Professional Documents
Culture Documents
The History and Development of The Fentanyl Series - TH Stanley - J Pain Symptom Manage, Apr 1992, 7 (3), Suppl 1, S3-S7 - PMID 1517629
Uploaded by
muopioidreceptorOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
The History and Development of The Fentanyl Series - TH Stanley - J Pain Symptom Manage, Apr 1992, 7 (3), Suppl 1, S3-S7 - PMID 1517629
Uploaded by
muopioidreceptorCopyright:
Available Formats
Vol. 7No.
3 (Zi~jd) Aprd 1992
Journal of Fain and Symptom Management S3
Theodore H. Stanley,
Departmentofrinesthesio~~, Universi~of Utah School~Medicine, Salt Lake Ci@, i//ah
In the bz.st Rplo akcad.., opioid ana~esics have assumedan important plare in general anesthetk practice in the United St~ti. Part of the reason forthis has been the introductionof thepotent new agonktsf2nkmyJ sufnztani~ and a#.Z.ZtaniL Because of pro6Lzm.r with morphinroxygen anesthesia(incompleieamnesia, occasionalhistamine-related reaction,marked increasesin in&a- and postoperhe rtipiratolydepression), a suitable altematiuewas soughtbut notfound amongtit@ opioids.A breakthrough came in 1960, when fentanyi was synthesize4 lying thefoutuiatio~~ a betterunderstandingof the structure-actin@ for rekzkuships of narcoticana~esics aad stimutatinginteres in deuelopiing compoundsm-th tzen gzzater poteiuy and saj+ margins. Inves@gators interested qtiioid in anesthesiabegan to study jkntanyl in animals and then in humans. Fentany (5e100 t..@@ Jjdh oygen (100%) was waluatedas an amzsthetic in Change in cardiovascular dynamics with patients undergoiq mitral ualveand coronq arterysqq.
induction doses rangingj?om 8 to 30 g/kg consistedof small decreasesin heart rate and arterial blood pressure. All other cardiovascular van*a&ks studti, includiq cardiac output, remainedunchanged, wen with additional doses up to 100 e/kg. It war detemzined thatfepltanyl had use as a nmcotix anesiWic, despite its pokmrialfor cardiovassnrlm deprRFsion stimuiatknz,respiratory and depression,muschzn@iity, and, occasionally,incompleteamxYuGa. Since the introduction offentanyb two other potentsynthetic opioidr have been introducedintoclinical practice-sufmztaniland ay2ntaniL.J Pain Symptom Manage
1992;?:S3-s7. K@ words Opioz&, fmtanyl, sufmtanir! a@ntanii
Although opium derivatives have been used for thousands of years, it was not until the 1970s that morphine and its congeners began to come ofage with their use as components of neurolept and balanced anesthesia and as complete anesthetics in cardiovascular sur.geries.Until that time morphine was employed as a preanesthetic, postanesthesia analgesic, and anesthetic supplement. In the late 19th and early 20th centuries, morphine in combination with scopolamine had heen employed
Addressreprintrequests Theodore Stanley,MD, Departto: ment of Anesthesiology, Universityof TJtah School of Medicine, 50 North Medical Drive, Salt Lake City, TJT 84132.
0 U.S. Cancer Pain Relief Committee, 1992 Published by Elsevier, New York, New York
as an anesthetic, but reports of increased operative morbidity and mortality led to the abandonment of this technique, It was not until the 195Os, in a search for new nonbarbiturate intravenous anesthetic agents, that researchers again turned their attention to opioids. In 1953, Paul Janssen became interested in developing the most potent narcotic analgesic possible. His initial discovery of dextromoramide, a 3.3~di-phenylpropylamine that was more potent than currently available analgesics, stimulated his interest in synthetic narcotics. He reasoned that with increased potency and increased receptor specificitywould come increased s&ety. The studies that led to the synthesis of fentanyl by Janssen in 1960 laid the foundation for a better
0885-3924/92/s5.00
s4
&v&v
Rl. 7flo. 3 (Su/&) April 1992
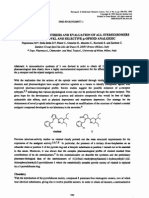
understm&ng of the structureactivity relationof narcotic analgesics and stimulated interest in developing compounds with even greater POtency and safety margins.-3 Structurally, narcotics are complex, three-dimensional compounds existing as two stereoisomers, ofwhich usually only one isomer is able to produce analgesia. Indeed, the presence or absence of analgesic activity is intimtely related to its stereochemical structure, in keeping with the lock-and-key hypothesis of narcotic action.5~0 Hence, relatively minor changes in conformation of a narcotic molecule significantly alter pharmacologic activity. This concept and dissatisfaction with available opioids, especially morphine and meperidine, as less-thanoptimal molecules to reach and stimulate the opioid Q receptor have been two major forces in the design and development of better compounds. Lipid solubiity has long been recognized as a key factor in the passage of drugs across the bloodbrain barrier. Because meperidine is almost 30-35 times more lipid soluble than morphine (octanol pH 7.4 buffer partition coefficient = 38.8 compared with 1.42), chemists began experimenting with congeners of meperidine. Because benzene rings are known to enhance lipid solubiity, a phenyl group replaced one hydrogen of the methyl group attached to the nitrogen in meperidine in one of the earliest compounds studied (P.Janssen, personal communication). The result was enhanced analgesic activity, although the spatial arrangements of those elements of the molecule chiefly responsible for interacting with the receptor were still less than ideal. It was subsequently found that by separating the phenyl group linking the nitrogen on meperidine by three carbons instead of one and then adding a hydroxyl group to the third carbon, a compound, later called phenoperidine, could be created. This compound was 20 times more potent than morphine and approximately 200 times more potent than meperidine.6 Continuing attempts to optimize molecular configuration eventuated in fentanyl, a compound with 100-300 times the potency of morphine (depending on the species evaluated).6*7*ts Note that the distance between the peperidiie nitrogen and the benzene ring is reduced from three to two carbon atoms, the ester on the right side of the molecule is reversed, and one of its oxygen molecules is replaced with a nitrogen. In addition to increased potency, fentanyl pasSesses an analgesic therapeutic index approximately four times that of morphine (277 vs. 70) and
ships
more than 50 times that of meperidine (277 vs. 5). With the attachment of a small C-O-C tail, fentanyl is converted to a new variant called carfentanil. This molecule has a potency of approximately 10,000 timps that of morphine and a therapeutic index of about 8500 in (nonventilated) rats. At the same time Janssen was beginning his research, attempts were being made in France to produce sedation with intense analgesia, termed twilight sleep or artificial hibernation. These techniques were popularized with the use of mixtures of tranquilizers (phenothiazines) and narcotics called lytic cocktails.* Early investigations in which these compounds were used focused attention on the need for more potent narcotic analgesics with fewer side effects and a higher safety margin. Among the opioids studied were the ones synthesized by Janssen-dextromoramide, phenoperidine, pi&amide, and, fmally, fentanyI.3~*3~16 Fentanyl was most impressive because of its greater potency (150 times that of morphine), its higher therapeutic index (LD~,/ED,o) (400 vs. 4.8 for mepericlme and 70 for morphine), and the absence of side effects. It was also during thii time that DeCastro and Mundeleer17 developed the concept of neurolept analgesia, which combines the use of a major tranquilizer, most frequently the butyrophenone droperidol, and a potent opioid analgesic, fentanyl or phenoperidine. Neurolep t analgesia is characterized by analgesia, amnesia, absence of overt motor activity, suppression of autonomic reflexes, and maintenance of cardiovascular stability. The use of droperidol and fentanyl, available in the United States as a 5&l mixture of 2.5 mg and 50 ug, respectively, gained popularity in both the United States and Europe. The combination is now used as a component of a balanced anesthetic technique with nitrous oxide (50-700/, in oxygen. Another important development in the evolution of the opioids occurred in 1969, when Iowenstein and colleagueP reintroduced the concept that opioids in sufficient doses can be anesthetic. The beginnings of open-heart surgery featured irnportantly in this event, because clinicians were attempting to anesthetize and operate on patients with markedly impaired cardiovascular and pulmonary function in whom even small degrees of myocardial depression could be catastrophic. Thus, the discovery that morphine (l-3 mg/kg) with oxygen (1OOO/o) produced anesthesia without myocardial depression, and often with increased cardiac output, was initially widely acclaimed.l~~~
Kll. 7 No. 3 (Suppl.) Apti
History and .D&opment
of Rentunyl Series .the
S5
Significant disadvantages soon became apparent, however, including incomplete amnesia, occasional histamine-related reactions (cutaneous flushing, hypotension, and bronchoconstriction), marked increases in intraoperative and postoperative blood and fluid requirements, and especially prolonged postoperative respiratory depression.g-*4 In addition, cardiovascular stability was not always complete: Bradycardia, bypotension, or hypertension occurred frequently, and the addition of nitrous oxide caused cardiovascular depression.*g~~Difficulties with morphine anesthesia were most evident in patients undergoing coronary artery surgery, particularly those lacking a history of heart failure_W&*4 Because of these problems with morphine oxygen anesthesia, a suitable alternative was sought among existing opioids. Meperidine was the first substitute studied. After about a year, it was concluded that meperidine was not a suitable alternative to morphine as an anesthetic in patients with serious cardiovascular disease. Studies showed that it caused sign&ant cardiovascular depression and tachycardia and, in anesthetic doses, a marked decrease in cardiac output and even cardiac arn~t.*~-*~ Additional studies demonstrated that alphaprodine and piritramide were not appreciably different from meperidine.30f1 Investigators interested in opioid anesthesia then began to study fentanyl.32-35 In animals anesthetixed with other anesthetics, fentanyl caused only minor changes in cardiovascular limction, e.g., small decreases in blood pressure and minimal or no change in ventricular performance.32*33135 Huge doses of fentanyl, up to 3 mg/kg, given to dogs under basal anesthesia with barbiturates were found to produce a dose-dependent decrease in heart rate; only small reductions in cardiac output, peripheral resistance, and arterial pressure; and an increase in stroke vol~re.34 These lindings suggested that fentanyl might be a useful anesthetic in humans. Fentanyl (50-100 ug/kg) with oxygen (100%) was then evaluated as an anesthetic in patients undergoing mitral valve and coronary artery surgery.34$3sChanges in cardiovascular dynamics with induction doses ranging from 8 to 30 pg/kg consisted of small decreases in heart rate and arterial blood pressure. All other cardiovascular variables studied, including cardiac output, remained unchanged, even with additional doses up to 100 lrg/kg. Fentanyl currently is popular for use as a narcotic
anesthetic, despite its potential for cardiovascular depression and stimulation, respiratory depression, muscle rigidity, and, occasionally, incomplete anesthesia.37-40hs success, particularly in higher doses, portends changes in anesthetic practice of the future, especially with newer, more potent analgcsim with higher therapeutic indices and other desirable pharmacokinetic characteristics. Sufentanil is a new synthetic opioid that is approximately 5-10 times more potent than fentanyl and has a therapeutic index (LD,/ED,~ approximately 100 times greater than that of fentanyl (25,000 vs. 277) in rats. Sufentanil, a derivative of carfentani& is about 5OOO times more potent than morphine and has an even higher analgesic therapeutic index than carfimtanil, more than 25,000. lo The degree of lipid solubility of sufimtanil is more than 1100 times that of morphine. lo An important concept in the search for better narcotics is the hypothesis that increased potency implies increased specificity for the opioid (u) receptor, including greater lipid solubility. Therefore, fewer molecules are required to cross the blood-brain barrier to reach receptor sites, thus leaving fewer molecules available in the circulation to produce unwanted reactions. Data indicate that the gain in potency of sufentanil has been achieved not with increased toxicity but with increased safety. Sufentanil was approved for clinical use by the United States Food and Drug Administration in 1984 as an anesthetic supplement and complete anesthetic? The cardiovascular actions of this opioid are similar to those of fimtanyl; however, sufentanil may be more effective in blocking sympathetic activation during surgical stimulation, especially in patients prone to intraoperative hypertension.4~42 Sufentanil also provides as much cardiovascular stability as fentanyl (or possibly greater) when employed in a balanced anesthetic technique.43-46 Alfentanil is another new narcotic analgesic. It is one-fourth as potent as and shorter acting than fentanyI.47Its therapeutic index is also high (1080) in rats.28These actions have indicated that the drug may be of use as an anesthetic induction agent or anaIgesic supplement, especially in patients undergoing short operative procedures. Studies in dogs demonstrated little change in hemodynamics with moderate doses (160 ug/kg) of alfentanil, whereas very large doses (5 mg/kg) resulted in transient cardiac stimulation (increases in left ventricle contractility, aortic blood flow velocity, and accel-
St5
Stanlq
Vol.fJVo.3 [&q11.)April 1992
eration).*fl Heart rate, cardiac output, and pulmonary and systemic vascular resistance also increased contractility; following 5 mg/kg of alfentanil. Transient increases in myocardial
administration
of opioids. Anesthesiology
1984;61:276.
12. Labotit H, Hugyenard P. Pratique de lbibernoth&apie en chirurgie et en mtdecine. Paris: Masson et tie, 1954. 13. Janssen PAJ, Jageneau AH. A new series of potent analgesics. J Pharm Pharmacol 1958;lO: 14. 14. Janssen PAJ, Eddy NB. Compounds related to pethidine-IVz new general chemical methods of increasing activity of pethidinc. J Med Chcm 1960;2:32. 15. Janssen PAJ. Pirinitramide (R3365), a potent analgesic with unusual chemical structure. J Pharm Pharmacol 1961;13:513. 16. Janssen PAJ. The inhibitory effect of fentanyl and other morphine-like analgesics on the warm waterinduced t&l withdrawal reflex in rats. Drug lies 1963;13:502. 17. De Castro J, Mundcleer R. Anesthbie sans barbituriques: la neuroleptanalgisie. Anaesth Analg (Paris) 1959;:6:1022. 18. Lowenstein E, Hallowell P, J&in FH, et al. Cardiovascular response to large doses of intravenous morphine in man. N Engl J Med 1969;28 1: 1389. 19. Stoelting RK, Gibbs PS. Hemodynamic effects of morphine and morphine-nitrous oxide in valvular heart disease and coronary artery disease. Anesthesiology 1973;38:45. 20. Arens JT, Benbow BP, Ochsner JL, Theard R. Morphine anesthesia for aorto-coronary by-pass procedures. Anesth Analg 1972;51:901-909. 2 1. Stanley TH, Gray NJ, Staford W, Armstrong R. The effects of high-dose morphine on fhtid and blood requirements in open-heart operations. Anesthesiology 1973;38:536. 22. HasbrouckJD. Morphine anesthesia for open heart surgery. Ann Thorac Surg 1970; 103364-369. 23. McDermott RW, Stanley TH. Cardiovascular effects of low concentrations of nitrous oxide dluring morphine anesthesia. Anesthesiology 1974;41:89-91. 24. Lowenstein E. Morphine anesthesia-a tive. Anesthesiology 1971;35:563. perspec-
mean aortic, pulmonary artery, left- and rightatrial pressures; and increased systemic vascular resistance have been reported with lower doses (ZOO pg/kg) of aifentanil in dog.48l49 Despite some problems (e.g., potential for cardiovascular depression and stimulation, respiratory depression, muscle rigidity, and, occasionally, incomplete anesthesia), opioids probably will remain popular as anesthetic supplements anesthetics in the future because effect on most organ systems.5o53 and as complete of their minimal
Rqf~ewes
1. Van Bever WFM, Niemegeers CJE, Schellekens KHL. N-4 substituted 1(2-aryl-rthyl)4-pipetidcnyl-N-phenylproanamides, a novel series of extremely potent analgesics with unusually high safety margin. Atzneimittelforsch 1973;26:1548. 2. Niemegeers CJE, Schellekens KHL, Janssen PAJ. Sufentanil, a very potent and extremely safe intravenous morphine-like compound in mice, rats and dogs. Drug Res 1976;26:1551. 3. Janssen PAJ. A review of the chemical features associated with strong morphine-like activity. Br J Anaesth 1962;34:260. 4. Snyder SH. Opiate receptors in the brain. N Engl J Mcd 1977;296:266. 5. Foldcs FF, Swerdlow M, Sier ES. Chemistry of narcotics and narcotic antagonists. In: Foldes FF, Swerdlow M, Siker ES, eds. Narcotics and narcotic antagonists. Springfield, IL: Charles C Thomas, 1954:10-26. 6. Beckett AH, Casey AF. Synthetic analgesics, stereochemical considerations. J Pharm Pharmacol 1954;6:986. 7. Beckett AH. Analgesics and their antagonists: some steric and chemical considerations. Part I. The dissociation constants of some tertiary amines and synthetic analgesics, the conformations of methadone-type compounds. J Pharm Pharmacol 1956;8:848. 8. Meuldermans WEG, Hurkmans RMA, HeykantsgP. Plasma protein binding and distribution of fentanyl, sufentanil, alfentanil and lofentanil in blood. Arch Int Pharmacodyn Ther 1982;257:4-19. 9. Irysen JE, Gommeren W, Niemegeers CJE. rH$ufcntanil, a superior ligand for p-opiate receptors: binding properties and regional distribution in rat brain and spinal cord. Eur J Pharmacol 1983;87:209-225. 10. Cookson RF, Towse GDW. Tbe search for new analgesics. Clin Res Rev 1981;1:219. 11.
COUGHS E/55, Mather
25. Eddy NB, Halbach H. Synthetic substances with morphine-like effect. Clinical experience: potency, sideeffects, addiction liability. Bull WHO 1957; 17:569. 26. Freye E. Cardiovascular effects of high dosages of fentanyl, mepelidine and naloxone in dogs. Anesth Analg 197*53:40-47. 27. Stanley TH, Bidwai AV, Lunn JK, Hodges MR. Cardiovascular effects of nitrous oxide during meperidine infusion in the dog. Anesth Analg 1977;56:836-841. 28. De Castro J, van de Water A, Wouters L, JShonneux R, Reneman R, Kay B. Comparative study of cardiovascular, neurological and metabolic side effects of eight narcotics in dogs. Acta Anaesthesiol kelg 1979;3&5. 29. Stanley TH, Liu WS. Cardiovascular effects of meperidine-N20 anesthesia before and after pancuronium. Anestb Analg 1977;56:FY-673.
LE. Intratheeal
and epidural
RI. 7&o. 3 (Suppl.)A@ 1992
History Devebpment theFentanyl and of Smes
s7
30. Straucr BE. Contractile pi&amide, meperidine and study of effects on the isolated Anesthesiology 1972;37:304-3
rcsponscs to morphine, fcntanyl: a comparative ventricular myocardium. 10.
sufcntanil anesthesia: a study in patients m&going cardiac surgery. Anesth A&g 1982;61:115. 43. Larsen R, Sonntag H, Schenk H, RadkeJ, mfiker 0. Die Wirkungen von Sufctnranil und Fentanyl auf hemodynamik, coronardorcholutnng and myocardialen Metabolismlus dca Menschen. Anaesthesist 1980;29:277279, 44. Rally G, Kay B, Cocks F. A double blind comparison of high doses of fentanyl and sufentanil in man: influence on cardiovascular, respiratory and metabolic parameters. Acta Anaesthesiol Belg 1979;3&247-254. 45. FlackeJw, Kripke BK, Bloor BC, Flacke WE, Katz RL. Intraoperative effectiveness of sufentanil, fentanyl, meperidine or morphine in balanced anesthesia: a double blind study. Anesth Analg 1983;62:259. 46. Van de Walle J, Lauwers P, Adriannen H. Double blind comparison of fentanyl and sufentanii in anesthesia. Acta Anaesthesiol Belg 1976;3:129-138. 47. Nauta J, de Lange S, Koopman D, Spierdijk J, van Kleef J, Stanley TH. Anesthetic induction with alfentan% a new short acting narcotic analgesic. Anesth Analg i982;61:267-271. 48. Schauble JF, Chen BB, Murray PA. Marked hemodynamic effects of bolus administration of alfentanil in conscious dogs. Anesthesiology 1983;59:A85. 49. Bailey DR, Miller ED, Kaplan JA, Rogers PW. The renin-angiotensinaldosterone system during cardiac surgery with morphine-nitrous oxide anesthesia. Anesthesiology 1975;42:538-544. 50. Stanley TH, Webster LR. Anesthetic requirements and cardiovascular effects of fentanyl-oxygen and fentanyl-diazepam-oxygen anaesthesia in man. Anesth Analg 1978;57:411. 51. Stanley TH, Philbin DM, Coggins CH. Femanyloxygen anaesthesia for coronary artery surgery: cardiovascular and antidiuretic hormone responses. Can Anaesth Sot J 1979;26:168-172. 52. Hug CC Jr, Murphy MR. Fentanyl disposition in cerebrospinal fluid and plasma and its dati~nship to ventilatory depression in the dog. Anesthesiology 1979;50:342-349. 53. Cooper GM, Holdcroft A, Hall GM, AlaghbandZadeh J. Epidural analgesia and the metabolic response to spry. Can Anaesth Sot J 1979;26:381-385.
31. Rcddy P, Liu WS, Port D, G&nor S, Stanley TH. Comparison of haemodynamic effects of anaesthetic doses of alphaprodine and sufentanil in the dog. Can Anaesth SocJ 1980;27:345-350. 32. Pats&e D, Gethmann Jw, Hess !%%Tajrrow J, Waibel H. Hemodynamic Korroardruchblutung und Myocardialer Sauerst&verbrauch unter hohen Fentanyl und Pirit=&dosen. Anaesthesist 1976;25:309. 33. Freye E. Effects of high doses of fentanyl on myocardial infarction and cardiogenic shock in the dog. Resuscitation 1974;s 105. 34. Liu WS, Bidwai AV, Stanley TH, Isem-Amaral S. Cardiovascular dynamics afler large doses of fentanyl and fentanyl plus N,O in the dog. Anesth Analg 1976;55:168-172. 35. Eisele JH, Reitan J, Torten M, Miller CH. Myocardial sparing effect of fcntanyl during halothane anesthesia in dogs. Br J Anaesth 1975;47:937. 36. Lunn JK, Stanley TH, Webster LB., Eisele J, Woodward A. High dose fentanyl anesthesia for coronary artery surgery: plasma fentanyl concentration and influence of nitrous oxide on cardiovascular responses. Anesth Analg 1979;58:390. 37. Bailey PL, Stanley TH. Narcotic intravenous anesthetics. fn: Miiler RD, ed. Anesthesia. New York: Churchill Livingstone, 1990:281-366. 38. Robinson S, Gregory GA. Fentanyl-air-oxygen anesthesia for ligation of patent ductus arteriosus in preterm infants. Anesth Analg 1981;60:331-334. 39. Stanley TH, Berman L, Green 0, et al. Plasma catecholamine and cortisol responses to fentanyl-xygen anesthesia for coronary-artery operations. Anesthesiology 1980;53:250. 40. Sebel PS, Bovill JG, Wauquier A, Rog P. Effects of high dose fentanyl anesthesia on the electroencephalogram. Anesthesiology 198 1;55:203-2 11. 41. De Lange S, Stanley TH, Boscoe h(J, Pace NL Comparison of sufentanil-0, and fentanyl-0, for coronary artery surgery. Anesthesiology 1982;56:112-118. 42. Sebel PS, Bovill JG. Cardiovascular effects of
You might also like
- Piperidine Derivatives. XVIII. The Condensation of Aromatic Aldehydes With 1-Methyl-4-Piperidone - JACS, 1948, 70 (5), 1820 - Ja01185a051Document6 pagesPiperidine Derivatives. XVIII. The Condensation of Aromatic Aldehydes With 1-Methyl-4-Piperidone - JACS, 1948, 70 (5), 1820 - Ja01185a051muopioidreceptorNo ratings yet
- OH&S Workplace Assessment ChecklistDocument9 pagesOH&S Workplace Assessment ChecklistAldrin ZlmdNo ratings yet
- Long-Acting Fentanyl Analogues: Synthesis and Pharmacology of N - (1-Phenylpyrazolyl) - N - (1-Phenylalkyl-4-Piperidyl) PropanamidesDocument11 pagesLong-Acting Fentanyl Analogues: Synthesis and Pharmacology of N - (1-Phenylpyrazolyl) - N - (1-Phenylalkyl-4-Piperidyl) PropanamidesBic0000No ratings yet
- Synthesis and Analgesic Properties of N-Substituted Trans-4a-Aryldecahydroisoquinolines - J. Med. Chem., 1988, 31 (3), PP 555-560Document6 pagesSynthesis and Analgesic Properties of N-Substituted Trans-4a-Aryldecahydroisoquinolines - J. Med. Chem., 1988, 31 (3), PP 555-560muopioidreceptor100% (1)
- The Biosynthesis of Ephedrine PDFDocument13 pagesThe Biosynthesis of Ephedrine PDFSchpyak Schmyak100% (1)
- Using The Pharmaceutical Literature (2006)Document303 pagesUsing The Pharmaceutical Literature (2006)muopioidreceptorNo ratings yet
- Synthetic Analgesics: DiphenylpropylaminesFrom EverandSynthetic Analgesics: DiphenylpropylaminesRating: 4 out of 5 stars4/5 (1)
- CENTRAL ANALGETICS Analgesics Chemistry Pharmacology of Drugs Daniel Lednicer 1982Document236 pagesCENTRAL ANALGETICS Analgesics Chemistry Pharmacology of Drugs Daniel Lednicer 1982BASKAR.LNo ratings yet
- Astm c1161 13Document19 pagesAstm c1161 13Taiana BonadioNo ratings yet
- ALKALOID With Some IsolationDocument24 pagesALKALOID With Some IsolationRajesh Kumar100% (1)
- Encyclopedia of Pharmaceutical Technology, Volume 20Document335 pagesEncyclopedia of Pharmaceutical Technology, Volume 20Mihai Petrescu88% (17)
- Chapter Wise QuestionsDocument6 pagesChapter Wise QuestionsDr. B. Sree Giri Prasad100% (2)
- Studies in Piperidone Chemistry. I. A Synthesis of 5-Homopiperazinones - J Org Chem, 1949, 14 (4), 530 - Jo01156a005Document7 pagesStudies in Piperidone Chemistry. I. A Synthesis of 5-Homopiperazinones - J Org Chem, 1949, 14 (4), 530 - Jo01156a005muopioidreceptorNo ratings yet
- Organic Synthesis - 2: Plenary Lectures Presented at the Second International Symposium on Organic SynthesisFrom EverandOrganic Synthesis - 2: Plenary Lectures Presented at the Second International Symposium on Organic SynthesisS. SarelNo ratings yet
- 1 - Piperidinyl) Methyl-2 - (4-Substituted Styryl) - 5-Chloro-Benzimidazole Derivatives: Synthesis and Analgesic ActivityDocument1 page1 - Piperidinyl) Methyl-2 - (4-Substituted Styryl) - 5-Chloro-Benzimidazole Derivatives: Synthesis and Analgesic Activitymuopioidreceptor100% (2)
- Pseudoephedrine: 1. Synonyms CFR: Nist #Document18 pagesPseudoephedrine: 1. Synonyms CFR: Nist #Yuyun Saputri NingsihNo ratings yet
- Synthesis of 3,6-Diazabicyclo (3.1.1) Heptanes As Novel Ligands For The Opioid Receptors - Bioorg Med Chem, 2006, 14 (3), 676Document16 pagesSynthesis of 3,6-Diazabicyclo (3.1.1) Heptanes As Novel Ligands For The Opioid Receptors - Bioorg Med Chem, 2006, 14 (3), 676muopioidreceptorNo ratings yet
- About The Dyes: Dyes For Cellulose FibersDocument4 pagesAbout The Dyes: Dyes For Cellulose FibersmanqabatNo ratings yet
- Atom Economical Synthesis of 4'-Methylpropiophenone by Friedel-Crafts Acylation of Toluene With Propionic Anhydride Over Solid Me So Porous Superacid UDCaT-5Document17 pagesAtom Economical Synthesis of 4'-Methylpropiophenone by Friedel-Crafts Acylation of Toluene With Propionic Anhydride Over Solid Me So Porous Superacid UDCaT-5S Bharadwaj ReddyNo ratings yet
- Chemical and Physical Prop of PetroleumDocument35 pagesChemical and Physical Prop of Petroleumshivam tiwari100% (1)
- Synthetic Analgesics: Morphinans: BenzomorphansFrom EverandSynthetic Analgesics: Morphinans: BenzomorphansRating: 2 out of 5 stars2/5 (2)
- Opiate - Chemistry.and - Metabolism BedfordDocument5 pagesOpiate - Chemistry.and - Metabolism BedfordSam SlaterNo ratings yet
- Development of Potent μ and δ Opioid Agonists with High Lipophilicity - J. Med. Chem., 2011, 54 (1), pp 382-386Document5 pagesDevelopment of Potent μ and δ Opioid Agonists with High Lipophilicity - J. Med. Chem., 2011, 54 (1), pp 382-386muopioidreceptorNo ratings yet
- Structure-Activity Relations in Analgesics Based On 4-AnilinopiperidineDocument7 pagesStructure-Activity Relations in Analgesics Based On 4-AnilinopiperidineJonathan Berry100% (2)
- Sharma2018 Article The Search For The Next Euphoric NonDocument17 pagesSharma2018 Article The Search For The Next Euphoric NonDr. Ghulam FareedNo ratings yet
- Fire cable performance standardsDocument3 pagesFire cable performance standardsRajan Varghese100% (1)
- Kratom Alkaloids An Historical Perspective - Arndt - FSI 208 (2011)Document6 pagesKratom Alkaloids An Historical Perspective - Arndt - FSI 208 (2011)dextroenantiomerNo ratings yet
- The Plant Alkaloids PDFDocument824 pagesThe Plant Alkaloids PDFSandro Rogério Giacomelli100% (1)
- Recent Advances in The Chemistry of Oripavine & DerivativesABB - 2014072111275178Document15 pagesRecent Advances in The Chemistry of Oripavine & DerivativesABB - 2014072111275178Ji ChemNo ratings yet
- NIDA Monograph 147 Discovery of Novel Opioid MedicationsDocument318 pagesNIDA Monograph 147 Discovery of Novel Opioid MedicationsAndrew Leyton100% (1)
- Hydrates of 1-Methyl-3 - and - 4-Piperidone Hydrochlorides - J Org Chem, 1959, 24 (3), 342 - Jo01085a015Document4 pagesHydrates of 1-Methyl-3 - and - 4-Piperidone Hydrochlorides - J Org Chem, 1959, 24 (3), 342 - Jo01085a015muopioidreceptor100% (1)
- The Simple Plant IsoquinolinesDocument162 pagesThe Simple Plant Isoquinolinesjj_dokov67% (6)
- 8 Absorber DesignDocument16 pages8 Absorber DesignilhamriswandaaNo ratings yet
- Safely Purging Air from Pipelines and VesselsDocument7 pagesSafely Purging Air from Pipelines and Vesselsgan_raoNo ratings yet
- Parker O-Ring Material Guide-2008Document72 pagesParker O-Ring Material Guide-2008Ian Pillay50% (2)
- Metal—Ammonia Solutions: Proceedings of an International Conference on the Nature of Metal-Ammonia Solutions: Colloque Weyl IIFrom EverandMetal—Ammonia Solutions: Proceedings of an International Conference on the Nature of Metal-Ammonia Solutions: Colloque Weyl IINo ratings yet
- 903Document8 pages903getjenNo ratings yet
- Forensic Science International: Shinichi Sato, Shinichi Suzuki, Xiao-Pen Lee, Keizo SatoDocument5 pagesForensic Science International: Shinichi Sato, Shinichi Suzuki, Xiao-Pen Lee, Keizo SatoCallum DuncanNo ratings yet
- Pharmacology of Oriental Plants: Proceedings of the First International Pharmacological Meeting, Stockholm, 22-25 August, 1961From EverandPharmacology of Oriental Plants: Proceedings of the First International Pharmacological Meeting, Stockholm, 22-25 August, 1961K. K. ChenNo ratings yet
- Synthesis and Biological Evaluation of Novel Epibatidine Analogues - Ying Liu (Dec 2003) - PHD ThesisDocument86 pagesSynthesis and Biological Evaluation of Novel Epibatidine Analogues - Ying Liu (Dec 2003) - PHD ThesismuopioidreceptorNo ratings yet
- Selective N-Dealkylation of Tertiary Amines With Vinyl Chloroform Ate - An Improved Synthesis of Naloxone - Tetrahedron Lett, 1977, No 18, P 1567-1570Document4 pagesSelective N-Dealkylation of Tertiary Amines With Vinyl Chloroform Ate - An Improved Synthesis of Naloxone - Tetrahedron Lett, 1977, No 18, P 1567-1570muopioidreceptor100% (1)
- THE STRUCTURE OF METOPON - J. Am. Chem. Soc., 1953, 75 (17), PP 4373-4374Document2 pagesTHE STRUCTURE OF METOPON - J. Am. Chem. Soc., 1953, 75 (17), PP 4373-4374muopioidreceptorNo ratings yet
- Advances in Endogenous and Exogenous Opioids: Proceedings of the International Narcotic Research Conference (Satellite Symposium of the 8th International Congress of Pharmacology) Held in Kyoto, Japan on July 26–30, 1981From EverandAdvances in Endogenous and Exogenous Opioids: Proceedings of the International Narcotic Research Conference (Satellite Symposium of the 8th International Congress of Pharmacology) Held in Kyoto, Japan on July 26–30, 1981Hiroshi TakagiNo ratings yet
- The Preparation and Properties of CodeinoneDocument3 pagesThe Preparation and Properties of Codeinonegeovani2100% (1)
- Alkaloid ExtractionDocument3 pagesAlkaloid ExtractionArun K.P.100% (1)
- Levo SynDocument7 pagesLevo Synziggy862003100% (1)
- The Six Trimethoxyphenylisopropylamines (Trimethoxyamphetamines)Document2 pagesThe Six Trimethoxyphenylisopropylamines (Trimethoxyamphetamines)geovani2No ratings yet
- Ronghui Lin Et Al - Enantiospecific Synthesis of Natural (-) - Cocaine and Unnatural (+) - Cocaine From D - and L-Glutamic AcidDocument10 pagesRonghui Lin Et Al - Enantiospecific Synthesis of Natural (-) - Cocaine and Unnatural (+) - Cocaine From D - and L-Glutamic AcidPoloGreenNo ratings yet
- Opium and Its AlkaloidsDocument9 pagesOpium and Its AlkaloidsMatthewNo ratings yet
- Differences Between The Mechanism of Action of MDMA, MBDB, and The Classic Hallucinogens. Identification of A New Therapeutic Class: EntactogensDocument9 pagesDifferences Between The Mechanism of Action of MDMA, MBDB, and The Classic Hallucinogens. Identification of A New Therapeutic Class: EntactogensAlex Fulkroad100% (1)
- Monographs On The Chemistry of Natural Products: Sir Bobbbt BobinsonDocument452 pagesMonographs On The Chemistry of Natural Products: Sir Bobbbt BobinsonLasitarda BluesNo ratings yet
- Stereoselective Synthesis and Evaluation of All Stereoisomers of Z4349, A Novel and Selective Μ-opioid Analgesic BOMCL 1995 5 (6) 589 0960-894X (95) 00077-7 SUPERPOTENT OpioidDocument4 pagesStereoselective Synthesis and Evaluation of All Stereoisomers of Z4349, A Novel and Selective Μ-opioid Analgesic BOMCL 1995 5 (6) 589 0960-894X (95) 00077-7 SUPERPOTENT OpioidJonathan BerryNo ratings yet
- Morfin 2Document6 pagesMorfin 2Nova DhilaNo ratings yet
- Opioid Peptides: Biology, Chemistry, and Genetics: The Peptides: Analysis, Synthesis, Biology, Vol. 6From EverandOpioid Peptides: Biology, Chemistry, and Genetics: The Peptides: Analysis, Synthesis, Biology, Vol. 6No ratings yet
- Satendra Singh - Chemistry, Design, and Structure-Activity Relationship of Cocaine AntagonistsDocument100 pagesSatendra Singh - Chemistry, Design, and Structure-Activity Relationship of Cocaine AntagonistsPoloGreen100% (1)
- Phase Transfer Catalysis Chemistry and Engineering - Journal Review - AIChE, Mar 1998, 44 (3), 612Document35 pagesPhase Transfer Catalysis Chemistry and Engineering - Journal Review - AIChE, Mar 1998, 44 (3), 612muopioidreceptorNo ratings yet
- Journal of Medicinal Chemistry, 1979, Vol. 22, No. 10Document2 pagesJournal of Medicinal Chemistry, 1979, Vol. 22, No. 10Slapdragonx100% (1)
- Neu 336753Document59 pagesNeu 336753Eduard RudenkoNo ratings yet
- Wilkinson The Acid King Pickard LSD Bust Rolling Stone Mag 2001Document18 pagesWilkinson The Acid King Pickard LSD Bust Rolling Stone Mag 2001deadlysins1No ratings yet
- An Advanced Laboratory Manual of Organic Chemistry 1923 - Heidelberger PDFDocument103 pagesAn Advanced Laboratory Manual of Organic Chemistry 1923 - Heidelberger PDFRodrigo Negrelli GuzzoNo ratings yet
- The Determination of Psilocin and Psilocybin in Hallucinogenic Mushrooms by HPLC Utilizing A Dual Reagent Acidic Potassium Permanganate and II Chemiluminescence Detection SystemDocument7 pagesThe Determination of Psilocin and Psilocybin in Hallucinogenic Mushrooms by HPLC Utilizing A Dual Reagent Acidic Potassium Permanganate and II Chemiluminescence Detection Systemgeovani2No ratings yet
- Tropane AlkaloidsDocument2 pagesTropane AlkaloidsEcha SuciNo ratings yet
- Determination of Alkaloid Structures I. Isolation Characterization and Physical MethodsDocument6 pagesDetermination of Alkaloid Structures I. Isolation Characterization and Physical Methodsgeovani2No ratings yet
- Nutmeg Oil Composition and EffectsDocument6 pagesNutmeg Oil Composition and EffectsjennyihateNo ratings yet
- 6171 Synthesis of N Isobutylnoroxymorphone From Naltrexone by A Selective Cyclopropane Ring Opening Reactionb77b PDFDocument4 pages6171 Synthesis of N Isobutylnoroxymorphone From Naltrexone by A Selective Cyclopropane Ring Opening Reactionb77b PDFlumik1234No ratings yet
- 279 291 DalCasonDocument13 pages279 291 DalCasontest1119163100% (1)
- Controlled Release OxycodoneDocument10 pagesControlled Release OxycodoneCarleta StanNo ratings yet
- Alcaloides MBDocument9 pagesAlcaloides MBSule Granados DNo ratings yet
- Chemical Composition and Profile Characteristics of Osage Orange Maclura Pomifera (Rafin.) Schneider Seed and Seed OilDocument8 pagesChemical Composition and Profile Characteristics of Osage Orange Maclura Pomifera (Rafin.) Schneider Seed and Seed OilrajrudrapaaNo ratings yet
- Ephedrine HCL - Ephedra Survey ResultsDocument12 pagesEphedrine HCL - Ephedra Survey ResultsDr. Ma Huang100% (1)
- Newer Methods of Preparative Organic Chemistry V2From EverandNewer Methods of Preparative Organic Chemistry V2Wilhelm FoerstNo ratings yet
- Multicomponent Reactions - Ambhaikar (July 2004)Document6 pagesMulticomponent Reactions - Ambhaikar (July 2004)muopioidreceptorNo ratings yet
- Multicomponent Reactions With Isocyanides - Alexander Domling Ivar Ugi - Angew Chem Int Ed, 2000, 39 (18), 3168-3210 - PII 1433-7851 (00) 3918-3169 DOI 10.1002/1521-3773 (20000915) 39:18 3.0.CO 2-UDocument43 pagesMulticomponent Reactions With Isocyanides - Alexander Domling Ivar Ugi - Angew Chem Int Ed, 2000, 39 (18), 3168-3210 - PII 1433-7851 (00) 3918-3169 DOI 10.1002/1521-3773 (20000915) 39:18 3.0.CO 2-UmuopioidreceptorNo ratings yet
- Preparation of 3-Cyano-4-Piperidone - J Am Chem Soc, 1947, 69 (6), 1535 - Ja01198a504Document1 pagePreparation of 3-Cyano-4-Piperidone - J Am Chem Soc, 1947, 69 (6), 1535 - Ja01198a504muopioidreceptor100% (1)
- Phase Transfer Catalysis Chemistry and Engineering - Journal Review - AIChE, Mar 1998, 44 (3), 612Document35 pagesPhase Transfer Catalysis Chemistry and Engineering - Journal Review - AIChE, Mar 1998, 44 (3), 612muopioidreceptorNo ratings yet
- Piperidine Derivatives. Xi. 3-Carbethoxy-4-Piperidone and 4-Piperidone Hydrochloride - Jacs, 1931, 53 (7), 2692 - Ja01358a035Document5 pagesPiperidine Derivatives. Xi. 3-Carbethoxy-4-Piperidone and 4-Piperidone Hydrochloride - Jacs, 1931, 53 (7), 2692 - Ja01358a035muopioidreceptorNo ratings yet
- Industrial Applications of Phase Transfer Catalysis (PTC) : Past, Present and FutureDocument12 pagesIndustrial Applications of Phase Transfer Catalysis (PTC) : Past, Present and FuturekvsrskNo ratings yet
- New Psychotropic Agents. VIII. Analogs of Amitriptyline Containing The Normeperidine Group - J Med Chem, 1967, 10 (4), 627 - Jm00316a024Document9 pagesNew Psychotropic Agents. VIII. Analogs of Amitriptyline Containing The Normeperidine Group - J Med Chem, 1967, 10 (4), 627 - Jm00316a024muopioidreceptorNo ratings yet
- Piperidine Derivatives. XXI. 4-Piperidone, 4-Piperidinol and Certain of Their Derivatives - J Am Chem Soc, 1949, 71 (3), 901-906 - Ja01171a038Document6 pagesPiperidine Derivatives. XXI. 4-Piperidone, 4-Piperidinol and Certain of Their Derivatives - J Am Chem Soc, 1949, 71 (3), 901-906 - Ja01171a038muopioidreceptorNo ratings yet
- Bromo Derivatives of 1-Methyl-3-Carbethoxy-4-Piperidone - SM McElvain - JACS, 1950, 72 (7), 3295 - Ja01163a524Document1 pageBromo Derivatives of 1-Methyl-3-Carbethoxy-4-Piperidone - SM McElvain - JACS, 1950, 72 (7), 3295 - Ja01163a524muopioidreceptorNo ratings yet
- Cannabimimetic Indole Derivatives (2001) - Wo0128557a1 - Am-2201 - Synthetic Cannabinoid (3 X THC Potency)Document27 pagesCannabimimetic Indole Derivatives (2001) - Wo0128557a1 - Am-2201 - Synthetic Cannabinoid (3 X THC Potency)muopioidreceptorNo ratings yet
- Atomoxetine Increases Extracellular Levels of Norepinephrine and Dopamine in Prefrontal Cortex of Rat A Potential Mechanism For Efficacy in Attention Deficit Hyperactivity Disorder (2002)Document13 pagesAtomoxetine Increases Extracellular Levels of Norepinephrine and Dopamine in Prefrontal Cortex of Rat A Potential Mechanism For Efficacy in Attention Deficit Hyperactivity Disorder (2002)muopioidreceptorNo ratings yet
- Novel Indoles Are Cannabinoid Receptor Ligands (2009) - Us2009149501a1Document54 pagesNovel Indoles Are Cannabinoid Receptor Ligands (2009) - Us2009149501a1muopioidreceptorNo ratings yet
- The Opioid Class of Analgesics - Tufts University - J David HaddoxDocument22 pagesThe Opioid Class of Analgesics - Tufts University - J David Haddoxmuopioidreceptor0% (1)
- Receptor Targeting Ligands - Wo2009080821a2 - CannabinoidsDocument115 pagesReceptor Targeting Ligands - Wo2009080821a2 - CannabinoidsmuopioidreceptorNo ratings yet
- Cannabinoid Receptor Ligands - US2004186148A1Document53 pagesCannabinoid Receptor Ligands - US2004186148A1muopioidreceptorNo ratings yet
- Substituted Furo (2,3-b) Pyridine Derivatives - US2005272763A1 - CB1 AgonistDocument96 pagesSubstituted Furo (2,3-b) Pyridine Derivatives - US2005272763A1 - CB1 AgonistmuopioidreceptorNo ratings yet
- Substituted Imidazoles As Cannabinoid Receptor Modulators - US2006089356A1Document50 pagesSubstituted Imidazoles As Cannabinoid Receptor Modulators - US2006089356A1muopioidreceptorNo ratings yet
- Cannabinoid Receptor Ligands and Uses Thereof - US2004157839A1Document72 pagesCannabinoid Receptor Ligands and Uses Thereof - US2004157839A1muopioidreceptorNo ratings yet
- Cannabinoid Receptor Ligands - US2006009528A1Document65 pagesCannabinoid Receptor Ligands - US2006009528A1muopioidreceptorNo ratings yet
- Indole Derivatives, Method For Preparating Same and Pharmaceutical Compositions Containing Same - US2006089345A1 - CB2 LigandsDocument16 pagesIndole Derivatives, Method For Preparating Same and Pharmaceutical Compositions Containing Same - US2006089345A1 - CB2 LigandsmuopioidreceptorNo ratings yet
- Keto Cannabinoids With Therapeutic Indications - US2005074408A1Document37 pagesKeto Cannabinoids With Therapeutic Indications - US2005074408A1muopioidreceptorNo ratings yet
- Benzodioxole Derivatives - US2005143373A1 - CB1 Agonists (Antiobesity)Document106 pagesBenzodioxole Derivatives - US2005143373A1 - CB1 Agonists (Antiobesity)muopioidreceptorNo ratings yet
- Cannabinoid Receptor Ligands and Uses Thereof - US2004214855A1 - CB LigandsDocument46 pagesCannabinoid Receptor Ligands and Uses Thereof - US2004214855A1 - CB LigandsmuopioidreceptorNo ratings yet
- Cannabinoid Receptor Ligands and Uses Thereof - US2004157838A1Document67 pagesCannabinoid Receptor Ligands and Uses Thereof - US2004157838A1muopioidreceptorNo ratings yet
- Cannabinoid Receptor Ligands and Uses Thereof - US2004122074A1Document33 pagesCannabinoid Receptor Ligands and Uses Thereof - US2004122074A1muopioidreceptorNo ratings yet
- Noble Gases 20 Aug 2022Document2 pagesNoble Gases 20 Aug 2022PLABAN DASNo ratings yet
- Chapter 03 AnnotDocument4 pagesChapter 03 AnnotNur Amira Mardiana ZulkifliNo ratings yet
- Kolorsafe Liquid Acid Neutralizer - SDS - NA - 012115 - FINALDocument8 pagesKolorsafe Liquid Acid Neutralizer - SDS - NA - 012115 - FINALJUAN FELIPE ORTIZ PARRANo ratings yet
- Toxicology: Metal Chosen: MERCURYDocument13 pagesToxicology: Metal Chosen: MERCURYsamarpita senguptaNo ratings yet
- Phosphorus, Reactive, TNT, PhosVer 3 Method 8048, 02-2009, 9th EdDocument7 pagesPhosphorus, Reactive, TNT, PhosVer 3 Method 8048, 02-2009, 9th EdRaúl BatistaNo ratings yet
- USCG Cargo Compatibility Chart For Chemical TankersDocument19 pagesUSCG Cargo Compatibility Chart For Chemical TankersRodcyn YumangNo ratings yet
- 07 10 2021 Bio AssignmentDocument4 pages07 10 2021 Bio AssignmentSuneel ReddyNo ratings yet
- Lecture 2 - Cellulose Structure PDFDocument55 pagesLecture 2 - Cellulose Structure PDFpipers10No ratings yet
- MSDS Mindray M-30 LyseDocument2 pagesMSDS Mindray M-30 LyseSandra HubayaNo ratings yet
- WWW - Ncbi.nlm - Nih.gov Pubmed 15151274Document2 pagesWWW - Ncbi.nlm - Nih.gov Pubmed 15151274Ethan MorganNo ratings yet
- 1995Document283 pages1995Robert BataraNo ratings yet
- Ssi Schaefer Container AsDocument8 pagesSsi Schaefer Container AsRebecca HartmanNo ratings yet
- 2012 - Cosmetic Ingredient Review - Amended Safety Assessment of Alkyl Esters As Used in CosmeticsDocument83 pages2012 - Cosmetic Ingredient Review - Amended Safety Assessment of Alkyl Esters As Used in CosmeticsymiyazyNo ratings yet
- ACROLEIN MSDSDocument6 pagesACROLEIN MSDSzaedmohd50% (2)
- Japanning 103, Traditional Japanning, The BlacDocument8 pagesJapanning 103, Traditional Japanning, The BlacFredy Alvarez LucasNo ratings yet
- Precipitation-Hardening Bolting (UNS N07718) For High Temperature ServiceDocument4 pagesPrecipitation-Hardening Bolting (UNS N07718) For High Temperature ServiceJose Anisio SilvaNo ratings yet
- DeLonghi Instruction Manual ECP3220 - 3420 - 3630Document7 pagesDeLonghi Instruction Manual ECP3220 - 3420 - 3630ureehwsenqNo ratings yet
- Balauro Worksheet Protein SynthesisDocument4 pagesBalauro Worksheet Protein SynthesisHami BalauroNo ratings yet
- METAL FABRICATION RAW MATERIALS GUIDEDocument8 pagesMETAL FABRICATION RAW MATERIALS GUIDEEdbert TulipasNo ratings yet
- SDS Body Mist GenericDocument4 pagesSDS Body Mist Genericsabuyexpress.worldwideNo ratings yet
- Case Studies of The EntrepreneursDocument14 pagesCase Studies of The EntrepreneursSneha DobariaNo ratings yet