Professional Documents
Culture Documents
4th Revised RRL
Uploaded by
Joshua ArcairaOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
4th Revised RRL
Uploaded by
Joshua ArcairaCopyright:
Available Formats
DE LA SALLE HEALTH SCIENCES INSTITUTE COLLEGE OF MEDICINE DEPARTMENT OF FAMILY AND COMMUNITY MEDICINE CM2 SY 2011-2012 OUTPUT 2: REVIEW
W OF RELATED LITERATURE (REVISED) Group 1A, Dr. Jovilia M. Abong Research Question: Among students aged 13-14 with allergic rhinitis of selected schools in Dasmarias, Cavite, will exposure to air-conditioned school rooms affect the severity of their allergic rhinitis? General Objective: To determine if the exposure to the air-conditioning system affects the severity of allergic rhinitis in high school students, aged 13-14, of selected schools in Dasmarias, Cavite. y Specific Objectives: o To identify the prevalence of allergic rhinitis among high school students, aged 13-14, of selected schools in of Dasmarias, Cavite based on their exposure to air-conditioned rooms. o To identify the prevalence of allergic rhinitis among high school students, aged 13-14, of selected schools in Dasmarias, Cavite based on their exposure to non-air-conditioned classrooms. o To determine the severity of allergic rhinitis according to ARIA classifications. o To identify the risk factors of allergic rhinitis present in the classroom or school, such as pollen, molds, and cockroaches. o To determine the number of hours exposed to the classroom with or without airconditioning system according to ARIA classifications. o Compare the severity of allergic rhinitis in students who are exposed to air-conditioned classrooms and those who are not exposed to air-conditioned classrooms. Background Information Regarding the Research Question: According to a demographic and epidemiologic study by Settipane, allergic rhinitis affects more than 20% of the American population. [1] This percentage is alarming on its own, making allergic rhinitis fairly common among the population. Furthermore, it was observed by the ISAAC (International Study of Allergy and Asthma in Children) that the Philippines was ranked with the highest prevalence rate of common allergies (rhinitis and asthma) - encompassing countries like Thailand, Indonesia, and South Korea. These studies have triggered interest into the disease and have inspired us to study the disease further as well. [2] From the same study by the ISAAC, they discovered that among Filipino teenagers, 13-14 yearolds presented with the highest prevalence rate among age groups with 32.5% of them having allergic rhinitis. [2] Hence, our study will be focusing on the specific age group mentioned. Ventilation and air-conditioning systems can be sources of microbial aerosols either from contaminated air entering the system or directly from microbial growth within the system. Poor ventilation may allow an accumulation of particulates, pollutants, and allergens inside school buildings and decreased air circulation may increase transmission of respiratory infections. Building structural problems, such as heating or air conditioning systems venting near an air intake may contribute to these exposures. Due to this, the associations between school absenteeism and poor ventilation, vermin, and 1
cumulative exposure to building condition problems are greater for younger students. Young children, aged 5 to 18 years old, are also known to be more susceptible to airborne pollutants than adults because of their greater activity, smaller airways, and faster ventilation rates.[3] Therefore, it is important to look into which of the learning environments is more likely to help students achieve their full potential and keep them healthy. According to Meltzer, approximately one in five children will develop symptoms of allergic rhinitis by two to three years of age. In children who are six years of age, about 40% of them will have symptoms and up to 30% will be affected during their adolescence. [4] Furthermore, a study by Blaiss pointed out that allergic rhinitis can interfere with a childs daily activities such as learning in school. It also affects a childs behavior and psychosocial health thus affecting the childs quality of life overall. Due to this, a consensus panel was formed in 2004 to assess the impact allergic rhinitis has on school children and determine how to improve prevention and treatment, so an affected childs quality of life and school performance could improve. One of the things they considered in this consensus is that poor environmental conditions, such as places that have inadequate ventilation or poor indoor quality, can exacerbate allergic rhinitis. It is advised that the best way to prevent allergic rhinitis from occurring is by providing clean indoor environments that will reduce the amount of allergens present indoors. This includes having an air-conditioning system and proper ventilation. [4], [5] Research Hypothesis: Exposure to air-conditioned rooms alleviates the symptoms and occurrence of allergic rhinitis and poor ventilation leads to its severity. Summary of Current Knowledge Regarding Disease and Exposure of Interest Short Description and Symptomatology of Allergic Rhinitis Allergic rhinitis (AR), a common chronic disease, is actually a collection of symptoms that include primarily the nose and eyes. [6] From the study done in Tehran among 7-18 years old, it is observed that rhinorrhea, rhinitis, sneezing, eye itching and nose itching are the most common with rhinorrhea as the most prevalent. [7] Aside from these symptoms, teary eyes, nasal congestion, post nasal drip are also included. AR is perennial, seasonal or perennial with seasonal exacerbation. According to the study done by Cauwenberge et. al., perennial AR is more difficult to define as chronic structural airway changes are more difficult to establish and recurrent infections can mimic some of the presentations of this disease. [8] When we say allergy, it is something that is triggered by an allergen which could come in different forms. It could be pollen, dust, smoke, or even pet fur. When these allergens are brought into our respiratory tract especially through our nose, it can cause an allergic reaction where the body releases chemicals such as histamine which causes inflammatory disease of the nasal mucosa induced by an Ig E mediated reaction. [9] But according to De-Yun Wang of National University of Singapore, genetic background in terms of a family history of atopic disease has been the strongest risk factor for the development of allergic symptoms, irrespective of the varying prevalence and environmental risk factors in different societies. The most convincing evidence for genetic effect in the development of atopy is derived from twin studies. And Wang concluded that atopy is a key condition in the development of allergic diseases, particularly with the Ig E-mediated mechanism. It is a disorder with strong familial tendency, usually starting in childhood or adolescence, when patients become sensitized and produce Ig E antibodies in response to ordinary allergens. [10] 2
Global Burden of Allergic Rhinitis Accurate records on the prevalence of allergic rhinitis are lacking before the 20th century. A study done on college students by Settipane et. al. showed that 64% of 1836 students originally tested 23 years ago were followed up. Seventeen new cases of asthma (10.5%) have developed in the 162 subjects who previously suffered from seasonal AR. Nineteen new cases of asthma (3.6%) had developed in the 528 subjects without previous symptoms. Subjects without symptoms but had previous positive skin prick tests were somewhat more likely to have developed asthma compared to people with negative tests (10.6% versus 3.2%). [8], [11] Although there are differences among countries, the incidence and prevalence of asthma and rhinitis is increasing worldwide.[12] Both developed and developing countries worldwide have dramatically rising prevalence of allergic disease which includes asthma; rhinitis; anaphylaxis; drug, food, and insect allergy; eczema; urticaria (hives) and angioedema. This is problematic for children because they are the ones who bear the greatest burden of the rising trend over the last two decades. In spite of the increase, even in developed countries, services for patients with allergic diseases are fragmented and far from ideal. Very few countries have comprehensive services in this field of medicine. [13] Treatment of AR is expensive; costing over 1,000 per individual per year in Germany. In addition, as the disease progresses its severity to severe asthma, the cost also rises by a staggering seven-fold increase. This increase is accounted for by second generation antihistamine medications which are better in efficacy but are more expensive. [14] Furthermore, there are almost no specialized services for these patients in numerous countries. Care and medications are mainly provided by organ-based specialists such as respiratory physicians, ear, nose and throat specialists (otorhinolaryngologists), and dermatologists. Even though the care given is mostly adequate, it is still somehow inadequate because such specialists generally view allergy only through their organ of interest. There is a vast majority of patients who have allergic disease in multiple organs, which may thus be overlooked. For example, AR, conjunctivitis, and asthma are three problems which commonly manifest together, yet affect three different organ systems. [13] Because the prevalence of allergy has increased to such an extent, allergy must be regarded as a major healthcare problem. The significant impact of AR is based on the degree of severity of the symptoms. It has several consequences which includes psychological effects that affect social interactions. This affectation creates an impact, not only on the subject, but for the family as well. According to World Health Organization (WHO) statistics, hundreds of millions of subjects in the world suffer from rhinitis and it is estimated that 300 million have asthma, which as aforementioned markedly affects the quality of life of these individuals and their families. This also negatively impacts the socioeconomic welfare of society. [13] The provision of allergy care must be led by allergy specialists so that an adequate standard of care is achieved for all patients with these diseases. The lack of such care leads to avoidable morbidity and mortality and to substantial increased and unnecessary cost to health care systems and national budgets. For example, it is estimated by WHO that 250,000 avoidable asthma deaths occur in the world each year. Because so little effort is made to provide clinical services for patients who suffer from allergies, they often seek non-scientifically-based alternative and complementary diagnostic and therapeutic remedies for their ailments. One of the main aspects of good allergy practice is to find the cause and prevent symptoms and disease progression, rather than just rely on medications to suppress the symptoms. [13]
Triggers of Allergic Rhinitis
According to Busse, an allergic reaction is usually caused by an allergen. In the cases of people with allergic rhinitis, when they breathe in these allergens such as pollens or dust, these cause their bodies to release certain chemicals like histamine, bradykinin, and the like. These chemicals cause the persons with AR to experience symptoms of allergic reactions such as itching, swelling, and mucous production. Pollens that cause AR may differ depending on the person who inhales such pollens. Usually the smaller, hard-to-see pollens cause AR more often than the bigger ones. Examples of plants that produce the said pollens are deciduous and evergreen trees, grasses, and ragweed. Development of symptoms may depend on the amount of pollen present in the air. During dry, hot, windy days there may be more pollens present in the air thus, the increasing the probability of developing symptoms of AR. However, during cool, damp, rainy days pollens may not be abundant in the air since they would most likely be washed in the ground. Reactions to allergens may also include eczema and asthma which are also part of the allergic reaction. The most common cause of developing AR is still genetic in nature. The chance of having AR is high if both parents have the disease. [15] Togias stated that inflammatory mediators produced by mast cells that are activated by antigenIgE cause the symptoms of AR. The mediators directly or indirectly target the end organs. For example, the histamine released by mast cells stimulates the sensory nerves which lead to sneezing, pruritus, rhinorrhea, and nasal congestion. Symptoms may also arise due to the phenomenon of hyperresponsiveness to non-allergenic stimuli like cold air and other irritants. The phenomenon is believed to have arisen from the allergic inflammation on the sensory nerves that supply the mucosa of the upper respiratory tract mucosa. Different kinds of non-allergenic triggers were shown to act on the nasal mucosa by the means of sensorineural stimulation. The responsiveness to these stimuli is also heightened in AR compared to healthy individuals. Also, stimulation of sensory nerves can produce inflammatory changes in AR. Such inflammation is called neurogenic inflammation but the mechanism behind this is not yet known. However, Alkis also stated that evidence exists that neurotrophin nerve growth factor, the one responsible for the changes in the sensory nerves, is found in elevated levels in the nasal secretions of persons with perennial AR compared to healthy individuals. The nerve growth factor is also acutely released into nasal fluids after being triggered by allergens in patients with allergic disease. AR is also very common among patients with asthma of atopic origin. [16] Severity of Allergic Rhinitis Allergic rhinitis has been classified into two according to its severity: namely, mild and moderate/severe. The difference between the two classifications of AR is seen in the impact of the illness to the patients regular daily activities. In moderate/severe AR, daily activities are impaired and sleep is disturbed because of its troublesome symptoms. On the other hand, the symptoms of mild AR are tolerable enough so as not to impair the activities of the person. To add, AR can be further classified based on the duration of symptoms manifested by the patient intermittent and persistent. Intermittent AR occurs when symptoms last less than four (4) days per week or less than four (4) consecutive weeks while the persistent type happens when the symptoms manifest more than four (4) days per week or for more than four (4) consecutive weeks. [17]
Figure 1. A diagrammatic representation of the classifications of AR. Risk Factors and Possible Confounding Variables of the Study Allergens/Irritants Allergens and irritants present in the environment are part of the confounding variables of the study. One of the allergens that commonly trigger allergic rhinitis is pollen. In a cohort study conducted in Sweden in 2003, it has been identified that pollen accounted for seventy-three percent (73%) of the trigger factors that cause Allergic Rhinitis. [18] Moreover, the incidence of allergic disease has been thought to be constantly increasing [19] and this has been attributed to the increased exposure of children to air pollution, probably because of the presence of particulates in the air. [20] Number of hours spent in air-conditioned rooms and non air-conditioned rooms Since one of the objectives of the research is to see whether or not air-conditioned rooms can help alleviate allergic rhinitis, the number of hours is a confounder to our study. A cross-sectional study conducted in Taiwan shows that persistent exposure to nitric oxides, carbon monoxide, and sulfur dioxide may increase the prevalence of allergic rhinitis in children. [21] This study suggests that, to a certain extent, exposure to outdoor air pollutants may increase the risk of allergic rhinitis in children. Condition of the room The condition of the classroom, as will be surveyed upon implementation of the study, is a confounding variable to this research because as already mentioned, allergens comprise a big part of the triggers of allergic rhinitis. Dust from unwashed curtains, carpets, or table cloths can be considered also as an allergen thus triggering a more severe allergic reaction. Furthermore, exposure to chalk dust, especially in a poorly ventilated classroom, may also trigger allergic rhinitis of the affected students. Summary of Related/Similar Studies According to Kutintara, allergic rhinitis (AR) is the most common of all allergic diseases. The prevalence, which ranges from 4% to 40%, of this disease is spreading worldwide, including the Asia Pacific region. It has a great impact on a persons daily life. 82% of AR sufferers in the United States reported that they always or usually have symptoms at work or school. It is responsible for about 2 million lost school-days 5
each year in the United States and a significant large number of Thai children indicated that their allergy symptoms were severe enough to limit their activities. [22] There are currently no cures for allergic rhinitis. However, there are ways to treat the symptoms. These treatments include medication, immunotherapy, and avoidance. The most common medications for allergic rhinitis are antihistamines, decongestants, and antihistamines-decongestant combinations. Unfortunately, side effects are a main concern for taking medications. It was reported that 31% of patients experienced side effects from the medications and 65% of patients would not take some drugs because of the side effects. Allergen immunotherapy includes allergen vaccinations and periodic allergen shots to lessen a patients sensitivity to allergens. It is for those who do not respond to medications or have adverse side effects from the medications. Although the immunotherapy can reduce allergy symptoms, patients should still continue practicing allergen avoidance. Practicing allergen avoidance while receiving immunotherapy can significantly enhance the effectiveness of the treatment against AR. [22] Avoidance is the primary method in treating AR. Those with allergies can reduce their allergic symptoms by reducing their exposure to allergens. This includes promoting a healthy indoor environment. The main allergens that are found indoors are allergens from dust mites, cockroaches, and molds. These allergens can be avoided by knowing how to eliminate them. These allergens commonly survive in environments that are warm, moist and humid. Dust mites cannot live in an environment that has a relative humidity of less than 50% while cockroaches and molds only thrive in areas of warmth and humidity. Therefore, other than keeping an AR patients surrounding environment clean, it is also recommended to have an air-conditioning system or proper ventilation system so that it can reduce the amount of allergens present in the patients environment by reducing the humidity and heat levels. [22] In congruence with the aforementioned study, according to Zacharisen, a member and a fellow of the American Academy of Asthma, Allergy, and Immunology, the key to reducing the severity of symptoms a child experiences at school is avoidance of these allergens. If it is possible, parents should talk to school personnel to make them aware of the allergy triggers of their children so as to avoid aggravating their allergies. [23] A study in Boston conducted by Blaisse stated that the symptoms of allergic rhinitis and the adverse effects of medications taken can diminish or lessen the cognitive function and learning of students. This can also affect the quality of student-life if aggravated. Whats unfortunate is that most conditions are left under-diagnosed or under-treated because symptoms are often discounted by parents as just allergies. [24] The study further noted that aside from the loss of cognitive function in children with moderate to severe AR, this can also cause irritability and fatigue leading to the inattentiveness and difficulty in concentrating in school. One of the most important components of management, according to the study, is to educate the patient and the family about avoiding the allergens that the children are allergic to. Another important thing to take note of is the environment of the school children in which they will be exposed to. The most common allergens at school that may cause AR include dust mites, chalk dust, animal dander, pollen, molds, and even exercise.[23] In response to these circumstances, there are a number of therapies than can be undertaken by children with AR. These include antihistamines, corticosteroids, leukotriene-receptor antagonists, mast cell stabilizers, anticholinergics, and allergen-specific immunotherapy depending on whether the AR is intermittent, persistent, severe, or mild. [24] It has been identified that second-generation antihistamines are the more preferred treatment though it can produce some sedative effects. 6
Oral and topical decongestants are also often used in addition with antihistamines. The only disadvantage is that it cannot alleviate any other symptoms of AR such as itching and sneezing. It can only alleviate the nasal decongestion experienced with AR. Another therapy mentioned is with the use of corticosteroids and these corticosteroids usually act on the nasal mucosa (intranasal action) and treat most of the symptoms of AR. This method is often recommended to children, especially those who present with severe symptoms. However, systemic corticosteroids are not recommended to children because of its serious side effects thus it should not be administered in chronic use. Leukotriene-receptor antagonists are more effective antihistamines but less effective than the intranasal corticosteroids. Aside from minor side effects such as headache and otitis media, it is generally safe for children and teenagers. Mast cell stabilizers usually inhibit mast cell degranulation relieving the common symptoms of AR. However, the disadvantage of this drug is that it has a short duration of action thus requiring more frequent doses. Anticholinergics inhibit the production of nasal secretions but have no effects on other symptoms of allergic rhinitis. The last therapy mentioned in the study is with the use of immunotherapy. This is the only disease-modifying therapy for AR and it should only be considered for use to children with moderate to severe allergies. [24] Another study in Spain conducted by Jauregui et. al. states that AR is the most common chronic disorder that affects the pediatric population.[26] Data shows that AR and rhinoconjunctivitis represent the main cause of 55.5% of all patients seen in Spanish allergology clinics. Again, it is important to note that a third of the population of 13-14 year-old teenagers suffer from the symptoms of AR. [27] It has been also stated in the study that AR somehow impairs daily activities such as visual coordination, retention capacity, and reaction time of students. [28] The study also states that if the AR is untreated, school performance is also affected. AR causes sleep disturbances, daytime sleepiness, absenteeism, presenteeism, irritability, restlessness, mood disorders, and an altered social life. [26] Sleep disturbances were caused by nasal congestion/blockade and also frequent awakenings during at night due to allergic inflammation. Presenteeism is the inattention, distraction, and lack of attention of the students while inside the classroom due to the symptoms of AR. Obviously, one of the main causes of learning difficulty and school failure is the students inability to concentrate due to untreated ARgiven that it is in fact one of the most common chronic illnesses that hits children and teenagers. [29] Focusing on the building conditions wherein classrooms are situated, a study that concerns transmission of airborne diseases was conducted in Peru. Rooms that only had natural measures for encouraging airflow were compared with mechanically ventilated rooms that were built much more recently. A comparison was also done between naturally ventilated rooms in old hospitals and naturally ventilated rooms in newer hospitals. Results showed that natural ventilation had high rates of air exchange, with an average of 28 air changes per hour. 50 year old hospitals had the highest ventilation with an average of 40 air changes per hour due to its structure. This rate is far higher compared to the 17 air changes per hour in naturally ventilated rooms in modern hospitals, which have lower ceilings and smaller windows. [30]
In a study about the impact of school building conditions on student absenteeism in Upstate New York, researchers investigated this by obtaining data from the 2005 Building Condition Survey of Upstate New York schools with 2005 New York State Education department students absenteeism data at the individual school level and evaluated associations between building conditions and absenteeism at or above the 90th percentile. As a result, researchers associated absenteeism with visible molds, humidity, poor ventilation, vermin, building condition problems, and building system or structural problems related to these conditions. They also saw that schools in lower socioeconomic districts and schools attended by younger students showed the strongest association between poor building conditions and absenteeism. With this study, there were some limitations. Some confounding variables were the external exposures such as traffic pollution and exposures from a students home could have affected this study. In addition, absenteeism due to illness or other reasons could not be distinguished. The study's ecological design did not allow collection of information on individual health outcomes or reasons for absenteeism. In conclusion, they found associations between student absenteeism and adverse school building conditions. As a recommendation, further studies should confirm these findings and prioritize strategies for school condition improvements. [3]
Conceptual Framework: Exposure Variable Exposure to Airconditioning System Confounders Allergens/Irritants such as pollen, molds, cockroaches, dust collecting furniture, and chalk dust Disease Variable Decreased Severity of Allergic Rhinitis and alleviation of symptoms Number of hours spent in classroom
Figure 2. Conceptual framework of proposed study. Bibliography: [1] Settipane, R.A. (2001). Demographics and Epidemiology of Allergic and Nonallergic Rhinitis [Abstract]. Allergy Asthma Proc. 22(4): 185-9. Retrieved July 8, 2011 from: http://www.medscape.com/medline/abstract/11552666. [2] Philippine Star (2008). Allergic Rhinitis Prevalent among Pinoys. Retrieved July 8, 2011 from: http://library.pchrd.dost.gov.ph/index.php/news-archive/1080. [3] Simons, E., Hwang, S., Fitsgerald, E., Keilb, C. & Lin, S. (2009). The Impact of School Building Conditions on Student Absenteeism in Upstate New York. 100 (9). Research and Practice. [4] Blaiss, MS. Allergic rhinitis and impairment issues in schoolchildren: a consensus report. Current Medical Research and Opinion. 2004 Dec; 20(12):1937-52. From: http://www.redorbit.com/news/health/131029/allergic_rhinitis_and_impairment_issues_in_school children_a_consensus_report/index.html [5] Meltzer, E.O. (1998). Treatment Options for the Child with Allergic Rhinitis. Clinical Pediatrics. Jan 1998; 37, 1; ProQuest Research Library. Accessed July 7, 2011. 8
[6] A.D.A.M. (2011). Allergic rhinitis Hay fever Nasal allergies. Retrieved July 16 2011 from http://www.nlm.nih.gov/medlineplus/ency/article/000813.htm [7] Ghazi, et. al. (2003). Frequency of Allergic Rhinitis in School-age Children (7-18 Years) in Tehran. Iranian Journal of Asthma, Allergy and Immunology. 2 (4). [8] Cauwenberge, et. al. (2004). Epidemiology of Allergic Rhinitis. The UCB Institute of Allergy, Brussels. [9] Sheikh, et al (2011). Allergic Rhinitis. Retrieved medicine.medscape.com/article/134825-overview#a0104 July 16, 2011 from http://e
[10] Wang (2005). Risk factors of allergic rhinitis: genetic or environmental? Retrieved July 16 2011 from http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1661616/ [11] Settipane, R.J., Hagy, G.W., Settipane, G.A.(1994). Long-term risk factors for developing asthma and allergic rhinitis: a 23-year follow-up study of college students. Allergy Proc. 15: 21-25. [12] Ryan, D., Yusuf, O., Ostergaard, M.S. & Rodriguez, M.R. (2011). Supporting statement by the international primary care respiratory group. Retrieved from http://www.worldallergy.org/UserFiles/file/WAO-White-Book-on-Allergy_web.pdf [13] Pawankar, R., Canonica, G.W., Holgate, S.T. & Lockey, R.F. (2011). WAO (World Allergy Organization) White Book on Allergy [pp. 11]. (PDF version), Retrieved from http://www.worldallergy.org/UserFiles/file/WAO-White-Book-on-Allergy_web.pdf [14] Msges, R. et. al. (2011). Emerging Areas of Interest in the Management and Treatment of Allergic Rhinitis. Retrevied from http://www.touchrespiratory.com/files/article_pdfs/Hassan.pdf [15] Busse, P. (2010). Allergic rhinitis. Medlineplus. Retrieved July 16, 2011, from http://www.nlm.nih.gov/medlineplus/ency/article/000813.htm. [16] Togias, A. (2004). Unique mechanistic features of allergic rhinitis. Journal of allergy and clinical immunology. Retrieved July 16, 2011, from http://www.sciencedirect.com/science/article/pii/S0091674900093143. [17] Bousquet, J., Reid, J., Van Weel, C., Baena Cagnani, C., Demoly, P., Denburg, J., Fokkens, W.J., Grouse, L., Mullol, K., Ohta, K., Schermer, T., Valovirta, E. & Zhong, N. (2008). Management of Allergic Rhinitis and its Impact on Asthma. ARIA Pocket Guide [Internet]. MCR Inc. [cited 2011 July 24]; [7 pages]. Available from: http://whiar.org/docs/ARIA_PG_08_View_WM.pdf [18] Alm B, Gokso r E, Thengilsdottir H, Pettersson R, Mo llborg P, Norvenius G, Erdes L, A berg N, Wennergren G. Early protective and risk factors for allergic rhinitis at age 4 years. Pediatric Allergy and Immunology 2011; 22: 398404. Retrieved July 22, 2011 from http://onlinelibrary.wiley.com/doi/10.1111/j.1399-3038.2011.01153.x/pdf [19] Nakagomi T, Itaya H, Tominaga T, et al. Is atopy increasing? Lancet 1994;343:1212. Retrieved July 22, 2011 from http://www.ncbi.nlm.nih.gov/pubmed/7903758 [20] Hajat S, et al. Association between air pollution and daily consultations with general practitioners for allergic rhinitis in London, United Kingdom. American Journal of Epidemiology (2001) 153 (7): 704-714. Retrieved July 22, 2011 from http://aje.oxfordjournals.org/content/153/7/704.full [21] Hwang B, et al. Relationship of air pollution and allergic rhinitis in Taiwanese school children. Respiratory Research 2006, 7:23. Retrieved July 22, 2011 from http://respiratoryresearch.com/content/7/1/23 9
[22] Kutintara, Benjamas. "Home Environments and Allergen Avoidance Practices in a Hot, Humid Climate." Virginia Polytechnic Institute and State University, 2002. United States -- Virginia: ProQuest Dissertations & Theses (PQDT). Web. 17 July 2011. [23] Health risks in the classroom: children with asthma and allergies need to take special precautions at school. (2007). American Academy of Asthma, Allergies, and Immunology. Retrieved July 15, 2011 from http://www.kidneeds.com/diagnostic_categories/articles/classrisks02.htm [24] Mahoney, D. (2005). Allergic rhinitis hits hard in the classroom. Retrieved July 16, 2011 from The CBS Interactive Business Network website: http://findarticles.com/p/articles/mi_hb4384/is_3_39/ai_n29168995/pg_2/?tag=mantle_skin;conte nt [25] Iannelli, V. (2010). Classroom triggers for asthma and allergies. American Academy of Asthma, Allergies and Immunology. Retrieved July 16, 2011 from http://pediatrics.about.com/od/allergies/a/04_class_trigrs.htm [26] Jauregui, I. et al. (2009). Allergic rhinitis and school performance. J Investig Allergol Clin Immunol. 19, 1: 32-39. Retrieved July 16, 2011 from http://www.jiaci.org/issues/vol19s1/6.pdf [27] Asher MI, Montefort S, Bjorksten B, Lai CK, Stachan DP, Weiland SK et al. Worldwide time trends in the prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in childhood: ISAAC Phases One and Three repeat multi-country crosssectional surveys. Lancet 2006; 368:733743. Retrieved July 16, 2011 from http://www.ncbi.nlm.nih.gov/pubmed/16935684 [28] Wilken JA, Berkowitz R, Kane R. Decrements in vigilance and cognitive functioning associated with ragweed-induced allergic rhinitis. Ann Allergy Asthma Immunol 2002;89:372380. Retrieved July 16, 2011 from http://www.sciencedirect.com/science/article/pii/S1081120610620388 [29] Karande S, Kulkarni M. Poor school performance. Indian J Pediatr 2005; 72(11):961-967. Retrieved July 16, 2011 from http://www.ncbi.nlm.nih.gov/pubmed/16391452 [30] Siriaksorn, S. (2011). Allergic rhinitis and immunoglobulin deficiency in preschool children with frequent upper respiratory illness. PubMed. 29(1):73-7. Retrieved July 8, 2011 from http://www.ncbi.nlm.nih.gov/pubmed/21560491.
10
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- OUTPUT 10 1st SubmissionDocument6 pagesOUTPUT 10 1st SubmissionJoshua ArcairaNo ratings yet
- Approach To Patients With Motor Ans Sensory DisordersDocument55 pagesApproach To Patients With Motor Ans Sensory DisordersJoshua ArcairaNo ratings yet
- Game MechanicsDocument2 pagesGame MechanicsJoshua ArcairaNo ratings yet
- Notables in Microbiology (PLE 2015)Document4 pagesNotables in Microbiology (PLE 2015)Joshua ArcairaNo ratings yet
- OUTPUTS 8 and 9Document3 pagesOUTPUTS 8 and 9Joshua ArcairaNo ratings yet
- OUTPUT 6 (Revised)Document7 pagesOUTPUT 6 (Revised)Joshua ArcairaNo ratings yet
- Research Protocol 1st SubmissionDocument31 pagesResearch Protocol 1st SubmissionJoshua ArcairaNo ratings yet
- Revised Output 7Document32 pagesRevised Output 7Joshua ArcairaNo ratings yet
- Letter of Assent (Draft 1)Document2 pagesLetter of Assent (Draft 1)Joshua ArcairaNo ratings yet
- Revised Outputs8 and 9Document4 pagesRevised Outputs8 and 9Joshua ArcairaNo ratings yet
- OUTPUT 6 SecondSubmission (For Real!)Document7 pagesOUTPUT 6 SecondSubmission (For Real!)Joshua ArcairaNo ratings yet
- IEC LetterDocument1 pageIEC LetterJoshua ArcairaNo ratings yet
- OUTPUT 6 First SubmissionDocument7 pagesOUTPUT 6 First SubmissionJoshua ArcairaNo ratings yet
- Study Where We Based Our Sample SizeDocument6 pagesStudy Where We Based Our Sample SizeJoshua ArcairaNo ratings yet
- Revised Output 5: Sample SizeDocument4 pagesRevised Output 5: Sample SizeJoshua ArcairaNo ratings yet
- Revised Output 5: Sample SizeDocument4 pagesRevised Output 5: Sample SizeJoshua ArcairaNo ratings yet
- 3rd Revised RRLDocument10 pages3rd Revised RRLJoshua ArcairaNo ratings yet
- Basis For Revised Output 5Document7 pagesBasis For Revised Output 5Joshua ArcairaNo ratings yet
- Research Design 3rd SubmissionDocument11 pagesResearch Design 3rd SubmissionJoshua ArcairaNo ratings yet
- Sampling Method, Size and CalculationDocument49 pagesSampling Method, Size and CalculationJoshua Arcaira100% (4)
- OUTPUT 4 Second RevisionDocument9 pagesOUTPUT 4 Second RevisionJoshua ArcairaNo ratings yet
- Research Design 1st SubmissionDocument5 pagesResearch Design 1st SubmissionJoshua ArcairaNo ratings yet
- Revised RRLDocument5 pagesRevised RRLJoshua ArcairaNo ratings yet
- Output 4 1st SubmissionDocument5 pagesOutput 4 1st SubmissionJoshua ArcairaNo ratings yet
- Research Design 2nd SubmissionDocument9 pagesResearch Design 2nd SubmissionJoshua ArcairaNo ratings yet
- Research Design 1st SubmissionDocument5 pagesResearch Design 1st SubmissionJoshua ArcairaNo ratings yet
- Changes Needed For RevisionDocument2 pagesChanges Needed For RevisionJoshua ArcairaNo ratings yet
- Preceptorial With Dra AbongDocument2 pagesPreceptorial With Dra AbongJoshua ArcairaNo ratings yet
- Review of Related LiteratureDocument5 pagesReview of Related LiteratureJoshua ArcairaNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Networks Lab Assignment 1Document2 pagesNetworks Lab Assignment 1006honey006No ratings yet
- Plants Life Cycles and PartsDocument5 pagesPlants Life Cycles and PartsseemaNo ratings yet
- Chapter One: Business Studies Class XI Anmol Ratna TuladharDocument39 pagesChapter One: Business Studies Class XI Anmol Ratna TuladharAahana AahanaNo ratings yet
- Bikini - USA - 03.2017Document68 pagesBikini - USA - 03.2017OvidiuNo ratings yet
- 1 Univalent Functions The Elementary Theory 2018Document12 pages1 Univalent Functions The Elementary Theory 2018smpopadeNo ratings yet
- Afrah Summer ProjectDocument11 pagesAfrah Summer Projectاشفاق احمدNo ratings yet
- © 2020 Lippincott Advisor Nursing Care Plans For Medical Diagnoses - Coronavirus Disease 2019 (COVID 19) PDFDocument7 pages© 2020 Lippincott Advisor Nursing Care Plans For Medical Diagnoses - Coronavirus Disease 2019 (COVID 19) PDFVette Angelikka Dela CruzNo ratings yet
- List of StateDocument5 pagesList of StatedrpauliNo ratings yet
- SRC400C Rough-Terrain Crane 40 Ton Lifting CapacityDocument1 pageSRC400C Rough-Terrain Crane 40 Ton Lifting CapacityStephen LowNo ratings yet
- Technical CommunicationDocument35 pagesTechnical CommunicationPrecious Tinashe NyakabauNo ratings yet
- BE 510 Business Economics 1 Problem Set 5 SolutionsDocument5 pagesBE 510 Business Economics 1 Problem Set 5 SolutionsCreative Work21stNo ratings yet
- Verification of First Law V-SonometerDocument3 pagesVerification of First Law V-SonometerRick astley's microphoneNo ratings yet
- ASCP User GuideDocument1,566 pagesASCP User GuideThillai GaneshNo ratings yet
- Dwarf Boas of The Caribbean PDFDocument5 pagesDwarf Boas of The Caribbean PDFJohn GamesbyNo ratings yet
- Government of The Punjab Primary & Secondary Healthcare DepartmentDocument3 pagesGovernment of The Punjab Primary & Secondary Healthcare DepartmentYasir GhafoorNo ratings yet
- 10CV54 Unit 05 PDFDocument21 pages10CV54 Unit 05 PDFvinodh159No ratings yet
- Lending Tree PDFDocument14 pagesLending Tree PDFAlex OanonoNo ratings yet
- AWK and SED Command Examples in LinuxDocument2 pagesAWK and SED Command Examples in Linuximranpathan22No ratings yet
- 2019 ASME Section V ChangesDocument61 pages2019 ASME Section V Changesmanisami7036100% (4)
- Popular Tools CatalogDocument24 pagesPopular Tools CatalogCarbide Processors IncNo ratings yet
- 2019 BioscienceJDocument14 pages2019 BioscienceJPatrícia Lima D'AbadiaNo ratings yet
- Experiment Vit CDocument4 pagesExperiment Vit CinadirahNo ratings yet
- Project On International BusinessDocument18 pagesProject On International BusinessAmrita Bharaj100% (1)
- Shell Omala S2 G150 DatasheetDocument3 pagesShell Omala S2 G150 Datasheetphankhoa83-1No ratings yet
- Capex Vs RescoDocument1 pageCapex Vs Rescosingla.nishant1245No ratings yet
- Case 1 1 Starbucks Going Global FastDocument2 pagesCase 1 1 Starbucks Going Global FastBoycie TarcaNo ratings yet
- CM Template For Flora and FaunaDocument3 pagesCM Template For Flora and FaunaJonathan Renier Verzosa0% (1)
- Ds 3805Document4 pagesDs 3805sparky2017No ratings yet
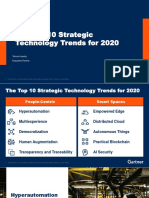
- The Top 10 Strategic Technology Trends For 2020: Tomas Huseby Executive PartnerDocument31 pagesThe Top 10 Strategic Technology Trends For 2020: Tomas Huseby Executive PartnerCarlos Stuars Echeandia CastilloNo ratings yet
- Unitary Small Air-Conditioners and Air-Source Heat Pumps (Includes Mixed-Match Coils) (RATED BELOW 65,000 BTU/H) Certification ProgramDocument65 pagesUnitary Small Air-Conditioners and Air-Source Heat Pumps (Includes Mixed-Match Coils) (RATED BELOW 65,000 BTU/H) Certification ProgramAmer GaladNo ratings yet