Professional Documents
Culture Documents
09 - Mohamed Reza
Uploaded by
rageshmrOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
09 - Mohamed Reza
Uploaded by
rageshmrCopyright:
Available Formats
SIM UNIVERSITY SCHOOL OF SCIENCE AND TECHNOLOGY
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
STUDENT PI NO. SUPERVISOR PROJECT CODE
: MOHAMED REZA S/O ABDUL ALI : W0503059 : DR LIM GEOK HIAN : JAN 09/ BME/08
A project report submitted to SIM University in partial fulfilment of the requirements for the Degree of Bachelor of Science in Biomedical Engineering 2009
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Acknowledgements
I would like to sincerely thank Dr Lim Geok Hian for granting me the opportunity to work on this project. It has been a fulfilling, enriching and most importantly an educational experience for me. Apart from the knowledge on COPD (Cardio Pulmonary Disease) and BODE index that I learnt while working under his guidance, I also had the opportunity to discuss a vast variety of topics with him, though at a rudimentary level. I truly enjoyed being his student and working with him. I would also like to thank Dr Alan Lim Teik Cheng of SIM University for his assistance in providing materials (templates, etc.) during this project course work. I would also like to express my token of appreciation to Dr Lim Tiek Cheng for his guidance and encouragement during the final lecture on 15th August 2009. Finally, my gratitude towards 2 very special persons goes beyond words. Without their infinite patience, unconditional love, and, everlasting support none of this would have been possible.
Final Report
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
TABLE OF CONTENTS
Description Title Page Acknowledgements Abstract List of Figures List of Tables List of Abbreviations Page 1 2 5 6 7 8
Chapter 1: Introduction to Project
1.1 Background to Chronic Obstructive Pulmonary Disease 1.2 Objective of the Project 1.3 Proposed approach and method to be employed 1.4 Scope of the Project 1.5 Organization and Overview of the Project 9 12 15 15 16
Chapter 2: Introduction to Assessment of COPD
2.1 Fundamentals of Cardiopulmonary Exercise Test 2.2 Fundamentals of Body Mass Index (BMI) 2.3 Fundamentals of Spirometry 2.4 Fundamentals of MMRC Dyspnoea Scale 2.5 Fundamentals of Six Minute Exercise Test 2.6 VBODE Index
19 19 21 23 29 30 31
Chapter 3: Methodology- Design of Software
3.1 Login Page 3.2 Questionnaire Page 3.3 Staffs Page 3.4 Doctors Page 34 35 36 40
Final Report
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Chapter 4: Observation 4.1 Analysis of Patients Data Chapter 5: Discussion and Conclusion Chapter 6: Recommendation Chapter 7: Critical Reviews and Logs 7.1 Critical Reviews 7.2 Logs Chapter 8: Reflections References Appendix A: BMI chart for children Appendix B: The BORG Scale Appendix C: Source Codes for (C#) C-Sharp Programming Appendix D: Lab Data of Cardiopulmonary Exercise Test on a Bicycle Ergometer Appendix E: Inspiration and Expiration Appendix F: Spirometry Staging
44 46 48
50 68 77 78 84 86 87
112 149 150
Final Report
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Abstract
Recent statistics of the (WHO) World Health Organization ranked (COPD) Chronic Obstructive Pulmonary Disease as the 5th leading cause of death in the world. COPD is the seventh leading cause of death in Singapore today. The WHO estimates that passive smoking is associated with a 10 to 43 percent increase in risk of COPD in adults. Longterm exposure to other lung irritants, such as air pollution, chemical fumes, or dust, also may contribute to COPD. The current method of COPD measurement includes Spirometric Test, Dyspnoea score test from MMRC (Modified Medical Research Council) scale which grades the degree of ones breathlessness, (6MWT) Six Minute walk test and calculation of (BMI) Body Mass Index. This is because Celli BR et al. [5] had found this subgroup of four variables with the strongest association in determining the risk of deaths in patients with COPD; predicting risk of hospitalizations and monitoring the prognosis of lung disease. Each of these possible explanatory variables was independently evaluated to determine its association with one-year mortality in a stepwise forward logistic-regression analysis. BODE index was found.
However, BODE index may not be efficient enough. Organs like lungs need to be progressively stressed so that the functional capacity of the lungs can be fully determined. In 6MWT, the lungs are not tested while in progressive stress. In 6MWT, the patient walks on his own pace and will tend to slow down when tired despite the encouragement given by the tester. Thats why the organs are not under progressive stress.
The use of (CPET) Cardiopulmonary Exercise Test together with the current tests in the evaluation of BODE index would help ease the problem. CPET uses either Treadmill or Cycle Ergometer. Cycle Ergometer is more preferred as it is safer, reliable and causes less strain on patients lower extremity muscles. CPET causes the organs to undergo progressive stress as the patient could not walk on his/her own pace. (VO2 max) Peak Oxygen consumption recorded during the exercise test can be examined for normal or compromised response. (VO2 max) value is important for COPD evaluation. Therefore adding (VO2 max) to the current BODE index; a new index was formed. I named it as VBODE index.
Final Report
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
List of Figures
Description Figure 1.1: In Emphysema Figure 1.2: In Chronic Bronchitis Figure 1.3: Healthy Alveoli and Damaged Alveoli Figure 1.4: Organization and Overview of the Project Figure 1.5: Gantt Chart Figure 2.1: CPET performed on a Bicycle Ergometer Figure 2.2: A patient blowing into the Spirometer Figure 2.3.1: Volume measuring Spirometer Figure 2.3.2: Flow measuring Spirometer Figure 2.4: Desktop Electronic Spirometer Figure 2.5: Small handheld Spirometer Figure 2.6: Gold Spirometric Criteria for COPD Severity Page 10 10 10 16 17 19 24 26 26 26 26 28
Final Report
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
List of Tables
Description Table 1: BODE Index vs. Approximate 4 year Survival Interpretation vs. Severity Table 2: Severity of COPD based on CEPT Table 3: BMI Formula Table 4: Asian BMI vs. Risk Table 5: BMI Scores in the BODE Index Table 6: FEV1 (% value) as in the BODE Index Table 7: MMRC Dyspnoea Score in the BODE Index Table 8: 6MWT result score as in the BODE Index Table 9: Calculation of VBODE Index Table 10: Peak Oxygen Consumption Table 11: Exercise Equipment: Cycle Ergometer Versus Treadmill Page 12 21 21 22 23 29 29 31 32 44 45
Final Report
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
List of Abbreviations
HR (Heart Rate): Number of heart beats per minute. VC (Vital capacity): Maximal volume of gas exhaled from the milliliters per minute per kilogram point of maximal inspiration, and corresponds to TLC _ RV. It is expressed in units of liters BMI: Body Mass Index: Weight divided by square of height in meters. FVC: Forced Vital Capacity the total volume of air that the patient can forcibly exhale in one breath. FEV1 : Forced Expiratory Volume in One Second the volume of air that the patient is able to exhale in the first second of forced expiration. Measured in liters and can also be expressed as a percentage of the predicted values for that individual.
FEV1 / FVC : The ratio of FEV1 to FVC expressed as a fraction. Values of FEV1 and FVC are measured in liters and are also expressed as a percentage of the predicted values for that individual. MMRC- Modified Medical Research Council CEPT- Cardiopulmonary Exercise Test COPD- Chronic Obstructive Pulmonary Test 6MWT- Six Minute Walk Test
Final Report
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Chapter 1: Introduction to Project
1.1 Background to Chronic Obstructive Pulmonary Disease Chronic Obstructive Pulmonary Disease (COPD) is one of the most common and important disorders. The WHO (World Health Organization) estimated that in 2000, 2.74 million people died of COPD worldwide and ranked COPD as the 5th leading cause of death in the world. In 1990, a study by the World Bank and WHO ranked COPD 12th as a burden of disease and by 2020, it is estimated that COPD will be ranked 5th [16, 39]. Chronic obstructive pulmonary disease is the seventh leading cause of death in Singapore today [38].
COPD is a progressive disease that makes it hard to breathe and is characterized by a gradual loss of lung function. "Progressive" means the disease gets worse over time. "Chronic disease" means an illness that cannot be cured. COPD can cause chronic cough, coughing that produces large amounts of mucus (a slimy substance), wheezing, shortness of breath, chest tightness, and other symptoms. Cigarette smoking is the leading cause of COPD. Smokers or ex-smokers over 40 years of age are normally at risk. Long-term exposure to other lung irritants, such as air pollution, chemical fumes, or dust, also may contribute to COPD. Also people who have a family history of COPD are more likely to get the disease if they smoke. Everyday, more than one person dies of COPD in Singapore according to the Chronic Obstructive Pulmonary Disease Association (Singapore) [33].
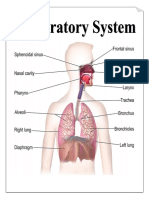
COPD is also termed as Chronic Obstructive Airway Disease (COAD), Chronic Obstructive Lung Disease (COLD), Chronic Obstructive Bronchitis and Emhysema. (COPD) includes 2 main disorders, namely Emphysema and Chronic Bronchitis diseases that are characterized by obstruction to air flow in and out of the lungs [33, 34]. Emphysema involves damage to the air sacs (alveoli) as shown below in diagram 1 and small airways (bronchioles) in the lungs causing it to lose its elasticity. As a result, body does not get the oxygen it needs making it hard to catch the breath. In Chronic Bronchitis, the airways become swollen and inflamed and produce large amounts of mucus. The swollen tissues and mucus make breathing difficult. The airways often become easily infected as shown in diagram 2. Below in diagram 3; it shows the respiratory system and images of healthy alveoli and alveoli damaged by COPD.
Final Report
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
COPD
develops slowly. Symptoms often worsen over time and can limit ones ability to do routine activities. Severe COPD can prevent one from doing even basic activities like walking, cooking, or taking care of him/her. Most of the time, COPD is diagnosed in middle-aged or older people. The disease is not passed from person to person. COPD has no cure yet, and doctors don't know how to reverse the damage to the airways and lungs. However, treatments and lifestyle changes can help COPD diagnosed patients feel better, stay more active and slow the progress of the disease.
Final Report
10
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Initially when the patient visits the doctor based on his/her signs and symptoms, the doctor will check his/her medical and family histories, and test results. He or she will be asked whether he/she smoke or had contact with lung irritants, such as air pollution, chemical fumes, or dust. If there is ongoing cough, the doctor may ask how long, how much cough, and how much mucus comes up when you cough. He or she also may ask whether there is a family history of COPD. Then doctor will examine and use a stethoscope to listen for wheezing or other abnormal chest sounds. If the patient has wheezing and does not smoke and is not exposed to lung irritants and has a history of asthma, it will be diagnosed as ASTHMA. These patients may choose to undergo Lung Function tests. Other than that, all patients with signs and symptoms are required to undergo Lung Function tests.
Lung function tests is a measure of how much air one can breathe in and out, how fast one can breathe air out, and how well the lungs can deliver oxygen to the blood. The main test for COPD testing is the Spirometry. Other lung function test, such as a lung diffusing capacity test, is rarely used. Basically Spirometry tests are used to diagnose and stage the severity of COPD.A physiological variable the forced expiratory volume in one second (FEV1) is often used by physicians in the diagnosis, treatment, monitoring and grading of the severity of COPD. However the severity of the disease cannot be assessed only on Spirometer and any measurement of airway obstruction. It must be assessed with 6minute walk test associated or not with the BODE index to better find disease-modifying interventions and to improve the outcome of COPD patients [28].
A BODE INDEX, a simple 10-point multidimensional grading system was invented in 2004 [5]. It proved to be better than the FEV1 based staging system by the ATS (American Thoracic Society) at staging the severity of COPD and predicting the risk of death [5, 7, 8,15, 28 and 25]. BODE index ranges from 0 to 10 points, with higher scores indicating a greater risk of death.
BODE is:
Final Report
11
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
(B) - Body mass index, BMI, ( Kg / m 2 ) (O) - Degree of Obstruction. FEV1 is the spirometric measure of airflow. (% predicted based on ethnicity, age, height, gender and weight) (D) - Dyspnoea. Patient's perception of symptoms measured with the MMRC dyspnoea score scale. (E) - Exercise capacity. Its the Six-minute walk distance measured in metres by the sixminute walk test. (Meters)
1.2 Objective of the project The synopsis of my topic was to determine the relationship between the fitness of a subject and the presence of lung disease from Cardio-pulmonary exercise testing. Subsequently, I have to develop an index in the prognosis of lung disease such as Chronic Obstructive pulmonary disease (COPD).
Currently from the BODE index, the approximate 4-Year Survival Interpretation is as shown below in table 1 [18, 35]. Experiment was done for 2 years to come up with this percentage of survival interpretation vs. Points vs. Severity [18]. Points Approximate 4 Year Survival Interpretation 80% 67% 57% 18% Severity
0-2 3-4 5-6
Mild Risk Moderate Risk Severe Risk Very Severe Risk
7-10 Table 1: BODE Index vs. Approximate 4 year Survival Interpretation vs. Severity
Final Report
12
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Both the Six Minute Walk Test (6MWT) and Cardiopulmonary Exercise Test (CPET) are used for functional assessment. Whether a 6MWT or CPET should be used depends on the questions being asked and the available resources available. It is proven that with resting pulmonary function, one cannot understand the functional capacity of the lungs. Also overall health status correlates better with exercise tolerance rather than with resting measurements [29 and 30].
The six-minute walk test (6MWT) fairly predicts morbidity (details of death) and mortality (deaths among this particular group of patients with COPD) when used with other data in the BODE index. But this six-minute walk test used in the BODE index is not very effective. The results from the 6MWT are not very accurate [30]. The reason, patients are motivated to walk fast during the six minutes to cover as much distance as possible. The patient will walk on his/her own pace fast, slow, and fast due to his /her capability. The patient may take chance to walk slower if tired. Speech motivation is not as effective as the motivation from the devices pedaling on the cycle ergometer or running on the treadmill. The organs and systems involved in the 6MWT exercise response are not under conditions of progressively intense physical stress. The lungs must be under progressive stress so that the maximum meters he/she can cover in six minutes can be accurately measured and made comparison with reference data.
It had been clearly shown that cardiopulmonary exercise testing (CPET) should be considered as an extension of the clinical examination. Since then exercise testing is used in the medical community [20, 28 and 30].CPET is a non invasive (involves no blood) assessment which helps evaluate the organs and systems involved in exercise responses. It involves the pulmonary, cardiovascular, hematopoietic (blood cell assessment), neuropsychological (brain assessment), and skeletal muscle systems that is not adequately reflected through the measurement of individual organ system. CPET results are attained under conditions of progressively intense physical stress. The primary objective of CPET is to analyze test results for normal or impaired responses. CPET is a safe procedure with the
Final Report
13
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
risk of death for patients between 2 and 5 per 100,000 exercise tests performed [30]. CPET involves the measurement of respiratory gas exchange: oxygen uptake (VO2 ) , carbon dioxide output ( VCO2 ), and minute ventilation ( VE ) in addition to monitoring (ECG) Electrocardiography, (BP) Blood Pressure, and pulse Oximetry.
CPET is clinically useful in the evaluation of patients with COPD; when an objective determination of exercise capacity (VO2 max) is necessary in establishing exercise limitations [30]. The (VO2 max) (peak Oxygen consumption during exercise) value is the very first cardiopulmonary measured parameter that is examined for normal or compromised response [20]. (VO2 max) value is important for COPD evaluation [10 and 27].
This Report will aim to further modify the BODE Index to VBODE Index. This VBODE index will be more accurate in determining the risk of death and hospitalization. This can be achieved by adding the parameter (VO2 max) together with the BODE index parameters. In other words, the CPET is to be performed together with all the current tests used to evaluate the BODE Index. This will result in the invention of VBODE index. VBODE index will be clearly explained in section 2.6.
VBODE is: (V) - VO2 max (ml / kg / min) .The measurement of V O2 max (peak oxygen consumption). (B) - Body mass index, BMI, ( Kg / m 2 ) (O) -Degree of Obstruction. FEV1 is the spirometric measure of airflow. (% predicted based on ethnicity, age, height, gender and weight) (D) -Dyspnoea. Patient's perception of symptoms measured with the MMRC dyspnoea score scale. (E) - Exercise capacity. Its the Six-minute walk distance measured in metres by the sixminute walk test. (Metres)
Final Report
14
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
1.3 Proposed Approach and Method to be Employed Using the knowledge attained from MT262- Putting Computer Systems to Work during my first year, a software program will be created using C Sharp (C#). This software will include the following: A questionnaire page in English to enable patient to enter his/her personal information, signs and symptoms. Hospital staffs page where one can click on the respective columns of the index to evaluate the VBODE index. Doctors/hospital staffs page where one can enter the measured data manually and evaluate the graphs. Comparison of data can be made between dates. 1.4 Scope of the project The scope of this report will cover the following: Design of software illustrating my VBODE index using C# (C Sharp). Explaining what is and how is: (1) V- VO2 max (ml / kg / min) (peak oxygen consumption) measured. (2) B- Body mass index, BMI, ( Kg / m 2 ) calculated. (3) O- Degree of Obstruction measured. FEV1 is the spirometric measure of airflow. (4) D- Dyspnoea evaluated. Patient's perception of symptoms measured with the MMRC dyspnoea scale. (5) E- Exercise capacity measured. Its the Six-minute walk distance measured in metres by the six-minute walk test. (Metres)
Using patients measured VO2 (ml / kg / min) from the hospital to evaluate the range where VO2 max (ml / kg / min) lies.
Final Report
15
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
1.5 Organization and Overview of the project COPD
Software
Background to COPD
Questionnaire
Cardiopulmonary Exercise Test
Analysis of patients oxygen consumption during Cardiopulmonary Exercise test
VBODE Index
BMI (Body Mass Index) Range of (ml/kg/min) (ml/kg per min)
Graph Analysis
Spirometry
MMRC Dyspnoea Scale
Six Minute Walk Test
Figure 1.4: Organization and Overview of the project
Final Report
16
Figure 1.5: Gantt chart
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
17
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Figure 1.5, shows the overview of the project task distribution. The Gantt chart seen above was used for organizing and assessing the progress of my project. It was created using Microsoft Excel and it provides a schedule of my tasks. The Gantt chart helped me to manage the progress of the project and achieve my target at a point in time. The Gantt chart allowed me to see how remedial action can bring my project back on track.
Final Report
18
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Chapter 2: Introduction to Assessment of COPD
2.1 Fundamentals of Cardiopulmonary Exercise Test Cardiopulmonary Exercise Test (CPET) is a unique tool to assess the limits and mechanisms of exercise tolerance. This test helps one determine how well the heart or lungs function when they are made to work harder. The information gained from the test helps physician make an accurate diagnosis and develop the most appropriate treatment. For people with shortness of breath, this CPET can determine whether the cause is cardiac or pulmonary. The goal of CPET protocols is to stress the organ systems involved in the exercise response in a controlled manner. For this reason the testing generally involves exercising large muscle groups, usually the lower extremity muscles [24 and 38]. CPET can be performed either on a treadmill or cycle ergometer. In NUH hospital (Singapore), the test is done on a cycle Ergometer. The patient is to pedal a stationary bicycle while the test is done. During the test, an electrocardiogram (ECG) records the electrical activity of the patients heart. The experienced technicians and/or doctors are to monitor.
Final Report
19
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Figure 2.1 shows a patient performing CPET on a bicycle ergometer. This exercise is similar to riding up a hill gradually becoming steeper as you progress. When this test is performed, the patient has to wear a mask which will be fitted with a device that is connected to extremely sensitive analysers. Several things are analysed and monitored. Namely, The amount of air the patient breathes in and blows out (expires) is measured breath by breath. This gas exchange is analysed to determine the amount of oxygen consumed and carbon dioxide produced.
The patients Heart Rate (HR), Electrocardiogram (ECG), Oxygen Saturation level ( SPO2 ) and Blood Pressure (BP).
Protocols need to be adhered so that reliable result like (VO2 ) can be attained. Trained technicians will show the patient how to use a stationary bicycle properly. The patient has to pedal at least 8-12 minutes. Pedalling will feel easy at first, and then it will gradually get harder. The patient will exercise to the limit till as he/she does not develop any danger signals such as a severe drop in BP, a change in ECG or encounter chest discomfort, shortness of breath, leg fatigue or dizziness.
The (VO2 max) (peak Oxygen consumption during exercise) value is the very first cardiopulmonary measured parameter that is examined for normal or compromised response [20]. (VO2 max) value is important for COPD evaluation [26 and 27].
Final Report
20
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Study was done to determine whether reliable data could be obtained at lower cost. After the CPXT test, the patients were classified according to the VO2 max as mild, moderate and severe [27]. Below in table 2, shows the classification due to the severity of respiratory disability. From CPXT test the (VO2 max) (ml/kg/min) is as follows:
NORMAL 25
MILD 20 to 24
MODERATE 15 to 19
SEVERE <15
Table 2: Severity of COPD based on CPET
I would merge this classification of COPD by CPET together with the BODE index to become VBODE index.
2.2 Fundamentals of Body Mass Index (BMI) BMI stands for Body Mass Index. It is used as a measure of body fat in adults and helps assess whether one is at risk for weight related health problems. BMI is calculated as shown below in table 3.
BMI =
Weight in (kg ) Height (metres) Height (metres ) Table 3: BMI Formula
Final Report
21
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
According to health promotion board [37], some Asian population, including Singaporeans have higher proportion of body fat compared to Caucasians of the same age, gender and BMI. Below shown in table 4 is the classification of BMI vs. Risk: BMI ( kg / m 2 ) BMI less than 18.5 RISK Underweight with risks of nutritional deficiency, disease and osteoporosis Healthy weight with low risk Overweight with moderate risk of developing Chronic Diseases like Heart Disease, High Blood Pressure, Stroke, Diabetes, etc. Obese with high risk BMI more than 27.4 Table 4: Asian BMI vs. Risk
BMI 18.5 to 22.9 (Healthy) BMI 23.0 to 27.4
BMI values do not apply to some people [36 and 37]: Pregnant Women and Nursing Mums. (BMI will be overestimated) People with muscular build. (BMI will be overestimated). eg. Athletes, body builders. Elderly or people with chronic disease (BMI will be underestimated because they had lost muscle) People with eating disorders like anorexia nervosa or people with extreme obesity. For children under the age of 18. During these years, the body is growing fast and that affects the calculation. For children, different age specific tables are used. This is shown in appendix A. Also in my case, VBODE index does not apply to the above mentioned group of people. In the Bode Index invented by Celli BR et al. [5], the BMI was fixed at > 21(0 points) or 21(1 point). This was because in the evaluation of the independent prognostic power of the body-mass index in the cohort study using different thresholds, there
Final Report
22
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
was inverse relation between body mass index and survival that was not linear but which had an inflection point 21 [17 and 26]. In other words observation study result reported that values below 21 were associated with an increased risk of death [5 and 26]. Therefore as in the BODE index, in my VBODE index, BMI scores will be as follows:
POINTS Body mass Index (kg / m 2 ) (BMI)
0 >21
1 21
Table 5: BMI Scores in the BODE Index
2.3 Fundamentals of Spirometry Spirometry is a painless test where the doctor/staff will ask one to take a deep breath in and then blow as hard as he/she can into a tube connected to a small machine. The machine is called a Spirometer. It measures how much air you breathe out and how fast you can blow air out.
Final Report
23
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Figure 2.2: A patient blowing into the Spirometer
The doctor may have the patient inhale medicine that helps open the airways and then blow into the tube again. The doctor then compare the test results before and after taking the medicine. Spirometry can help confirm, assess severity of airflow obstruction and detect COPD long before its symptoms appear. Doctors also may use the results from this test to find out how severe your COPD is and to help set your treatment goals. The test results also may help find out whether another condition, such as asthma or heart failure, is causing the symptoms. Spirometry is the gold standard for COPD diagnosis. Under-use of Spirometry leads to inaccurate COPD diagnosis. Widespread uptake has been limited by:
Concerns over technical performance of operators Difficulty with interpretation of results
Final Report
24
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Lack of approved local training courses Lack of evidence showing clear benefit of Spirometry
Many types of Spirometers are available in the industry. Bellows Spirometers: Measures flow, volume; mainly in lung function units. Electronic Desk Top Spirometers: Measure flow and volume with real time display. Small Hand-Held Spirometers: Inexpensive and quick to use but no print out.
Final Report
25
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
26
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Information provided by the Spirometer after maximal forced exhalation (greatest effort possible) after a maximum deep inspiration (completely full lungs). Several indices can be derived from this blow [21 and 32]. o FVC Forced Vital Capacity the total volume of air that the patient can forcibly exhale in one breath. o FEV1 Forced Expiratory Volume in One Second the volume of air that the patient is able to exhale in the first second of forced expiration. FEV1 /FVC the ratio of FEV1 to FVC expressed as a fraction (This will be expressed as a percentage in the VBODE index).
Values of FEV1 and FVC are measured in liters and are also expressed as a percentage of the predicted values for that individual. The ratio of FEV1 /FVC is normally between 0.7 and 0.8. Values below 0.7 are a marker of airway obstruction, except in older adults where values 0.650.7 may be normal. Caution particularly needs to be taken in patients over 70 years, where the use of predicted values taken from the younger population may result in over-diagnosing COPD. In people over 70 years old, the FEV1 /FVC ratio may need to be lowered to 0.65 as a lower limit of normal. Conversely, in people under the age of 45, using a ratio of 0.7 may result in under-diagnosis of airway obstruction. To avoid both of these problems, many experts recommend use of the lower limit of normal for each population. Predicted values are calculated from thousands of normal people and vary with sex, height, age and ethnicity. The standard predicted values in most of Europe are those established by the European Respiratory Society or the European Community Health and Respiratory Survey (ECHRS), but other values may be used in different countries. Those values most appropriate for the local population should be used.
Final Report
27
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Bode Index invented by Celli BR et al. [5] classified the severity of COPD from Spirometry based on the FEV1 predicted value in percentage. In other words,
FEV1 of the patient 100% FEV1 predicted based on sex, height, age and ethnicity.
Final Report
28
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Therefore as in the BODE index, in my VBODE index, FEV1 will be classified as: POINTS FEV1 (% of predicted) 0 65 1 50-64 2 36-49 3 35
Table 6: FEV1 (% value) as in the BODE index
2.4 Fundamentals of MMRC Dyspnoea Scale MMRC (Modified Medical Research Council) dyspnoea scale is also referred to as MRC dyspnoea scale, MMRC dyspnea scale or MRC dyspnea scale. This scale is used for grading of the degree of a patient's breathlessness. Dyspnoea is a perception or the uncomfortable conscious awareness the patient has of his breathing. As used in the BODE index, I will be using this in my VBODE index. Points 1 to 5 are illustrated below: 0. Not troubled by breathlessness except on strenuous exercise. 1. Short of breath when hurrying or walking up a slight hill. 2. Walks slower than contemporaries on the level because of breathlessness, or has to stop for breath when walking at own pace. 3. Stops for breath after about 100 m or after a few minutes on the level. 4. Too breathless to leave the house, or breathless when dressing or undressing. So as in the BODE Index, in my VBODE Index it will appear as: POINTS MMRC Dyspnea Scale 0 0-1 1 2 2 3 3 4
Table 7: MMRC Dyspnoea Score as in the BODE index
Final Report
29
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
2.5 Fundamentals of Six-Minute Exercise Test The Six-minute walk test is a simple test measuring the maximal distance that a patient can walk at his own pace in 6 minutes. This test is used in the evaluation of the BODE index. The 6MWT test helps detect pulmonary and cardiac disease.
In the 1960s, a simple test was developed to evaluate the walking distance during a defined period of time, for instance the 12-minute walk test. This test would better represent functional activity in daily life. Later the 6-minute walk test (6MWT) was found to perform as well as the 12-minute walk test. It is now largely used because it is very simple and does not require special equipment and trained technicians. Clinicians are therefore responsible for instructing technicians performing the test to assure continuous quality in measurements. Minimal requirements for a 6MWT: 1) Corridor of 30 m free of any walk obstacle and 2 cones 2) Distance marked every 3 meters 3) Standardized instructions 4) At least two practice walks 5) Graded scale in meters 6) Standard encouragement 7) Supervision from behind 8) End exercise Borg scale (Shown in Appendix B)
The 6MWT is standardized and the clinicians should adhere to the guidelines which provide a step-by step protocol and safety measures, define the preparation of the patient and procedures, and offer recommendations for the interpretation of results. If the recommended guidelines are adhered, this test is a very useful tool to assess the functional status of COPD patients and measure impairment in their daily life activity. This test is affordable and easy to perform. 6MWT helps to predict the risk of death in patients with COPD [5]. The better of the two 6MWT results performed at least 30 minutes apart is taken into consideration.
Final Report
30
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Both the Six Minute Walk Test (6MWT) and the Cardiopulmonary Exercise Test (CPET) will be used for functional assessment. My VBODE Index with (13 points) will be more precise than the current BODE Index (10 points). 6MWT will help to predict the risk of deaths in patients with COPD [5]. On the other hand, CPET will help to determine the functional assessment of the organs under progressive stress. In 6MWT, the patient walks on his own pace and will tend to slow down when tired despite the encouragement given by the tester. Thats why the organs are not under progressive stress. But in CPET -treadmill or cycle ergometer causes the organs to undergo progressive stress as the patient could not walk on his own pace [29]. As in the BODE Index, in my VBODE Index, it will be as follows: POINTS Six-min walk test 0 350 1 250 349 2 150 249 3 149
Table 8: 6MWT result Score as in the BODE index
2.6 VBODE Index Therefore improving on the current BODE Index (10 points Scale) to my VBODE Index (13 points Scale), there will be an additional (V), VO2 max (ml / kg / min) .VBODE index will be a simple 13-point scale, multidimensional grading system which is better than the BODE index at predicting the prognosis of lung disease and predict hospitalisations. VBODE index will range from 0 to 13 points, with higher scores indicating a greater risk of death.
VBODE SCORE will be calculated as follows: NOTE: VBODE index = Sum of all VBODE Score Only one Tick accepted per Row. Calculate the points at the respective ticks.
Final Report
31
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
POINTS VO2 max (ml/kg/min) (ml/kg per min) FEV1 (% of predicted) MMRC Dyspnea Scale Body mass Index (BMI) ( kg / m 2 ) Six-min walk test (meters)
0 Normal = >25
1 Mild = (20-24)
2 Moderate = (15-19)
3 Severe = (<15)
65 0-1 21
50-64 2 21
36-49 3
35 4
350
250 349
150 249
149
Table 9: Calculation of VBODE Index
Final Report
32
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Chapter 3: Methodology- Design of Software
Software was created using C Sharp. This software ia an application programming. Using the knowledge attained from MT262- Putting Computer Systems to Work during my first year this was made possible. The source codes are shown in Appendix C. This program is case sensitive. The following will be illustrated in the following sessions: 3.1: The Login Page 3.2: A Questionnaire page in English to enable patient to enter his/her personal information, signs and symptoms. 3.3: Hospital Staffs page where one can click on the respective columns of the index to evaluate the VBODE index. 3.4: Doctors/hospital staffs page where one can enter the measured data manually and evaluate the graphs. Comparison of data can be made between dates.
Final Report
33
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
3.1 Login Page
Click on Take Survey: The patient is required to enter his identification number. It can also be passport number from any country.
Click on Add VBODE in the Staff Access: Hospital staff can enter his/her password: Password in my case, it is saved as 12345. The hospital staff will select appropriate ticks in the result column to determine the VBODE Index.
Click on View Records in the Doctor Access: Doctor can enter his/her password. Password in my case, it is saved as 12345. The doctor can manually key in the exact result to evaluate the graph.
Final Report
34
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
3.2 Questionnaire Page
Once the user enters his/her identification number on the Login page, the above questionnaire appears. The user is required to enter his Name, Age, and Race and choose his/her gender. If any of these are left blank, the patients cannot submit. Error message will appear asking them to fill up the blank. The user can only do this questionnaire once daily. The dates and times are as in the computer. If the user does this questionnaire more than once in a day, error message will appear as shown below. By default it will chosen NO. For future recommendations, nothing should be selected at default.
Final Report
35
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
I decided to set values to Yes= 5 and No=1. This value will be used to tabulate graph. Total value for the 9 questions will be 45.
3.3 Staffs Page Once the staff enters the password, it is redirected to another page as shown below.
Final Report
36
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
The Staff has to enter Patients ID to save this VBODE Index. If the staff enters wrong ID number, error message like the one shown below appears.
Final Report
37
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
By Default VBODE Index will be Zero. This VBODE will change with respective to the chosen result. This is shown below:
Final Report
38
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
If VBODE is saved successfully, a message as shown below appears.
This approximate 4 Year Survival Interpretation is the modification from the present BODE index. In the BODE index it was classified within 10 points. I modified it into 13 points.
Final Report
39
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
3.4 Doctors Page Once the doctor enters the password, it will redirected to another page as shown below.
The doctor has to enter the patients ID to load his test results. After loading it will appear as shown below.
Final Report
40
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
The doctor has to manually key in patients exact result to plot the graph. Only the VBODE index and the survey results are carried forward from the staffs page and stored. By default, other values are set at 1000. The doctor will enter exact data and can choose which dates he/she wants the graph to be plotted. Plotted graph with exact result is shown below.
Final Report
41
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Only the survey and the VBODE index cannot be changed as they are carried forward from previous page entries. The survey result was made to calculate: Yes= 5 points No =1point Total 9 Questions= total is 9 5= 45 points SurveyScore = Accumulated Score Total possible Score(45)
This calculation was done so that it can be easily plotted on the axis of the graph.
Final Report
42
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
The Doctor can choose to view the Survey Graph, VO2 Graph, FEV1 Graph, MMRC Graph, BMI Graph, Walk Graph or VBODE Graph.
The doctor can make changes to any of the dates (for instance last visit result) at any time.
Final Report
43
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Chapter 4: Observation
4.1 Analysis of Patients Data I wanted to have a look and learn more about COPD testing at NUH (National University of Hospital). In NUH, they are using bicycle ergometer for COPD testing [33].But due to H1N1, students are not allowed to hospitals for research/study. However I managed to get COPD test results from an old student in UNISIM. Ms.Neo Pei Ling in 2007 [40] had done Cardiac Analysis from Stress Testing from a bicycle Ergometer and had received data from hospital. Her main goal was to develop a Cardiac Fitness Index. But I am to develop an index in the prognosis of lung disease such as Chronic Obstructive pulmonary disease (COPD). The hospital data retrieved from Ms.Neo PL are shown in Appendix D. Maximum Oxygen Consumption of all the 18 patients (16 male and 2 female) is as shown below in table 10. Patient Number 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 Gender/Age Peak Oxygen Consumption(ml/k g per min) 18.30 8.88 15.25 16.18 11.33 18.85 9.04 17.20 17.89 14.25 8.76 15.02 10.88 12.54 13:35 11.47 17.87 12.05 Time after start of the test (Hours:Mins:Secs 0:01:10 0:00:40 0:01:10 0:00:20 0:01:10 0:01:40 0:01:10 0:01:10 0:00:50 0:01:30 0:00:40 0:00:30 0:01:30 0:01:20 0:00:50 0:01:40 0:00:55 0:01:20
Male/37 Male/50 Female/34 Male/49 Male/29 Male/35 Male/53 Male/32 Male/47 Male/41 Male/64 Male/39 Male/48 Female/35 Male/45 Male/42 Male/37 Male/34
Table 10: Peak Oxygen Consumption
Final Report
44
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
The data shows that the peak oxygen consumption ( VO2 max ) lies within 0:00:20 (20 seconds) to 0:01:40 (1 minute 40 Seconds) for male. Peak Oxygen Consumption ( VO2 max ) for female lies within 0:01:20 (1 minute 20 seconds).The data gathered for female patients are insufficient. More female patients data is required to determine the peak oxygen consumption range. However to conclude, the patient is required to perform the Cardiopulmonary Exercise test on a bicycle ergometer for at least 2 minutes to determine.
Table 11 from [30] shows that ( VO2 max ) will be lower from the Cycle Ergometer than from the Treadmill. This is because the patient sits on bicycle ergometer. He/she will be more comfortable and has to cycle at his own speed. But in the treadmill he/she will require more energy as he/she has to overcome the speed of the treadmill. The treadmill test is more appropriate for active subjects rather than for patients [30]. Bicycle Ergometer is preferred because it is safer and more appropriate for patients. The degree of leg muscle training is lower and the weight bearing in obese is lower as compared to Treadmill test. Also specialized staff is required to perform the treadmill test and hence the test will be more expensive. Bicycle ergometer requires no specialized staff. The nurses/ doctor can perform the test. Therefore I would like to recommend the use of Bicycle Ergometer for the evaluation of VO2 max to be used in my VBODE index.
Final Report
45
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Chapter 5: Discussions and Conclusions
Celli BR et al. [5] done experiments on patients and evaluated the following: Forced Expiratory Volume in one second ( FEV1 ) as a percentage (%) when compared to reference values based on age, gender, ethnicity and height. The best of the two Six-Minute Walk Tests performed at least 30 minutes apart. The degree of Dyspnea, measured with the use of the (MMRC Scale) Modified Medical Research Council Scale. The Body mass index FEV (Forced Expiratory Volume), FVC (Forced Vital Capacity) measurements The Hematocrit (the proportion of blood volume that is occupied by red blood cells. It is normally about 46% for men and 38% for women) and the albumin level (protein with water solubility) The Functional residual capacity and Inspiratory capacity.
Each of these possible explanatory variables was independently evaluated to determine its association with one-year mortality in a stepwise forward logistic-regression analysis. A subgroup of four variables had the strongest association [5]. Namely the, Forced Expiratory Volume in one second ( FEV1 ) as a percentage (%) when compared to reference values based on age, gender, ethnicity and height. The best of the two Six-Minute Walk Tests performed at least 30 minutes apart. The degree of Dyspnea, measured with the use of the (MMRC Scale)Modified Medical Research Council Scale. The Body mass index
Therefore Celli et al. created a BODE index which would help detect the prognosis (disease development) of lung disease, predict risk of death and predict hospitalization. In Critical Review 6 of chapter 7, Celli et al. work will be elaborated.
Final Report
46
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
However, I feel that BODE index is not efficient enough to predict the disease prognosis or hospitalization or risk of deaths. This is because the (VO2 max) (peak Oxygen consumption during exercise) value is the very first cardiopulmonary measured parameter that is examined for normal or compromised response [20]. (VO2 max) value is important for COPD evaluation [10 and 27]. Organs like lungs need to be progressively stressed so that the functional capacity of the lungs can be determined. In Six Minute Walk tests (6MWT), the lungs are not in progressive stress. In 6MWT, the patient walks on his own pace and will tend to slow down when tired despite the encouragement given by the tester. Thats why the organs are not under progressive stress. But in Cardiopulmonary Exercise Test, CPET -treadmill or cycle ergometer causes the organs to undergo progressive stress as the patient could not walk on his own pace [29]. For CPET, Cycle ergometer is better for the patient because it is safe, reliable and causes less strain on patients lower extremity muscles.
Hence I would encourage the use of my VBODE Index, a 13 point scale scoring system to better help monitor disease prognosis, predict hospitalization and predict the risk of death.
Final Report
47
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Chapter 6: Recommendations
The patient has to undergo the many tests to evaluate the VBODE index.
6MWT VBODE Index
B BMI
Dyspnoea
CEPT
Several Six-Minute walk tests till the best of the two Six-Minute Walk Tests performed at least 30 minutes apart is measured.
Final Report
48
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Spirometry Test to evaluate FEV1 (Forced Expiratory Volume in one second)
CEPT (cardiopulmonary Exercise Tests) to evaluate VO2 max (maximum oxygen consumption. Measurement of weight, height to evaluate BMI (Body Mass Index). Dyspnoea result. Questions asked grade the degree of a patient's breathlessness.
The patient will feel lethargic and irritated. He/she has to waste precious time waiting for the respective tests and undergo so many tests. At least half a day would be wasted. Future work can be done to arrange the tests in a way that everything can be finished in 1 or 2 hours. Future work may also exclude or modify the tests to save time. Future work may also modify my VBODE index to another simpler index. Future work may include additional Pulmonary Rehabilitation (PR) in the BODE Index/VBODE Index or replace some test with PR. PR is a medically supervised program that helps improve the health and well-being of people who have lung problems. PR may include an exercise program to determine the prognosis of lung disease, predict hospitalization and predict risk of death. PR also includes disease management training and nutritional and psychological counseling. The program aims to help one stay more active and carry out day-to-day activities. PR has proven effective in the improvement of the patients BODE Index [7, 15 and 31].
Final Report
49
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Chapter 7: Critical Reviews and Logs
Critical Review 1 A Critical Review of Donohue JF. Minimal Clinically Important Differences in COPD Lung Function, Journal of Chronic Obstructive Pulmonary Disease, March 2005; 2:111124. Using Jaeschkes (1989) [3], Beatons (2002) [11] definitions for MCID, Donohue conducted a study in an attempt to establish a MCID for FEV1. FEV1 is a physiological variable the forced expiratory volume in one second (FEV1). It is a readily available, inexpensive and standardized method which helps in the diagnosis, staging, treatment, monitoring and establishing prognosis for patients with COPD. The FEV1 is determined by the lung elastic recoil pressure, upstream frictional pressure loss, the cross-sectional area and pressure at the choke point. The MCID (Minimal Clinically Important Differences) in COPD lung function is a small difference in patients management in which patients perceive as beneficial, in the absence of troublesome side effects. This research is aimed to determine the general level of improvement in FEV1 which is both perceptible and clinically meaningful which corresponds well to normal activities, detect small airway disease and does correlate all that well with symptoms, survival and quality of life.
The study reveals that chronic obstructive pulmonary disease (COPD) is a common disease where tobacco smoking is the main risk factor for COPD, although other inhaled noxious particles and gases may contribute. The objectives of COPD management according to the GOLD (Global Obstructive Lung Disease) Guidelines, the ATS (American Thoracic Society) and the ERS (European Respiratory Society) are to adhere to the guidelines. Namely, to prevent disease progression, relieve symptoms, improve exercise tolerance, improve health status, prevent and treat complications, reduce mortality and minimize side effects from treatments. Spirometry helps in the diagnosis and staging of the severity of COPD. FEV1 and FVC (Forced Vital Capacity) are expressed in both absolute values (litres). For optimal performance of spirometry, standardized technique must be employed. One of the standards is that the patient must exhale down to a plateau and exhalation should usually exceed 6 seconds. ATS has issued guidelines for the standards of spirometry. For instance, spirometry must be capable of measuring volumes
Final Report
50
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
of at least 8 litres with an accuracy of at least +-3% or +-0.0050L with flows between Zero and 14L/S. Both the Gold Guidelines and the ATS/ERS stage the severity of COPD on the basis of Spirometry because it is readily available, inexpensive and standardized. The spirometer does not correspond well to normal daily activities, does not detect small airway disease and does not correlate all that with symptoms, survival, quality of life and economic outcomes.
In summary, since major decisions on COPD are based on the FEV1, Donohue stated that the MCID for FEV1 will be made for further study. To improve on the situation, proposals are recommended. Try to correlate FEV1 with functional indices such as BODE index which is currently in practice. The BODE index, a simple 10-point scale, multidimensional grading system to be used to correlate FEV1.It is better than the FEV1 at predicting the risk of death from any cause and from respiratory causes among patients with COPD. This may be a better indicator of survival in COPD. This index includes FEV1, Basal Metabolic Index (BMI), a Dyspnea Scale, and the six minute walk distance providing more functional data. Secondly Donohue wants to obtain additional data on lung volumes both in stable patients and during exercise when evaluating new modalities in the future. Relationship between the fitness of a subject and the subject with presence of lung disease will be determined. Additional considerations in MCID for FEV1, factors influencing MCID for FEV1, considerations in determining MCID for FEV1, other issues on the importance to define a MCID for FEV1 have been discussed. As these parts were irrelevant to my research study, I decided to skip the rest of the journal paper. This study has provided me with some insights on FEV1, MCID, spirometry and BODE index.
_______________________________________________________________________
Final Report
51
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Critical Review 2 A Critical Review of ZuWallack RL, Hashim A, McCusker C, et al. The Trajectory Of Change Over Multiple Outcomes Areas During Comprehensive Outpatient Pulmonary Rehabilitation, Journal of Chronic Repiratory Disease 2006; 3:11-18. Abstract: Aim: This study was conducted to find out the optimal duration of the exercise training component in pulmonary rehabilitation (PR) although PR has proven effective in multiple outcome areas of importance to the patient. For instance in exercise performance, dyspnea and health related quality of life. Background: PR (Pulmonary Rehabilitation) is a program for patients with chronic lung disease such as emphysema, chronic bronchitis, asthma, bronchiectasis and intersititial lung disease. This rehabilitation program helps in the restoration of the patient to the fullest medical, mental, emotional, social and vocational potential of which they are capable, hence improving the quality of life. PR includes emotional support, medical management, education, exercise, breathing, retraining and nutritional counseling. The dose of exercise training in PR reflects its intensity and duration. Both high intensity and low intensity approaches had proven effective in PR [4, 22 and 23].
Method: This study was conducted on 13 patients (5 male and 8 female) aged 668 years with their FEV1 3411% of predicted. PR was extended to 24 sessions over 12 weeks instead of the customary 16 sessions over 8 weeks. Outcomes assessments which were usually performed at the beginning and the end of pulmonary rehabilitation were changed and done more frequently. Initial assessments for PR included valuations by the nurse coordinator and medical director, review of medical and physicians office records, spirometry, and incremental cardiopulmonary exercise testing on treadmill. Each session included one-hour of group education, 45mins of light training and 30 mins of higher intensity exercise on a stationary cycle ergometer/ treadmill.
Results: Outcome variables were measured at baseline (immediately before rehabilitation), at weeks 2, 4, 6, 8, 10, 12, 16, 20 and 24. The results demonstrate that the effect of PR on exercise performance, dyspnea and health related quality of life occur early in the course of comprehensive outpatient pulmonary rehabilitation. The trajectory of improvement in exercise performance appears linear, with maximal short-term gains realized after at least 20 sessions. Conclusions: Although this study do lend support earlier studies showing better outcomes with longer durations, this study did not test changes in outcome following the completion of formal rehabilitation. Ideally the optimal duration of PR for the individual patient should depend on
Final Report
52
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
his/her baseline condition and the evaluation of ongoing progress during training. This study did not include an untreated control group. The number of subjects was small and the analyses was limited. Also subjects used in this study had severe airflow limitation (FEV 1 34% of predicted) making it difficult to apply these results to patients with less severe physiological impairment. A larger study would be helpful to confirm these observations.
Critical Review 3 A Critical Review of Tschopp JM. COPD: Moving Beyond Bronchodilation, Swiss Medical Weekly 2007; 137:161-165. Abstract: Aim: This journal paper is trying to prove that the concept of COPD has changed in the last years. COPD is a systemic disease affecting not only the lungs but many other organs of the patient. Cardiopulmonary exercise test assesses physiological and biological reserves but is not a most suitable test to assess the functional state of a systemic disease. Background: COPD, the 4th leading cause of death in the US and Europe (in 2007) is defined as airflow limitation with poor reversibility. COPD is a chronic disease where the severity of the disease cannot be assessed only on spirometer and any measurement of airway obstruction. It must be assessed with 6-minute walk test associated or not with the BODE index to better find disease-modifying interventions and to improve the outcome of COPD patients. Exercise testing is a most suitable test to assess the functional limitations of patients with a systemic disease such as COPD. The 6-minute walk test, a simple test is highly reproducible. It reflects real life limitations of the patients better. If the clinicians adhere to the defined standards of this test, the measurements are precise and it will be a good predictor of mortality. Laboratory exercise testing has been developed in the 1960s and was commonly known as spiro-ergometry when simultaneously recording respiratory and cardiac parameters. In 1982, Jones had written a manual of exercise testing
Final Report
53
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
summarizing knowledge of that time [12 and 13]. He had clearly shown that exercise testing should be considered an extension of the clinical examination. Since then exercise testing is used in the medical community. The treating physicians possess well defined graph plots with the response predicted for a normal individual.
Advantages of exercise test: 1) Very reproducible with simultaneous measurement 2) Allows precise definition of limitations of any individual patient 3) Considered as a gold standard in the evaluation of any patient suffering
In the 1960s, a simple test was developed to evaluate the walking distance during a defined period of time, eg the 12-minute walk test. This test would better represent functional activity in daily life. Later the 6-minute walk test (6MWT) was found to perform as well as the 12-minute walk test. It is now largely used because it is very simple and does not require special equipment and trained technicians. The 6MWT has now many recognized indications such as measuring results of medical interventions in patients with heart or lung diseases. Clinicians are therefore responsible for instructing technicians performing the test to assure continuous quality in measurements. It is the only way to get reliable data about a patients improvement related to medication or any other therapeutic intervention.
Minimal requirements for a 6MWT: 1) Corridor of 30 m free of any walk obstacle and 2 cones 2) Distance marked every 3 meters 3) Standardized instructions 4) At least two practice walks 5) Graded scale in meters 6) Standard encouragement 7) Supervision from behind 8) End exercise Borg scale (Appendix B)
Final Report
54
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
The 6MWT is standardized and the clinicians should adhere to the guidelines which provide a step-by step protocol and safety measures, define the preparation of the patient and procedures, and offer recommendations for the interpretation of results. If the recommended guidelines are adhered, this test is a very useful tool to assess the functional status of COPD patients and measure impairment in their daily life activity. BODE index is a multi-systemic grading assessing respiratory and systemic expressions of COPD which would better predict outcome in these patients. This index includes four parameters, ie the body mass index (B), the degree of airflow obstruction (O) as defined by FEV1, the level of dyspnoea (D) according to the modified Medical Research Council questionnaire (MMRC; table 1) and the exercise (E) capacity expressed as the distance walked in 6 minutes. One can therefore for each patient assess his/her own BODE index (table 2). This index has proven to be a much better predictor of survival than all the commonly used parameters. Table 1: Grade 1 :breathlessness with strenuous exercise Grade 2 :short of breath when hurrying on the level or walking up a slight hill Grade 3 :walks slower than people of the same age on the level or stops for breath when walking at own pace on the level Grade 4 :stops for breath after walking 100 meters Grade 5 :too breathless to leave the house, or breathless when dressing or undressing Note: Dyspnoea is a perception or the uncomfortable conscious awareness the patient has of his breathing. Table 2:
Final Report
55
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Method: There was no method used. Results: As no experiment was done, there are no results. Conclusions: From cardiopulmonary exercise test, the treating physicians possess welldefined graph plots of the patient with the response predicted for a normal individual. It is easy to rapidly recognize patterns of abnormalities and associated clinical disorders. Cardiopulmonary exercise test assesses physiological and biological reserves but is not a most suitable test to assess the functional state of a systemic disease. It is because this test is costly as it involves high powered and expensive technologies and specialized staffs are required to obtain important information about metabolic, cardiac, ventilatory or muscular limitation in diseases. Simpler exercise tests such as the 6-minute walk test associated or not to the BODE index to better find disease-modifying interventions and to improve the outcome of COPD patients are encouraged.
_____________________________________________________________________ Critical Review 4 A Critical Review of Cote CG and Celli BR. Pulmonary Rehabilitation and the BODE Index in COPD, European Respiratory Journal 2005; 26:630-636. Abstract: Aim: This study was conducted to find out whether (PR) Pulmonary Rehabilitation improves BODE index. Background: PR (Pulmonary Rehabilitation) is a program for patients with chronic lung disease such as emphysema, chronic bronchitis, asthma, bronchiectasis and intersititial lung disease. This rehabilitation program helps in the restoration of the patient to the fullest medical, mental, emotional, social and vocational potential of which they are capable, hence improving the quality of life. PR includes emotional support, medical management, education, exercise, breathing, retraining and nutritional counseling. The BODE index, which integrates body mass index, airflow limitation (forced expiratory volume in one second), dyspnoea and 6-min walk distance predicts mortality in COPD patients. Celli et al. developed the BODE index [5].
Final Report
56
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Method: This study was conducted on 246 patients (98% male) with similar age group with their BODE quartiles (2-4). These patients were divided into 2 groups, 116 patients who were willing to participate in PR and 130 patients who either do not want PR or dropped out of PR. These patients were monitored for at least two years. The 116 patients completed all sessions Results: Firstly for those with no PR, BODE worsened by 4% at 12 months and 18% at 2 years. Respiratory mortality at 2 years was 39%. Length of stay in hospitals for COPD increased 25%. But for those with PR, BODE improved by 19% and returned to baseline (normal category) after 2 years. Respiratory mortality at 2 years was 7%. The difference in respiratory mortality among PR and no PR group was 20 %.That means there were more respiratory-related hospitalizations in the no PR group. The length of stay in hospitals for COPD in the PR group decreased by 20%. Conclusions: PR participation improved BODE and is associated with better outcomes. The BODE index change after PR provides valuable prognostic information.
____________________________________________________________________
Final Report
57
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Critical Review 5 A Critical Review of Enright MD PL. The Six-Minute Walk Test, Respiratory Care, August 2003; Volume 48:No8. Abstract: Aim: This Journal paper is saying that the six-minute walk test is better than other walk tests (such as shuttle walk test) as it is safer, easier to administer, better tolerated and better reflects activities of daily living. Background: Instead of doing walk tests, patients functional capability can be assessed with a questionnaire or self report. For instance asking the patient How many flights of stairs can he/she climb or how many blocks can he/she walk? But this kind of information may overestimate or underestimate patients true functional capacity. Several kind of walking tests had been around since 1960s, when the 12 minute walk was found. These walking tests help assess a patients functional capacity. This 12 minute walk test was later modified to the present 6 minute walk test as it was found to provide the same result. ATS (American Thoracic Society) has issued guidelines to be adhered when performing the 6-minute walk test. There are minimal requirements for a 6 minute walk test. Namely, corridor of 30 m free of any walk obstacle and 2 cones, distance marked every 3 meters, standardized instructions, at least two practice walks, graded scale in meters, standard encouragement, supervision from behind, end exercise Borg scale. The 6MWT is standardized and the clinicians should adhere to the guidelines which provide a step-by step protocol and safety measures, define the preparation of the patient and procedures, and offer recommendations for the interpretation of results. If the recommended guidelines are adhered, this test is a very useful tool to assess the functional status of COPD patients and measure impairment in their daily life activity. This six minute walk test fairly accurately predicts morbidity and mortality from heart or lung disease. The shuttle walk test is better correlated with peak oxygen uptake, as measured by the full cardiopulmonary exercise test. But this shuttle walk test pressures the patient to meet deadlines, according to beeps from an audio cassette tape. Method: No experiment was done. Results: As no experiment was done, there was no result.
Final Report
58
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Conclusions: The six- minute walk test is a useful measure of functional capacity. It helps detect pulmonary and cardiac disease. However factors do influence the six-minute walk test. For instance shorter people and women having a shorter stride length, the elderly having reduced muscle mass, the less motivated all would have a decrease distance walked during the six minutes. The distance walked by the patient measured would be calculated and compared with similar age group results. Supplemental oxygen for COPD patients or other patients diagnosed with other lung disease would help improve 6MWD.
Critical Review 6 A Critical Review of Celli BR, Cote CG, Marin JM, et al. The Body-Mass Index, Airflow Obstruction, Dyspnea, and Exercise capacity Index in Chronic Obstructive Pulmonary Disease, March 4, 2004; Volume 350:1005-1012. Abstract: Aim: This Journal paper is proving that the BODE index, a simple 10-point multidimensional grading system devised is better than FEV1 at predicting the risk of death from any cause and from respiratory causes among patients with COPD. Background: COPD (Chronic Obstructive Pulmonary Disease) is characterized by an incompletely reversible limitation in airflow. A physiological variable- the forced expiratory volume in one second (FEV1) helps to grade the severity of COPD. But FEV1 is not accurate to access the diagnosis of COPD. The multidimensional 10- point grading system would help categorize and predict outcome in patients with COPD. Method: Firstly between 1995 and 1997, 207 patients were recruited. Age, sex, pack years of smoking, FVC (forced vital capacity), FEV1 measured in liters, and as a percentage of the predicted value according to the guidelines of the ATS (American Thoracic Society), the best of the two six-minute walk tests performed at least 30 minutes apart, the degree of dyspnea, measured with the use of the modified Medical
Final Report
59
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Research Council (MMRC) dyspnea scale, the functional residual capacity (the amount of air left in the lungs after a tidal breath out/ the amount of air that stays in the lungs during normal breathing)and inspiratory capacity (the maximal volume that can be inspired following a normal expiration), the hematocrit (the proportion of blood volume that is occupied by red blood cells. It is normally about 46% for men and 38% for women.), the albumin level (protein with water solubility) and the body mass index were determined. The Charlson index was used to predict mortality. Each of these possible explanatory variables was independently evaluated to determine its association with oneyear mortality in a stepwise forward logistic-regression analysis. The variables, body-mass index (B), the degree of airflow obstruction (O) and dyspnea (D), and exercise capacity (E), measured by the six-minutewalk test used to construct the BODE index, in which higher scores indicate a higher risk of death were secondly validated in a cohort of 625 patients, with death from any cause and from respiratory causes as the outcome variables.
Results: A subgroup of four variables had the strongest association. Namely the body mass index, FEV1 as a percentage of the predicted value, score on the MMRC scale, and the distance walked in six minutes (generalized r=0.21, P<0.001).These variables which predict important outcomes are easily measured. These four factors predict the risk of death. FEV1 as a percentage of the predicted value which is classified according to three stages identified by the ATS helps predict health status, the rate of exacerbation (bad to worse situation) and the risk of death. MMRC dyspnea scale helps predict the likelihood of survival among patients with COPD. Also it correlates well with other scales and health- status scores. The standardized 6-min walk test helps predict the risk of death in patients with COPD, patients who have undergone lung-reduction surgery, patients with congestive heart failure, and those with pulmonary hypertension. There were 25 deaths among the first 207 patients and 162 deaths (26 percent) in the validation cohort. Sixty-one percent of the deaths in the validation cohort were due to respiratory insufficiency, 14 percent to myocardial infarction, 12 percent to lung cancer, and 13 percent to other causes. Patients with higher BODE scores were at higher risk for death; the hazard ratio for death from any cause per one-point increase in the BODE score was 1.34 (95 percent confidence interval, 1.26 to 1.42), and the hazard ratio for death from respiratory causes was 1.62 (95 percent confidence interval, 1.48 to 1.77). The C statistic for the ability of the BODE index to predict the risk of death was larger than that for the FEV1 (0.74 vs. 0.65).
Final Report
60
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Conclusions: The BODE index, a simple multidimensional grading system, is better than the FEV1 at predicting the risk of death from any cause and from respiratory causes among patients with COPD. BODE index is simple to calculate and requires no special equipment.
Recommendation: To find out what is stepwise forward logistic-regression analysis? To find out how is hazard ratio and C statistic calculated? More research is needed to find these. Since in this study, only few women were recruited, the problem of the underdiagnosis in COPD in women exists.
Critical Review 7 A Critical Review of Kian CO, Suat JL and Cindy Seok CS. Does the Multidimensional Grading System (BODE) Correspond to Differences in Health Status of Patients with COPD? , International journal of COPD 2006, 1(1) 91-96. Abstract: Aim: Study objective was to verify whether to what extent the BODE index correlates with a disease-specific index of health status in patients with COPD. Background: Global initiative for chronic obstructive pulmonary disease (GOLD Expert Panel 2003) describes COPD as a slowly progressive disorder characterized by airflow obstruction that is not fully reversible. Spirometry derived parameter, FEV1 is a simple and valid measurement of the degree of airflow obstruction determining the COPD severity. Previously it has been shown that the FEV1 -based staging system by the (GOLD) corresponds to important differences in health status .But previous study by (Mahler et al 1984 [14]), [41] had revealed that FEV1 correlates poorly with patients symptoms, quality of life, exacerbation frequency and exercise intolerance. Also previous study by (Celli et al 2004 [5]) had revealed that BODE index is better than the FEV1 , at predicting the risk of
Final Report
61
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
death among patients with COPD.BODE assessment is a multidimensional grading system which is better than the FEV1 , to predict the risk of death among patients with COPD. This scoring system incorporates an assessment of symptoms, (body habitus -dyspnea and body mass index), exercise capacity and spirometric measure of airflow ( FEV1 ).Although the BODE index has shown to be a predictor of the risk of death; it is not known whether this index is a useful indicator of patients health status as well. Method: Between October 2003 and April 2004, 100 patients with stable COPD in experiment were recruited from the outpatient clinic of a single institution. Diagnosis of COPD was established by a respiratory physician based on medical history, current symptoms and available pulmonary function tests following the (GOLD) guidelines. Patients completed the St Georges Respiratory Questionnaire (SGRQ).The SGRQ is a standardized, self administered pulmonary-specific health status questionnaire containing 50 items that is divided into 3 subscales: symptoms (8 items), activity (16items), and impacts (26 items). SGRQ scores were calculated using score calculation algorithms. The higher the SGRQ score, the worse is the situation.
Results: The BODE index was calculated for each patient using variables obtained within 2 weeks of enrolment. The Higher BODE scores are associated with higher (worse) SGRQ scores. Conclusions: The BODE scoring system is better correlated to health status as assessed by a disease- specific index for COPD than the GOLD staging criteria based largely on the FEV1 . The study concluded that the BODE scoring system corresponds to important differences in health status of patients with COPD. BODE index is a better predictor of the risk of death in COPD patients compared with the FEV1 -based staging system by the American Thoracic society (ATS). This experiment was done on 90 males and 10 females only. Few females (only 10%) were included. Therefore, the findings from the current study may not be applicable to both sexes.This experiment was done for age groups 70.8 7.9 years old. Thus, the findings from the current study could only be applicable to that group of patients. Recommendations: Have equal number of both sexes in the experiment and have groups of patients with different age groups.
Final Report
62
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Critical Review 8 A Critical Review of Starobin D, Kramer MR, Yarmolovsky A, et al. Assessment Of Functional Capacity In Patients With Chronic Obstructive Pulmonary Disease: Correlation Between Cardiopulmonary Exercise, 6 Minute walk and 15 step Exercise Oximetry Test. IMAJ Volume 8, (July 2006); 8:460-463. Abstract: Aim: Study objective of this study was to determine whether reliable data could be obtained at a lower cost. Background: Different tests are used to evaluate the functional capacity in chronic obstructive pulmonary disease. Pulmonary function test. This test included spirometry, lung volume, maximal voluntary ventilation and diffusion capacity by single-breath technique. For calibration, a 3 L syringe was used at the beginning of each session on each day. Measurements were corrected for body temperature and pressure saturation. Testing was performed with the Medical Graphics Pulmonary Function System. Lung volumes were obtained by body plethysmography. MVV (maximal voluntary ventilation) was assessed by asking the patient to breathe as fast and deep as possible for 12 seconds, and the result was multiplied by 5. Cardiopulmonary exercise test. This exercise testing was done in labs. Patients were encouraged to take their medications as usual. Each participant underwent an incremental exercise test according to the protocol. On arrival at the exercise laboratory, patients were connected to a 12-lead with a single-lead monitor. Oxygen saturation ( SaO2 ) was measured by pulse oximetry and blood pressure with a sphygmomanometer. The patient was then positioned on an electrically braked cycle ergometer. After a 2 minute rest (arms at sides) the patients performed unloaded pedalling for 2 minutes at a rate of 60 rpm. The load was then progressively increased by 15 watts/min (ramp protocol). The duration of the test was symptom-limited; the endpoint was defined as the point at which the patient could not maintain a pedalling rate of more than 40 rpm. Cardiopulmonary data were collected and analyzed with an Exercise metabolic unit (CPX, Medical Graphics). Heart rate, minute ventilation, tidal volume (VT), oxygen consumption ( VO2 ), carbon dioxide production ( VCO2 ), oxygen pulse ( O2 P ) and oxygen saturation ( SaO2 ) were recorded and calculated over 30 second intervals using standard formulas. Blood pressure was measured with a sphygmomanometer at rest and every 2 minutes until peak exercise. The dyspnea index (VE/MVV), expressed in percent, and was calculated manually. ie. VE = minute ventilation.
Final Report
63
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
6 minute walk test. This 6 min walk test was performed along a measured indoor. Participants were encouraged to cover as much distance as possible. Protocols should be adhered. 15 step exercise oximetry test. A finger oximeter with continuous online recording of heart rate and oxygen saturation was connected to each patient. Data were sampled every 2 seconds, and the mean value was recorded every 10 seconds. A step measuring 25 x 25 x 20 cm was used. Patients were asked to climb up and down the step 15 times as fast as they could (without any fixed pacing). Each test was repeated twice, and the mean value was taken. When oximeter readings were not optimal, as indicated by yellow or red signals, the data were discarded. The time of exercise was recorded (exercise time), as was the time from start to lowest saturation (desaturation time).The total test time was defined as the time from the start of exercise to complete recovery. Baseline oxygen saturation, lowest saturation, and highest heart rate were recorded as well. The cardiopulmonary exercise test is considered the gold standard (expensive), but the 6 minute walk and the 15 step exercise oximetry test are considerably less expensive.
Method: The study sample consisted of 50 patients with mild to severe COPD. All underwent pulmonary function test and the cardiopulmonary exercise test, 6 minute walk and 15 step exercise oximetry test. The study was conducted over a 6 month period. The patients had stable COPD for the 2 months preceding the study. COPD was diagnosed according to the criteria of the ATS (American Thoracic Society).Patients with any acute or chronic cardiac disease, or other pulmonary or infective diseases within 2 months preceding the trial were excluded.
Results: Lung function test. Pulmonary function test revealed severe COPD in most of the patients, mean FEV1 was 46.3 19.9% of predicted value (range 99% to 16%). There was no statistically significant correlation between the pulmonary function test results and exercise tests. Exercise test. Mean VO2 max was 13.5 4.1 ml/kg/min. 37 patients had severe disability (mean VO2 max 12.0 3.5 ml/kg/min), 9 had moderate disability (16.2 1.1 ml/kg/min) and 4 had mild disability (21.4 0.5 ml/kg/min).The mean 6 minute walk distance was 434.7 88.0 m. Disability was severe in 19 patients, moderate in 28 and mild in 4.
Patients were classified according to the VO2 max results obtained by CPXT (exercise test) as mild, moderate or severe impairment. Separate grading was also done for the 6 minute walk and 15 step exercise oximetry test [Table 1], and the results were compared with the CPXT.
Final Report
64
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
21-24
Conclusions: There was a good correlation between the CPXT and the 6 minute walk test. No correlation was noted between the 15 step exercise oximetry test results and either the CPXT or the 6 min walk test. Analysis of the relationship between the CPXT, the 6 minute walk and the 15 step exercise oximetry test showed a significant correlation for the functional capacity findings between the CPXT and the 6 min walk test. The strongest correlation was found for the mild and moderate disability classes. Specifically, all patients with mild disability by the CPXT ( VO2 max > 20 ml/kg/min) achieved a distance of more than 520 m on the 6 min walk, whereas those with moderate disability by the CPXT ( VO2 max between 1520 ml/kg/min) achieved a distance of not less than 420 m. The correlation was less clear in the severe disability CPXT subgroup ( VO2 max < 15 ml/kg/min), which had a wide distribution of results on the 6 min walk from 250 to 550 m. This study concluded that the 6 minute walk test is cheap, relatively reliable and is an accurate test for the assessment of functional capacity in patients with COPD. The 15 step exercise oximetry test, however is not reliable. The mean age of the participants was 64.3 11.7 years (range 2778 years); 28 were male and 22 female. The sample size is small and this result only applies to this agegroup of elderly. _________________________________________________________________
Final Report
65
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Critical Review 9 A Critical Review of Sanchez FF, Faganello MM, Tanni SE, et al. Relationship between Disease Severity and Quality of Life in Patients with Chronic Obstructive Pulmonary Disease. Brazilian Journal of Medical and Biological Research, October 2008; Volume 41(10): 860-865.
Abstract: Aim: Study objective of the present study was to investigate the relationship of forced expiratory volume in 1 s (FEV1), body mass index, fat-free mass index, 6-min walk test (6MWT) results, dyspnea sensation and peripheral oxygen saturation (SpO2) with the quality of life of COPD patients. Background: Global initiative for chronic obstructive pulmonary disease (GOLD Expert Panel 2003) describes COPD as a slowly progressive disorder characterized by airflow obstruction that is not fully reversible. Spirometry derived parameter, FEV1 is a simple and valid measurement of the degree of airflow obstruction determining the COPD severity. Previously it has been shown that the FEV1 -based staging system by the (GOLD) corresponds to important differences in health status [32].But previous study by [2 and 14] had revealed that FEV1 correlates poorly with patients symptoms, quality of life, exacerbation frequency and exercise intolerance. Also previous study by [5] had revealed that BODE index is better than the FEV1 , at predicting the risk of death among patients with COPD.BODE assessment is a multidimensional grading system which is better than the FEV1 , to predict the risk of death among patients with COPD. This scoring system incorporates an assessment of symptoms, (body habitus -dyspnea and body mass index), exercise capacity and spirometric measure of airflow ( FEV1 ).Although the BODE index has shown to be a predictor of the risk of death; it is not known whether this index is a useful indicator of patients health status as well. Method: Between October 2003 and April 2004, 100 patients with stable COPD in experiment were recruited from the outpatient clinic of a single institution. Diagnosis of COPD was established by a respiratory physician based on medical history, current symptoms and available pulmonary function tests following the (GOLD) guidelines. Patients completed the St Georges Respiratory Questionnaire (SGRQ).The SGRQ is a standardized, self administered pulmonary-specific health status questionnaire containing 50 items that is divided into 3 subscales: symptoms (8 items), activity
Final Report
66
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
(16items), and impacts (26 items). SGRQ scores were calculated using score calculation algorithms. The higher the SGRQ score, the worse is the situation.
Results: The BODE index was calculated for each patient using variables obtained within 2 weeks of enrolment. The Higher BODE scores are associated with higher (worse) SGRQ scores. Conclusions: The BODE scoring system is better correlated to health status as assessed by a disease- specific index for COPD than the GOLD staging criteria based largely on the FEV1 . The study concluded that the BODE scoring system corresponds to important differences in health status of patients with COPD. BODE index is a better predictor of the risk of death in COPD patients compared with the FEV1 -based staging system by the American Thoracic society (ATS). This experiment was done on 90 males and 10 females only. Few females (only 10%) were included. Therefore, the findings from the current study may not be applicable to both sexes.This experiment was done for age groups 70.8 7.9 years old. Thus, the findings from the current study could only be applicable to that group of patients. Recommendations: Have equal number of both sexes in the experiment and have groups of patients with different age groups.
Final Report
67
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
LOG 1 NAME: Mohamed Reza SIM ID: W0503059 SUPERVISOR: Dr Lim Geok Hian Date of Meeting: 07/02/2009 Time of Meeting: 1400hrs-1430hrs Venue: SIM
Matters Discussed: Advice from Supervisor: Has to work hard. A successful project comes from a lot of hard work. Measures taken and solutions for a problem must be meaningful. A problem must have the best solution. For instance, instead of the solution being the glass must be thick enough to withstand the weight, the solution could be the glass must be at least 10mm to withstand the weight. Question: What does index stands for? Answer: It is the desired/ accurate value for TMA 01 due on 27th February.
Consensus/Decision Taken: Has to read Journals and books to gather information for the project. TMA 1 is due in few more days. Has to work harder.
Final Report
68
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
LOG 2 NAME: Mohamed Reza SIM ID: W0503059 SUPERVISOR: Dr Lim Geok Hian Date of Meeting: 04/03/2009 Time of Meeting: 1730hrs-1830hrs Venue: Novena Square (Burger King)
Matters Discussed: TMA01 Gantt chart not in detail. Journal Reviews not done.
Insufficient journals read. To obtain journals from Sciencedirect.com To see if MOH website has any relevant data on COPD.
To also get and read journal papers from Uni-SIM library and Google scholar.
To evaluate the most appropriate Index in the prognosis of lung disease (COPD). Has to judge which data is important for the determination of this index. Is it BMI and/or FEV1 and/or Cardio-pulmonary exercise testing and/or etc? To plot graph. May use Microsoft Excel, Mat lab or any software from SIM Labs.
Final Report
69
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Consensus/Decision Taken:
To do a detailed Gantt chart on the progress of my project. To read Journal papers from Uni-SIM library website, Google Scholar. To review on the journal papers read. To gather information from Science direct website and MOH website. To understand on the current method being used to evaluate the BODE index. Then evaluate ways to improve on the current situation. To plot graph.
Final Report
70
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
LOG 3 NAME: Mohamed Reza SIM ID: W0503059 SUPERVISOR: Dr Lim Geok Hian Date of Meeting: 16/05/2009 Time of Meeting: 1000hrs-1100hrs Venue: Novena Square (Burger King)
Matters Discussed: Interim report References to be in right format. If there are 3 or more authors to the journal paper et al. to be used. In the interim report, referencing to be improved.
Gantt chart-the key due date to be stated clear.
Aim of the project is to be able to understand the subject clearer, be advanced and see ways to improve on current situation. To read more of the latest journal papers and keep up with the latest trend. If possible, try to understand the hospitals protocol in dealing with COPD patients. Is the index I created (VBODE) better than available BODE index?
Final Report
71
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Consensus/Decision Taken: To do a detailed Gantt chart on the progress of my project. To read more Journal papers. To review on the journal papers read. To familiarize with C++ builder software. To develop program for both hospital staff and patient. To prove the VBODE index is better and more appropriate than the available BODE index in the prognosis of lung disease (COPD) To evaluate graphs.
Final Report
72
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
LOG 4 NAME: Mohamed Reza SIM ID: W0503059 SUPERVISOR: Dr Lim Geok Hian Date of Meeting: 11/07/2009 Time of Meeting: 1030hrs-1130hrs Venue: Novena Square (Burger King)
Matters Discussed: Programming Change the D.O.B to Age. Omit the IC No as some patients may use foreign passports. Avoid different colours. Black must be consistent.
VBODE Index
BMI (Body mass index) is calculated as weight (in Kg) divided by square of height (in m2) The BMI differs in male from female. Units should be shown for BMI (Kg/ m2). Is MMRC Dyspnea Scale same/different from MRC Dyspnoea Scale? Calculation of FEV1 (% of predicted as measured by spirometry) - is it the FEV1 ratio? Why Six-min walk test and not longer or shorter?
Final Report
73
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
The treadmill test (Cardiopulmonary exercise test) duration? The intensity of the exercise is increased incrementally until symptoms limit testing or the patient reaches maximal levels.
What are VQ measurements from the cardiopulmonary exercise test?
To show a scale where green indicate the patient as mildly obstructive, pink indicating the patient as severely obstructive and dark red indicating the patient as critically obstructive. Aim of the project is to be able to understand the subject clearer, be advanced and see ways to improve on current situation. Insufficient work done and not up to standard.
Consensus/Decision Taken: To reread the journal papers and criticize on their writings. To read more Journal papers. To expand the project. Spend more hours on capstone project.
Final Report
74
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
LOG 5 NAME: Mohamed Reza SIM ID: W0503059 SUPERVISOR: Dr Lim Geok Hian Date of Meeting: 07/09/2009 Time of Meeting: 1730hrs-1830hrs Venue: Novena Square
Matters Discussed: Programming Round up the data calculated to 2 decimal place. In the final report, write about the algorithms of C++. To prove how is VBODE index better than BODE index in determining the risk of deaths and hospitalization for patients diagnosed with COPD.
BMI (Body mass index) is calculated as weight (in Kg) divided by square of height (in m2). To find out why is the value fixed at either <21 kg/ m2 or >= 21 kg/ m2 ?
The calculation of BMI is the same in male and female for BODE index. However
BMI is not accurate for pregnant mum, nursing mums, elderly and sportsman. MMRC (Modified Medical Research Council) Dyspnea Scale is also referred to as MRC (Medical Research Council) Dyspnoea Scale. Calculation of FEV1 (% predicted as measured by spirometry) is the FEV1 ratio. FEV1 is calculated in litres. Then it is compared with similar age, size and ethnic group. (Actual value of FEV1 in litres / Estimated FEV1 value for that group)*100%
Final Report
75
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
The Six-min walk test is fixed at 6 mins by the ATS (American Thoracic Society) and the ERS (European Respiratory Society). Protocols should be adhered. For instance patients need to be encouraged during the test. Previously it used to be 12mins and now 6mins is proven to produce the same reliable results. The treadmill test (Cardiopulmonary exercise test) duration? The intensity of the exercise is increased incrementally until symptoms limit testing or the patient reaches maximal levels. To read others critical reviews on journal papers. To do critical reviews and send in to DR LIM for editing. Start on the first two chapters in the final report. Referencing should be consistent.
Final Report
76
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Chapter 8: Reflections
o Initially I misunderstood the question. I spent a lot of time searching for journals and data relating to Spirometer and BODE Index. I thought that I must derive an index replacing the BODE. I came to dead-end because I had no idea what I can do. I reread the question, read several journals and information from websites and then realized I have a way to come up with an index to predict the risk of deaths, predict hospitalisations and prognosis of disease in COPD diagnosed patients. I was slow and running out of time. During the first 6 month ,the Gantt chart helped me to manage the progress of the project and achieve my target at a point in time. The Gantt chart allowed me to see how remedial action can bring my project back on track. Then after July I could not keep up with the schedule. Gantt chart in TMA 01 compared with the current Gantt chart, has changed very much. Towards the last two months, I had to rush. Now I have learnt how important the Gantt chart is for success. Instead of talking about the positive and negative of journal papers, initially I criticised the journal papers. Dr Lim corrected me. I should do Critical Review and not criticise review. Some of the journals papers read were of no use. In other words, it was very far from the topic. For example. Treatments and Medication of COPD, etc. Now I have learnt how to pick relevant and the most appropriate journals. I had problem saving my application programming due to insufficient memory space. I had to clear up some memory space. Once I opened up my C# software. There was an error message. Corrupted File. I could not open the program. I didnt know what to do. I was stuck. I thought I had to redo the source codes. Luckily the next day, when I reopen the program, it worked smoothly.
o o
Final Report
77
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
References
[1]. Alsaeedi A, Sin DD and McAlister FA. The Effects of Inhaled Corticosteroids in Chronic Obstructive Pulmonary Disease, A Systemic Review Of Randomized Placebo-Controlled Trials, American Medical Journal 2002; 113:59-65.
[2]. Antonelli IR, Imperiale C, Bellia V, et al. Do Gold Stages of COPD Severity Really Correspond to Differences in Health Status, European Respiratory Journal 2003; 22:444-449.
[3]. Beaton DE, Boers M and Wells GA. Many Faces of the Minimal Clinically Important Differences (MCID): A Literature Review and Directions for Future Research, Curr Opin Pheumatol 2002; 14:109-114.
[4]. Casaburi R, Patessio A, Ioli F, et al. Reductions in Exercise Lactic Acidosis and Ventilation as a Result of Exercise Training in Patients with Obstructive Lung Disease, American Review Respiratory 1991; 143:9-18.
[5]. Celli BR, Cote CG, Marin JM, et al. The Body-Mass Index, Airflow Obstruction, Dyspnea, and Exercise capacity Index in Chronic Obstructive Pulmonary Disease, March 4, 2004; Volume 350:1005-1012.
[6]. Celli BR, Macnee W, Agusti AGN, et al. Standards for the Diagnosis and Treatment of Patients with COPD: A Summary of the ATS/ERS Position Paper, European Respiratory Journal, Feb 2004; 23:932-946.
Final Report
78
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
[7]. Cote CG and Celli BR. Pulmonary Rehabilitation and the BODE Index in COPD, European Respiratory Journal 2005; 26:630-636. [8]. Donohue JF. Minimal Clinically Important Differences in COPD Lung Function, Journal of Chronic Obstructive Pulmonary Disease, March 2005; 2:111-124.
[9].
Enright MD PL. The Six-Minute Walk Test, Respiratory Care, August 2003; Volume 48: No8.
[10]. Eschenbacher WL and Mannina A. An Algorithm for the Interpretation of Cardiopulmonary Exercise Tests, Chest, Feb 1990; 97:263-267. [11]. Jaesche R, Singer J, Guyatt GH. Measurement of Health Status
Ascertaining the Minimal Clinically Important Difference, Control Clinical Trials 1989; 10:407-415.
[12]. Jones NL. Editorial. Not Enough Exercise, Thorax. 1982; 37:793794.
[13]. Jones NL and Campbell EJM. Clinical Exercise Testing, WB Saunders Company, London 1982.
[14]. Jones PW, Quirk FH, Bavestock CM, et al. A Self-Complete Measure of Health Status for Chronic Airflow Limitation, American Medical Journal 1992; 145: 13211327.
[15]. Kian CO, Suat JL and Cindy Seok CS. Does The Multidimensional Grading
System (BODE) Correspond To Differences In Health Status Of Patients With COPD?, International journal of COPD 2006; 1(1):91-96.
Final Report
79
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
[16]. Kian Co, Weiberg Fc and Patessio NC. Pulmonary Disease in Primary Healthcare, National Healthcare Group Polyclinics and Department of Respiratory Medicine (Tan Tock Seng Hospital).
[17]. Landbo C, Prescott E, lange P, et al. Prognostic Value of Nutritional Status in Chronic Obstructive Pulmonary Disease, American Journal Respiratory Critical Care Medical 1999; 160:1856-1861.
[18]. Mahler DA and Wells CK. Evaluation of Clinical Methods for Rating Dyspnea, Chest, March 1988; 93(3): 580-586.
[19]. Mahler DA, Weinberg DH, Wells CK, et al. The Measurement of Dyspnea: Contents, Agreement and Physiological Correlates of Two New Clinical Indexes, Chest 1984; 85: 751-758.
[20]. Mashikian V. Understanding Cardiopulmonary Stress Test Results: Is it the heart or the lungs?, Current Applications and Economics.
[21]. Miller MR, Hankinson J, Brusasco V, et al. ATS-ERS Taskforce : Standardisation of Lung Function Testing, Standardisation of Spirometry, European Respiratory Journal 2005, 26;31938.
[22]. Normandin EA, McCuskerC, Connors M, et al. An Evaluation Of Two Approaches To exercise Conditioning In Pulmonary Rehabilitation, Chest 2002; 121:1085-1091.
[23]. Puente-Maestu L, Sanz ML, Cubillo JM, et al. Comparison of Effects of Supervised Versus Self-Monitored Training Programs in Patients with Chronic Obstructive Pulmonary Disease, European Respiratory Journal 2000; 15:517-526.
Final Report
80
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
[24]. Roca J, Whipp BJ, Agusti AGN, et al. Clinical Exercise Testing with Reference to Lung Diseases: Indications, Standardization and Interpretation Strategies, European Respiratory Journal 1997; 10:2662-2689.
[25]. Sanchez FF, Faganello MM, Tanni SE, et al. Relationship Between Disease
Severity and Quality of Life in Patients with Chronic Obstructive Pulmonary Disease. Brazilian Journal of Medical and Biological Research, October 2008; Volume 41(10):860-865.
[26]. Schols AM, Slangen J,Volovics L, et al. Weight Loss is a Reversible Factor in the Prognosis of Chronic Obstructive Pulmonary Disease, American Journal Respiratory Critical Care Medical 1998; 157:1791-1797.
[27]. Starobin D, Kramer MR, Yarmolovsky A, et al. Assessment of Functional
Capacity in Patients with Chronic Obstructive Pulmonary Disease: Correlation between Cardiopulmonary Exercise, 6 Minute walk and 15 step Exercise Oximetry Test. IMAJ Volume 8, (July 2006); 8:460-463.
[28]. Tschopp JM. COPD: Moving Beyond Bronchodilation, Swiss Medical Weekly 2007;137:161-165.
[29]. Weisman IM , ATS Committee on proficiency standards for Clinical Pulmonary Function Laboratories ATS Statement. Guidelines for the SixMinute Walk Test, American Journal of Respiratory and Critical Care Medicine, 2002; Volume 166(1):111-117.
[30]. Weisman IM, ATS Committee and the ACCP Health Science Policy Committee.ATS/ACCP Statement on Cardiopulmonary Exercise Testing,
Final Report
81
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
American Journal of Respiratory and Critical Care Medicine, 2003, Volume 167; 211-277.
[31]. ZuWallack RL, Hashim A, McCusker C, et al. The Trajectory of Change over Multiple Outcomes Areas during Comprehensive Outpatient Pulmonary Rehabilitation, Journal of Chronic Respiratory Disease 2006; 3:11-18.
[32]. Global Initiative for Chronic Obstructive Lung Disease (GOLD).Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. Bethesda (MD): Global Initiative for Chronic Obstructive Lung Disease, 2005. http://www.goldcopd.org.
[33]. http://www.copdas.com/ [34]. http://en.wikipedia.org/wiki/Chronic_obstructive_pulmonary_disease [35]. http://medcalc3000.com/ [36]. http://wwww.cdc.gov/healthyweight/assessing/bmi/index.html [37]. http://www.hpb.gov.sg/health_articles/bmi [38]. Ministry of Health. Health Facts Singapore 2005. http://www.gov.sg/moh. [39]. World health Organization. Burden of COPD. http://www.who.int/respiratory/ copd/burden/en/.
Final Report
82
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
[40]. Lab data from Ms.Neo Pei Ling Final report ( Jan07/BSBE/12)- Cardiac Analysis from Stress Testing.
Final Report
83
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Appendix A: BMI Chart for Children
Young children naturally start out with high body fat, but tend to get leaner as they get older. Girls and boys also have different body compositions. To take into account the differences between boys and girls and children of different ages, a special BMI for children was created, called BMI-for-age. A set of growth charts to track the development of children and young adults between ages of 2 and 20 were used. The BMI-for-age figures in a childs height, weight and age helps determine how much body fat he/she has. It compares the results to those of the other children of the same age and gender, and can help predict whether children will be at risk for being overweight when they get older.
Final Report
84
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Each chart contains a set of curved lines indicating the childs percentile. For instance, if a 15-year old boy is in the 75th percentile for BMI, 75% of boys of the same age have a lower BMI. He is at a normal weight.
The normal BMI range becomes higher for girls as they mature, because teenage girls normally have more body fat than teenage boys. A boy and girl of the same age may have the same BMI, but the girl could be of normal weight and the boy could be at risk of overweight.
Final Report
85
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Appendix B: The BORG scale
The Borg Scale is used to measure your sensation of breathlessness during various activities. Monitoring your breathlessness can help you safely adjust your activity by speeding up or slowing down your movements. It can also provide important information to your health care provider. Important points to remember: Should never go higher than 4 on the scale. If your breathlessness is Somewhat Severe or worse, you need to stop what you are doing and rest. If exercising and your breathlessness is only very, very slight (less than 1 on the scale), then you should work a little harder. Should use the scale to make note of any changes that occur and report them to your health care provider. For example, an activity that made you very slightly breathless (1 on the scale) a month age now makes you moderately breathless (3 on the scale) or vise versa. SCALE 0 0.5 1 2 3 4 5 6 7 8 9 10 SEVERITY No Breathlessness At All Very Very Slight (Just Noticeable) Very Slight Slight Breathlessness Moderate Somewhat Severe Severe Breathlessness Inbetween 5 and 7 Very Severe Breathlessness Inbetween 7 and 9 Very Very Severe (Almost Maximum) Maximum
Final Report
86
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Appendix C: Source Codes for (C#) C- Sharp Programming
File.cs
using using using using System; System.Collections.Generic; System.Text; System.IO;
namespace REZAHEALTHCLINIC { class File { private String filename = "C:\\Documents and Settings\\Mohamed Reza\\Desktop\\Reza Capstone Prog\\REZAHEALTHCLINIC\\Files\\Data.txt"; //"C:\\REZAHEALTHCLINIC\\Files\\Data.txt" //C:\\Documents and Settings\Mohamed Reza\Desktop\Reza Capstone Prog\Files private private private private private private private int int int int int int int threshhold_def = 80; defVO = 1000; defFEV = 1000; defMRC = 1000; defBMI = 1000; defWalk = 5; defVBODE = 0;
private List<Patient> patients = new List<Patient>(); private StreamReader sr; private StreamWriter sw; private private private private private private private private private private private private private List<String> List<String> List<String> List<String> List<String> List<String> List<String> List<String> List<String> List<String> List<String> List<String> List<String> dt; ic; name; gender; age; race; survey; vo; fev; mrc; bmi; walk; vbode;
Final Report
87
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE public void initpatients() { dt = new List<String>(); ic = new List<String>(); name = new List<String>(); gender = new List<String>(); age = new List<String>(); race = new List<String>(); survey = new List<String>(); vo = new List<String>(); fev = new List<String>(); mrc = new List<String>(); bmi = new List<String>(); walk = new List<String>(); vbode = new List<String>(); } public List<Patient> getPatients() { return patients; } public Boolean loadPatients() { Boolean success = false; String textline = null; //load information from file to temp variables try { sr = new StreamReader(filename); textline = sr.ReadLine(); if (textline != null) { initpatients(); } while (textline != null) { processline(textline); textline = sr.ReadLine(); } sr.Close(); } catch { } //completed loading info //check temp variables for read errors and convert to object try { int count = dt.Count; if (ic.Count == count && name.Count == count && gender.Count == count && age.Count == count && race.Count == count &&
Final Report
88
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE survey.Count == count && vo.Count == count && fev.Count == count && mrc.Count == count && bmi.Count == count && walk.Count == count && vbode.Count == count) { for (int i = 0; i < ic.Count; i++) { patients.Add(new Patient(dt[i], ic[i], name[i], gender[i], age[i], race[i], survey[i], vo[i], fev[i], mrc[i], bmi[i], walk[i], vbode[i])); } dt = null; ic = null; name = null; gender = null; age = null; race = null; survey = null; vo = null; fev = null; mrc = null; bmi = null; walk = null; vbode = null; success = true; } } catch { } //finished checking and converting return success; } private void processline(String line) { try { if (line != null) { //check if line is to be neglected if (line.StartsWith("*")) { //do nothing } //check if line is Date else if (line.StartsWith(">Date:") && line.Length > { line = line.Substring(6); dt.Add(line); } 6)
//check if line is IC else if (line.StartsWith(">IC:") && line.Length > 4) { line = line.Substring(4);
Final Report
89
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE ic.Add(line); } //check if line is Name else if (line.StartsWith(">Name:") && line.Length > 6) { line = line.Substring(6); name.Add(line); } //check if line is Gender else if (line.StartsWith(">Gender:") && line.Length > 8) { line = line.Substring(8); gender.Add(line); } //check if line is Age else if (line.StartsWith(">Age:") && line.Length > 5) { line = line.Substring(5); age.Add(line); } //check if line is race else if (line.StartsWith(">Race:") && line.Length > 6) { line = line.Substring(6); race.Add(line); } //check if line is Survey else if (line.StartsWith(">Survey:") && line.Length > 8) { line = line.Substring(8); survey.Add(line); } //check if line is VO else if (line.StartsWith(">VO:") && line.Length > 4) { line = line.Substring(4); vo.Add(line); } //check if line is FEV else if (line.StartsWith(">FEV:") && line.Length > 5) { line = line.Substring(5); fev.Add(line); } //check if line is Name else if (line.StartsWith(">MRC:") && line.Length > 5)
Final Report
90
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE { line = line.Substring(5); mrc.Add(line); } //check if line is BMI else if (line.StartsWith(">BMI:") && line.Length > 5) { line = line.Substring(5); bmi.Add(line); } //check if line is Walk else if (line.StartsWith(">WALK:") && line.Length > 6) { line = line.Substring(6); walk.Add(line); } //check if line is VBODE else if (line.StartsWith(">VBODE:") && line.Length > 7) { line = line.Substring(7); vbode.Add(line); } } } catch { } } public Boolean storePatients(List<Patient> updated) { Boolean success = false; //write information back to file if (updated.Count > 0) { try { sw = new StreamWriter(filename); sw.WriteLine("************************************** *******************************"); sw.WriteLine("\n****************FILE To STORE PATIENT RECORDS************************"); for (int i = 0; i < updated.Count; i++) sw.WriteLine("\n**********************PATIENT " + (i + 1).ToString() + " RECORD*******************************"); sw.WriteLine("\n>Date:" + updated[i].dt); sw.WriteLine("\n>IC:" + updated[i].ic); sw.WriteLine("\n>Name:" + updated[i].name); sw.WriteLine("\n>Gender:" + updated[i].gender); sw.WriteLine("\n>Age:" + updated[i].age);
Final Report
91
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE sw.WriteLine("\n>Race:" + updated[i].race); sw.WriteLine("\n>Survey:" + updated[i].survey); sw.WriteLine("\n>VO:" + updated[i].vo); sw.WriteLine("\n>FEV:" + updated[i].fev); sw.WriteLine("\n>MRC:" + updated[i].mrc); sw.WriteLine("\n>BMI:" + updated[i].bmi); sw.WriteLine("\n>WALK:" + updated[i].walk); sw.WriteLine("\n>VBODE:" + updated[i].vbode);
} sw.WriteLine("\n*****************************END**** *********************************"); sw.Close(); success = true; } catch { success = false; } } //finished writing return success; } public Boolean saveSurvey(String newIC, String newname, String newage, String newgender, String newrace, float newsurvey) { Boolean success = false; try {
String newdate = DateTime.Now.ToShortDateString(); float sur = newsurvey / 45; String survey = sur.ToString(); Patient temp = new Patient(); temp.dt = newdate; temp.ic = newIC; temp.name = newname; temp.gender = newgender; temp.age = newage; temp.race = newrace; temp.survey = survey; temp.vo = defVO.ToString(); temp.fev = defFEV.ToString(); temp.mrc = defMRC.ToString(); temp.bmi = defBMI.ToString(); temp.walk = defWalk.ToString(); temp.vbode = defVBODE.ToString(); if (loadPatients()) { int existing = 0; for (int i = 0; i < patients.Count; i++) {
Final Report
92
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE if (patients[i].ic == newIC && patients[i].dt == newdate) { existing++; } } if (existing == 0) { patients.Add(temp); if (storePatients(patients)) success = true; } } } catch { } return success; } }
struct Patient { public String public String public String public String public String public String public String public String public String public String public String public String public String
dt; ic; name; gender; age; race; survey; vo; fev; mrc; bmi; walk; vbode;
public Patient(String _dt, String _ic, String _name, String _gender, String _age, String _race, String _survey, String _vo, String _fev, String _mrc, String _bmi, String _walk, String _vbode) { dt = _dt; ic = _ic; name = _name; gender = _gender; age = _age; race = _race; survey = _survey; vo = _vo; fev = _fev; mrc = _mrc; bmi = _bmi; walk = _walk; vbode = _vbode; }
Final Report
93
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE } }
Doctor.cs
using using using using using using using using System; System.Collections.Generic; System.ComponentModel; System.Data; System.Drawing; System.Text; System.Windows.Forms; ZedGraph;
namespace REZAHEALTHCLINIC { public partial class Doctor : Form { private List<Patient> patients = new List<Patient>(); private String ic; File data = new File(); List<int> ret = new List<int>(); public Doctor() { InitializeComponent(); } private void button1_Click(object sender, EventArgs e) { dataGridView1.Rows.Clear(); if (textBox1.Text != "") { ic = textBox1.Text; ret.Clear(); patients.Clear(); if (data.loadPatients()) { patients = data.getPatients(); if (patients.Count > 0) { for (int i = 0; i < patients.Count; i++) { if (patients[i].ic == ic) { ret.Add(i); dataGridView1.Rows.Add(new object[] { "Yes", patients[i].dt, patients[i].survey, patients[i].vo,
Final Report
94
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE patients[i].fev, patients[i].mrc, patients[i].bmi, patients[i].walk, patients[i].vbode }); } } if (dataGridView1.Rows.Count == 0) { MessageBox.Show("Patient with IC No. " + ic + " not found"); } if (dataGridView1.Rows.Count > 1) { CreateGraph(zg1, "Survey"); } } else { MessageBox.Show("File loaded but no patient records found"); } } else { MessageBox.Show("Unable to load from the data file. Please check if the file exists and contains correct information"); } } else { MessageBox.Show("Please enter the patient IC No. to search"); } } private void CreateGraph(ZedGraphControl zgc, String type) { GraphPane myPane = zgc.GraphPane; myPane.CurveList.Clear(); PointPairList list = new PointPairList(); int i = 0; if (type == "Survey") { // Set the titles and axis labels myPane.Title.Text = ic + " : Survey Data/Date Graph"; myPane.XAxis.Title.Text = "Date"; myPane.YAxis.Title.Text = "Survey Data"; DateTime celldate; Double gavg; Double gdate; for (i = 0; i < dataGridView1.Rows.Count; i++) {
Final Report
95
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE if (dataGridView1.Rows[i].Cells["Sketch"].Value.Equals("Yes")) { celldate = DateTime.Parse(dataGridView1.Rows[i].Cells["Date"].Value.ToString()); gdate = (double)new XDate(celldate.Year, celldate.Month, celldate.Day); gavg = Double.Parse(dataGridView1.Rows[i].Cells["Survey"].Value.ToString()); list.Add(gdate, gavg); } } } else if (type == "VO") { // Set the titles and axis labels myPane.Title.Text = ic + " : VO2 Max/Date Graph"; myPane.XAxis.Title.Text = "Date"; myPane.YAxis.Title.Text = "VO2 Max Value"; DateTime celldate; Double gavg; Double gdate; for (i = 0; i < dataGridView1.Rows.Count; i++) { if (dataGridView1.Rows[i].Cells["Sketch"].Value.Equals("Yes")) { celldate = DateTime.Parse(dataGridView1.Rows[i].Cells["Date"].Value.ToString()); gdate = (double)new XDate(celldate.Year, celldate.Month, celldate.Day); gavg = Double.Parse(dataGridView1.Rows[i].Cells["VO"].Value.ToString()); list.Add(gdate, gavg); } } } else if (type == "FEV") { // Set the titles and axis labels myPane.Title.Text = ic + " : FEV/Date Graph"; myPane.XAxis.Title.Text = "Date"; myPane.YAxis.Title.Text = "FEV Value (% Predicted)"; DateTime celldate; Double gavg; Double gdate; for (i = 0; i < dataGridView1.Rows.Count; i++) { if (dataGridView1.Rows[i].Cells["Sketch"].Value.Equals("Yes"))
Final Report
96
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE { celldate = DateTime.Parse(dataGridView1.Rows[i].Cells["Date"].Value.ToString()); gdate = (double)new XDate(celldate.Year, celldate.Month, celldate.Day); gavg = Double.Parse(dataGridView1.Rows[i].Cells["FEV"].Value.ToString()); list.Add(gdate, gavg); } } } else if (type == "MRC") { // Set the titles and axis labels myPane.Title.Text = ic + " : MMRC Value/Date Graph"; myPane.XAxis.Title.Text = "Date"; myPane.YAxis.Title.Text = "MMRC Dyspnoea Scale Value"; DateTime celldate; Double gavg; Double gdate; for (i = 0; i < dataGridView1.Rows.Count; i++) { if (dataGridView1.Rows[i].Cells["Sketch"].Value.Equals("Yes")) { celldate = DateTime.Parse(dataGridView1.Rows[i].Cells["Date"].Value.ToString()); gdate = (double)new XDate(celldate.Year, celldate.Month, celldate.Day); gavg = Double.Parse(dataGridView1.Rows[i].Cells["MRC"].Value.ToString()); list.Add(gdate, gavg); } } } else if (type == "BMI") { // Set the titles and axis labels myPane.Title.Text = ic + " : BMI/Date Graph"; myPane.XAxis.Title.Text = "Date"; myPane.YAxis.Title.Text = "BMI Value"; DateTime celldate; Double gavg; Double gdate; for (i = 0; i < dataGridView1.Rows.Count; i++) { if (dataGridView1.Rows[i].Cells["Sketch"].Value.Equals("Yes")) {
Final Report
97
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE celldate = DateTime.Parse(dataGridView1.Rows[i].Cells["Date"].Value.ToString()); gdate = (double)new XDate(celldate.Year, celldate.Month, celldate.Day); gavg = Double.Parse(dataGridView1.Rows[i].Cells["BMI"].Value.ToString()); list.Add(gdate, gavg); } } } else if (type == "Walk") { // Set the titles and axis labels myPane.Title.Text = ic + " : Walk Test Value/Date Graph"; myPane.XAxis.Title.Text = "Date"; myPane.YAxis.Title.Text = "6-min Walk Test Value"; DateTime celldate; Double gavg; Double gdate; for (i = 0; i < dataGridView1.Rows.Count; i++) { if (dataGridView1.Rows[i].Cells["Sketch"].Value.Equals("Yes")) { celldate = DateTime.Parse(dataGridView1.Rows[i].Cells["Date"].Value.ToString()); gdate = (double)new XDate(celldate.Year, celldate.Month, celldate.Day); gavg = Double.Parse(dataGridView1.Rows[i].Cells["Walk"].Value.ToString()); list.Add(gdate, gavg); } } } else if (type == "VBODE") { // Set the titles and axis labels myPane.Title.Text = ic + " : VBODE Index/Date Graph"; myPane.XAxis.Title.Text = "Date"; myPane.YAxis.Title.Text = "VBODE Index"; DateTime celldate; Double gavg; Double gdate; for (i = 0; i < dataGridView1.Rows.Count; i++) { if (dataGridView1.Rows[i].Cells["Sketch"].Value.Equals("Yes")) { celldate = DateTime.Parse(dataGridView1.Rows[i].Cells["Date"].Value.ToString());
Final Report
98
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE gdate = (double)new XDate(celldate.Year, celldate.Month, celldate.Day); gavg = Double.Parse(dataGridView1.Rows[i].Cells["VBODE"].Value.ToString()); list.Add(gdate, gavg); } // Generate a blue curve with circle symbols, and "My Curve 2" in the legend LineItem myCurve = myPane.AddCurve("My Curve", list, Color.Blue, SymbolType.Circle); // Fill the area under the curve with a white-red gradient at 45 degrees myCurve.Line.Fill = new Fill(Color.White, Color.Red, 45F); // Make the symbols opaque by filling them with white myCurve.Symbol.Fill = new Fill(Color.White); // Fill the axis background with a color gradient myPane.Chart.Fill = new Fill(Color.White, Color.LightGoldenrodYellow, 45F); // Fill the pane background with a color gradient myPane.Fill = new Fill(Color.White, Color.FromArgb(220, 220, 255), 45F); //set axis myPane.XAxis.Type = AxisType.Date; myPane.XAxis.Scale.Format = "dd-MMM-yy"; //myPane.YAxis.Scale.MaxAuto = true; // Calculate the Axis Scale Ranges zgc.AxisChange(); zgc.Refresh(); } private int getChecks() { int checks = 0; for (int i = 0; i < dataGridView1.Rows.Count; i++) { if (dataGridView1.Rows[i].Cells["Sketch"].Value.Equals ("Yes")) { checks++; } } if (checks < 2) { MessageBox.Show("Select at least 2 entries to sketch a graph"); } return checks; } private void btnSurvey_Click(object sender, EventArgs e) {
Final Report
99
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE if (getChecks() >= 2) CreateGraph(zg1, "Survey");
private void btnVO_Click(object sender, EventArgs e) { if (getChecks() >= 2) CreateGraph(zg1, "VO"); } private void btnFEV_Click(object sender, EventArgs e) { if (getChecks() >= 2) CreateGraph(zg1, "FEV"); } private void btnMRC_Click(object sender, EventArgs e) { if (getChecks() >= 2) CreateGraph(zg1, "MRC"); } private void btnBMI_Click(object sender, EventArgs e) { if (getChecks() >= 2) CreateGraph(zg1, "BMI"); } private void btnWalk_Click(object sender, EventArgs e) { if (getChecks() >= 2) CreateGraph(zg1, "Walk"); } private void btnVbode_Click(object sender, EventArgs e) { if (getChecks() >= 2) CreateGraph(zg1, "VBODE"); } private void btnSave_Click(object sender, EventArgs e) { int val; Patient temp; dataGridView1.EndEdit(); if (dataGridView1.Rows.Count == ret.Count) { for (int i = 0; i < ret.Count; i++) { val = ret[i]; temp = patients[val]; temp.vo = dataGridView1.Rows[i].Cells["VO"].Value.ToString();
Final Report
100
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE temp.fev = dataGridView1.Rows[i].Cells["FEV"].Value.ToString(); temp.mrc = dataGridView1.Rows[i].Cells["MRC"].Value.ToString(); temp.bmi = dataGridView1.Rows[i].Cells["BMI"].Value.ToString(); temp.walk = dataGridView1.Rows[i].Cells["Walk"].Value.ToString(); patients[val] = temp; } if (data.storePatients(patients)) { MessageBox.Show("Successfully saved !"); CreateGraph(zg1, "Survey"); } else { MessageBox.Show("Could not save to file. Please check if file exists and is writable!"); } } } private void textBox1_TextChanged(object sender, EventArgs e) { } private void dataGridView1_CellContentClick(object sender, DataGridViewCellEventArgs e) { } } }
Form1.cs using using using using using using using System; System.Collections.Generic; System.ComponentModel; System.Data; System.Drawing; System.Text; System.Windows.Forms;
namespace REZAHEALTHCLINIC
Final Report
101
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE { public partial class Form1 : Form { public Form1() { InitializeComponent(); } private void btnSurvey_Click(object sender, EventArgs e) { if (txtIC.Text.Length > 0 && txtIC.Text.Length <= 12) { Survey sur = new Survey(); sur.ic = txtIC.Text; sur.FormClosed += new FormClosedEventHandler(MakeVisibleAgain); sur.Show(); sur.Activate(); this.Visible = false; } else { MessageBox.Show("Enter a correct IC number"); } } private void MakeVisibleAgain(object sender, FormClosedEventArgs e) { this.Visible = true; this.txtIC.Text = ""; this.txtPassword.Text = ""; this.txtStaffPassword.Text = ""; } private void btnRecords_Click(object sender, EventArgs e) { if (txtPassword.Text == "12345") { Doctor doc = new Doctor(); doc.FormClosed += new FormClosedEventHandler(MakeVisibleAgain); doc.Show(); doc.Activate(); this.Visible = false; } else { MessageBox.Show("Please enter a valid password"); } } private void btnAdd_Click(object sender, EventArgs e) { if (txtStaffPassword.Text == "12345")
Final Report
102
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE { Staff stf = new Staff(); stf.FormClosed += new FormClosedEventHandler(MakeVisibleAgain); stf.Show(); stf.Activate(); this.Visible = false; } else { MessageBox.Show("Please enter a valid staff password"); } } private void label4_Click(object sender, EventArgs e) { } private void Form1_Load(object sender, EventArgs e) { }
Staff.cs using System; using System.Collections.Generic; using System.ComponentModel; using System.Data; using System.Drawing; using System.Text; using System.Windows.Forms; namespace REZAHEALTHCLINIC { public partial class Staff : Form { private List<Patient> patients = new List<Patient>(); private String ic; File data = new File(); public Staff() { InitializeComponent(); }
Final Report
103
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE private void Staff_Load(object sender, EventArgs e) { txtDate.Text = DateTime.Now.ToShortDateString(); dispBar(getTotal()); } private void updateBar() { dispBar(getTotal()); } private int getTotal() { int total = 0; if (rad12.Checked == true) total += 1; else if (rad13.Checked == true) total += 2; else if (rad14.Checked == true) total += 3; if (rad22.Checked == true) total += 1; else if (rad23.Checked == true) total += 2; else if (rad24.Checked == true) total += 3; if (rad32.Checked == true) total += 1; else if (rad33.Checked == true) total += 2; else if (rad34.Checked == true) total += 3; if (rad42.Checked == true) total += 1; if (rad52.Checked == true) total += 1; else if (rad53.Checked == true) total += 2; else if (rad54.Checked == true) total += 3; return total; } private void dispBar(int val) { try { Label lbl;
Final Report
104
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE Control[] all; int i = 0, j = 0; for (i = 1; i <= 13; i++) { all = this.Controls.Find("lblcol" + i.ToString(), for (j = 0; j < all.Length; j++) { lbl = all[j] as Label; lbl.Visible = false; }
true);
for (i = 1; i <= val; i++) { all = this.Controls.Find("lblcol" + i.ToString(), true); for (j = 0; j < all.Length; j++) { lbl = all[j] as Label; lbl.Visible = true; } } } catch { }
private void button2_Click(object sender, EventArgs e) { if (txtDate.Text != null && txtID.Text != null) { int ret = -1; ic = txtID.Text; patients.Clear(); if (data.loadPatients()) { patients = data.getPatients(); if (patients.Count > 0) { for (int i = 0; i < patients.Count; i++) { if (patients[i].ic == ic && patients[i].dt == txtDate.Text) { ret = i; } } if (ret == -1) { MessageBox.Show("Survey entry matching specified date and ic not found"); }
Final Report
105
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE else {
Patient pat = new Patient(patients[ret].dt, patients[ret].ic, patients[ret].name, patients[ret].gender, patients[ret].age, patients[ret].race, patients[ret].survey, patients[ret].vo, patients[ret].fev, patients[ret].mrc, patients[ret].bmi, patients[ret].walk, getTotal().ToString()); patients[ret] = pat; if (data.storePatients(patients)) { MessageBox.Show("VBODE Value Saved !"); } else { MessageBox.Show("VBODE value could not be saved. Please check file"); } } } else { MessageBox.Show("Patient data loaded from file, but no records found !"); } } else { MessageBox.Show("Unable to load patient data. Please check file."); } } else { MessageBox.Show("Patient IC and Test Date are required"); } } private void rad11_CheckedChanged(object sender, EventArgs e) { if (rad11.Checked == true) updateBar(); } private void rad12_CheckedChanged(object sender, EventArgs e) { if (rad12.Checked == true) updateBar(); } private void rad13_CheckedChanged(object sender, EventArgs e) { if (rad13.Checked == true) updateBar();
Final Report
106
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE } private void rad14_CheckedChanged(object sender, EventArgs e) { if (rad14.Checked == true) updateBar(); } private void rad21_CheckedChanged(object sender, EventArgs e) { if (rad21.Checked == true) updateBar(); } private void rad22_CheckedChanged(object sender, EventArgs e) { if (rad22.Checked == true) updateBar(); } private void rad23_CheckedChanged(object sender, EventArgs e) { if (rad23.Checked == true) updateBar(); } private void rad24_CheckedChanged(object sender, EventArgs e) { if (rad24.Checked == true) updateBar(); } private void rad31_CheckedChanged(object sender, EventArgs e) { if (rad31.Checked == true) updateBar(); } private void rad32_CheckedChanged(object sender, EventArgs e) { if (rad32.Checked == true) updateBar(); } private void rad33_CheckedChanged(object sender, EventArgs e) { if (rad33.Checked == true) updateBar(); } private void rad34_CheckedChanged(object sender, EventArgs e) { if (rad34.Checked == true) updateBar();
Final Report
107
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE } private void rad41_CheckedChanged(object sender, EventArgs e) { if (rad41.Checked == true) updateBar(); } private void rad42_CheckedChanged(object sender, EventArgs e) { if (rad42.Checked == true) updateBar(); } private void rad51_CheckedChanged(object sender, EventArgs e) { if (rad51.Checked == true) updateBar(); } private void rad52_CheckedChanged(object sender, EventArgs e) { if (rad52.Checked == true) updateBar(); } private void rad53_CheckedChanged(object sender, EventArgs e) { if (rad53.Checked == true) updateBar(); } private void rad54_CheckedChanged(object sender, EventArgs e) { if (rad54.Checked == true) updateBar(); } private void lblcol3_Click(object sender, EventArgs e) { } private void label40_Click(object sender, EventArgs e) { } private void tableLayoutPanel1_Paint(object sender, PaintEventArgs e) { } }
Final Report
108
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE }
Survey.cs using using using using using using using System; System.Collections.Generic; System.ComponentModel; System.Data; System.Drawing; System.Text; System.Windows.Forms;
namespace REZAHEALTHCLINIC { public partial class Survey : Form { public String ic; public Survey() { InitializeComponent(); } private void Survey_Load(object sender, EventArgs e) { txtIC.Text = ic; } private void clearform() { txtName.Text = ""; txtAge.Text = ""; txtRace.Text = ""; radSmokerNo.Checked = true; radFSmokerNo.Checked = true; radHistoryNo.Checked = true; radSHNo.Checked = true; radExpNo.Checked = true; radCoughNo.Checked = true; radSputumNo.Checked = true; radDysNo.Checked = true; radResNo.Checked = true; } private void btnSave_Click(object sender, EventArgs e) { if (txtName.Text != null && txtAge.Text != null && cboGender.Text != null && txtRace.Text != null) {
Final Report
109
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE float total = 0; //q1 if (radSmokerYes.Checked == true) total += 5; else total += 1; //q2 if (radFSmokerYes.Checked == true) total += 5; else total += 1; //q3 if (radHistoryYes.Checked == true) total += 5; else total += 1; //q4 if (radSHYes.Checked == true) total += 5; else total += 1; //q5 if (radExpYes.Checked == true) total += 5; else total += 1; //q6 if (radCoughYes.Checked == true) total += 5; else total += 1; //q7 if (radSputumYes.Checked == true) total += 5; else total += 1; //q8 if (radDysYes.Checked == true) total += 5; else total += 1; //q9 if (radResYes.Checked == true) total += 5; else
Final Report
110
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE total += 1; File fl = new File(); if (fl.saveSurvey(txtIC.Text, txtName.Text, txtAge.Text, cboGender.Text, txtRace.Text, total)) { MessageBox.Show("Information saved with success"); clearform(); } else { MessageBox.Show("Information could not be saved. Duplicate surveys found/file could not be written to"); } } else MessageBox.Show("Please check if you have left any field blank in the patient details input"); } private void button1_Click(object sender, EventArgs e) { clearform(); } private void label6_Click(object sender, EventArgs e) { }
} }
Final Report
111
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Appendix D: Lab Data of Cardiopulmonary Exercise Test on a Bicycle Ergometer [40]
Final Report
112
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
113
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
114
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
115
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
116
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
117
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
118
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
119
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
120
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
121
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
122
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
123
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
124
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
125
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
126
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
127
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
128
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
129
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
130
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
131
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
132
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
133
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
134
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
135
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
136
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
137
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
138
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
139
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
140
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
141
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
142
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
143
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
144
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
145
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
146
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Final Report
147
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Appendix E: Inspiration and Expiration
The amount of air left in the lungs after a tidal breath out. Functional residual = ERV The amount of air that stays in the lungs during normal capacity (FRC) + RV breathing. Inspiratory capacity = Vt + The maximal volume that can be inspired following a (IC) IRV normal expiration.
Final Report
148
NON-INVASIVE ASSESSMENT OF PULMONARY DISEASE
Appendix F: Spirometry Staging
COPD can be classified due to its severity. Below in table 1 lists Stage 0 to stage IV of COPD. Table 1:
Final Report
149
You might also like
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (890)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Medical Surgical Nursing Module 11Document26 pagesMedical Surgical Nursing Module 11weissNo ratings yet
- The Use of Bubble CPAP in Premature InfantsDocument7 pagesThe Use of Bubble CPAP in Premature InfantsRyan Rahman OesmanNo ratings yet
- Form 4 Biology Chapter 7 RespirationDocument33 pagesForm 4 Biology Chapter 7 RespirationPau Siew LingNo ratings yet
- Parts & Function of Respiratory SystemDocument4 pagesParts & Function of Respiratory SystemLucille Ballares83% (6)
- Respiratory Physiology BIII - BIV J Lee 17.3.10Document43 pagesRespiratory Physiology BIII - BIV J Lee 17.3.10muraruandreiNo ratings yet
- Modes of VentilatorDocument10 pagesModes of VentilatorSatya Biomed100% (1)
- NCM 112 Lecture Notes (Respiratory System and Its Diseases)Document9 pagesNCM 112 Lecture Notes (Respiratory System and Its Diseases)Kyle FernandezNo ratings yet
- 1-Mechanism and Regulation of Respiration ModifiedDocument10 pages1-Mechanism and Regulation of Respiration Modifiedخالد القرشيNo ratings yet
- QuestionsDocument5 pagesQuestionsRiyad AliNo ratings yet
- Module 12 - Health Conditions RajDocument6 pagesModule 12 - Health Conditions RajRajesh MakwanaNo ratings yet
- Securing Airways and Suctioning Endotracheal TubesDocument28 pagesSecuring Airways and Suctioning Endotracheal TubesJohn Mark ParacadNo ratings yet
- Lungs - Facts, Function and Diseases - Live ScienceDocument12 pagesLungs - Facts, Function and Diseases - Live ScienceImtiax LaghariNo ratings yet
- Airway Management 1Document17 pagesAirway Management 1kamel6No ratings yet
- Lower Airways ConditionsDocument6 pagesLower Airways ConditionsMabesNo ratings yet
- Pulmonary Function Testing: David A. Kaminsky Charles G. Irvin EditorsDocument322 pagesPulmonary Function Testing: David A. Kaminsky Charles G. Irvin EditorsJulie Anne Mariflor AtongNo ratings yet
- Oxygen, A Clear, Odorless Gas That Constitutes Approximately 21% of The Air We Breathe, IsDocument5 pagesOxygen, A Clear, Odorless Gas That Constitutes Approximately 21% of The Air We Breathe, IsJean ZulykaNo ratings yet
- 07.04.06 Non-Rebreathing MaskDocument3 pages07.04.06 Non-Rebreathing MaskNena_mileyNo ratings yet
- UworldDocument721 pagesUworldIrish Eunice FelixNo ratings yet
- Adminstering Oxygen To A PatientDocument2 pagesAdminstering Oxygen To A PatientJake Yvan DizonNo ratings yet
- Newport e 360 VentilatorDocument6 pagesNewport e 360 VentilatorNeil AcostaNo ratings yet
- Respiratory Procedures: Tracheal Intubation PreparationDocument46 pagesRespiratory Procedures: Tracheal Intubation PreparationRhea Andrea UyNo ratings yet
- The Six Minute Walk TestDocument4 pagesThe Six Minute Walk Testhm3398No ratings yet
- 118 RLE Mechanical Ventilation PDFDocument5 pages118 RLE Mechanical Ventilation PDFclaire yowsNo ratings yet
- Respiratory Notes 1.1Document7 pagesRespiratory Notes 1.1diceNo ratings yet
- Equipment Catalogue - IndonesiaDocument100 pagesEquipment Catalogue - IndonesiarayNo ratings yet
- Nur 400 Clinical ProjectDocument25 pagesNur 400 Clinical Projectapi-308919608No ratings yet
- Respiration in Plants: The Process of Cellular RespirationDocument3 pagesRespiration in Plants: The Process of Cellular RespirationSpandan DasNo ratings yet
- Foreign Body Aspiration.Document40 pagesForeign Body Aspiration.Maria DodonNo ratings yet
- Analysis of COD, BOD and DO Levels in Wastewater TreatmentDocument10 pagesAnalysis of COD, BOD and DO Levels in Wastewater TreatmentSeptifa DiteNo ratings yet
- Cell 3dDocument8 pagesCell 3dStefania DavidNo ratings yet