Professional Documents
Culture Documents
Neonatal Resuscitation
Uploaded by
2012Original Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Neonatal Resuscitation
Uploaded by
2012Copyright:
Available Formats
OS 215 Reproductive Ma.
Esterlita Villanueva-Uy
Neonatal Resuscitation and Depressed Infant Exam 2
OUTLINE
I. How does a baby receive oxygen after birth? resistance < Systemic
A. Before birth (in utero) Vascular resistance –
B. Transition to neonatal circulation note: There is only functional closing of the foramen ovale
C. At completion of this normal transition
D. What can go wrong during transition?
and ductus arteriosus during delivery. The actual closing of
E. How can you tell if a newborn had in utero or these two shunts takes several days to complete.
perinatal compromise?
F. Risk factors associated with need for resuscitation
II. APGAR Score Pulmonary hypertension in the newborn happens if there is no
III. A Depressed Infant increase in PBF and no decrease in PVR. The lungs remain
constricted and the baby becomes cyanotic.
How does a baby receive Oxygen after birth?
C. At completion of this normal transition
A. Before birth (in utero)
Baby breathing and using his lungs
Crying moves the fluid out of his lungs
Lungs have no ventilatory purpose, gasless (because it Oxygen and gaseous distension make pulmonary vessels
is fluid-filled), and have decreased blood flow relax
- only 10% of the blood goes into the pulmonary Baby turns from blue to pink
circulation (due to high resistance in the lungs)
while the other 90% is shunted through the D. What can go wrong during transition?
ductus arteriosus and goes to the systemic
circulation Fetal PO2 = 24-28mmHg; Adult PO2=50-
60mmHg
90% of the time, transition is very smooth. 10% would
need resuscitation. But what could possibly go wrong?
Placenta is the gas-exchange organ- “lungs” Baby does not breathe sufficiently to force fluid or foreign
- it has very low resistance compared to high material (meconium) from the alveoli, thus lungs will not
resistance of the peripheral circulation be filled with air.
Right to left shunts: Excessive blood loss (ex. Abruption placenta) or poor
- foramen ovale cardiac contractility (ex. Due to infection) will result to no
- ductus arteriosus increase in blood pressure hence the shunts remain open
Lack of oxygen or gaseous distension will cause
sustained constriction of the pulmonary arterioles hence
not enough blood will be brought to the lungs(Persistent
Pulmonary Hypertension of the Newborn)
E. How can you tell if a newborn had in utero or
perinatal compromise?
In an experiment done in the 60s, they observed
newly born baboons whose heads were wrapped in
plastic after being born. The following changes (in
chronological order) were observed as they
desperately gasped for air and progressive hypoxia
occurred:
Breathing
Rapid breathing Primary apnea Irregular gasping Secondary apnea
Figure 1. Fetal Circulation. Maternal blood carrying food and
oxygen for the fetus goes to the umbilical vein (vessel with Heart rate
highest oxygenation) and into the ductus venosus. From the
inferior vena cava, blood goes to the right atrium and is shunted
through the foramen ovale into the left atrium. From the left
atrium, blood goes to the left ventricle and eventually to the aorta.
Blood from the superior vena cava goes to the right atrium, into Blood pressure
the right ventricle and into the pulmonary artery. Blood is then
shunted into the ductus arteriosus and then goes to the aorta.
B. Transition to Neonatal Circulation
Table 1.Changes occurring during delivery and their effects. Rapid breathing
Changes Effects
Umbilical cord is clamped Eliminate the placenta Primary apnea
Expansion of the lungs
resulting in a ten-fold Irregular gasping
First breath is taken increase Pulmonary Blood
Flow (PBF) and a ten-fold Secondary apnea
decrease in Pulmonary
vascular resistance (PVR) HYPOXIA
Blood flow increases to the Figure 2. Physiologic changes associated with primary and
Lung fluid gradually
lungs pulmonary vein secondary apnea. Initial oxygen deprivation results in a transient
leaves the alveoli
left atrium period of rapid breathing. If such deprivation persists, breathing
Blood flow to lung Closes foramen ovale movements cease (primary apnea). This is accompanied by a
increases and Left atrial decrease in heart rate and loss of neuromuscular tone. Blood
pressure compensates and increases. If oxygen deprivation and
pressure > Right atrial asphyxia persists, the infant will develop deep gasping
pressure respirations, followed by secondary apnea. This is associated
Pulmonary vascular Closes the ductus arteriosus
September 16, 2008 Tuesday Page 1 of 6
Iris. Hannie. Ezra. Dianne
OS 215 Reproductive Ma. Esterlita Villanueva-Uy
Neonatal Resuscitation and Depressed Infant Exam 2
with a further decline in heart rate, falling blood pressure and loss pink
of neuromuscular tone. Mnemonic:
The same response can be said about newborns in utero A – appearance (color)
or perinatal compromise. An objective measure that can P – pulse rate (heart rate)
tell you whether the newborn is in perinatal compromise or G – grimace (reflex irritability)
not can be obtained through APGAR Score. A – activity (muscle tone)
Apnea is the best indicator of neonatal compromise R – respiration
because it is the earliest manifestation. Blood
pressure is the last to go. 1 minute APGAR Score
In primary apnea, when hypoxic stimulus is removed, the - more of a measure of state of infant in utero, or
baby will start breathing. In secondary apnea, removing how bad his or her condition in the womb was
hypoxic stimulus will not make the newborn breathe. - use to identify the need for immediate
In the clinics, primary and secondary apnea cannot be resuscitation
differentiated, so when faced with an apneic newborn,
always assume that the baby might already be in 5 minute APGAR Score and particularly the change in
secondary apnea so resuscitate aggressively. the score between 1 and 5 minutes
- useful index of the effectiveness of resuscitation
F. Risk Factors Assoc. with Need for Resuscitation efforts
- be aware of these Risk Factors so you can have all - a score of less than 3 could lead to the
equipment ready in the OR development of cerebral palsy
1. Maternal Most infants at birth are in excellent condition, as indicated by
infection aminionitis APGAR Scores of 7 to 10, and they require no aid other than
pneumonia, asthma, ARDS perhaps simple nasopharyngeal suction. Median score is 9 due
Lungs (Adult respiratory distress to acrocyanosis related to temperature instability
syndrome)
Scoring an infant should be logical. An infant would logically not
arrythmia, structural defects,
heart have good activity if heart sounds are not present.
failure
blood anemia, hemoglobinopathies An infant with a score of 4 to 6 at 1 minute demonstrates
blood vessel SLE, DM, HPN depressed respirations, flaccidity and pale to blue color. Heart
uterus hypertonus, rupture rate and reflex irritability, however, are good.
genetic, drugs, PTL (Preterm
others Infants with scores of 0 to 3 usually have slow and inaudible
labor) , MG (multiple gestation),
abnormal FP (fetal presentation) heart rates and depressed or absent reflex responses.
2. Placenta A Depressed Infant
age postmaturity
size, abruption, previa The only way to check if infant is depressed is through
morphology the APGAR score.
Low APGAR score (0-5) in 5 minutes
3. Fetal May be due to a lot of reasons:
umbilical knot, prolapse, compression, - Maternal sedation or anesthesia
cord thrombosis - Substance abuse
blood anemia - Trauma
metabolic IEM (Inborn errors of - Infection
metabolism) - Congenital anomalies
others infection, hydrops, MG - CNS disorders
- Cardiovascular disorders
- Neuromuscular disorders
APGAR Score
Does not necessarily mean that infant is asphyxiated
Objective method of quantifying the newborn’s condition
Conveys information about the newborn’s overall status A. Perinatal asphyxia
and response to resuscitation
Not used to decide how or when to resuscitate – it is Interference in gas exchange between organ systems of
measured in the 1st and then 5th minute after delivery of mother and fetus resulting in impairment of tissue
the baby. If sufficient distress is noted before the 1st perfusion and oxygenation of vital organs in the fetus
minute, when APGAR scoring hasn’t yet been done, then Lactic acidosis and hypercapnea
infant must be resuscitated. Multi-organ damage
Assigned at 1 and 5 minutes of life
When <7, additional scores every 5 min for up to 20 New ACOG/AAO Definition
minutes All four requirements must be met
APGAR SCORE 1. Evidence of antenatal distress
SIGN 0 1 2 - Meconium stained fluid, electronic fetal
Heart Rate Absent <100 >100 heart rate abnormality, fetal tachycardia
Respiration Absent Slow, Good, 2. Low APGAR score (3 or less in the first 5
irregular crying mins.)
Muscle Limp Some Active 3. Evidence of end organ damage
Tone flexion Motion - Brain, lungs, gastrointestinal and
Reflex No Grimace Cough, kidney damages
irritability response sneeze, cry 4. Acid-base abnormality (ph <7.0)
Color Blu or pale Pink body Completely
September 16, 2008 Tuesday Page 1 of 6
Iris. Hannie. Ezra. Dianne
OS 215 Reproductive Ma. Esterlita Villanueva-Uy
Neonatal Resuscitation and Depressed Infant Exam 2
B. Criteria that Suggest an Intrapartum Timing but 3. Pulmonary blood flow decrease in hypoxemia
Nonspecific to Asphyxial Insults and asphyxia
A sentinel hypoxic event occurring immediately before or during =from this point on, these are the slides in the powerpoint
labor
which were skipped by Dr. Uy, except those in bold. So
A sudden and sustained fetal bradycardia or absent fetal
variability in presence of late decelerations please read these parts. =)
Apgar score of 0-3 beyond 5 minutes
Onset of multi-system involvement within 72 hours of birth D. Injury from Asphyxia
Early imaging study showing evidence of acute non-focal
cerebral abnormality
C. Changes in Cardiac Output, Percentage
Distribution, Heart Rate, and Pulmonary Blood
Flow During Asphyxia - What happens during
asphyxia?
- absence of blood flow from placenta to baby will
lead to hypoxia
- carbon dioxide is not released
- hypoperfusion will cause baby to undergo
anaerobic metabolism and thus develop acidosis
- fetus becomes a preferential organ organism:
blood flow to brain, heart and adrenal glands
are increased while blood flow to other organs
will be compromised:
New development regarding mechanism of brain
1. Fetal cardiac output and percentage distribution injury in the term neonate due to asphyxia: cell death
during asphyxia occurs during oxidative stress, inflammation, and
DURING REPAIR STAGE. Why is there injury during
the repair stage? Cytotoxic effects of oxygen radicals
Cardiac Output (ml/min/kg) after blood flow to the tissues is re-established and
molecular oxygen is re-introduced into the tissue.
REPERFUSION INJURY
700
600 1. Generation of Oxygen Radicals
500
400
• Hypoxanthine degradation by hypoxanthine
300
oxidase and oxygen oxygen radicals
• Blood vessels dilated by and oxygen radicals
200
generated by prostaglandin
100
• Proteases and lipases eat up plasma
0
membrane and lead to radical oxygen
Normal Asphyxia species generation
Figure 3. Difference in total fetal cardiac output in
ATP
normal and asphyxiated newborns
AMP
Distribution of Cardiac Output (%) Adenosine
Inosine
60
50 Hypoxanthine
40
Normal
30
Asphyxia Figure 5. Conversion of ATP into hypoxanthine. When
20 ischemia occurs, ATP is converted into hypoxanthine after
a series of steps.
10
0
Brain
Placenta
Spleen
Lungs
U. Body
Heart
Gut
Adrenals
L. Body
Kidney
Figure 4. Distribution of cardiac output in normal and
asphyxiated newborns. In asphyxia, placenta has
greatest allocation of blood. There is also preferential
perfusion to the brain, the heart, and the adrenals.
2. Heart rate response to hypoxemia and asphyxia
- Heart rate decreases in response to
hypoxemia and asphyxia
September 16, 2008 Tuesday Page 1 of 6
Iris. Hannie. Ezra. Dianne
OS 215 Reproductive Ma. Esterlita Villanueva-Uy
Neonatal Resuscitation and Depressed Infant Exam 2
Release of Reactive Oxygen Species
Pathophysiology
Ischemia ATP depletion
Calcium influx
Phospholipase activation
Arachidonic release
Prostaglandins Proteases, lipases
Vasodilation Increase
microvascular
permeability Sarnat scoring determines/ predicts how severe
-
Reperfusion the cerebral palsy is/ will be
- Not rare for sarnat score to increase and
ROS release progress
G. Neonatal Encephalopathy and Cerebral Palsy
ROS
The Report of ACOG’s Task Force on Neonatal
DNA strand Neutrophil
Encephalopathy and Cerebral Palsy
Lipid peroxidation
breakage accumulation
1. Neonatal encephalopathy
Membrane Release of proteases, - Defined clinically on the basis of findings to
myeloperoxidase,
damage
prostaglandins
PMN plugging include a combination of abnormal
of capillaries consciousness, tone and reflexes, feeding,
Phagocytosis respiration or seizure and can result from a
Cell death myriad of conditions
- May or may not result in permanent brain
Ischemia
Tissue damage damage
- Term or near term
Figure 6. The release of reactive oxygen species and
its effects. Ischemia leads to the production of 2. Cerebral Palsy
reactive oxygen species, which in turn causes tissue - Chronic disability of the CNS characterized
damage and further cell death. by aberrant control of movement and
posture, appearing early in life and not as a
2. Neurotoxicity is secondary to increase in: result of a progressive neurologic damage
• Increase turnover of NA into MHPG (3- - Spastic diplegia
methoxy-4-hydroxyphenylglycol) - Pathway from intrapartum hypoxic-ischemic
• Excitatory amino acids injury to subsequent CP must progress
- Glutamate and aspartate through neonatal encephalopathy
• Adenosine and gamma aminobutyric acid - Why do we need to predict the development
of cerebral palsy?
This disease is usually detected around
1-2 years of age. Early detection and
intervention like physical therapy and
E. Resuscitation:Immediate Treatment of Asphyxia!
maternal counseling lead to less
1. Airway sequelae
2. Breathing 3. Epidemiology
- room air vs. 100% oxygen Neonatal encephalopathy
- bad effects of excessive oxygen: - Majority (70%) of NE due to events arising
decreased cerebral blood flow and
before labor
increased oxygen radicals
- new studies showing that room air H. Criteria to Define an Acute Intrapartum Event
leads to higher 5th minute APGAR Sufficient to Cause Cerebral Palsy
score, shorter time to first breath,
and less neurologic impairment Essential Criteria
3. Circulation Evidence of a metabolic acidosis in fetal umbilical arterial
4. Drugs cord blood obtained at delivery
Early onset of severe or moderate neonatal
F. Risks of Permanent Sequelae encephalopathy in infants at 34 or more weeks of
gestation
Table 2. Classifying the Degree of Encephalopathy to Cerebral palsy of the spastic quadriplegic or dyskinetic
Establish the “Pretest” Probability of Poor Outcome. type
Exclusion of other identifiable etiologies such as trauma,
coagulation disorders, infectious conditions or genetic
disorders
I. Possible Post Resuscitation Strategies
1. Hypothermia
Decrease of 2-6% below baseline
September 16, 2008 Tuesday Page 1 of 6
Iris. Hannie. Ezra. Dianne
OS 215 Reproductive Ma. Esterlita Villanueva-Uy
Neonatal Resuscitation and Depressed Infant Exam 2
Started <6 hours after hypoxic insult (eg. Dopamine) or
Decrease brain metabolism volume
Better neurologic outcome replacement
2. Selective Head Cooling (Gunn 1998) Kidneys • Acute • Monitor urine
In selective head cooling, the hypothermic baby tubular output
is said to have a band around his/her head that is acidosis • Restrict fluids if
maintained at a temperature of 33oC. oliguria is present
• Monitor serum
Infants Control (10) Minimal(6) Mild(6) electrolyte levels
CT scan Brain • Apnea • Monitor for apnea
Severe 1 2 0 • Seizures • Monitor glucose
Mild changes 4 1 2 and electrolyte
Normal 2 1 4 levels
EEG • Avoid
Abnormal 2 3 0 hyperthermia
Normal 4 2 6 • Consider
Dead 2 1 0 anticonvulsant
Severe 1 1 0 Gastroin- • Ileus • Delay initiation of
handicap testinal • Necrotizing feeding
Mild to 2 1 0 enterocolitis • Administer
moderate intravenous fluids
Normal at 6-12 5 2 6 • Consider
mos parenteral
nutrition
3. Whole Body Cooling (Shankaran Pediatrics Metabolic/ • Hypoglycemi • Monitor blood
2002) Hematolo- a glucose
Gic • Hypocalcemi • Monitor electrolyte
In a study done, it was noted that there were a/ levels
improvements in the following parameters: hypotension, Hyponatremi • Monitor hematocrit
renal failure, length of hospital stay, oxygen use, and a • Monitor platelets
seizures; however, the samples are still too small since it • Anemia
is an ongoing study.
• Thrombocyt
o-
Hypothermia (9)Normothermia (10)
penia
Hypotension 8 10
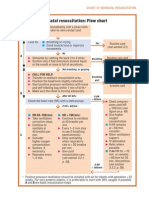
Neonatal Resuscitation Algorithm (next page)
PPHN 3 2
Renal failure 3 5
Hepatic dysfunction 1 1 Notes:
DIC 1 1 • Mnemonic for the first questions to ask:
Death 2 3 Nucleotides TACG
Days on oxygen 6.8 8.4 • Routine Care
Length of stay 14.9 21.6 o Warmth: Equipment to be used such as
Discharge status radiant warmers should be pre-warmed
Gavage feeding 0 2 before delivery
Abnormal Neuro exam 1 4 o Aiway: semi-sniffing head position (to
Seizure (on meds) 0 2 align airway, slightly chin-up)
Abnormal MRI 3 3 o Dry: dry with linen; replace wet linens
with dry ones
Table 3. Neonatal Postresuscitation Complications o Assessing Color: note for
and Actions acrocyanosis(pink but with pale
Organ Potential Post Resuscitation nailbeds) which may be secondary to
System Complication Action mechanical problems after birth
Lungs • Pulmonary • Maintain adequate • To stimulate: flick the toes or rub the back but
Hypertensio oxygenation and don’t take too long to avoid compromising the
n ventilation baby. If the baby doesn’t breathe immediately,
• Pneumonia • Consider assume secondary apnea.
• Pneumothor antibiotics • Things to assess to decide whether to resuscitate
ax • Delay oral feeding o Color
• Transient if respiratory o Heart/Pulse Rate
Tachypnea distress is evident o Respiration
• • Consider
Meconium
surfactant therapy
• PPV without chest compression
aspiration
o Breathe-2-3-breathe-2-3
syndrome
o 40 breaths/min
• Surfactant
o 100% O2 ideally
deficiency
• Types of Positive Pressure Ventilation
Cardiovas- • Hypotension • Monitor blood o Bagmask
cular pressure and Ambubag: self-inflating w/ one-
heart rate way valve therefore cannot be
• Consider inotrope used for free-flow O2
September 16, 2008 Tuesday Page 1 of 6
Iris. Hannie. Ezra. Dianne
OS 215 Reproductive Ma. Esterlita Villanueva-Uy
Neonatal Resuscitation and Depressed Infant Exam 2
Anesthesia Bag: needs O2 for
inflation Withdrawing resuscitation:
o Laryngeal mask: used when the baby • If there are no signs of life with continuous and
cannot be intubated adequate resuscitation, rescue efforts are
• PPV w/ Chest Compressions stopped after ten minutes
o Heart rate is checked for 6seconds
(multiplied by 10) because you have to Jeopardy Notes:
do everything in 30s. • Most important single step in resuscitation is
o Cadence: 1-and-2-and-3-and-breathe pulmonary ventilation
o 90 compressions,30 breaths per min • Three indications for PPV
• 2 Methods of Chest Compression 1. Apnea
o Two-finger: 1 hand at the back of the 2. Heart rate <100
baby for support; 3. Persistent cyanosis despite O2 support
Pointer + middle • Indications for chest compressions: HR<60 after
Middle+ ring 30 sec of PPV
o Two- thumb: more stable • Landmark for chest compressions: imaginary
*depth: 1/3 of AP diameter mammary line
• Epinephrine • Room air resuscitation is sometimes better than
o IV: 0.1ml/kg, 1cc syringe the 100% O2
o ET(endotracheal tube): 1ml/kg, 3-5cc • Best way to asses if endotracheal tube is in:
syringe (1:10,000 dilution) increase in HR
• Causes of bradycardia
o Adult: MI
o Child: Myocardial hypoxia secondary to
pulmonary cause
Neonatal Resuscitation Algorithm
If preterm:
A. Oxygenation
• O2 blender
• O2 sat goal 90-95%
• Ambu w/o reservoir: 40% (mixed w/ room air)
• Ambu w/ reservoir: roughly 100%
B. Thermoregulation
• Preterms are at risk for hypothermia
• Use radiant warmer, dry baby and replace wet
with dry linen
• If <28 weeks, ziplock is used as a warming back
September 16, 2008 Tuesday Page 1 of 6
Iris. Hannie. Ezra. Dianne
OS 215 Reproductive Ma. Esterlita Villanueva-Uy
Neonatal Resuscitation and Depressed Infant Exam 2
If meconium stained:
September 16, 2008 Tuesday Page 1 of 6
Iris. Hannie. Ezra. Dianne
You might also like
- Textbook of Neonatal Resuscitation 8th EditionDocument333 pagesTextbook of Neonatal Resuscitation 8th Editionmirandad784100% (1)
- NICU Manual Cheat SheetDocument2 pagesNICU Manual Cheat Sheetlori_quintal92% (13)
- Inpatient Obstetric Nurse Exam Prep 2020-2021: A New Study Guide for Certification Including 300 Test Questions and Answers with Full Explanations (RNC-OB)From EverandInpatient Obstetric Nurse Exam Prep 2020-2021: A New Study Guide for Certification Including 300 Test Questions and Answers with Full Explanations (RNC-OB)No ratings yet
- NRP Quizzes & AnswersDocument10 pagesNRP Quizzes & Answersmark_295100% (3)
- Preemies - Second Edition: The Essential Guide for Parents of Premature BabiesFrom EverandPreemies - Second Edition: The Essential Guide for Parents of Premature BabiesRating: 3.5 out of 5 stars3.5/5 (5)
- Manual de RCP - NEONATAL - 7°ED PDFDocument328 pagesManual de RCP - NEONATAL - 7°ED PDFNatanael Librado97% (29)
- Pediatric and Neonatal Mecanical Ventilation PDFDocument309 pagesPediatric and Neonatal Mecanical Ventilation PDFsdufhq100% (1)
- Patient Worksheet - NICU 2-PatientDocument2 pagesPatient Worksheet - NICU 2-PatientJerry G75% (4)
- NICU BrainDocument9 pagesNICU BrainSarah Boyce Cernik100% (1)
- Nicu Must KnowsDocument7 pagesNicu Must KnowsCyfern100% (2)
- Pediatric Potpourri 200+ New CPEN Questions: Certified Pediatric Emergency Nurse Review (3rd Edition Supplement)From EverandPediatric Potpourri 200+ New CPEN Questions: Certified Pediatric Emergency Nurse Review (3rd Edition Supplement)No ratings yet
- P.01D Foundations of Neonatal Resuscitation Part 1 & 2Document8 pagesP.01D Foundations of Neonatal Resuscitation Part 1 & 2Yndhira Xheyenn LayloNo ratings yet
- NEONATOLOGYDocument8 pagesNEONATOLOGYmymamym100% (1)
- NICU Pocket GuideDocument28 pagesNICU Pocket GuideCharles S. Williams RRT, AE-C86% (7)
- 7th Edition NRPDocument18 pages7th Edition NRPBenny WicaksonoNo ratings yet
- NRP Baby Saver III June 2011Document24 pagesNRP Baby Saver III June 2011nursesedNo ratings yet
- Neonatal Ventilation Made EasyDocument97 pagesNeonatal Ventilation Made EasyCảnh HoàngNo ratings yet
- Neonatal Resuscitation Program Flow ChartDocument3 pagesNeonatal Resuscitation Program Flow ChartChin Nam80% (5)
- Neonatal Ventilation - Basics of Mechanical Ventilation: Authors: Sam Wallis - Catriona FirthDocument21 pagesNeonatal Ventilation - Basics of Mechanical Ventilation: Authors: Sam Wallis - Catriona FirthEduardo Rios DuboisNo ratings yet
- NRP 8th Edition Advanced 1-11 Provider Curriculum Ecard Katya KirklandDocument1 pageNRP 8th Edition Advanced 1-11 Provider Curriculum Ecard Katya Kirklandapi-643862582No ratings yet
- Neonatal Lab InterpretationDocument18 pagesNeonatal Lab InterpretationWidelmark FarrelNo ratings yet
- Neonatal Pulmonary GraphicsDocument192 pagesNeonatal Pulmonary Graphicschetan100% (2)
- Nicu Survival Guide For ResidentsDocument26 pagesNicu Survival Guide For ResidentspeppepagNo ratings yet
- Certified Pediatric Emergency Nurse Review: Putting It All TogetherFrom EverandCertified Pediatric Emergency Nurse Review: Putting It All TogetherNo ratings yet
- Herpes Antidote UnlockedDocument125 pagesHerpes Antidote Unlockedfcuevaspr180% (5)
- Amniiotic Band Syndrome Cleft Lip/palate Congenital Limb Defects Duodenal AtresiaDocument18 pagesAmniiotic Band Syndrome Cleft Lip/palate Congenital Limb Defects Duodenal AtresiaMJ Amarillo100% (3)
- NICU Survival GuideDocument14 pagesNICU Survival Guidesedaka26No ratings yet
- Neonatal Resuscitation Program: 7 EditionDocument64 pagesNeonatal Resuscitation Program: 7 EditionStacy LuceroNo ratings yet
- NICU ProtocolDocument75 pagesNICU ProtocolCatherine Lee100% (6)
- Neonatal EmergenciesDocument123 pagesNeonatal EmergenciesMaria Babette Almazan Talavera100% (2)
- Mechanical Ventilation in NeonatesDocument60 pagesMechanical Ventilation in NeonatesZuhair Aldajani زهير عمر الدجاني100% (3)
- Neonatal Care Pocket Guide For Hospital Physicians PDFDocument319 pagesNeonatal Care Pocket Guide For Hospital Physicians PDFelmaadawy2002100% (7)
- Neonatal Ventilator Vent Set-Up CheatsheetDocument1 pageNeonatal Ventilator Vent Set-Up CheatsheetRick Frea50% (2)
- Admission To NICU CA4068v3Document12 pagesAdmission To NICU CA4068v3Hana ChristyantiNo ratings yet
- Complete Issue NeoReviewsDocument68 pagesComplete Issue NeoReviewsArvin E. PamatianNo ratings yet
- Neonatal Reurscitation PDFDocument347 pagesNeonatal Reurscitation PDFAlina Andreica100% (1)
- Respiratory Distress Management in NewbornDocument5 pagesRespiratory Distress Management in Newbornagirl_9807100% (1)
- Neonatal NotesDocument34 pagesNeonatal Notesgridchan100% (2)
- A Guide To The Newborn Intensive Care Unit (NICU)Document36 pagesA Guide To The Newborn Intensive Care Unit (NICU)Jean Wallace100% (3)
- Nicu Sheet Date: / / By: Sherif ElgamilyDocument1 pageNicu Sheet Date: / / By: Sherif ElgamilysherifNo ratings yet
- Stable 2Document115 pagesStable 2Avyel KramNo ratings yet
- Infection in NeonateDocument28 pagesInfection in Neonateamel015No ratings yet
- 2013 Neonatal HandbookDocument123 pages2013 Neonatal Handbookirmanikkimei100% (2)
- NRPDocument24 pagesNRPrajvikram8750% (6)
- Interpretting Neonatal Xrays (Click Enable Macros)Document304 pagesInterpretting Neonatal Xrays (Click Enable Macros)John Phamnguyen100% (5)
- NICU NurseDocument2 pagesNICU NursesojanNo ratings yet
- Neonatal Ventilation - Neocon 2017-2Document156 pagesNeonatal Ventilation - Neocon 2017-2RAM SOFTWARE100% (2)
- Neonatal ResucitationDocument47 pagesNeonatal ResucitationLeighton Ricardo WynterNo ratings yet
- Neonatal Ventilation PDFDocument29 pagesNeonatal Ventilation PDFIsabella HosanaNo ratings yet
- NMCSD Nicu 2015Document39 pagesNMCSD Nicu 2015Bibu BhaskarNo ratings yet
- DR Johnson On Neonatal Resuscitation Guidelines 041707Document44 pagesDR Johnson On Neonatal Resuscitation Guidelines 041707sameerarswNo ratings yet
- Neonatal Resuscitation ProgramDocument6 pagesNeonatal Resuscitation ProgramRick Frea100% (5)
- NRP PrestudyDocument14 pagesNRP Prestudynursesed100% (1)
- 66 Neonatal Resuscitation Show Notes 1Document3 pages66 Neonatal Resuscitation Show Notes 1Rabbani IcksanNo ratings yet
- Neonatal Resuscitation AH, AAPDocument15 pagesNeonatal Resuscitation AH, AAPAldair Cantillo BarriosNo ratings yet
- NEONATAL NURSE PRACTITIONER: Passbooks Study GuideFrom EverandNEONATAL NURSE PRACTITIONER: Passbooks Study GuideNo ratings yet
- NEONATAL INTENSIVE CARE NURSING: Passbooks Study GuideFrom EverandNEONATAL INTENSIVE CARE NURSING: Passbooks Study GuideNo ratings yet
- Nursing the NeonateFrom EverandNursing the NeonateMaggie MeeksNo ratings yet
- Quick Hits for Pediatric Emergency MedicineFrom EverandQuick Hits for Pediatric Emergency MedicineCristina M. Zeretzke-BienNo ratings yet
- Neonatal Nurse Practitioner A Complete Guide - 2020 EditionFrom EverandNeonatal Nurse Practitioner A Complete Guide - 2020 EditionNo ratings yet
- Boards SyllabusDocument14 pagesBoards Syllabus2012No ratings yet
- Diseases of The Anus Rev#1CDocument77 pagesDiseases of The Anus Rev#1C2012No ratings yet
- Boards SyllabusDocument14 pagesBoards Syllabus2012No ratings yet
- Fa Step 1 ScheduleDocument5 pagesFa Step 1 ScheduleDinesh DalviNo ratings yet
- ADA Summary of Guidelines 2011Document7 pagesADA Summary of Guidelines 2011IffatNaeemNo ratings yet
- CEBM Levels of EvidenceDocument2 pagesCEBM Levels of Evidence2012100% (2)
- The Division of Plastic SurgeryDocument36 pagesThe Division of Plastic Surgery2012No ratings yet
- Review Lectures Forlu6: Basic Eye Exam Common Opd Complaints Common Er Cases PharmacologyDocument110 pagesReview Lectures Forlu6: Basic Eye Exam Common Opd Complaints Common Er Cases Pharmacologyupmed2012block9No ratings yet
- CSAP Full 2002Document125 pagesCSAP Full 20022012No ratings yet
- Review of The Evidence For Herbal Medications and NutraceuticalsDocument5 pagesReview of The Evidence For Herbal Medications and Nutraceuticals2012No ratings yet
- HANDOUT - Vomiting in AdultsDocument3 pagesHANDOUT - Vomiting in Adults2012No ratings yet
- Organ Transplantation, Immunology and RejectionDocument2 pagesOrgan Transplantation, Immunology and Rejection2012No ratings yet
- American Diabetes Association (ADA) gUIDELINESDocument43 pagesAmerican Diabetes Association (ADA) gUIDELINESSamuel Rudolf Maranatha JulioNo ratings yet
- Pharma EvaluationDocument1 pagePharma Evaluation2012No ratings yet
- Patho Lab Trans - ButchDocument6 pagesPatho Lab Trans - Butch2012No ratings yet
- Trans Pulmopatho ColoredDocument8 pagesTrans Pulmopatho Colored2012No ratings yet
- OS 213 Pediatric AsthmaDocument8 pagesOS 213 Pediatric Asthma2012No ratings yet
- About BatsDocument200 pagesAbout BatsDbaltNo ratings yet
- Fapc Finals ReviewerDocument303 pagesFapc Finals ReviewerC BajamondeNo ratings yet
- Portal HypertensionDocument4 pagesPortal HypertensiondrstalamNo ratings yet
- Esophagus: Pipe or Gullet, Is An Organ in Vertebrates Through Which Food PassesDocument12 pagesEsophagus: Pipe or Gullet, Is An Organ in Vertebrates Through Which Food PassesCrow LordNo ratings yet
- Mengenal Aspergillosis, Infeksi Jamur Genus Aspergillus Uswatun HasanahDocument10 pagesMengenal Aspergillosis, Infeksi Jamur Genus Aspergillus Uswatun HasanahTiza JulyanNo ratings yet
- What Is Dairy RanchingDocument3 pagesWhat Is Dairy RanchingBright SamuelNo ratings yet
- Local Anesthesia Techniques in Oral and Maxillofacial SurgeryDocument102 pagesLocal Anesthesia Techniques in Oral and Maxillofacial Surgerydr_jamal1983No ratings yet
- Ingested Foreign BodyDocument18 pagesIngested Foreign BodyTeuku FaisalNo ratings yet
- Model Test One Structure and Written ExpressionDocument10 pagesModel Test One Structure and Written ExpressionEka KurniatiNo ratings yet
- Guidelines For The Identification Birds in ResearchDocument8 pagesGuidelines For The Identification Birds in ResearchadenadiaNo ratings yet
- 10.anatomy of Respiratory SystemDocument23 pages10.anatomy of Respiratory SystemMai Z HaniyaNo ratings yet
- Sterek - A Mating MoonDocument79 pagesSterek - A Mating MoonPaola GarciaNo ratings yet
- Biology 9 Science Al-Raza Institute Paper I Group-I Time Allowed: 20 Min Objective Marks: 12Document3 pagesBiology 9 Science Al-Raza Institute Paper I Group-I Time Allowed: 20 Min Objective Marks: 12Anonymous WDvB6A0No ratings yet
- Piis0894731715003879 PDFDocument49 pagesPiis0894731715003879 PDFDuoc Kien VangNo ratings yet
- Worm Infestation and HomoeopathyDocument15 pagesWorm Infestation and HomoeopathyDr. Rajneesh Kumar Sharma MD Hom100% (2)
- Rat DissectionDocument5 pagesRat DissectionAcidri AbdulkarimNo ratings yet
- Bmi Lab Viva QuestionDocument7 pagesBmi Lab Viva QuestionnijafancyNo ratings yet
- Practical Hematology ManualDocument48 pagesPractical Hematology ManualHaael88No ratings yet
- 5a - Osteology of Thorax - Intercostal SpacesDocument68 pages5a - Osteology of Thorax - Intercostal SpacesINTERNET MONEY HACKNo ratings yet
- Asuhan Keperawatan (Severe Acute Respiratory Syndrome) : Ns. Kristina., MSNDocument25 pagesAsuhan Keperawatan (Severe Acute Respiratory Syndrome) : Ns. Kristina., MSNMuhammad Sofyan NurNo ratings yet
- Module 11Document7 pagesModule 11Jamille Nympha C. BalasiNo ratings yet
- Animal Testing Rough DraftDocument6 pagesAnimal Testing Rough Draftapi-645494061No ratings yet
- WT Classifieds 230714Document5 pagesWT Classifieds 230714Digital MediaNo ratings yet
- Lacunar Infarct - Radiology Reference Article - RadiopaediaDocument8 pagesLacunar Infarct - Radiology Reference Article - RadiopaediaRismanto TorsioNo ratings yet
- Cara Baca Foto ThoraxDocument23 pagesCara Baca Foto ThoraxNofilia Citra CandraNo ratings yet
- Blood and Blood Components CollectionDocument33 pagesBlood and Blood Components CollectionAbas Rashid BhatNo ratings yet
- Papular UrticariaDocument10 pagesPapular UrticariaNuri Sakina SuhartoNo ratings yet
- AQA Biol A Unit 1 Jan02Document20 pagesAQA Biol A Unit 1 Jan02Raymond RayNo ratings yet
- Protozoa PowerpointDocument36 pagesProtozoa PowerpointHarriza Macapundag Haron-GangcoNo ratings yet