Professional Documents
Culture Documents
Ca Cervix
Uploaded by
Vinisia TakaraiOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Ca Cervix
Uploaded by
Vinisia TakaraiCopyright:
Available Formats
Ca cervix
Background
Cervical cancer is the second most common malignancy in women worldwide, and it remains a leading cause of cancer-related death for women in developing countries. In the United States, cervical cancer is relatively uncommon. (See Epidemiology.) The incidence of invasive cervical cancer has declined steadily in the United States over the past few decades; however, it continues to rise in many developing countries. The change in the epidemiological trend in the United States has been attributed to mass screening with Papanicolaou tests. Because women are screened routinely, the most common finding is an abnormal Papanicolaou test result (see Clinical). The complete evaluation for cervical cancer should include a Papanicolaou test with cytobrush and endocervical and endometrial samplings. If the smear result is suggestive of adenocarcinoma in situ, a cone biopsy should be performed. (See Workup.) The treatment of cervical cancer varies with the stage of the disease. For early invasive cancer, surgery is the treatment of choice. In more advanced cases, radiation combined with chemotherapy is the current standard of care. In patients with disseminated disease, chemotherapy or radiation provides symptom palliation. (See Treatment.)
Etiology
Early epidemiological data demonstrated a clear association between cervical cancer and sexual activity. Major risk factors observed were sex at a young age, multiple sexual partners, promiscuous male partners, and history of sexually transmitted diseases. However, the search for a potential sexually transmitted carcinogen was unsuccessful until breakthroughs in molecular biology enabled scientists to detect viral genome in cervical cells. Strong evidence now implicates human papillomaviruses (HPVs) as prime suspects.[1, 2, 3] HPV viral DNA has been detected in more than 90% of squamous intraepithelial lesions (SILs) and invasive cervical cancers compared with a consistently lower percentage in controls. Both animal data and molecular biologic evidence confirm the malignant transformation potential of papilloma virusinduced lesions. SILs are found predominantly in younger women, while invasive cancers are detected more often in women 10-15 years older, suggesting slow progression of cancer. HPV infection occurs in a high percentage of sexually active women. Most of these infections clear spontaneously within months to a few years, and only a small proportion progress to cancer. This means that other crucial factors must be involved in the process of carcinogenesis. Three main factors have been postulated to influence the progression of low-grade SILs to high-grade SILs. These include the type and duration of viral infection, with high-risk HPV
type and persistent infection predicting a higher risk for progression; host conditions that compromise immunity, such as multiparity or poor nutritional status; and environmental factors such as smoking, oral contraceptive use, or vitamin deficiencies. In addition, various gynecologic factors significantly increase the risk for cervical cancer. These include early age of first intercourse and higher number of sexual partners.
Human papillomavirus
HPV is a heterogeneous group of viruses that contain closed circular double-stranded DNA. The viral genome encodes 6 early open reading frame proteins (ie, E1, E2, E3, E4, E6, E7), which function as regulatory proteins, and 2 late open reading frame proteins (ie, L1, L2), which make up the viral capsid. To date, 77 different genotypes of HPV have been identified and cloned, among which types 6, 11, 16, 18, 26, 31, 33, 35, 39, 42, 43, 44, 45, 51, 52, 53, 54, 55, 56, 58, 59, 66, and 68 have the propensity to infect anogenital tissues. The HPVs that infect the human cervix fall into 2 broad risk categories. The low-risk types, HPV 6b and 11, are associated with low-grade SILs but are never found in invasive cancer. The high-risk types, mostly HPV 16 and 18, are found in 50-80% of SILs and in up to 90% of invasive cancers. Although less common, types 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68, 73, and 82 should also be considered carcinogenic. The major difference between the 2 types is that after infection, the low-risk HPVs are maintained as extrachromosomal DNA episomes, while the high-risk HPV genome is found integrated into the host cellular DNA. The recombination event often leaves E6 and E7 directly coupled to the viral promoter and enhancer sequences, allowing their continued expression after integration. Because E7 binds and inactivates the Rb protein while E6 binds p53 and directs its degradation, the functional loss of both TP53 and the RB genes leads to resistance to apoptosis, causing uncensored cell growth after DNA damage. This ultimately results in progression to malignancy.
Human immunodeficiency virus
The role of human immunodeficiency virus (HIV) infection in the pathogenesis of cervical cancer is not fully understood. Studies have shown a higher prevalence of HPV infection in HIV-seropositive women than in seronegative women, and the HPV prevalence was directly proportional to the severity of immunosuppression as measured by CD4 counts. Impaired lymphocyte function has been postulated to enhance latent or subclinical HPV activity, resulting in a higher rate of persistent infection. Whether HIV has a synergistic effect on HPV infection, either by direct molecular interaction or through an indirect immunologic effect, remains unclear.
Epidemiology
Cervical cancer is the second most common malignancy in women worldwide, and it remains a leading cause of cancer-related death for women in developing countries. In the United States, cervical cancer is relatively uncommon. The incidence of invasive cervical cancer has declined steadily in the United States over the past few decades; however, it continues to rise in many developing countries. The change in the epidemiological trend in the United States has been attributed to mass screening with Papanicolaou tests.[4] The American Cancer Society estimated that in the United States in 2010, 12,200 new cases of cervical cancer would be diagnosed.[5] In addition, more than 50,000 cases of carcinoma in situ are diagnosed each year. Internationally, 500,000 new cases are diagnosed each year. Unlike the United States, where the annual incidence is 6.8 cases or less per 100,000 women, rates in parts of South America and Africa range as high as 52.8 cases per 100,000 women.[6]
Race- and age-related demographics
In the United States, cervical cancer is more common in Hispanic, African American, and Native American women than in white women. The Center for Disease Control and Preventions Surveillance of Screening-Detected Cancers (Colon and Rectum, Breast, and Cervix)United States, 20042006 reported that incidence rates of late-stage cervical cancer were highest among women aged 50-79 years and Hispanics.[7] However, cervical cancer may be diagnosed in any woman of reproductive age.
Prognosis
Prognosis of cervical cancer depends on disease stage. In general, the 5-year survival rates are as follows:
Stage I - Greater than 90% Stage II - 60-80% Stage III - Approximately 50% Stage IV - Less than 30%
The American Cancer Society estimated that 4,210 women would die of cervical cancer in the United States in 2010.[5] This represents 1.3% of all cancer deaths and 6.5% of deaths from gynecologic cancers.
Patient Education
Cervical cancer is overrepresented among underserved and minority groups in the United States. It is imperative to increase awareness about the benefits of Papanicolaou test screening in these groups. A Cochrane review found that the best approach to encourage women to undergo cervical screening involved invitations, such as fixed or open appointments, letters, telephone calls, verbal recommendations, prompts, and follow-up letters.[8] However, these findings relate to screening in developed countries, and their relevance to developing countries is unclear. Further studies are required to determine the effectiveness of promising interventions, such as revealing in an invitation letter the gender of the smear taker, using a health promotion nurse, the use of lay outreach health workers, and intensive attempts at recruitment.
For patient education information, see the Cancer and Tumors Center, Women's Health Center, and Procedures Center, as well as Cervical Cancer, Pap Smear, and Colposcopy.
You might also like
- Kanker ServiksDocument13 pagesKanker ServiksVhiaLiviaNo ratings yet
- Cervical Cancer: Emedicine Specialties Obstetrics and Gynecology Gynecologic OncologyDocument19 pagesCervical Cancer: Emedicine Specialties Obstetrics and Gynecology Gynecologic OncologyFatah Abdul YasirNo ratings yet
- Cervical Cancer - A Global Health CrisisDocument9 pagesCervical Cancer - A Global Health Crisispb.nakulaNo ratings yet
- RRLDocument6 pagesRRLsheenayeahNo ratings yet
- Cervical CancerDocument27 pagesCervical CancerHanif RezaNo ratings yet
- Review ArticleDocument12 pagesReview ArticleNoka YogaNo ratings yet
- KarsinomaDocument12 pagesKarsinomaWahyudi Pratama HarliNo ratings yet
- CANCER Preventing Cervical CancerDocument4 pagesCANCER Preventing Cervical CancerLeonardo Rodríguez BottacciNo ratings yet
- Molecular Pathogenesis of Cervical CancerDocument13 pagesMolecular Pathogenesis of Cervical CancerKamilah NasarNo ratings yet
- Wjco 5 744 PDFDocument10 pagesWjco 5 744 PDFFlorencia Irena GunawanNo ratings yet
- Iva Screening2Document9 pagesIva Screening2ponekNo ratings yet
- Cervical Intraepithelial NeoplasiaDocument16 pagesCervical Intraepithelial Neoplasiaalejandro fernandezNo ratings yet
- Cervical CA Proposal Jan152010Document21 pagesCervical CA Proposal Jan152010redblade_88100% (2)
- Cervical CADocument10 pagesCervical CAAby ShauNo ratings yet
- Guidelines for Cervical Cancer ScreeningDocument3 pagesGuidelines for Cervical Cancer ScreeningKen WayNo ratings yet
- Historia Natural Del HPVDocument5 pagesHistoria Natural Del HPVpatologiacervicalupcNo ratings yet
- Kessler 2017Document12 pagesKessler 2017Hary BudiartoNo ratings yet
- Cervical Cancer: Prevention, Diagnosis, and TherapeuticsDocument23 pagesCervical Cancer: Prevention, Diagnosis, and TherapeuticsranggadrNo ratings yet
- Human Papillomavirus in The HIV-Infected Host - EpidemiologyDocument10 pagesHuman Papillomavirus in The HIV-Infected Host - EpidemiologyRenan RodriguesNo ratings yet
- 1 s2.0 S2050052119301015 MainDocument10 pages1 s2.0 S2050052119301015 MainELSA DÍAZ LÓPEZNo ratings yet
- Pap IntroductionDocument390 pagesPap IntroductionAnish VeettiyankalNo ratings yet
- ObGyn Secrets, 3rDocument1 pageObGyn Secrets, 3rCahyadi PangemananNo ratings yet
- Ca CervixDocument20 pagesCa CervixNathy MontoyaNo ratings yet
- HPV Testing Reduces Unneeded Visits and Extends Cancer PreventionDocument16 pagesHPV Testing Reduces Unneeded Visits and Extends Cancer PreventionSilvia Cerda RodríguezNo ratings yet
- Stewart 2019Document6 pagesStewart 2019tika apriliaNo ratings yet
- Cervicalcancerprevention: Immunization and Screening 2015Document9 pagesCervicalcancerprevention: Immunization and Screening 2015behanges71No ratings yet
- 10 1097@aog 0000000000001708Document20 pages10 1097@aog 0000000000001708oodarkfireooNo ratings yet
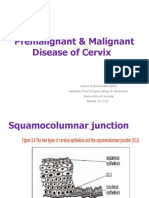
- Premalignant & Malignant Disease of CervixDocument64 pagesPremalignant & Malignant Disease of CervixDegefaw BikoyNo ratings yet
- Nejmcp 2108502Document9 pagesNejmcp 2108502Manuel GilNo ratings yet
- 01 Mike Global ImpactDocument8 pages01 Mike Global ImpactDeviati Juwita SariNo ratings yet
- Project Title High Risk HPV Genotyping in Patient With Clinically Suspected Precancerous and Cancerous Lesions of CervixDocument16 pagesProject Title High Risk HPV Genotyping in Patient With Clinically Suspected Precancerous and Cancerous Lesions of CervixEmam MursalinNo ratings yet
- Cancer de PeneDocument12 pagesCancer de PeneAndelcass DellNo ratings yet
- Bullet Point CANCER CervicouterinoDocument20 pagesBullet Point CANCER CervicouterinoDaniela DuránNo ratings yet
- Human Papillomavirus Disease: EpidemiologyDocument30 pagesHuman Papillomavirus Disease: EpidemiologyGabriela LemNo ratings yet
- Breast CancerDocument29 pagesBreast CancerSherly CanceritaNo ratings yet
- Malignancy ReportDocument52 pagesMalignancy Reportapi-3758497No ratings yet
- ACOG Cervical Cancer ScreeningDocument20 pagesACOG Cervical Cancer ScreeningAlan Ahlawat SumskiNo ratings yet
- HPV Vaccination Against Cervical Cancer in Women Above 25 Years of AgeDocument9 pagesHPV Vaccination Against Cervical Cancer in Women Above 25 Years of Agegringo6969No ratings yet
- Improvement of Cervical Cancer TherapyDocument1 pageImprovement of Cervical Cancer TherapyFree Escort ServiceNo ratings yet
- Low Risk of Cervical Cancer Precancer Among Most.3Document11 pagesLow Risk of Cervical Cancer Precancer Among Most.3Yosie Yulanda PutraNo ratings yet
- Secondary Prevention of CancerDocument8 pagesSecondary Prevention of CancerlilianadasilvaNo ratings yet
- Current Status of Knowledge, Attitude and Practice (KAP) and Screening For Cervical Cancer in Countries at Different Levels of DevelopmentDocument7 pagesCurrent Status of Knowledge, Attitude and Practice (KAP) and Screening For Cervical Cancer in Countries at Different Levels of DevelopmentHuzaifa SaeedNo ratings yet
- Seminars in Oncology NursingDocument9 pagesSeminars in Oncology NursingangelitostorresitosNo ratings yet
- Case Study of Cervical Cancer Stage III (Final)Document82 pagesCase Study of Cervical Cancer Stage III (Final)DRJC94% (32)
- Ovarian Cancer - StatPearls - NCBI BookshelfDocument13 pagesOvarian Cancer - StatPearls - NCBI BookshelfeeeeeeNo ratings yet
- Screening Guidelines for Preventing Cervical CancerDocument16 pagesScreening Guidelines for Preventing Cervical CancerLis RibeiroNo ratings yet
- RH Fs Risk FactorsDocument2 pagesRH Fs Risk FactorsfentroispNo ratings yet
- Nej MCP 2108502Document9 pagesNej MCP 2108502Marialejandra GuevaraNo ratings yet
- Ca MamaeDocument7 pagesCa MamaeKevin RadittyaNo ratings yet
- Cervical Cancer A Review On Young WomenDocument5 pagesCervical Cancer A Review On Young WomenKIU PUBLICATION AND EXTENSIONNo ratings yet
- Cervical Cancer - An Overview of Pathophysiology and ManagementDocument9 pagesCervical Cancer - An Overview of Pathophysiology and ManagementIndah 15No ratings yet
- Cervical CancerDocument6 pagesCervical CancerJohndave CazarNo ratings yet
- Aetiology, Pathogenesis, and Pathology of Cervical NeoplasiaDocument9 pagesAetiology, Pathogenesis, and Pathology of Cervical NeoplasiaKamilah NasarNo ratings yet
- Testicular Cancer Cure Saves $150M AnnuallyDocument26 pagesTesticular Cancer Cure Saves $150M AnnuallyFeddyFebriyantoManurungNo ratings yet
- Multifactorial DiseaseDocument17 pagesMultifactorial Diseasepratibha mishraNo ratings yet
- VPH CancerDocument4 pagesVPH CancerJader Aldair Pavon GomezNo ratings yet
- ESMO Relapsed Ovarian CaDocument9 pagesESMO Relapsed Ovarian CasusdoctorNo ratings yet
- Cervical Cancer ESMODocument12 pagesCervical Cancer ESMOAndrei CorhaNo ratings yet
- Description: Cervical Cancer IsDocument22 pagesDescription: Cervical Cancer IsmeanneclavioNo ratings yet
- FOLLOW UPDocument1 pageFOLLOW UPVinisia TakaraiNo ratings yet
- FOLLOW UPDocument1 pageFOLLOW UPVinisia TakaraiNo ratings yet
- FOLLOW UPDocument1 pageFOLLOW UPVinisia TakaraiNo ratings yet
- Suikoden II 2 Recruiting 108 Stars of Destiny ListDocument2 pagesSuikoden II 2 Recruiting 108 Stars of Destiny ListVinisia TakaraiNo ratings yet
- Evaluation of Fetal DeathDocument9 pagesEvaluation of Fetal DeathVinisia TakaraiNo ratings yet
- Brosur Sy135cDocument9 pagesBrosur Sy135cDenny KurniawanNo ratings yet
- Alcon Capacitor AC Mp4aDocument6 pagesAlcon Capacitor AC Mp4aDAC Secretary EENo ratings yet
- Maize Package of Practices in BriefDocument3 pagesMaize Package of Practices in Briefkomandla venkatkiran reddyNo ratings yet
- Research Article (Lavandula Angustifolia) Essential Oil On: Effect of Lavender Acute Inflammatory ResponseDocument10 pagesResearch Article (Lavandula Angustifolia) Essential Oil On: Effect of Lavender Acute Inflammatory ResponseAndreeaNo ratings yet
- Đánh giá chế độ ăn kiêng: Nhịn ăn gián đoạn để giảm cân- wed HarvardDocument14 pagesĐánh giá chế độ ăn kiêng: Nhịn ăn gián đoạn để giảm cân- wed HarvardNam NguyenHoangNo ratings yet
- Organization Structure Training KAJARIADocument30 pagesOrganization Structure Training KAJARIAViswanth GanaparthiNo ratings yet
- Homework Helpers - Chemistry PDFDocument311 pagesHomework Helpers - Chemistry PDFTamby100% (1)
- Pancreatic NekrosisDocument8 pagesPancreatic Nekrosisrisyda_mkhNo ratings yet
- Real Possibility of Future ConditionDocument3 pagesReal Possibility of Future ConditionHusNo ratings yet
- 2019 Torch and Consumables Catalog: For Mechanized Plasma SystemsDocument64 pages2019 Torch and Consumables Catalog: For Mechanized Plasma SystemsRaj DomadiyaNo ratings yet
- STPM Chemistry Topic 16 Haloalkanes Short Notes PDFDocument2 pagesSTPM Chemistry Topic 16 Haloalkanes Short Notes PDFbendanNo ratings yet
- Electronics Meet Animal BrainsDocument44 pagesElectronics Meet Animal BrainssherrysherryNo ratings yet
- Xoro Hrs 8540 HD Sat ReceiverDocument33 pagesXoro Hrs 8540 HD Sat ReceiverPinoNo ratings yet
- Masterbrand Guidelines - September 2012: Confidential - For Internal Use OnlyDocument35 pagesMasterbrand Guidelines - September 2012: Confidential - For Internal Use OnlyDemerson CamposNo ratings yet
- Sherco 450 Se R Workshop Manual 1Document79 pagesSherco 450 Se R Workshop Manual 1miguelNo ratings yet
- Indo American Journal of Pharmaceutical Research (India)Document4 pagesIndo American Journal of Pharmaceutical Research (India)Pharmacy2011journalsNo ratings yet
- Analytical Methods To Measure The Constants of Fats and OilsDocument5 pagesAnalytical Methods To Measure The Constants of Fats and OilsPenicillium Notatum67% (3)
- IB Chemistry HL Test 2nd FEBDocument13 pagesIB Chemistry HL Test 2nd FEBprasad100% (1)
- Lea 2 PDFDocument21 pagesLea 2 PDFKY Renz100% (1)
- The Focus Shooting Method CourseDocument48 pagesThe Focus Shooting Method CourseKobiXDNo ratings yet
- Msds PentaneDocument6 pagesMsds PentaneMuhammad FikriansyahNo ratings yet
- Malaria Epidemiology & PreventionDocument92 pagesMalaria Epidemiology & PreventionritikaritikaNo ratings yet
- Radiesse Pálpebras Gox-8-E2633Document7 pagesRadiesse Pálpebras Gox-8-E2633Camila CrosaraNo ratings yet
- Ichroma™ COVID-19 Ab (With Ichroma™ II Reader) Test SystemDocument6 pagesIchroma™ COVID-19 Ab (With Ichroma™ II Reader) Test SystemGopinath AgnihotramNo ratings yet
- Contemporary Philippine Arts From The Regions: Quarter 3Document15 pagesContemporary Philippine Arts From The Regions: Quarter 3Ackie Inacay RosarioNo ratings yet
- Service and Repair Instructions: Water & WastewaterDocument72 pagesService and Repair Instructions: Water & WastewaterLa Marina Mantenimiento100% (1)
- Swami Brahmananda - The Spiritual Son of Sri RamakrishnaDocument7 pagesSwami Brahmananda - The Spiritual Son of Sri RamakrishnaEstudante da Vedanta100% (2)
- 0580 w15 QP 42Document16 pages0580 w15 QP 42Shahrizan Noor100% (1)
- El DoradoDocument12 pagesEl Doradoandrewwilliampalileo@yahoocomNo ratings yet
- COMPRESSED AIR VALIDATION SYSTEMDocument13 pagesCOMPRESSED AIR VALIDATION SYSTEMbpharmba100% (5)