Professional Documents
Culture Documents
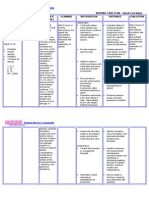
Impaired Skin Integrity
Uploaded by
Macmac ReyesOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Impaired Skin Integrity
Uploaded by
Macmac ReyesCopyright:
Available Formats
Impaired Skin Integrity
Published on Saturday March 10th , 2007
Impaired Skin Integrity
(_)Actual (_) Potential
Related To:
[Check those that apply]
(_) Burns of_______________________ (_) Decreased sensation (_) Immobility (_) Malnutrition (_) Pressure ulcer (_) Puritus (_) Stoma problems (_) Other:_____________________________ ____________________________________ ____________________________________
As evidenced by:
[Check those that apply]
Major: (_) Disruption of epidermal and dermal tissue. (Must be present) Minor: (_) Denuded skin. (May be present) (_) Erythema. (_)Lesions.
Other:
Date & Sign.
Plan and Outcome
[Check those that apply]
Target Date:
Nursing Interventions
[Check those that apply]
Date Achieved:
The patient will: (_)Maintain or develop clean and intact skin. (_) Other:
(_) Inspect and chart skin integrity q_____hrs. (_) Do wound care/dressing change as ordered. Describe:__________ ________________________ ________________________ ________________________ ________________________ ________________________ (_) Provide measures to decrease
pressure/irritation to skin: y y y y
fleece pad egg crate mattress keep skin clean and dry other:
(_) Turn and reposition q____hrs. (_) Up in chair for ___ minutes q____. (_) Gently massage bony prominences and pressure points with lotion q____. (_) Maintain adequate nutrition and hydration. (_) Change incontinent pad ASAP after voiding or defecation. (_) Expose skin to air if indicated. (_) Initiate health teaching and referrals as indicated. List:___________ ________________________ ________________________ (_) Keep nails short. (_) Mittens to decrease skin breakdown from scratching. (These are considered a restraint in some facilities. Get an order first.) (_) Change ostomy appliance prn when leaking. (_) Other:________________ ________________________ ________________________ ________________________
__________________________ Patient/Significant other signature
__________________________ RN signature
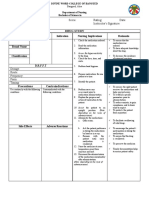
Impaired Physical Mobility
Published on Saturday March 10th , 2007
Impaired Physical Mobility
(_)Actual (_) Potential
Related To:
[Check those that apply]
(_) Amputation (_) Cardiovascular (_) External devices (_) Impaired balance (_) Limited ROM (_) Musculoskeletal impairment
(_) Neuromuscular impairment (_) Pain (_) Surgical procedure (_) Trauma (_) Other:_____________________________ ____________________________________ ____________________________________
As evidenced by:
[Check those that apply]
Major: (Must be present)
(_) Inability to move purposefully within the environment, including bed mobility, transfers, and ambulation.
Minor: (_) Range of motion limitations. (May be present) (_) Limited muscle strength or control. (_) Impaired coordination.
Date & Sign.
Plan and Outcome
[Check those that apply]
Target Date:
Nursing Interventions
[Check those that apply]
Date Achieved:
The patient will: (_) Maintain or increase strength and endurance of upper/lower limbs A.E.B.:
(_) Assess symmetry, strength, and degree of mobility. (_) Passive/active ROM exercises as ordered by physician q_____ to:__________(body part). (_) Position in proper alignment and
(_) Will not develop complications of
immobility. (_) Demonstrate use of adaptive device(s) to increase mobility. Device:
resposition q____ hrs. (_) Encourage isometric exercises when indicated. (_) Up in chair _____ minutes q____. (_) Check/teach proper use/function of adaptive equipment. (_) Provide progressive mobilization. (_) Referral: y y y PT OT other:
(_) Other:
(_) Other:________________ ________________________ ________________________ ________________________
__________________________ Patient/Significant other signature
__________________________ RN signature
NCP Nursing Care Plans for Burns Injury. A major burn is a devastating injury, requiring painful treatment and a long period of rehabilitation. Burns have a catastrophic effect on people in terms of human life, suffering, disability, and financial loss. Burns can be fatal, permanently disfiguring, and incapacitating, both emotionally and physically. Infections are a major cause of morbidity and mortality in seriously burned patients. The skin injury from burns has six different mechanisms of injury: scalds, contact burns, fire, chemical, electrical, and radiation. Causes for Burns Injury Thermal burns, the most common type, result from preventable accidents occur because of fires from motor vehicle crashes, accidents in residences, and arson or electrical malfunctions. Chemical burns result from the contact, ingestion, inhalation, or injection of acids, alkali, or vesicants. Electrical burns commonly occur after contact with faulty electrical wiring or high-
voltage power lines. Friction, or abrasion, burns happen when the skin is rubbed harshly against a coarse surface. Sunburn follows excessive exposure to sunlight and improper use of tanning lights. Complications for Burns Injury Leading causes of death in burn patients are respiratory complications and sepsis. Other possible complications include:
y y y y
Hypovolemic shock Anemia Malnutrition Multisystem organ dysfunction.
Nursing Assessment Nursing Care Plans for Burns Injury Patient history. Obtain a complete description of the burn injury, including the time, the situation, the burning agent, and the actions of witnesses. The time of injury is extremely important since any delay in treatment may result in a minor or moderate burn becoming a major injury. Elicit specific information about the location of the accident, since closed-space injuries are related to smoke inhalation. If abuse is suspected, obtain a more in-depth history from a variety of people who are involved with the child. The injury may be suspect if there is a delay in seeking health care, if there are burns that are not consistent with the story, or if there are bruises at different stages of healing. Note whether the description of the injury changes or differs among family or household members. Basic assessment of airway, breathing, and circulation (ABCs) takes first priority. Once the ABCs are stabilized, perform a complete examination of the burn wound to determine burn severity. First, determine the depth of tissue damage. A partial-thickness burn damages the epidermis and part of the dermis; a full-thickness burn also affects the subcutaneous tissue. The more traditional method is to gauge burns by degree. Most burns include a combination of degrees and thicknesses
RULE OF NINES The rule of nines is a practical technique used to estimate the extent of TBSA total body surface area involved in a burn. The technique divides the major anatomic areas of the body into percentages: in adults, 9% of the TBSA is the head and neck, 9% is each upper extremity, 18% is each anterior and posterior portions of the trunk, 18% is each lower extremity, and 1% is the perineum and genitalia. Clinicians use the patients palm area to represent approximately 1% of TBSA. Serial assessments of wound healing determine the patients response to treatment. Ongoing monitoring throughout the acute and rehabilitative phases is essential for the burn patient. Fluid balance, daily weights, vital signs, and intake and outpu Nursing diagnosis Nursing Care Plans for Burns Injury
y y y y y y y y y y y
Impaired gas exchange Ineffective airway clearance Acute pain Decreased cardiac output Deficient fluid volume Ineffective tissue perfusion: Peripheral Hypothermia Impaired skin integrity Impaired physical mobility Disturbed body image Risk for infection
Nursing outcomes Nursing Care Plans for Burns Injury Nursing Key outcomes Nursing Care Plans for Burns Injury, Patient will:
y y y y y y y y y y y y y y y
Ventilation will remain adequate. Airway will remain patent Achieve pain relief with analgesia or other measures. Maintain adequate cardiac output. Fluid volume will remain within the acceptable range. Exhibit signs of adequate peripheral perfusion Communicate understanding of special dietary needs. Maintain normal body temperature. Wounds and incisions will appear clean, pink, and free of purulent drainage. Attain the highest degree of mobility possible within the confines of the injury. Express positive feelings about self. Express that he feels less anxious. Demonstrate effective coping mechanisms. Remain free from signs and symptoms of infection. Express his feelings and fears about the traumatic event.
Nursing interventions Nursing Care Plans for Burns Injury
y y
y y
Provide immediate, aggressive burn treatment to increase the patient's chance for survival. Airway management; Anxiety reduction; Oxygen therapy; Airway suctioning; Airway insertion and stabilization; Cough enhancement; Mechanical ventilation; Positioning; Respiratory monitoring Airway Management Facilitation of patency of air passages Pain Management: Alleviation of pain or a reduction in pain to a level of comfort that is acceptable to the patient. Analgesic Administration Use of pharmacologic agents to reduce or eliminate pain. Environmental Management Manipulation of the patients surroundings for promotion of optimal comfort Hemodynamic Regulation Optimization of heart rate, preload, afterload, and contractility. Circulatory Care Mechanical Assist Devices: Temporary support of the circulation through the use of mechanical devices or pumps Fluid Management Promotion of fluid balance and prevention of complications resulting from abnormal or undesired fluid levels. Hypovolemia Management Reduction in extracellular and/or intracellular fluid volume. Shock Management: Volume: Promotion of adequate tissue perfusion for a patient with severely compromised intravascular volume. Fluid/Electrolyte Management Promotion of fluid/electrolyte balance and prevention of complications resulting from abnormal or undesired fluid/serum electrolyte levels. Circulatory Care Arterial/Venous Insufficiency: Promotion of arterial/venous circulation Hypothermia Treatment Rewarming and surveillance of a patient whose core body temperature is below 35C. Temperature Regulation: Attaining and/or maintaining body temperature within a normal range
y y
Wound Care Prevention of wound complications and promotion of wound healing Exercise Therapy Use of active or passive body movement to maintain or restore flexibility; use of specific activity or exercise protocols to enhance or restore controlled body movement Body Image Enhancement improving a patients conscious and unconscious perceptions and attitudes toward his/her body. Self Esteem Enhancement Assisting a patient to increase his/her personal judgment of self worth. Infection Protection Prevention and early detection of infection in a patient at risk. Infection Control Minimizing the acquisition and transmission of infectious agents. Surveillance: Purposeful and ongoing acquisition, interpretation, and synthesis of patient data for clinical decision making
You might also like
- Discharge Planning BurnsDocument12 pagesDischarge Planning BurnsChaa Maii100% (1)
- HIV Case Study: Priority Nursing Diagnoses and CareDocument3 pagesHIV Case Study: Priority Nursing Diagnoses and CarechoobiNo ratings yet
- NCM 100 Case AnaDocument3 pagesNCM 100 Case AnaCharissa Magistrado De LeonNo ratings yet
- Primary entry point into healthcare systemDocument3 pagesPrimary entry point into healthcare systemDeen Philip OlegarioNo ratings yet
- NCP Total Hip ReplacementDocument11 pagesNCP Total Hip ReplacementDoneva Lyn MedinaNo ratings yet
- Endocrine System Nursing ReviewDocument7 pagesEndocrine System Nursing ReviewMeiJoyFlamianoIINo ratings yet
- Cutask 5Document2 pagesCutask 5Nicole RagustaNo ratings yet
- Diet: Bath: ActivityDocument2 pagesDiet: Bath: ActivityKristian Karl Bautista Kiw-isNo ratings yet
- Case 1Document9 pagesCase 1Joselyn M. LachicaNo ratings yet
- Applying a Tourniquet for Bleeding EmergenciesDocument3 pagesApplying a Tourniquet for Bleeding EmergenciesTom-tom LunaNo ratings yet
- CVD Pt Comm ImproveDocument12 pagesCVD Pt Comm ImproveRaphael FranciscoNo ratings yet
- NCPDocument9 pagesNCPHendy Hency YunusNo ratings yet
- Lack of Knowledge On Diabetes Management or Blood Glucose ManagementDocument2 pagesLack of Knowledge On Diabetes Management or Blood Glucose ManagementDanica Kate GalleonNo ratings yet
- QuestionDocument6 pagesQuestiontravelbeeNo ratings yet
- Nursing Care Plan: Sweating Temperature Rigors Nausea Vomiting Diarrhoea Lethargy MalaiseDocument1 pageNursing Care Plan: Sweating Temperature Rigors Nausea Vomiting Diarrhoea Lethargy Malaise06eltianNo ratings yet
- Patient with Cellulitis Right Arm ReportDocument1 pagePatient with Cellulitis Right Arm ReportJhevilin RMNo ratings yet
- Situation 1Document18 pagesSituation 1Maler De VeraNo ratings yet
- Subjective Cues:: Nursing Care ProcessDocument8 pagesSubjective Cues:: Nursing Care ProcessBianca Marithè RejanoNo ratings yet
- Nursing Care Plan: Subjective: During 8 Hours Nursing Management: (5) After 8 HoursDocument4 pagesNursing Care Plan: Subjective: During 8 Hours Nursing Management: (5) After 8 HoursRawan KhateebNo ratings yet
- NCP Intra FinalDocument7 pagesNCP Intra FinalRoxanne Ganayo ClaverNo ratings yet
- Drug StudyDocument17 pagesDrug StudyKenneth ManalangNo ratings yet
- Subjective Data: Long Term Goal: Diagnostic:: "I Was Trying To Vomit in The Emergency Department."Document5 pagesSubjective Data: Long Term Goal: Diagnostic:: "I Was Trying To Vomit in The Emergency Department."Erle Gray CadangenNo ratings yet
- Gordons TypologyDocument3 pagesGordons TypologyMaxinne Allyssa Cancino RoseñoNo ratings yet
- Arellano U College of Nursing Case Analysis: Med-Surg Nursing 1Document1 pageArellano U College of Nursing Case Analysis: Med-Surg Nursing 1Charissa Magistrado De LeonNo ratings yet
- Hypertension NclexDocument5 pagesHypertension Nclexハニファ バランギNo ratings yet
- Week 1 - Ms1 Course Task Cu1Document1 pageWeek 1 - Ms1 Course Task Cu1jaira magbanuaNo ratings yet
- Board Questions 2009Document16 pagesBoard Questions 2009Erick EspinoNo ratings yet
- Case Study RespiDocument3 pagesCase Study RespiMark Jheran AlvarezNo ratings yet
- NCP PainDocument2 pagesNCP PainApril_Ivy_Raga_3835No ratings yet
- Jenny Anne Pimentel - ReflectionDocument1 pageJenny Anne Pimentel - ReflectionRona Bersamina AsuncionNo ratings yet
- DX Fracture PDFDocument8 pagesDX Fracture PDFSherree HayesNo ratings yet
- Im Case Study 04Document49 pagesIm Case Study 04Shaine BalverdeNo ratings yet
- Answer Key Simulated Pre Board Set 4 NagaDocument11 pagesAnswer Key Simulated Pre Board Set 4 NagaRaymark MoralesNo ratings yet
- Digestive System 2Document32 pagesDigestive System 2Johnmer AvelinoNo ratings yet
- FractureDocument4 pagesFractureRaveen mayiNo ratings yet
- Nursing Care Plan for Spinal Cord InjuryDocument3 pagesNursing Care Plan for Spinal Cord InjuryDan Leo UnicoNo ratings yet
- CetirizineDocument2 pagesCetirizinelintangNo ratings yet
- CHN 2 JournalDocument2 pagesCHN 2 Journalinah krizia lagueNo ratings yet
- COMMUNITY HEALTH NURSING ROLES AND RESPONSIBILITIESDocument40 pagesCOMMUNITY HEALTH NURSING ROLES AND RESPONSIBILITIESBONGNo ratings yet
- Fever: What Is A Fever?Document2 pagesFever: What Is A Fever?Sheikh ZakirNo ratings yet
- NCP For Rapid Shallow BreathingDocument1 pageNCP For Rapid Shallow Breathingbamboo2dNo ratings yet
- Cu 5Document2 pagesCu 5Clareze AbadNo ratings yet
- NCP Impaired Physical MobilityDocument1 pageNCP Impaired Physical MobilityCharmaine SolimanNo ratings yet
- Couretask SampleDocument2 pagesCouretask Sampleej ragoNo ratings yet
- NCPDocument10 pagesNCPCristina L. JaysonNo ratings yet
- Case Study 2Document7 pagesCase Study 2desdav100% (1)
- Meniere's Disease - Case StudyDocument3 pagesMeniere's Disease - Case StudyZORANASNNo ratings yet
- Are You Kidding MeDocument10 pagesAre You Kidding MeChelsea RoseNo ratings yet
- NCP For ChronicPain PDFDocument2 pagesNCP For ChronicPain PDFjay kusainNo ratings yet
- Disturbed Body Image Nursing InterventionsDocument11 pagesDisturbed Body Image Nursing InterventionsNdel LindaNo ratings yet
- NCLEX Practice Exam For Pharmacology - Musculoskeletal Medications - RNpediaDocument8 pagesNCLEX Practice Exam For Pharmacology - Musculoskeletal Medications - RNpediaKristine SingsonNo ratings yet
- InsulinDocument6 pagesInsulinJorelle-Nickolai RodriguezNo ratings yet
- Course Task Week 7 NCMB 312Document6 pagesCourse Task Week 7 NCMB 312Angie BaylonNo ratings yet
- KardexDocument2 pagesKardexKristian Karl Bautista Kiw-isNo ratings yet
- Parenteral Fluid Therapy: Types of Intravenous SolutionDocument18 pagesParenteral Fluid Therapy: Types of Intravenous SolutionKathleen Joy Costales Magtanong100% (1)
- Soapie Charting: Date, Time, and Shift Progress NotesDocument3 pagesSoapie Charting: Date, Time, and Shift Progress NotesBianx Flores DosdosNo ratings yet
- NCP, Ent, Risk For InfectionDocument1 pageNCP, Ent, Risk For InfectionGale DizonNo ratings yet
- The Impact of Pressure Ulcers: Bony Sacrum Coccyx Heels Hips Elbows Knees Ankles CraniumDocument48 pagesThe Impact of Pressure Ulcers: Bony Sacrum Coccyx Heels Hips Elbows Knees Ankles CraniumVanessa Camille DomingoNo ratings yet
- Burn NotesDocument4 pagesBurn NotesRiza Angela BarazanNo ratings yet
- Pressure Ulcers and Wound CareDocument52 pagesPressure Ulcers and Wound CareKarina Mega WNo ratings yet
- Jibachha Veterinary Hospital Kathmandu, BranchDocument8 pagesJibachha Veterinary Hospital Kathmandu, BranchJibachha ShahNo ratings yet
- Cultural Humility Versus Cultural CompetenceDocument15 pagesCultural Humility Versus Cultural CompetenceJosé Luis PsicoterapeutaNo ratings yet
- AIIMS Merit List for DM/MCH/MD Courses July 2022Document15 pagesAIIMS Merit List for DM/MCH/MD Courses July 2022sarath6872No ratings yet
- Haa149Document10 pagesHaa149dadi hartonoNo ratings yet
- 3060directory PDFDocument233 pages3060directory PDFtejasNo ratings yet
- BJSTR MS Id 004577Document8 pagesBJSTR MS Id 004577SartajHussainNo ratings yet
- Indian Pharma Threatened by COVID-19 Shutdowns in ChinaDocument1 pageIndian Pharma Threatened by COVID-19 Shutdowns in ChinaPankaj HatwarNo ratings yet
- 6.1 DRRM-H Step 3 Update - Devt of The Plan - Prevention and Mitigation PlanDocument14 pages6.1 DRRM-H Step 3 Update - Devt of The Plan - Prevention and Mitigation PlanFrab Edar100% (1)
- Drug Study NCP Template 2Document2 pagesDrug Study NCP Template 2Janico Lanz BernalNo ratings yet
- Health Management For Fattening PigsDocument24 pagesHealth Management For Fattening PigsMarwin NavarreteNo ratings yet
- 5e Official Diseases Lists - 03 - 03 - 21 - GM BinderDocument4 pages5e Official Diseases Lists - 03 - 03 - 21 - GM BinderAryssia MendonçaNo ratings yet
- Stage 2 PDHPE Scope and SequenceDocument4 pagesStage 2 PDHPE Scope and SequenceAnthony Dunn100% (1)
- Pre Board XIIDocument4 pagesPre Board XIISamyak OswalNo ratings yet
- 2018.pelvic Inflammatory DiseaseDocument4 pages2018.pelvic Inflammatory DiseaseObgynism 2019No ratings yet
- Irl KH Final Report RMW Rapid Assessment2020 0Document84 pagesIrl KH Final Report RMW Rapid Assessment2020 0Duong TranNo ratings yet
- Health Promotion Stress Management AssignmentDocument10 pagesHealth Promotion Stress Management Assignmentapi-211472021No ratings yet
- FPGEE Blueprint: Area 1 - Basic Biomedical Sciences - 21%Document9 pagesFPGEE Blueprint: Area 1 - Basic Biomedical Sciences - 21%angelflairNo ratings yet
- 3 s2.0 B9781455748013003301 MainDocument120 pages3 s2.0 B9781455748013003301 MainInzamam Ul HaqNo ratings yet
- Purposal Part 2&3Document6 pagesPurposal Part 2&3Mark Vincent Sta. RitaNo ratings yet
- Bacls PDFDocument23 pagesBacls PDFAngelo Domingo0% (1)
- Danone Case PreparationDocument7 pagesDanone Case PreparationXiuNo ratings yet
- Office of The Secretary: Administrative Order (014-ADocument1 pageOffice of The Secretary: Administrative Order (014-ACharlemagne Sabio GalamgamNo ratings yet
- Knowledge Attitudes and Practice of Community PharDocument16 pagesKnowledge Attitudes and Practice of Community Pharfirda amir parumpuNo ratings yet
- The Effect of Long-Term Aspirin Intake On The Outcome of Non-Surgical Periodontal Therapy in Smokers: A Double-Blind, Randomized Pilot StudyDocument8 pagesThe Effect of Long-Term Aspirin Intake On The Outcome of Non-Surgical Periodontal Therapy in Smokers: A Double-Blind, Randomized Pilot StudyOctavian BoaruNo ratings yet
- JNTU Hyderabad: B.Pharmacy Regular/Supplementary Examinations Time Table 2011-2012Document6 pagesJNTU Hyderabad: B.Pharmacy Regular/Supplementary Examinations Time Table 2011-2012MahabubnagarNo ratings yet
- The Ottawa Charter For Health PromotionDocument5 pagesThe Ottawa Charter For Health PromotionANA LILIA CALDERON YELANo ratings yet
- 1.113.medication Administration TimingDocument14 pages1.113.medication Administration TimingSophiaNo ratings yet
- Sleep Disorders in The ElderlyDocument50 pagesSleep Disorders in The ElderlykikimarioNo ratings yet
- 2007 DoH Collaborative Recruitment Solutions in Social Care - Getting and Keeping Your WorkforceDocument49 pages2007 DoH Collaborative Recruitment Solutions in Social Care - Getting and Keeping Your WorkforcecarlselbyNo ratings yet
- Statement of The ProblemDocument13 pagesStatement of The ProblemDaniel LeoNo ratings yet