blood & tissue cells thru: Fenestrations ~ large pores allow large particle exchange CAPILLARY BEDS ~ Capillary Plexus ~ Microcirculation Network of capillaries ~ controls flow to tissues Allow blood to flow between arterioles & venules Artery O2 Arteriole O2 metarteriole O2 Vein CO2 Microcirculation Venule CO2 post capillary venule CO2 Capillary bed O2/CO2
Thorough fare channel Mixed Blood
Vasomotion ~ automatic vasoconstriction & vasodilation
Arterioles ~ Most important in regulating flow to tissues & control of blood pressure Blood entering capillary beds depends on BODY NEEDS Dilation of arterioles blood flow into capillaries BP Constriction of arterioles flow into capillaries BP
Causes pooling in various body parts at different times: Examples: Blood to digestive organs after a meal
6
Blood Vessels & Circulation ~ Chapter 21~7/13/2011
Dr. Vince Scialli BSC 1086
Blood to skeletal muscle after exercise Exercise after eating > muscle cramps
VENOUS SYSTEM
Systemic veins always carry unoxygenated blood ~ CO2 Pulmonary veins always carry oxygenated blood ~ O2
Types of Veins
1.
VENULES ~ very small ~ flow into veins
Extremely porous Fluid & white blood cells move from blood into tissue cells very easily ~ diffusion & pressure Ascites Edema Inflammation
2.
VEINS
Walls thinner but lumen larger than arteries Tunica externa ~ thick outer wall . . . Very thick near heart Tunica media ~ thin ~ smooth muscle ~ no constriction Expandable ~ Veins dilate & hold large volumes of blood Capacitance Vessels ~ expandable & can collapse Blood Reservoirs contain 65% of body blood volume Blood pressure is much lower in veins than arteries
Blood Vessels & Circulation ~ Chapter 21~7/13/2011
Dr. Vince Scialli BSC 1086
Farthest distance from heart ~ no constriction
VENOUS VALVES
In veins of limbs & extremeties . . . not in body cavities Veins can move blood against gravity ~ valves & muscles Valves prevent backward flow of blood ~ Prevents pooling
Valve Dysfunction: Vericose Veins & Hemorrhoids VASCULAR ANASTAMOSIS
Organs receive blood from more than one arterial source
Arterial anastamosis ~ artery to artery merge
By-Pass Surgery ~ coronary artery anastamosis
Venous anastamosis ~ veins to veins
Arterio-venous anastamosis ~ arterioles to venules Collateral Circulation ~ alternative supply of blood vessels Maintains blood supply to an area when main supply is cut or blocked by a clot or injury Part of the Healing process to improve blood supply Aerobic exercise Myocardial infarct Cerebral clot Occlusion of veins is rare ~ DO NOT become blocked
Blood Vessels & Circulation ~ Chapter 21~7/13/2011 8
Dr. Vince Scialli BSC 1086
Tissue death is rare as a result of venous occlusion
PHYSIOLOGY OF CIRCULATION
HEART ARTERIES = = PUMP CONDUITS RESISTANCE VESSELS EXCHANGE SITES O2/ CO2 CO2 O2
ARTERIOLES = CAPILLARIES = VEINS =
CONDUITS & BLOOD RESERVOIRS
FACTORS AFFECTING CIRCULATION
BLOOD FLOW . . . BLOOD PRESSURE . . . RESISTANCE
1.
BLOOD FLOW ~ ml/minute
VOLUME OF BLOOD FLOWING THROUGH A VESSEL, ORGAN, or ENTIRE CIRCULATION IN A GIVEN PERIOD VARIES WIDELY BASED ON ORGAN NEEDS Skeletal Muscles . . . Digestive Organs
2.
BLOOD PRESSURE ~ mmHg
FORCE PER UNIT AREA EXERTED ON THE WALL OF A BLOOD VESSEL BY ITS CONATINED BLOOD Defined: MEAN SYSTEMIC ARTERIAL PRESSURE IN THE LARGEST ARTERIES ~ NEAR THE HEART
Blood Vessels & Circulation ~ Chapter 21~7/13/2011
Dr. Vince Scialli BSC 1086
PRESSURE DIFFERENCE PROVIDES THE FORCE THAT KEEPS BLOOD MOVING . . . FROM HIGH PRESSURE TO LOW PRESSURE 3.
RESISTANCE
OPPOSITION TO BLOOD FLOW due to friction RESISTANCE -----> FLOW
Causes of Resistance:
1. Blood Viscosity ~ THICKNESS OR STICKINESS H2O & BLOOD PARTICULATES PLASMA PROTEIN & LIPIDS LOW RBCS ---> LOW VISCOSITY HIGH RBCS ---> HIGH VISCOSITY 2. Blood Vessel Length LONGER VESSELS ---> greater RESISTANCE FAT REQUIRES MORE & LONGER VESSELS WHICH INCREASES RESISTANCE 3. Blood Vessel Diameter . . . Most Significant Factor GREATER DIAMETER ----> LESS RESISTANCE SMALLER DIAMETER ----> MORE RESISTANCE Vasoconstriction . . . Vasodilation As radius decreases by ~ resistance increases 16X
Blood Vessels & Circulation ~ Chapter 21~7/13/2011 10
Dr. Vince Scialli BSC 1086
4.
Turbulance ~ increases resistance Fatty Plaques ~ atherosclerosis ~ cholesterol
Blood Vessels & Circulation ~ Chapter 21~7/13/2011
11
Dr. Vince Scialli BSC 1086
FACTORS AFFECTING BLOOD CIRCULATION
KNOW RELATIONSHIPS: VESSEL DIAMETER BLOOD FLOW VOLUME BLOOD FLOW VELOCITY BLOOD PRESSURE RESISTANCE ~ most dominant factor BLOOD PRESSURE ----> BLOOD FLOW VELOCITY
Vessel Diameter is the greatest resistance factor
RESISTANCE RESISTANCE KNOW VASODILATION VESSEL DIAMETER FLOW VOLUME RESISTANCE BLOOD PRESSURE FLOW VELOCITY
Blood Vessels & Circulation ~ Chapter 21~7/13/2011
----> ---->
BLOOD FLOW VOLUME BLOOD PRESSURE VASOCONSTRICTION VESSEL DIAMETER FLOW VOLUME RESISTANCE BLOOD PRESSURE FLOW VELOCITY
12
Dr. Vince Scialli BSC 1086
SYSTEMIC BLOOD PRESSURE ~ Circulatory Pressure
Heart PUMP generates the circulatory pressure Difference in pressure between the base of the AORTA & the entrance to the RIGHT ATRIUM via vena cava Average Circulatory Pressure ~ 100 mgHg Depends on: Arterial Pressure ~ 120 mmHg Capillary Pressure ~ 20 to 40 mmHg Venous Pressure ~ 0 to 20 mmHg
PRESSURE IS GREATEST CLOSE TO THE PUMP ~ Heart PRESSURE GRADIENT FLOW FROM HIGH TO LOW PUMP . . . CREATES FLOW
RESISTANCE . . . CREATES PRESSURE AORTA ARTERIES ARTERIOLES CAPILLARIES VENULES VEINS VENA CAVA
Blood Vessels & Circulation ~ Chapter 21~7/13/2011
~ ~ ~ ~ ~ ~ ~
120 mm Hg 120 mm Hg 60 mm Hg 40 - 20 mm Hg (most critical) 20 mm HG 10 mm Hg 1-5 mm Hg
13
Dr. Vince Scialli BSC 1086
RIGHT ATRIUM
ARTERIAL PRESSURE ~ BLOOD PRESSURE
It is what we Actually Measure in determining Blood Pressure Blood Pressure Dependent on TWO Factors 1. 2. ELASTICITY OF ARTERIES CLOSE TO HEART VOLUME OF BLOOD FORCED INTO ARTERIES
BLOOD PRESSURE RISES & FALLS WITH EACH BEAT . . . as measured in arteries nearest the heart
SYSTOLIC PRESSURE
PRESSURE produced in arteries AFTER each left ventricular contraction AVERAGE ~ 120 mm Hg
DIASTOLIC PRESSURE
PRESSURE remaining in AORTA & major ARTERIES during DIASTOLE ~ Ventricular filling /heart relaxed AORTIC SEMI-LUNAR VALVES CLOSED Prevents back flow into left ventricle Maintains a lower arterial pressure in diastole Keeps blood flowing when heart is not pumping AVERAGE ~ 80 mm Hg
Blood Vessels & Circulation ~ Chapter 21~7/13/2011 14
Dr. Vince Scialli BSC 1086
Normal blood pressure = 120/80 = Systolic/Diastolic
Blood Vessels & Circulation ~ Chapter 21~7/13/2011
15
Dr. Vince Scialli BSC 1086
PULSE PRESSURE SYSTOLIC minus DIASTOLIC PRESSURE
AVERAGE ~ 120mm Hg 80 mm Hg = 40mm Hg
Factors Increasing Pulse Pressure
INCREASED STROKE VOLUME ~ systolic pressure INCREASED CONTRACTILITY ~ systolic pressure ATHEROSCLEROSIS ~ resistance
MEAN ARTERIAL PRESSURE ~ The Real Pressure
AVERAGE PRESSURE THAT PROPELS BLOOD TO ALL TISSUE DURING CARDIAC CYCLE Lower than SYSTOLIC but higher than DIASTOLIC DIASTOLE lasts longer than SYSTOLE ~ 2/3 to 1/3 Know How to Calculate
MAP = Diastolic Pressure + 1/3 Pulse Pressure
EXAMPLE: Systolic pressure Diastolic pressure Pulse Pressure = = = 120 80 40
MAP = 80 + 40/3 = 93 mm Hg NOTE: BOTH MAP & PULSE PRESSURE DECREASES WITH INCREASING DISTANCE FROM THE HEART ---> systolic pressure
Blood Vessels & Circulation ~ Chapter 21~7/13/2011 16
Dr. Vince Scialli BSC 1086
CAPILLARY PRESSURE ~ Capillary Hydrostatic Pressure
BEGINNING CAPILLARY BED PRESSURE END CAPILLARY BED PRESSURE ~ ~
40 mm Hg 20 mm Hg
LOW CAPILLARY BED PRESSURE is DESIRABLE Capillary Walls very fragile ~ only one cell layer thick HIGH PRESSURE ----> RUPTURE Nose Bleeds ~ mixed O2/CO2 blood Capillaries very permeable ~ pushes fluid out of capillaries HIGH PRESSURE ----> EDEMA EDEMA ~ abnormal accumulation of fluid in tissue
Pulmonary Edema ~ LEFT SIDED FAILURE
Accumulation in lungs
Peripheral Congestion ~ edema/ascites
RIGHT SIDED FAILURE Accumulation in abdomen & tissue
Arterioles are most critical in regulating blood flow to tissues & controlling of blood pressure
Blood Vessels & Circulation ~ Chapter 21~7/13/2011
17
Dr. Vince Scialli BSC 1086
CAPILLARY BLOOD FLOW
BLOOD FLOW THROUGH CAPILLARY BEDS IS SLOW & INTERMITTENT . . . NOT STEADY FLOW IS FROM HIGH PRESSURE TO LOW PRESSURE
CAPILLARY EXCHANGE ~ Occurs by DIFFUSION
SOLUTES ~ Diffuse ~ HIGH TO LOW SOLUTE CONC. OXYGEN & CARBON DIOXIDE NUTRIENTS ~ AA, GLUCOSE, LIPIDS METABOLIC WASTES OTHER IONS ~ Na+, Ca+, K+ FLUID Moves ~ HIGH TO LOW PRESSURE LOW SOLUTE TO HIGH SOLUTE CONC. ~ via OSMOSIS DEPENDS ON:
HYDROSTATIC PRESSURE
PRESSURE INSIDE Capillary vs. CELL PRESSURE ~ pushes fluid out of capillaries into tissues
COLLOID OSMOTIC PRESSURE ~ Draws in H2O
Solutes carry H2O with them by OSMOSIS
Net Filtration Pressure ~ difference between net
(NFP)
Blood Vessels & Circulation ~ Chapter 21~7/13/2011
hydrostatic pressure & net osmotic pressure
18
Dr. Vince Scialli BSC 1086
VENOUS BLOOD PRESSURE
NO PULSATION ~ pressure too low ~ from 20 mmHg to 0 BEGINNING VENOUS PRESSURE ~ 20 mm Hg at capillaries END VENOUS PRESSURE ~ 0 mm Hg at Rt. Atrium
FACTORS AIDING VENOUS RETURN
Small PRESSURE GRADIENT = 20 to NEAR 0 mm Hg PRESSURE GRADIENT is too small to allow adequate return to heart by itself GRAVITY will allow some blood to flow from head & neck back to the heart while standing or sitting
Respiratory Pump ~ (pressure/volume relationship)
Breathing action sucks blood upward toward Heart Inhaling ---> increased abdominal pressure ---> squeezes local veins ---> forcing blood toward heart Inhaling ---> decreased chest cavity pressure --> thoracic veins to expand ---> speeds blood entry into right atrium
Muscular Pump
Skeletal muscle contraction ---> milking action of blood toward heart & prevents blood pooling Valves in extremity veins prevent flow back
Blood Vessels & Circulation ~ Chapter 21~7/13/2011 19
Dr. Vince Scialli BSC 1086
MAINTAINING BLOOD PRESSURE PHYSIOLOGIC FACTORS ~ INFLUENCE PRESSURE
CARDIAC OUTPUT BLOOD VOLUME PERIPHERAL RESISTANCE BLOOD PRESSURE = CARDIAC OUTPUT SV HR Volume X ----> ----> ----> BP BP BP
PERIPHERAL RESISTANCE Constriction Dilation Viscosity Vessel Length
NEURAL . . . HORMONAL . . . RENAL
CONTROLS
COMPENSATES for changes in Blood Pressure SHORT TERM CONTROL ~ Neural & Hormonal Mechanisms AFFECT PERIPHERAL RESISTANCE ~ VASOMOTOR Involves: Brain . . . Heart . . . Blood Vessels
LONG TERM CONTROL ~ Hormonal & Renal Mechanisms AFFECT BLOOD VOLUME & FLUID RETENTION Involves: Adrenals & Kidney
20
Blood Vessels & Circulation ~ Chapter 21~7/13/2011
Dr. Vince Scialli BSC 1086
SHORT TERM CONTROLS of Blood Pressure
AFFECTS ARE IMMEDIATE & SHORT-ACTING CONTROLS PERIPHERAL RESISTANCE by controlling vessel diameter 1.
NEURAL Mechanisms
Sympathetic NS controls peripheral resistance ALTERS VESSEL DIAMETER
Constriction ~ INCREASES blood pressure Dilation ~ LOWERS blood pressure
ALTERS BLOOD FLOW TO MEET TISSUE DEMANDS Digestion ~ shunts blood from skeletal muscle to digestive organs . . . cramps Exercise ~ shunts blood from digestive organs to skeletal muscle Skin Vasodilation ~ shunts blood from internal organs to skin to loose body heat Skin Vasoconstriction ~ shunts blood from skin to internal organs to retain heat
Blood Vessels & Circulation ~ Chapter 21~7/13/2011
21
Dr. Vince Scialli BSC 1086
NEURAL Control Mechanisms VASOMOTOR CENTER ~ MEDULLA OBLONGATA
Rapid REFLEX response to changes in blood pressure
Adrenergic Stimulation ----> Adrenaline Released
Increases heart rate & myocardial contraction Potent peripheral Vasoconstriction
HIGH BRAIN CENTERS ~ Hypothalamus ~ Cerebral Cortex
Blood Pressure changes sensed in Medulla >>> relays stimuli to higher brain centers >>> Gives us awareness ONLY . . . but NO conscious control Generalized fight or flight sympathetic response
CHEMORECEPTORS ~ chemical detectors
Detect blood & CSF changes in . . . O2, CO2, & H+ LOCATED IN: Aortic Bodies ~ in AORTIC ARCH Carotid Bodies ~ in NECK ARTERIES
O2, pH, CO2 ---> STIMULATES VASOMOTOR
Reflex Center in Medulla Increases Heart Rate & Myocardial Contraction & Vasoconstriction
Blood Vessels & Circulation ~ Chapter 21~7/13/2011 22
Dr. Vince Scialli BSC 1086
> > > INCREASES BLOOD PRESSURE BARORECEPTORS ~ detect ARTERIAL pressure changes LOCATED IN: CAROTID SINUSES AORTIC SINUSES An INCREASED Arterial Pressure ----> Triggers Reflex Stretches receptors ---> impulses to medulla oblongata ----> Sympathetic inhibiton ----> VASODILATION ----> Parasympathetic Stimulation ----> SLOWS HR Results in ----> LOWER Cardiac Output & LOWER BP A DECREASED Arterial Pressure ----> Triggers Reflex Stretches receptors ----> Impulses to medulla oblongata ----> Sympathetic Stimulation ----> Faster HR, increased myocardial contractility & consriction Results in ----> HIGHER Cardiac Output & HIGH BP
CAROTID SINUS REFLEX ~ ISCHEMIC REFLEX
Prevents fainting during rapid posture changes PROTECTS BLOOD SUPPLY TO BRAIN Stimulates sympathetic nervous system
Blood Vessels & Circulation ~ Chapter 21~7/13/2011 23
Dr. Vince Scialli BSC 1086
Lose capability with age ~ causes syncopy ~ fainting HORMONAL CONTROL MECHANISMS ~ Blood Pressure
ADRENAL MEDULLA HORMONES ~ catecholamines
INCREASES BLOOD PRESSURE
Norepinephrine ----> VASOCONSTRICTION Epinephrine ----> INCREASED CARDIAC OUTPUT
----> VASOCONSTRICTION
ANTI-DIURETIC HORMONE ~ ADH ~ vasopressin
Secreted By POSTERIOR PITUITARY INCREASES BLOOD PRESSURE WATER RETENTION > INCREASED BLOOD VOLUME CAUSES VASOCONSTRICTION If SEVERE FLUID LOSS OR DROP IN BLOOD PRESSURE
ATRIAL NATRIUETIC PEPTIDE ~ secreted by HEART
LOWERS BLOOD PRESSURE ANTAGONIZES ALDOSTERONE INCREASES Na+ EXCRETION IN KIDNEYS WATER LOSS > DECREASED BLOOD VOLUME CAUSES VASODILATION
Blood Vessels & Circulation ~ Chapter 21~7/13/2011 24
Dr. Vince Scialli BSC 1086
BLOCKS ADH & CATECHOLAMINE RELEASE
RENAL REGULATION ~ Long Term Control
KIDNEY RETAINS or EXCRETES H2O IN RESPONSE TO BLOOD PRESSURE CHANGES . . REGULATES BLOOD VOLUME
RENAL Autoregulation
Increased blood volume & pressure increases blood flow to kidney which increases urine formation (Nervousness) Decreased blood volume or pressure decreases renal blood flow which reduces urine formation
RENIN-ANGIOTENSIN-ALDOSTERONE MECHANISM
DROP BLOOD PRESSURE ----> Kidneys release RENIN
RENIN becomes Angiotensin I in blood Angiotensin I becomes Angiotensin II
POTENT VASOCONSTRICTOR ~ B P
Angiotensin II ----> Adrenals release of ALDOSTERONE
----> NA+ REABSORPTION & H2O RETENTION ----> INCREASED BLOOD VOLUME & BLOOD PRESSUE
ERYTHROPOIETIN
Large BP drop stimulates release by kidney
EPO stimulates release of RBCs from bone marrow
Blood Vessels & Circulation ~ Chapter 21~7/13/2011 25
Dr. Vince Scialli BSC 1086
INCREASES VOLUME & VISCOSITY OF BLOOD TISSUE PERFUSION ~ BLOOD FLOW THROUGH TISSUES 1) 2) 3) 4) DELIVERS O2 & NUTRIENTS REMOVES CO2 AND METABOLIC WASTES GAS EXCHANGE IN THE LUNGS URINE FORMATION
Determined by VOLUME & VELOCITY of Blood Flow
VOLUME
BRAIN HEART KIDNEYS ABDOMINAL ORGANS SKELETAL MUSCLE
AT REST 13% 4% 20% 24% 20%
EXERCISE 4% 4% 3% 3% 71%
VELOCITY
VELOCITY IS INVERSELY PROPORTIONAL TO CROSS SECTIONAL AREA OF THE BLOOD VESSEL BLOOD FLOWS FASTEST WHERE THE TOTAL CROSS SECTIONAL AREA IS SMALLEST INDIVIDUAL CAPILLARY HAS SMALL LUMEN BUT TOTAL CROSS SECTION AREA OF CAPILLARY BED IS VERY LARGE TOTAL CROSS SECTIONAL AREA AORTA 250 cm sq ARTERIES 500 cm sq ARTERIOLES 3000 cm sq * * * CAPILLARIES 4500 cm sq VENULES 3000 cm sq VEINS 500 cm sq
Blood Vessels & Circulation ~ Chapter 21~7/13/2011 26
FLOW SPEED FASTEST FAST SLOW SLOWEST SLOW FAST
Dr. Vince Scialli BSC 1086
* * * SLOW CAPILLARY FLOW ALLOWS ADEQUATE TIME FOR EXCHANGES TO BE MADE CIRCULATORY IMBALANCES ~ (May Not Covered in Lecture)
HYPOTENSION ~ LOW BLOOD PRESSURE
SYSTOLIC PRESSURE DROPS BELOW < 100 mm Hg
ACUTE HYPOTENSION ~ MOST common
DUE TO: DROP IN BLOOD VOLUME & PRESSURE
-----> CIRCULATORY SHOCK ~ SYSTEM SHUTDOWN Hypovolemic ~ large volume loss ~ Hemorrhage Anaphylaxis ~ system vasodilation ~ Histamine Cardiogenic ~ heart failure ~ inadequate circulation Vascular ~ Septic ~ bacterial toxins IMMEDIATE THERAPY: IV FLUIDS TO REPLACE VOLUME ~ TRANSFUSIONS
CHRONIC HYPOTENSION
DUE TO: THIN BLOOD ~ LOW VISCOSITY POOR NUTRITION & ANEMIA LOW PROTEIN ~ low hemoglobin
ORTHOSTATIC HYPOTENSION ~ OLD AGE
Loss of Carotid Sinus SYMPATHETIC RESPONSE LOW BLOOD PRESSURE & DIZZINESS
Blood Vessels & Circulation ~ Chapter 21~7/13/2011 27
Dr. Vince Scialli BSC 1086
FAINTING WHEN STAND UP . . . BLOOD POOLS
Blood Vessels & Circulation ~ Chapter 21~7/13/2011
28
Dr. Vince Scialli BSC 1086
HYPERTENSION ~ HIGH BLOOD PRESSURE
SYSTOLIC PRESSURE > 140 mm Hg (BORDERLINE) DIASTOLIC PRESSURE > 90 mm Hg (now > 85) NORMAL INCREASES: FEVER EXERCISE & EXCITEMENT EMOTIONAL UPSET
CHRONIC HYPERTENSION ~ MOST COMMON
High Stress for Years > INCREASE VESSEL RESISTANCE SLOWLY STRAINS HEART & DAMAGES VESSELS SILENT KILLER HEART FAILURE RENAL FAILURE ATHEROSCLEROSIS STROKE Causes: DIET ~ NA+, FAT, CHOLESTEROL OBESITY ~ LONGER VESSEL LENGTH AGE ~ > 40 STRESS & SMOKING ~ NICOTINE is a vasoconstrictor
PRIMARY HYPERTENSION ~ NO SPECIFIC CAUSE IN 90%
RACE ~ BLACKS > WHITE HEREDITARY ~ FAMILIES
Blood Vessels & Circulation ~ Chapter 21~7/13/2011 29
Dr. Vince Scialli BSC 1086
AGING EFFECTS ON CARDIOVASCULAR SYSTEM HEART CHANGES
REDUCTION IN MAXIMUM CARDIAC OUTPUT CHANGES IN CONDUCTION CAPABILITIES REDUCTION IN ELASTACITY OF FIBROUS SKELETON PROGRESSIVE ATHEROSCLEROSIS RESTRICTS CORONARY CIRCULATION ~ Resistance DAMAGED CARDIAC CELLS REPLACED BY SCAR TISSUE
VESSEL CHANGES
WALLS LOOSE ELASTICITY LESS TOLERANT TO SUDDEN PRESSURE CHANGES MORE PRONE TO ANEURYSM FORMATION CALCIUM DEPOSITS ON WEAKENED VESSEL WALLS INCREASED RISK OF STROKE OR INFARCTION PRONE TO THROMBI FORMATION ~ ATHEROSCLEROSIS
Blood Vessels & Circulation ~ Chapter 21~7/13/2011
30
Dr. Vince Scialli BSC 1086
The remaining material will not be covered in lecture ~ Reference Only
TISSUE PERFUSION AUTO REGULATION Constant Dilation/Constriction of Capillaries regulates local blood flow Due to CHANGES in DIAMETERS of ARTERIOLES FEEDING CAPILLARY BEDS METABOLIC CONTROLS RESPONSE TO NUTRIENTS, O2 & CO2 VASODILATION OF ARTERIOLES ----> INCREASES PERFUSION VASOCONSTRICTION ----> DECREASES PERFUSION MYOGENIC CONTROLS LOW PERFUSION ----> DEATH OF TISSUE ~ Necrosis High PERFUSION ----> RUPTURED VESSELS ~ nose bleeds REACTIVE HYPEREMIA ~ Local Redness & Swelling DRAMATIC INCREASE IN BLOOD FLOW INTO TISSUE AFTER BLOCKAGE OR INJURY ANGIOGENESIS ~ COLLATERAL CIRCULATION NEW ARTERIOLES DEVELOP ~ COLLATERAL CIRCULATION EG. CORONARY ~ Heart Attacks HIGH ALTITUDE CONDITIONS
Blood Vessels & Circulation ~ Chapter 21~7/13/2011 31
Dr. Vince Scialli BSC 1086
UNIQUE TISSUE PERFUSION ~ (Not Covered in Lecture- Reference Only) SKELETAL MUSCLE EXTREMELY VARIABLE WITH MUSCLE ACTIVITY HYPEREMIA: FLOW INCREASES DIRECTLY WITH METABOLIC ACTIVITY AND O2 REQUIREMENT CHOLINERGIC RECEPTORS ----> STIMULATE VASODILATION BLOOD FLOW CAN INCREASE 10X DURING EXERCISE BLOOD DIVERTED FROM SKIN & DIGESTIVE ORGANS BRAIN TOTAL BLOOD FLOW TO BRAIN REMAINS CONSTANT 750 ml/min BRAIN NEURONS TOTALLY INTOLLERANT OF ISCHEMIA CEREBRAL EDEMA > DEATH BRAIN IS MOST METABOLIC ACTIVE ORGAN IN BODY BRAIN IS LEAST ABLE TO STORE ESSENTIAL NUTRIENTS GLUCOSE VERY RESPONSIVE TO CO2 INCREASE & H+ DECREASE VERY SENSITIVE TO CHANGES IN ARTERIAL PRESSURE FAINTING OR SYNCOPE IF MAP < 60 mm Hg CEREBRAL EDEMA IF MAP > 160 mm Hg Transient Ischemic Attacks ~ TIAs
Blood Vessels & Circulation ~ Chapter 21~7/13/2011 32
Dr. Vince Scialli BSC 1086
Cerebro-vascular Accident ~ CVA ~ stroke UNIQUE TISSUE PERFUSION ~ (Not Covered in Lecture ~ Reference Only) SKIN BLOOD FLOW THROUGH THE SKIN 1) 2) 3) SUPPLIES NUTRIENTS TO CELLS BODY TEMPERATURE REGULATION BLOOD RESERVOIR
WHEN BODY TEMPERATURE INCREASES > SYMPATHETIC STIMULATION IS INHIBITED > VASODILATION OF SKIN VESSELS WHEN BODY TEMPERATURE DECREASES > SYMPATHETIC STIMULATION > VASOCONSTRICTION OF SKIN VESSELS LUNGS PULMONARY CIRCULATION VERY SHORT LOW PRESSURE SYSTEM ~ SYSTOLIC = 24 mm Hg DIASTOLIC = 8 mm Hg ARTERIAL VESSELS STRUCTURED LIKE VEINS THINNER WALLS LARGER LUMEN AUTOREGULATION IS OPPOSITE SYSTEMIC CIRCULATION LOW BLOOD O2 > VASOCONSTRICTION TO ALLOW MORE O2 TO MOVE INTO BLOOD HIGH BLOOD O2 > VASODILATION TO ALLOW O2 TO MOVE OUT OF BLOOD
Blood Vessels & Circulation ~ Chapter 21~7/13/2011
33
Dr. Vince Scialli BSC 1086
UNIQUE TISSUE PERFUSION ~ (Not Covered in Lecture ~ Reference Only) HEART WHEN VENTRICLES CONTRACT, CORONARY VESSELS BECOME COMPRESSED ----> BLOOD FLOW THROUGH THE MYOCARDIUM STOPS BLOOD FLOW TO THE MYOCARDIUM OCCURS WHEN THE HEART IS IN DIASTOLE OR RELAXED ABNORMALLY FAST HEARTBEAT REDUCES THE ABILITY OF THE MYOCARDIUM TO RECEIVE ADEQUATE O2 CARDIAC CELLS USE 65% OF O2 CARRIED TO IT COMPARED TO 25% FOR NON-CARDIAC CELLS 25% of Cardiac Cell is Mitochondria 2% of Skeletal Muscle cell is Mitochondria
Blood Vessels & Circulation ~ Chapter 21~7/13/2011
34
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Hand Hygiene Audit March 19Document17 pagesHand Hygiene Audit March 19Sammie WainainaNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Daftar Kalibrasi Alat 2020Document18 pagesDaftar Kalibrasi Alat 2020Budi SetyawanNo ratings yet
- Mindmap METENDocument1 pageMindmap METENIpulCoolNo ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Name of Pharmacy: ................................. CityDocument1 pageName of Pharmacy: ................................. Cityravi sheladiyaNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Hipertensi PBLDocument56 pagesHipertensi PBLVandra PrinosaNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- General Paper September 2020Document26 pagesGeneral Paper September 2020Kumah Wisdom100% (1)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Experimental Design in Clinical TrialsDocument18 pagesExperimental Design in Clinical Trialsarun_azamNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Cytomegalovirus (CMV) : R.Varidianto Yudo T., Dr.,MkesDocument21 pagesCytomegalovirus (CMV) : R.Varidianto Yudo T., Dr.,MkesIndah WahyuningtyasNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- FamilyDocument19 pagesFamilytugba1234No ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- SESSION 13 Abnormal PsychologyDocument47 pagesSESSION 13 Abnormal PsychologyKainaat YaseenNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Diagnosis and Management of Atypical Preeclampsia-Eclampsia: Obstetric Anesthesia Digest March 2010Document8 pagesDiagnosis and Management of Atypical Preeclampsia-Eclampsia: Obstetric Anesthesia Digest March 2010Fedrik Monte Kristo LimbongNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Pricing Reimbursement of Drugs and Hta Policies in FranceDocument20 pagesPricing Reimbursement of Drugs and Hta Policies in FranceHananAhmedNo ratings yet
- Lequesne Eng NdexDocument3 pagesLequesne Eng NdexGhioc Mihaela AlinaNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- DR Paul Krawitz - Ultimate Insiders Guide To Eye HealthDocument60 pagesDR Paul Krawitz - Ultimate Insiders Guide To Eye HealthPro ANo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Altamash Shabbir Maniyar Resume 22-05-2023-04-03-54 230601 200613Document3 pagesAltamash Shabbir Maniyar Resume 22-05-2023-04-03-54 230601 200613Kanhaiya VermaNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- 1238-Article Text-5203-1-10-20220916Document3 pages1238-Article Text-5203-1-10-20220916srirampharmNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- VIII. Problem Identification and Prioritization XDocument3 pagesVIII. Problem Identification and Prioritization XMichelle HutamaresNo ratings yet
- SHD Form 4 T - NTPDocument3 pagesSHD Form 4 T - NTPElle RochNo ratings yet
- Disseminated Intravascular Coagulation (DIC)Document24 pagesDisseminated Intravascular Coagulation (DIC)Atiya HajjajNo ratings yet
- Referat ObesitasDocument20 pagesReferat ObesitasfaisalNo ratings yet
- Chirorab Prescribing InformationDocument2 pagesChirorab Prescribing Informationsr bNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- CASE SCENARIO 3 PreopDocument3 pagesCASE SCENARIO 3 PreopEdgarNo ratings yet
- SAFE520bP - Injury ReportDocument1 pageSAFE520bP - Injury ReportMiracle DavidNo ratings yet
- Automated DatabasesDocument14 pagesAutomated DatabasesAnilkumar Sagi100% (4)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Nursing Care For HipopituitarismeDocument10 pagesNursing Care For Hipopituitarismevita marta100% (1)
- Sales and Distribution Management PDFDocument30 pagesSales and Distribution Management PDFNalin SenthilNo ratings yet
- Protocolo Cochrane REHABILITACIÓN COGNITIVA en Demencia (2019)Document17 pagesProtocolo Cochrane REHABILITACIÓN COGNITIVA en Demencia (2019)Sara Daoudi FuentesNo ratings yet
- Branding Strategies DecisionsDocument40 pagesBranding Strategies DecisionsnishatalicoolNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Presented by Amir Sadaula BVSC & Ah, 8 Sem Rampur Campus Roll No: 01Document19 pagesPresented by Amir Sadaula BVSC & Ah, 8 Sem Rampur Campus Roll No: 01naturalamirNo ratings yet
- Ventilator Draeger Evita V300 - Spesifikasi Teknis PDFDocument4 pagesVentilator Draeger Evita V300 - Spesifikasi Teknis PDFArifyadin SudonoNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)