Professional Documents
Culture Documents
Glass Coma Scale
Uploaded by
RnspeakcomOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Glass Coma Scale
Uploaded by
RnspeakcomCopyright:
Available Formats
HEAD (NEUROLOGICAL/ PSYCHIATRIC)
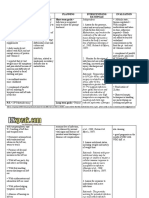
I. Cerebrovascular accident: sudden loss of brain functioning A. Types: 1. Ischemic: Decrease blood supply to brain vessels 2. Hemorrhagic: Intracranial bleeding B. Symptoms: Slurred speech, unilateral movement, drooped face, blurred vision, numbness C. Interventions: 1. Maintain airway function 2. Provide neuro-checks every hour and vital signs 3. Assess gag reflex related to aspiration risks 4. Perform a Glasgow Coma Scale every 30min-hour D. Glasgow Coma Scale (Normal 8-15 or <7 indicates coma)
Spontaneous; open with blinking at baseline Opens to verbal command, speech, or shout Opens to pain None Obeys verbal commands Purposeful movement to painful stimulus Flexion: withdraws from pain Flexion: abnormal (spastic) decorticate Extension: abnormal (rigid) decerebrate None Orientedx3 (person, place, time) Confused conversation Speech (Inappropriate) Speech (Incomprehensible) None 4 3 2 1 6 5 4 3 2
Eye Opening Response
Motor Response
1
5 4 3 2 1
Verbal Response
II.
Seizure or Epilepsy: A seizure results from a chaotic or excessive discharge of neurons. It is considered a symptom that has many underline causes such as head injury, drugs, intoxication, feveretc. Epilepsy is a clinical diagnosis, which is characterized as recurring seizures. A. Types 1. Generalized: Involves both sides of the brain i.e. tonic-clonic (formerly grand mal) or absence (petit mal) 2. Partial: Involves a specific part of the brain or one hemisphere; loss consciousness (complex) or no loss of consciousness (simple) 3. Status Epilepticus: Life-threatening condition in which the seizure lasts longer than 30min. Treatment should begin within 5min. Airway management and benzodiazepines are
III.
IV.
imperative. The longer the seizure occurs, the more the brain is damage and should be treated promptly B. Documentation (COLD) 1. Character: What was the seizure activity occurring? Document the body parts involved, the activities beforehand 2. Onset: When did start? What was happening? Note any incontinence or trauma that occurred. 3. Location: Where did the activity start? 4. Duration: How long did the seizure last and its post-ictal stage? C. Interventions: 1. Place the patient in seizure precautions 2. Obtain capillary blood sugar so hypoglycemia is not confused with the person post-ictal phase 3. Obtain blood samples: Used to assess medication, alcohol levels Spinal Cord Injury: A disruption of nerve tracts that cause sensory loss, paralysis, or nervous system dysfunction A. Types of injury 1. Cervical: Quadriplegia a. Ventilated dependent related to diaphragm paralysis b. All four extremities paralyzed c. Injury above C3 is usually fatal 2. Thoracic: Paraplegia a. Paralysis of lower extremities b. Bladder and bowel incontinence c. Increased risk of having autonomic dysreflexia: A complication occurring above T6, symptoms include severe hypertension (systolic<200), headache, diaphoresis 3. Lumbar: Decrease control or paralysis of lower extremities and loss bowel/bladder function B. Interventions 1. Immobilized the client or place a c-collar on him/her until cleared by the attending physician, usually after x-ray and CT scan results 2. Maintain respiratory function 3. Assess vital sign hourly Meningitis is an infection of the meninges, a protective membrane that cover the brain and spinal cord. There are different types of meningitis, however, bacterial meningitis is life threatening that has a very high mortality rate if left untreated
V.
A. Three Classic Symptoms: Change in LOC, nuchal rigidity neck stiffness, and a sudden high fever B. Interventions 1. Anticipate a lumbar puncture to isolate the organism 2. Promptly administer IV antibiotics, hydration, oxygen Suicidal Ideation: To have thoughts or a plan of committing suicide A. Identify High Risk Groups: adolescents, elderly, stressful life events i.e. sexual orientation conflicts, chronic illnesses, substance abusers B. Interventions 1. Initiate suicide/safety precautions a. Stay with the patient or implement using a sitter b. Use restraints as ordered and document the incident accordingly c. Remove sharp or dangerous objects 2. Anticipate psychiatric services; the patient may be cleared of threatening behavior and sent home with follow-up/ outpatient treatment 3. If discharged make sure the patient is aware of resources readily available 4. Psychotic episodes should follow similar interventions
You might also like
- Nursing Informatics: Bachelor of Science in NursingDocument6 pagesNursing Informatics: Bachelor of Science in NursingMichelle MallareNo ratings yet
- Guillain Barre SyndromeDocument200 pagesGuillain Barre SyndromeclarisedeasisNo ratings yet
- 12 - DeathDocument18 pages12 - DeathMo'taz Ahmed TelebNo ratings yet
- Neuro-Dr AsmaaDocument35 pagesNeuro-Dr AsmaaSoad RedaNo ratings yet
- Seizure DisorderDocument4 pagesSeizure DisorderJohanna ChavezNo ratings yet
- RSNG 2539 - CognitionDocument7 pagesRSNG 2539 - CognitionEciOwnsMeNo ratings yet
- NCM 114 Lesson1 1Document8 pagesNCM 114 Lesson1 1Trisha Lopez100% (1)
- Nursing Assessment 1Document6 pagesNursing Assessment 1Kedir AliyiNo ratings yet
- DeathDocument49 pagesDeathSriram ShirkeNo ratings yet
- Epilepsyppt 180618175748Document38 pagesEpilepsyppt 180618175748Vasu LohraNo ratings yet
- Neuro CH 14 Study GuideDocument9 pagesNeuro CH 14 Study GuideMichael J MillerNo ratings yet
- SeizuresDocument2 pagesSeizureskaythe08No ratings yet
- PoliomyelitisDocument4 pagesPoliomyelitisJohn Paul NavaltaNo ratings yet
- SeizuresDocument60 pagesSeizuresEman SleemNo ratings yet
- Anticonvulsant Part 1Document42 pagesAnticonvulsant Part 1Rameez ShamounNo ratings yet
- (3.2) EpilepsyDocument14 pages(3.2) EpilepsyFarhaNo ratings yet
- Seizure Disorders: International Classification of SeizuresDocument13 pagesSeizure Disorders: International Classification of SeizuresYousef KhalifaNo ratings yet
- NCM 118 - Lesson 17 (Ishemic and Hemorrhagic CVA)Document5 pagesNCM 118 - Lesson 17 (Ishemic and Hemorrhagic CVA)Bobby Christian DuronNo ratings yet
- By Abraham Belay: Approach To ComaDocument36 pagesBy Abraham Belay: Approach To ComaashuNo ratings yet
- Team 2 Case Study EpilepsyDocument15 pagesTeam 2 Case Study EpilepsytmgursalNo ratings yet
- Communicable Disease Nursing: Mrs. Dionesia Mondejar NavalesDocument64 pagesCommunicable Disease Nursing: Mrs. Dionesia Mondejar NavalesChevelle Valenciano-Gaan0% (1)
- Brain Abscess: Mohd Roslee Bin Abd GhaniDocument36 pagesBrain Abscess: Mohd Roslee Bin Abd GhaniSaha DirllahNo ratings yet
- Management of Multiple Traumatised PatientDocument4 pagesManagement of Multiple Traumatised PatientOmar MohammedNo ratings yet
- UnconsciousnessDocument23 pagesUnconsciousnessmtlqhsn78No ratings yet
- Comatose: DR Tanveer HJ IqbalDocument37 pagesComatose: DR Tanveer HJ IqbalTanveerHajiIqbalNo ratings yet
- Neuro Disorders Study OutlineDocument9 pagesNeuro Disorders Study OutlineHeather Russell100% (1)
- Guidelines For Management of Head InjuryDocument18 pagesGuidelines For Management of Head InjuryChellamani UmakanthanNo ratings yet
- CHAPTER 38 Neurological and Cognitive Problems - Nanda - PPTDocument24 pagesCHAPTER 38 Neurological and Cognitive Problems - Nanda - PPTBagus DwiyanNo ratings yet
- Neurological Disorders - SIMCLEXDocument10 pagesNeurological Disorders - SIMCLEXLLLJJJNo ratings yet
- Health Week 1-3 - 3rd QuarterDocument8 pagesHealth Week 1-3 - 3rd QuarterNoemelyn VecinaNo ratings yet
- Points To Remember EverDocument11 pagesPoints To Remember EverAnalyn Tomes PabillaranNo ratings yet
- Documentation in NCM 104 Class Exhibit: Traumatic Brain InjuriesDocument7 pagesDocumentation in NCM 104 Class Exhibit: Traumatic Brain InjuriesMinhwa KimNo ratings yet
- Chapter Six-: Shock, Sudden Illness and UnconsciousnessDocument36 pagesChapter Six-: Shock, Sudden Illness and Unconsciousnessbirhanu Ayenew AnleyNo ratings yet
- NeuroDocument31 pagesNeuroLouise Marie Palamos Damasco100% (3)
- Seizure Disorder, Spinal Injury Neural TumorDocument52 pagesSeizure Disorder, Spinal Injury Neural TumornipoNo ratings yet
- ComaDocument13 pagesComaMamoon J. MehdiNo ratings yet
- Dzino's SurgeryDocument718 pagesDzino's SurgeryHuram SeremaniNo ratings yet
- PPTDocument61 pagesPPTRheal P EsmailNo ratings yet
- Advance Nursing PracticeDocument12 pagesAdvance Nursing PracticebldewnaNo ratings yet
- MeniningitaDocument3 pagesMeniningitaAlina Elisabeta Tiniuc căs LehaciNo ratings yet
- MS Neurologic Conditions J2018 Ans KeyDocument13 pagesMS Neurologic Conditions J2018 Ans KeyPaul Lexus Gomez LorenzoNo ratings yet
- Seminar ON Seizure: Presented To Presented byDocument35 pagesSeminar ON Seizure: Presented To Presented byShitaljit IromNo ratings yet
- ABC TraumaDocument27 pagesABC TraumarikarzNo ratings yet
- Electro Convulsive TherapyDocument15 pagesElectro Convulsive TherapyjyotichoithramNo ratings yet
- ATLS (Advanced Trauma Life Support) Teaching Protocol Pretest (30 Min) Context of Tutorial (2 Hours)Document16 pagesATLS (Advanced Trauma Life Support) Teaching Protocol Pretest (30 Min) Context of Tutorial (2 Hours)anon_778118144No ratings yet
- Basic Principles of Trauma ManagementDocument53 pagesBasic Principles of Trauma ManagementMohamed Saeed BachooNo ratings yet
- Seizure Disorder: Presented By: Binisha Dahal M.SC Nursing 2 YearDocument39 pagesSeizure Disorder: Presented By: Binisha Dahal M.SC Nursing 2 YearMalathi VarnaNo ratings yet
- Neurological Assessment 3RD 1Document135 pagesNeurological Assessment 3RD 1maitriNo ratings yet
- Neurologic AssessmentDocument7 pagesNeurologic AssessmentFerric Lapenas100% (1)
- Pediatric Emergencies: Presented By: Ziyad SalihDocument51 pagesPediatric Emergencies: Presented By: Ziyad SalihNana MuktiNo ratings yet
- Common Medical EmergenciesDocument25 pagesCommon Medical EmergenciesZnieh ZniehNo ratings yet
- Baseline Vital Kefah 1ADocument38 pagesBaseline Vital Kefah 1AShahd Abu SnenehNo ratings yet
- 4 ConvulsionDocument40 pages4 ConvulsionMohamed Na3eemNo ratings yet
- EPILEPSYDocument37 pagesEPILEPSYPauline AñesNo ratings yet
- COMADocument37 pagesCOMAPooja ShashidharanNo ratings yet
- Medicolegal Aspects of DeathDocument26 pagesMedicolegal Aspects of DeathRonald Alasa-as AtigNo ratings yet
- Module 4Document6 pagesModule 4Christian Jay Sacueza BucadNo ratings yet
- Epilepsy Lesson PlanDocument14 pagesEpilepsy Lesson PlanShree Kalidass100% (4)
- Nurse Practitioner Board ReviewFrom EverandNurse Practitioner Board ReviewRating: 5 out of 5 stars5/5 (1)
- Obsessive Compulsive Disorder Nursing Care Plan - Severe AnxietyDocument2 pagesObsessive Compulsive Disorder Nursing Care Plan - Severe AnxietyRnspeakcom80% (5)
- (IMCI) Integrated Management of Childhood IllnessDocument34 pages(IMCI) Integrated Management of Childhood Illnessɹǝʍdןnos97% (34)
- Hip Fracture Nursing Care PlanDocument6 pagesHip Fracture Nursing Care PlanRnspeakcom100% (1)
- 6th Central Pay Commission Salary CalculatorDocument15 pages6th Central Pay Commission Salary Calculatorrakhonde100% (436)
- Nursing Care Plan Breast CancerDocument2 pagesNursing Care Plan Breast CancerRnspeakcom0% (1)
- Otitis Media Nurisng Care PlanDocument11 pagesOtitis Media Nurisng Care PlanRnspeakcom100% (1)
- Pathophysiology HypokalemiaDocument1 pagePathophysiology HypokalemiaRnspeakcomNo ratings yet
- Nursing Care Plan For Alzheimer's DiseaseDocument4 pagesNursing Care Plan For Alzheimer's DiseaseRnspeakcom100% (1)
- Risk For Constipation-Cancer Nursing Care PlanDocument1 pageRisk For Constipation-Cancer Nursing Care PlanRnspeakcomNo ratings yet
- Thyroidectomy Nursing Care PlanDocument2 pagesThyroidectomy Nursing Care PlanRnspeakcom100% (1)
- Ineffective Airway Clearance-Nursing Care Plan For COPDDocument2 pagesIneffective Airway Clearance-Nursing Care Plan For COPDRnspeakcom100% (1)
- Room Assignment PNLE 122011Document126 pagesRoom Assignment PNLE 122011NonoyTaclinoNo ratings yet
- Urinary Incontinence Nursing ManagementDocument3 pagesUrinary Incontinence Nursing ManagementRnspeakcomNo ratings yet
- December 2011 NLE Room Assignment in Davao CityDocument275 pagesDecember 2011 NLE Room Assignment in Davao CityRnspeakcomNo ratings yet
- Urinary Tract Infection Nursing-Care-PlanDocument3 pagesUrinary Tract Infection Nursing-Care-PlanRnspeakcomNo ratings yet
- Acute Glomerulonephritis (AGN) Pathophysiology & Schematic DiagramDocument1 pageAcute Glomerulonephritis (AGN) Pathophysiology & Schematic DiagramRnspeakcom50% (2)
- Schedule of Seminars (January To May 2012)Document2 pagesSchedule of Seminars (January To May 2012)RnspeakcomNo ratings yet
- Nurses Nle Cebu December 2011 Room AssignmentDocument321 pagesNurses Nle Cebu December 2011 Room AssignmentkapitannwelNo ratings yet
- Nurs0612ra MlaDocument924 pagesNurs0612ra MlaPRC BoardNo ratings yet
- December 2011 NLE Room Assignment in Iloilo CityDocument233 pagesDecember 2011 NLE Room Assignment in Iloilo CityRnspeakcomNo ratings yet
- NURSE 12 - 11 PagdianDocument74 pagesNURSE 12 - 11 PagdianNonoyTaclinoNo ratings yet
- Nle122011 LegazpiDocument93 pagesNle122011 LegazpiNonoyTaclinoNo ratings yet
- June - July 2012 Nurse Licensure Examination Room Assignment (MANILA) - ConditionedDocument1 pageJune - July 2012 Nurse Licensure Examination Room Assignment (MANILA) - ConditionedjamieboyRNNo ratings yet
- Nle Zamboanga December 2011 Room AssignmentDocument90 pagesNle Zamboanga December 2011 Room AssignmentkapitannwelNo ratings yet
- December 2011 NLE Room Assignment in ManilaDocument872 pagesDecember 2011 NLE Room Assignment in ManilaRnspeakcomNo ratings yet
- Nurses Romassign Dec2011Document165 pagesNurses Romassign Dec2011NonoyTaclinoNo ratings yet
- DOH Nurse Volunteer Termination ElucidationDocument1 pageDOH Nurse Volunteer Termination ElucidationRnspeakcomNo ratings yet
- PRC Room Assignment For December 2011 Nursing Board Exam (Pampanga)Document60 pagesPRC Room Assignment For December 2011 Nursing Board Exam (Pampanga)PhilippineNursingDirectory.com0% (1)
- RN Heals 2Document6 pagesRN Heals 2NonoyTaclino0% (2)
- Pediatric Neurology - Lawson Peter N. (SRG)Document200 pagesPediatric Neurology - Lawson Peter N. (SRG)Hriday DeNo ratings yet
- Regulation of RespirationDocument21 pagesRegulation of RespirationSheeraz ShahzadNo ratings yet
- CEREBRUM Functional Areas 2022Document7 pagesCEREBRUM Functional Areas 2022GURNOOR DHILLONNo ratings yet
- Test Bank For Essentials of Pediatric Nursing 1st Edition Theresa KyleDocument13 pagesTest Bank For Essentials of Pediatric Nursing 1st Edition Theresa KyleAnthonyRiveraqion100% (33)
- Binaural Frequency List GuideDocument30 pagesBinaural Frequency List GuideChristopher Parker100% (7)
- Veterinary: Prathmesh DeshmukhDocument1 pageVeterinary: Prathmesh DeshmukhFaizan SheikhNo ratings yet
- 2192-Article Text-4309-1-10-20230105Document11 pages2192-Article Text-4309-1-10-20230105MellowNo ratings yet
- Model Nursing Early Warning System Score (Newss) Dengan Aplikasi Tehnologi Informasi Sebagai Pengkajian Deteksi Kegawatan Pada Klien Stroke Di Rs Kabupaten TangerangDocument12 pagesModel Nursing Early Warning System Score (Newss) Dengan Aplikasi Tehnologi Informasi Sebagai Pengkajian Deteksi Kegawatan Pada Klien Stroke Di Rs Kabupaten Tangeranganggita putriNo ratings yet
- Advances in Cognitive Neurodynamics (VI)Document385 pagesAdvances in Cognitive Neurodynamics (VI)Víctor FuentesNo ratings yet
- Anatomy PhysiologyDocument20 pagesAnatomy PhysiologyAneez Malik100% (2)
- Stahl' Essential Psychopharmacology 291Document1 pageStahl' Essential Psychopharmacology 291Muhammad AzkaNo ratings yet
- Why One Neuroscientist Started Blasting His CoreDocument4 pagesWhy One Neuroscientist Started Blasting His CoreVinceNo ratings yet
- Human Biology PASS Mid-Tri Exam Buster 2021Document12 pagesHuman Biology PASS Mid-Tri Exam Buster 2021Robert100% (1)
- Facial Nerve Trauma Clinical Evaluation And.41Document15 pagesFacial Nerve Trauma Clinical Evaluation And.41Razaria DailyneNo ratings yet
- Neonatal SeizuresDocument22 pagesNeonatal SeizuresKatrin Marcelina SihombingNo ratings yet
- STOP, LOOK, AND LISTEN: The Challenge For Children With ADHDDocument13 pagesSTOP, LOOK, AND LISTEN: The Challenge For Children With ADHDJFNo ratings yet
- The Stroop Color and Word Test: Federica Scarpina and Sofia TaginiDocument8 pagesThe Stroop Color and Word Test: Federica Scarpina and Sofia TaginiHafiidh0% (1)
- Abstracts Book - 1623231029Document158 pagesAbstracts Book - 1623231029DennyNo ratings yet
- Candle MeditationDocument5 pagesCandle Meditationapi-481596914100% (1)
- Cheat Sheet: Responses Control of The Heart Rate Neurones & The Resting PotentialDocument1 pageCheat Sheet: Responses Control of The Heart Rate Neurones & The Resting PotentialLaila MahmudahNo ratings yet
- Apraxia de Conducción PDFDocument5 pagesApraxia de Conducción PDFIvana VilNo ratings yet
- Frederique de Vignemont - Mind The Body - An Exploration of Bodily Self-Awareness-Oxford University Press (2018)Document278 pagesFrederique de Vignemont - Mind The Body - An Exploration of Bodily Self-Awareness-Oxford University Press (2018)Julián David GranadaNo ratings yet
- Nervous System Exam-Style Questions (+ Mark Scheme)Document20 pagesNervous System Exam-Style Questions (+ Mark Scheme)shakeel shahulNo ratings yet
- NCP AssigmentDocument18 pagesNCP AssigmentMuhammad Na'imNo ratings yet
- WMS-IV Webinar September 2011 Handout PDFDocument23 pagesWMS-IV Webinar September 2011 Handout PDFMishal FatimaNo ratings yet
- Protocolos Pulsed PariedDocument13 pagesProtocolos Pulsed PariedAugusto ManoelNo ratings yet
- L16.2 OPHTHA Ocular Motility (Nov1622)Document5 pagesL16.2 OPHTHA Ocular Motility (Nov1622)Erald PaderangaNo ratings yet
- Histology of GangliaDocument18 pagesHistology of GangliaTahir AzizNo ratings yet
- ACTIVITIES IN Motor LearningDocument12 pagesACTIVITIES IN Motor LearningVolleyverseNo ratings yet
- Cts Massage PDFDocument6 pagesCts Massage PDFTsaniodi Fatra Nur ArintraNo ratings yet