Professional Documents
Culture Documents
Study Guide Immunosupressants Antihistamines COxX
Uploaded by
squicciariniOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Study Guide Immunosupressants Antihistamines COxX
Uploaded by
squicciariniCopyright:
Available Formats
Study Guide Antihistamines 1. Differentiate between 1st and 2nd generation antihistamines. How do they act?
The principal difference between the groups is that first-generation antihistamines are highly sedating, whereas second-generation antihistamines are not. PP SLIDES: first generation is sedating, is more anticholinergic, and has peripheral and CNS effects. Second generation are non sedating and do not pass the BBB Histamine1 blockers bind selectively to H1-histaminic receptors, thereby blocking the actions of histamine at these sites. H1 antagonists do not block H2 receptors. Also, they do not block release of histamine from mast cells or basophils 2. What are prototypes and common side effects? 1st generation antihistaminesdiphenhydramine (Benadryl) most sedating; promethazine (Phenergan) quite sedating; chlorpheniramine (Chlor-Trimeton) less sedating 2nd generation antihistamines azelastine (Astelin-nasal spray), cetirizine (Zyrtec), fexofenadine (Allegra), loratadine (Claritin), desloratidine (Clarinex) Common side effects: CNS depression (negligible with second generation), anticholinergic effects (dry mouth, nasal passages, and throat; urinary hesitancy, constipation, palpitations). PP SLIDES: Sedation first generation, other CNS effects such as dizziness, confusion avoid driving /operating heavy machinery, possibly GI disturbances helps to take with food, anticholinergic effects: frequent sips of fluid, suck on candy for dry mouth, caution interaction with alcohol 3. What are important teaching points? Avoid driving/operating heavy machinery, advise against drinking alcohol, advise against using any CNS depressants, should not be used while breast feeding, acute toxicity Immunosuppressants What are immunosuppressants used for? To suppress immune response to prevent organ rejection after transplants (Lifelong), to treat autoimmune diseases What are common adverse effects? Nephrotoxicity, infection, and hepatotoxicity (interactions with grapefruit juice resulting in toxicity) What are prototypes identified? Cyclosporine (Sandimmune), azathioprine (Immuran), tacrolimus (Prograf NSAID and Acetaminophen Study Guide How Do NSAIDS work?
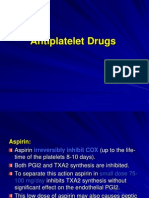
They are nonselective inhibitors of cyclooxygenase, which is an enzyme that converts arachidonic acid into prostaglandins and related compounds. They reduce inflammation, pain, and fever. Describe the action of NSAIDS. At sites of tissue injury, COX catalyzes the synthesis of prostaglandin E2 (PGE2) and prostaglandin I2 (PGI2, prostacyclin), which promote inflammation and sensitize receptors to painful stimuli. In the brain COX-derived prostaglandins mediate fever and contribute to perception of pain. Promotes platelet aggregation. Inhibits all of this, thereby inhibiting inflammation, fever, and pain. What is the difference between a typical NSAID and a COX 2 inhibitor? Typical NSAIDs inhibit COX1 and COX2, whereas COX2 inhibitors only inhibit COX2. COX2 inhibitors are able to suppress pain and inflammation while causing fewer adverse gastric effects, however, increase risk of heart attack and stroke How does acetaminophen differ from aspirin and other NSAIDS? Acetaminophen can reduce pain and fever but cannot suppress inflammation. What are known worrisome side effects of NSAIDS? Gastric ulceration, renal impairment, bleeding What organ function can be damaged by acetaminophen? Liver What caution must be exercised when considering aspirin for children? Reyes syndrome: acetaminophen can be used in children with chickenpox or influenza (aspirin should not be) Rheumatoid Arthritis & Gout What is a DMARD and what are goals of treatment? Disease-modifying antirheumatic drugs Reduce joint destruction and retard disease progression (In general) Treatment is directed at (1) relieving symptoms (pain, inflammation, and stiffness), (2) maintaining joint function and range of motion, (3) minimizing systemic involvement, and (4) delaying disease progression What are adverse effects to be concerned about? Hepatic damage, bone marrow suppression, GI ulceration, pneumonitis What are colchicine and allopurinol used for? Colchicine: Treats acute attack or abort an impending attack (gout) Allopurinol: Treats chronic gout, decreases elevated uric acid caused by chemotherapy What type of drug is indomethicin?
NSAID
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (74)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Drug Guideline: Prostacyclin - NebulisedDocument11 pagesDrug Guideline: Prostacyclin - NebulisedJoana MoreiraNo ratings yet
- Pregnancy Induced Hypertension Case StudyDocument77 pagesPregnancy Induced Hypertension Case StudyJoe Anne Maniulit, MSN, RN84% (49)
- PrasenohadiDocument10 pagesPrasenohadiBonjava1989No ratings yet
- Eicosanoids: (Prostaglandins, Thromboxanes, Leukotrienes)Document26 pagesEicosanoids: (Prostaglandins, Thromboxanes, Leukotrienes)BOsch VakilNo ratings yet
- Systemic PharmacologyDocument37 pagesSystemic PharmacologyMoNiruzzaman MoNirNo ratings yet
- Hypertensive DisordersDocument8 pagesHypertensive DisordersCT Johara MusorNo ratings yet
- Saranya Wattanakumtornkul, MDDocument46 pagesSaranya Wattanakumtornkul, MDPattanop NgaodulyawatNo ratings yet
- ACOG Committee Opinion No. 743 Low-Dose Aspirin Use During PregnancyDocument9 pagesACOG Committee Opinion No. 743 Low-Dose Aspirin Use During PregnancyJaime RdNo ratings yet
- Experiment 8 Analgesic and Anti-Inflammatory WorksheetDocument17 pagesExperiment 8 Analgesic and Anti-Inflammatory WorksheetJANNIE BELLE RODRIGUEZNo ratings yet
- Endothelial Dysfunction in Diabetic Erectile DysfunctionDocument11 pagesEndothelial Dysfunction in Diabetic Erectile DysfunctionILham SyahNo ratings yet
- Prostaglandins: DR Nazakat Hussain Assistant ProfessorDocument33 pagesProstaglandins: DR Nazakat Hussain Assistant ProfessorMuhammad JamalNo ratings yet
- Pharmaglimps Mcqs For Pharmacology 2 PDFDocument39 pagesPharmaglimps Mcqs For Pharmacology 2 PDFDrAmit Verma100% (2)
- The Mechanism of The Physiological Action of BromelainDocument6 pagesThe Mechanism of The Physiological Action of BromelainEllisaTanNo ratings yet
- NSAID's "Non-Steroidal Anti-Inflammatory Drugs": Mmbakhaitan@uqu - Edu.saDocument19 pagesNSAID's "Non-Steroidal Anti-Inflammatory Drugs": Mmbakhaitan@uqu - Edu.saAhmed HossamNo ratings yet
- European Patent SpecificationDocument50 pagesEuropean Patent SpecificationHellz NguyenNo ratings yet
- Antiplatelet DrugsDocument15 pagesAntiplatelet Drugsngan321100% (1)
- Blood RevisedDocument105 pagesBlood RevisedKanelle SisayanNo ratings yet
- Primary Dysmenorrhea Advance in Pathogenesis and ManagementDocument14 pagesPrimary Dysmenorrhea Advance in Pathogenesis and ManagementRafiqy Sa'adiy FaizunNo ratings yet
- Ninja - Autacoids PDFDocument3 pagesNinja - Autacoids PDFErica Hyeyeon LeeNo ratings yet
- 0208 Sulfa SlideDocument24 pages0208 Sulfa SlidetvvsagarNo ratings yet
- Test Inflammation Bds24Document12 pagesTest Inflammation Bds24misdduaaNo ratings yet
- Vasospasm: Endothelial Cell InjuryDocument4 pagesVasospasm: Endothelial Cell InjuryPuja ArgaNo ratings yet
- Pathology Book - Chapter 2 - Inflammation - HKDocument12 pagesPathology Book - Chapter 2 - Inflammation - HKagar agarNo ratings yet
- Cyclooxygenase PathwayDocument8 pagesCyclooxygenase PathwayIradatullah SuyutiNo ratings yet
- Coenzyme Q10 A Therapy For Hypertension and Statin-Induced MyalgiaDocument8 pagesCoenzyme Q10 A Therapy For Hypertension and Statin-Induced MyalgiajohnweakNo ratings yet
- Mechanisms Underlying The Cardiovascular Effects of COX-InhibitionDocument14 pagesMechanisms Underlying The Cardiovascular Effects of COX-InhibitionRangwani NesbitNo ratings yet
- With Important Actions On Smooth MuscleDocument90 pagesWith Important Actions On Smooth MuscleGeraldine Marie Salvo100% (1)
- Hetrocyclic Compound: by Dr. Moona Mehboob Khan Associate Professor Chairperson: Pharmaceutical Chemistry Dcop, DuhsDocument74 pagesHetrocyclic Compound: by Dr. Moona Mehboob Khan Associate Professor Chairperson: Pharmaceutical Chemistry Dcop, DuhsKhan NehalNo ratings yet
- Bromelain, The Enzyme Complex of PineappleDocument13 pagesBromelain, The Enzyme Complex of PineappleEllisaTanNo ratings yet
- Prostaglandins in Pregnancy: Scott W. Walsh, PHDDocument21 pagesProstaglandins in Pregnancy: Scott W. Walsh, PHDIrene AtimNo ratings yet