Professional Documents
Culture Documents
To The Hospital and Back Home Again-A Nurse-Practitioner Based Program
Uploaded by
oldsjeOriginal Description:
Original Title
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
To The Hospital and Back Home Again-A Nurse-Practitioner Based Program
Uploaded by
oldsjeCopyright:
Available Formats
MODELS OF GERIATRIC CARE, QUALITY IMPROVEMENT, AND PROGRAM DISSEMINATION
To the Hospital and Back Home Again: A Nurse Practitioner-Based Transitional Care Program for Hospitalized Homebound People
Katherine Ornstein, MPH, w Kristofer L. Smith, MD, MPP,w Dinah Herlands Foer,z BA, Maria Tereza Lopez-Cantor, ANP-BC,w and Theresa Soriano, MD, MPHw
Homebound older adults may receive suboptimal care during hospitalizations and transitions home or to postacute settings. This 2-year study describes a nurse practitioner (NP)-led transitional care program embedded within an existing home-based primary care (HBPC) program. The transitional care pilot program was designed to improve coordination and continuity of care, reduce readmissions, garner positive provider feedback, and demonstrate nancial benets through shorter length of stay, lower cost of inpatient stay, and better documentation of patient complexity. A detailed mixed-methods evaluation was conducted to characterize the hospitalized homebound population and investigate provider feedback and program feasibility, effectiveness, and costs. Length of stay (LOS), case-mix index, and admission-related nancial costs were compared before and after the intervention using a prepost design. Structured focus groups were conducted with inpatient and primary care providers to collect feedback on the usefulness of and satisfaction with the program. The program improved communication between home-based primary care providers and inpatient providers of all disciplines and facilitated the timely and accurate transfer of critical patient information. The intervention failed to decrease hospital LOS and readmission rate signicantly for people who were hospitalized. The nancial implications were reassuring, although future studies are necessary. This model of a NP-led program may be feasible for enhancing inpatient management and transitional care for older adults in HBPC programs and should be considered to augment the HBPC care model. J Am Geriatr Soc 59:544551, 2011.
Key words: home care; homebound older adults; homebased primary care; house calls; transitions of care
From the Department of Epidemiology, School of Public Health, Columbia University, New York, New York; wDivision of General Internal Medicine, Samuel Bronfman Department of Medicine, Mount Sinai School of Medicine, New York, New York; and zSchool of Medicine, Yale University, New Haven, Connecticut. Address correspondence to Katherine Ornstein, The Mount Sinai Visiting Doctors, Box 1216, One Gustave L. Levy Place, New York, NY 10029. E-mail: Katherine.ornstein@mssm.edu DOI: 10.1111/j.1532-5415.2010.03308.x
eamless transitions between care settings are critical to high-quality care for frail older persons.1 This holds particularly true for the growing number of older homebound adults.2 With a high prevalence of chronic and endstage disease,3 older homebound adults have higher rates of hospitalizations and ED visits than their age-matched peers.4 With low socioeconomic status, high rates of cognitive impairment, and complex treatment plans, homebound patients are particularly vulnerable to poor outcomes during care transitions.5,6 Transitions of care settings challenge patients, families, and providers.7 After a transition from one care setting to another, patients are often confused regarding medications,8 fail to complete further recommended evaluation,9 and do not follow up on outstanding test results.10,11 Advance directives are often not transferred with the patient.12 Mistakes can undermine patient and family satisfaction and contribute to more-frequent hospital readmissions and greater use of medical services.11,13,14 Primary care providers (PCPs) are also dissatised with care transitions.15 Few PCPs are notied of patient discharges or are involved in discharge planning.15,16 Important hospitalization information is often missing or not communicated.17,18 Despite the high volume of transitions and the greater likelihood of poor outcomes, there have been no reports of transitional care programs specically for people who are homebound, who have multiple comorbidities and present with greater baseline functional and cognitive impairment. Although several trials of nurse-led transitional care models in older and other high-risk populations have been successful at reducing or delaying readmissions and costs,1921 they have not been tested in homebound people.
JAGS 59:544551, 2011 r 2011, Copyright the Authors Journal compilation r 2011, The American Geriatrics Society
0002-8614/11/$15.00
JAGS
MARCH 2011VOL. 59, NO. 3
TRANSITIONAL CARE FOR HOSPITALIZED HOMEBOUND PEOPLE
545
Although home-based primary care (HBPC) programs serve a critical need for the underserved homebound by ensuring that they receive regular primary care services and ancillary support at home, they do not directly address transitional care needs. At the Mount Sinai Visiting Doctors Program (MSVD), a HBPC program serving urban homebound people, poor patient outcomes and provider dissatisfaction associated with care transitions were commonly noted problems. In response, drawing on prior successful models,19,2224 MSVD developed a rst-ever nurse practitioner (NP)-led transitional care program for homebound people embedded within an existing HBPC program. The core processes of MSVDs Inpatient NP Transitional Care Program are described below. In addition to characterizing MSVDs hospitalized population, results of a mixed methods evaluation of the implementation process, program effectiveness, and costs are provided.
Intervention Setting: MSVD Founded in 1995, MSVD, a joint program of Mount Sinais departments of medicine and geriatrics, is currently the largest academic HBPC program in the United States. Previously described in detail,25 the program employs 15 physicians, two NPs, and support personnel including two nurses, four social workers, and ve clerical staff to serve more than 1,000 homebound patients annually. To be enrolled in the program, patients must meet the Medicare denition of homebound (able to leave home only with great difculty and for absences that are infrequent or of short duration). Patients are referred from a variety of sources, including emergency departments (EDs), inpatient units, and local nursing and social service agencies. PCPs visit patients on average once every 2 months but can make more-frequent urgent home visits when clinical need arises. Phone coverage is provided for after-hours care needs. PCPs coordinate all aspects of care including laboratory work, specialty referrals and nursing care. MSVD patients are primarily older (mean age 81) and female (74%), and many (34%) live alone. They have multiple chronic medical conditions (59% dementia, 25% diabetes mellitus, and 24% depression). The majority (61%) require assistance with ve or more activities of daily living, take multiple daily medications (mean 8.2),26 and can be highly burdensome to their informal caregivers.24 More than 60% of patients have documented advance directives, and at the time of referral to the program, 14% of MSVD patients are primarily receiving palliative care. Because of high disease burden, it is not uncommon for patients in the program to require inpatient hospitalization. When necessary, as part of program protocol, patients and their caregivers contact their MSVD PCP, who facilitates hospitalization at Mount Sinai Hospital (MSH). MSVD PCPs do not serve as attending doctors for the patients during their inpatient hospitalization. Whenever possible, they work with the inpatient team, but they are unable to see their patients when hospitalized and rarely are able to make timely postdischarge home visits. Intervention Description MSVD set out to build a formal transition of care program within an existing HBPC program with the following goals:
maintain continuity between PCPs and patients; improve communication between hospital providers and PCPs; improve inpatient documentation of medical comorbidities, social services needs, and advance directives; garner positive provider feedback; demonstrate nancial benets to the institution through shorter length of stay, lower cost of inpatient stay, and better documentation of patient complexity; and reduce hospital readmissions. Communication strategies such as preparing patients and caregivers for transitions, reconciling medications, giving instructions on symptoms and signs of worsening condition, and providing clear follow-up plans for tests and appointments have been identied as ways to improve care for geriatric patients.27 Adapting these strategies and protocols from previous transitional care studies,19,20,23,28,29 MSVD clinicians, researchers, and support staff crafted a multifaceted liaison program to reach the above goals. Careful consideration of the literature led the study team to devise a protocol that included an inpatient visit and a postdischarge follow-up house call. Numerous prior studies have demonstrated the cost and health outcomes benets of such a structure.19,20,22,28,30 NPs were chosen for the role to minimize costs because they are less expensive than physicians but have more extensive clinical training than nurses. Two NPs were necessary for the project to ensure continuous weekday inpatient coverage and timely postdischarge visits, even during vacation periods, but because there was not sufcient clinical work for two full-time NPs, they each provided 0.8 fulltime equivalents (FTEs) to the transitional care role; their remaining effort was used to follow a continuity panel of homebound patients. A ve-step standardized protocol was developed. 1. Initial information exchange and documentation: Each morning, the NP cross-checked hospital records with the MSVD active patient list for new hospital admissions. The ED paged the NP directly when a patient arrived in which the admission was facilitated through MSVD. The NPs were immediately notied of other new patient admissions through an electronic medical record (EMR) system developed before the implementation of the intervention that identied patients as followed by MSVD to facilitate communication between PCPs and ED staff regarding patient status. After visiting the patient, reviewing the patients MSVD EMR, and communicating with the MSVD PCP, the NP entered a standardized note (see inpatient NP progress note described below) in the hospital chart and documented the admission for the MSVD provider. 2. Initial contact with hospital staff: The inpatient NP endeavored to speak with the inpatient care team early in the patients admission. Although the NP more often initiated communication, other inpatient staff who read the inpatient NP progress note placed in the patient chart also initiated communication. Because the NPs were visiting hospitalized patients daily, they were able to maintain frequent contact with inpatient staff, especially on general medicine services in which most MSVD patients were admitted. The information communicated included the patients medical problems, reason for admission (from the PCPs perspective),
546
ORNSTEIN ET AL.
MARCH 2011VOL. 59, NO. 3
JAGS
advance directives, home medication regimen, and social service needs. 3. Follow-up: The NP saw the patient daily or every other day depending on inpatient census. All NP visits were documented in the patient hospital chart. The NP also documented pertinent details of the patients hospital course within the MSVD EMR (see inpatient communique described below) and communicated with the patients PCP regularly through electronic messaging or over the telephone. The NP also served as an advocate for patients and families when appropriate. 4. Discharge: As discharge approached, the NP again contacted the inpatient team to better understand the changes made to the patients treatment plan, the results of studies and consultations, and the postdischarge social services arranged. If there were difculties arranging the social services necessary to ensure a safe discharge, the NP interfaced with hospital social workers and case managers. When appropriate, the inpatient NP communicated to the hospital team that follow-up appointments with primary care would be arranged within MSVD. The NP documented in the MSVD EMR each patients discharge date with discharge medications and plan of care, including any change or new referrals to home care and skilled nursing services. 5. After discharge: For patients discharged home, the NP made a single postdischarge home visit as soon as possible but always within 3 weeks of discharge. During this visit, the NP performed a focused physical examination and addressed the following using a structured note: whether reasons for admission were resolved or improved, new problems, medication reconciliation, appropriateness of home care services, and adequacy of patient and caregiver education. Regularly scheduled visits by the MSVD PCPs continued as appropriate (approximately once every 68 weeks) on the broader elements of patient care. Simultaneous to the protocol development, two standardized communication tools to facilitate information exchange between inpatient and outpatient providers were developed: the inpatient NP progress note and the inpatient communique. The inpatient NP progress note was placed in the inpatient chart for all newly admitted MSVD patients. The note was formatted as a written letter from the inpatient NP to the inpatient team, and included the following critical data: identication of the patient as a MSVD patient, PCP name and contact number, NP liaison name and contact number, proxy or surrogate information, code status if known, living or home care situation, active medical problems, current medications, a short clinical summary, and NP clinical recommendations. The inpatient communique was an electronic message within the MSVD EMR that the NP used to inform the MSVD physician immediately of the admission and allow the physician to communicate any concerns (e.g., planned procedures, discharge considerations, updated family communications, medication changes) back to the NP liaison for follow-up with the inpatient team. Before full program implementation, MSVD administration met with hospitalist, house staff, social work, and ED staff to inform them of the goals of the new NP-led
intervention, what documentation and communication to expect from the NPs, and how and when they could be contacted. NP contact information was included in the hospital-wide text paging system to facilitate communication. NPs were also trained to check institutional patienttracking databases in which MSVD patients were already identied and established to ensure that all MSVD patients who were admitted could be identied.
METHODS The MSH institutional review board approved this project. Patient demographic data were extracted from the MSVD EMR. Process measures, including number of MSVD patients admitted, proportion of admitted MSVD patients followed in the inpatient setting by NPs, and discharge location, were tracked prospectively for the study. The MSH billing department provided hospital inpatient data for MSVD admissions. Project effectiveness was measured by evaluating the effect of the intervention on length of stay (LOS), case-mix index (CMI), readmission rates, and hospital nancial outcomes using a pre/post design. Changes in these outcomes were compared between the study period (September 1, 2006December 31, 2008) and the period before the start of the program (January 1, 2004May 30, 2006). Data from June through August 2006 were not included because this was the pilot period during which the program was introduced and iteratively modied. Admissions were analyzed in the following ways: number and percentage of all hospital admissions during the study period (all admissions), number of rst-time admissions for unique patients during study period (rst admission), and number and percentage of admissions occurring within 30 days of rst admission for patient during the study period (30-day readmission). Continuous hospitalizations that were billed as separate admissions but were same-day transfers between services (usually medicine and psychiatry) were removed from the analyses (n 5 69). Mean LOS and all nancial comparisons were calculated after removing outliers, dened as discharges that were more than 3 standard deviations above the mean LOS (n 5 40). Complete data were available on 97% of all MSVD admissions during the study period. Thirty-day readmission rate was dened as the number of patients discharged from MSH and readmitted within 30 days divided by the total number of MSVD patients discharged from MSH. Net revenue was dened as charges minus contractual adjustments. Expenditures assigned to each episode of care included direct and indirect care costs. Direct costs are those associated with delivery of care to the patient such as nursing, drugs, tests, and supplies. Indirect costs are those incurred by areas of a hospital that do not provide direct clinical care but are necessary for the clinical enterprise such as information technology and billing departments. Taken together, these data allow for an accounting of the contribution to margin (payment minus direct and indirect care costs) for each hospitalization. Contribution to margin represents the sum of money left after subtracting costs for direct and indirect clinical activities for the inpatient episode. This amount is the prot per case that a hospital can use to subsidize other non-revenue-generating missions or priorities.
JAGS
MARCH 2011VOL. 59, NO. 3
TRANSITIONAL CARE FOR HOSPITALIZED HOMEBOUND PEOPLE
547
The Z test for independent proportions was used to compare percentage of rst admissions that resulted in 30day readmissions between the intervention and nonintervention periods. Differences in LOS between the prestudy period and the intervention period were evaluated using the Wilcoxon rank-sum test for all admissions, rst admissions, and 30-day readmissions. Differences between CMI and inpatient costs between the prestudy period and the intervention period were evaluated using t-tests after logtransforming data. All analyses were completed using Stata version 8.1 (Stata Corp., Chicago, IL). Cost for each NP for the transitional care role was based on 0.8 FTEs, because 0.2 FTEs for each NP were dedicated to following a continuity panel. Revenue generated from NP visits was estimated based on 2008 Medicare reimbursement rates for NPs (based on an average of 26 postdischarge visits per month). Provider feedback was evaluated using focus groups with MSH inpatient physicians (n 5 5), MSH inpatient NPs (n 5 5), MSH inpatient social workers (n 5 5), and MSVD physicians (n 5 6). A question guide was developed and used as a basis for discussion. Written and audio records of these conversations were reviewed, and themes were extracted.
RESULTS During the 27-month study period, 1,464 patients were active in MSVD. The majority (63.6%) of these patients had no hospitalizations at MSH during this period. During the study period, 1,088 inpatient discharges for 532 MSVD patients occurred. Of patients hospitalized, 53% had only one admission, and 47% had repeat hospitalizations. The demographics of the patients who were hospitalized during the study period are shown in Table 1. More than 90% of all admissions occurred through the ED. Patients were admitted to 11 different services within the hospital. The majority of MSVD patients were admitted to general internal medicine services: 48% to the NonHouse Staff Hospitalist Service and 26% to the General
Table 1. Characteristics of Patients of Mount Sinai Visiting Doctors (MSVD) Discharged from Mount Sinai Hospital During the Study Period (N 5 532)
Characteristic Value
Age at rst admission, mean SD Female, n (%) Race or ethnicity, n (%) White Black Latino Other Medicaid, n (%) Number of daily medications, mean SD Weeks in MSVD at rst hospitalization, mean SD (range)
SD 5 standard deviation.
81.1 13.8 386 (72.7) 178 (33.5) 157 (29.6) 172 (32.4) 23 (4.3) 310 (58.3) 10.5 8.0 120.2 111.2 (0579)
Medicine House Staff Service. Patients were discharged with a variety of diagnoses, the most common of which were renal failure (6.5%), heart failure and shock (6.2%), simple pneumonia (5.7%), septicemia (5.3%), respiratory infection and inammation (4.7%), and chronic obstructive pulmonary disease (3.2%). Eight hundred thirty-eight (77%) hospitalizations ended with the patient returning home (Table 2). NPs saw 98% of hospitalized patients during their inpatient stay; the exceptions were patients admitted and discharged over weekends. The rst point of contact averaged 1.05 days after admission. The NP liaisons followed 12 to 15 MSVD patients daily. On average, there were 39 patients discharged from the hospital each month, ranging from 26 to 51 per month. The NP attended 75% of all family meetings conducted during patient hospitalizations (12 per week). Over the course of the study, 663 postdischarge visits were made (mean 26 per month) to patients who were discharged home (78%). Seventy-nine percent of postdischarge visits were made within 7 days of hospital discharge (mean 5 days). A postdischarge visit was not completed on a minority of patients discharged home for the following reasons: PCP saw patient after discharge (n 5 68), visiting nurse who knew the patient well saw patient (n 5 44), patient readmission (n 5 39), patient contacted over the telephone (n 5 9), patient death or discharge from MSVD (n 5 16), and refusal (n 5 3). Complete billing and LOS data were available on 97% (n 5 1,055) of the documented MSVD patient discharges during the study period. LOS for admissions that occurred during the intervention period was not signicantly shorter during the study period than before the program (n 5 1,314) (Table 3). The mean LOS was 6.15 days before the intervention and 6.45 days during the intervention period, 4.9% greater. There were no differences in mean LOS between the two time periods when examining rsttime admissions or 30-day admissions. The 30-day rehospitalization rate decreased from 16.6% to 15.8%, but this also did not reach statistical signicance. CMI was signicantly different between the control and intervention period; for all admissions, CMI increased from 1.25 to 1.35 during the intervention period (P 5.005), and for all rsttime admissions, CMI was signicantly greater during the intervention period (P 5.02). During the intervention, there were signicant increases (Po.001) in net revenue, support costs, and direct care costs. Although not statistically signicant, the median contribution to margin increased 5% from a median of $5,658 to $5,940 per admission, or $282 per admission. The annual cost to the program for the 1.6 FTE NPs was $197,000. Together, the two NPs generated $37,642 in billable services annually, representing 19% of their direct costs. Positive feedback was reported across all provider groups involved in the care of MSVD patients. For the inpatient providers, this was largely due to the inpatient NP progress note: This note is a relief [emphasis participant] when you see it. Because you know that you are going to have some real information about the patient. Information about code status, home care hours, diagnoses, and medications were cited as most critical: [It] is really helpful
548
ORNSTEIN ET AL.
MARCH 2011VOL. 59, NO. 3
JAGS
Table 2. Mount Sinai Visiting Doctors Patient Outcomes After Discharge from Mount Sinai Hospital (n 5 532 Patients)
n (%) All Admissions n 5 1,088 First Admissions n 5 532 30-Day Readmissions n 5 93
Status
Discharged home Discharged to nursing home or rehabilitation facility Discharged to hospice Death
Multiple admissions per patient included when applicable.
844 (77.6) 165 (15.2) 18 (1.7) 61 (5.6)
417 (78.4) 77 (14.5) 9 (1.7) 29 (5.5)
62 (66.7) 22 (23.6) 2 (2.2) 7 (7.5)
that they always bring in the updated list of meds and diagnoses. Information sharing between NP and hospital providers on the oor and through the progress note allowed providers to use their time more effectively: Information about home care helps with discharge planningFwe dont have to searchFwe dont have to call a hundred numbers and still get nowhere. Providers suggested that the NPs function as an important communication link that benets the providerFand ultimately the patient. As one hospitalist noted, When were really busy I have to admit Im not as good as I should be about contacting the primary [physician], but its good to know that even when Im not, [the NPs] are, . . . and even if I dont see the primary til the next day its OK because they still have an update about whats going on. MSVD providers also reported greater professional satisfaction because of time saved: They reconcile meds that we dont always do. Denitely saves us time in the eld. Facilitating discharge was another theme that emerged. Providers noted that there was greater comfort sending
chronically ill patients home because they knew that the patient would be seen within days after discharge. One hospitalist noted, I had a patient whose platelet count was lower, but I felt comfortable discharging them knowing that the NPs would follow up. Otherwise I probably would have kept her, and it was Friday and that would have been through the weekend.
DISCUSSION Despite care goals focused on patient comfort and minimizing transfers of care, homebound patients have high rates of hospitalization. Homebound patients also typically have multiple chronic medical conditions, numerous medications, difcult social situations, and complex goals of care. The intersection of complexity and high rates of hospitalization leaves homebound seniors extremely vulnerable to poor transition-of-care outcomes. As a result, MSVD sought to enhance its HBPC model by implementing a NP-led transitional care program to improve care for hospitalized homebound patients. This project, based on
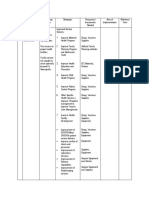
Table 3. Comparison of Hospital Readmission, Length of Stay (LOS), Case-Mix Index, and Financial Costs Before the Intervention and During the Study Period
Variable Preintervention Study Period P-Value
Total admissions, n First admissions, n 30-day readmissions, n Admissions that generated !one 30-day readmission, % Financial data LOS, mean SD All admissions First admission 30-day readmission Case-mix index, mean SD All admissions First admission 30-day readmission Net revenue, $, median (IQR) Direct care costs, $, median (IQR) Indirect cost, $, median (IQR) Contribution to margin, $, median (IQR)
1,267 628 119 16.6
1,055 527 90 15.7
.71
6.15 5.22 6.23 5.42 6.23 4.74 1.25 .88 1.19 .66 1.50 1.62 9,753 (7,94514,684) 3,245 (1,9775,834) 666.5 (3991,199) 5,658 (3,3088,408)
6.45 5.47 6.60 5.57 6.83 5.05 1.35 1.14 1.32 .91 1.25 1.24 10,807 (8,17415,832) 3,699 (2,3896,703) 740 (4661,355) 5,940 (3,5439,034)
.09 .10 .05 .005 .02 .08 o.001 o.001 o.001 .34
1,055 admissions were available using billing data representing 97% of all cases. SD 5 standard deviation; IQR 5 interquartile range.
JAGS
MARCH 2011VOL. 59, NO. 3
TRANSITIONAL CARE FOR HOSPITALIZED HOMEBOUND PEOPLE
549
well-established models19,20,23,28,29 but adapted to work within an established HBPC program and to meet the needs of patients with a wide range of diseases and high levels of dementia, has received positive feedback from inpatient and outpatient providers, who have noted that the liaison program saves time, improves inpatient management, and smoothes the discharge process. Nevertheless, for operational outcomes such as LOS and readmission rates, it was not possible to demonstrate signicant differences between the prestudy period and the intervention period. The overwhelmingly positive qualitative feedback on this project conrms the importance of a transition-of-care program within a HBPC program. Members of the inpatient teams and the MSVD PCPs reported that they believed that the program reduced errors and unnecessary inpatient procedures. The program accomplished the stated goal of communicating comprehensive information for clinically and socially complex patients. Furthermore, the presence of a liaison made inpatient providers more comfortable and condent that patients could remain home successfully after discharge. This study was unable to assess patient or caregiver satisfaction with the program directly; future studies should address this component as well as examining reduction in caregiver burden, which can increase during care transitions. Future work should also endeavor to directly measure outcomes related to errors and inpatient testing to conrm provider reports. Review of the hospitalization data generated by this study reveals a complex picture of the acute care usage of homebound people. The study showed that, although a substantial proportion of MSVD patients are hospitalized at least once per year, the majority are not. Reassuringly, a large majority of these hospitalized patients, despite being exceeding frail and having multiple comorbidities, are successfully discharged back home. A 30-day readmission rate of approximately 16% was also found, which is lower than the average rate for all Medicare patients.31 Unfortunately, the study design did not allow comparisons with prior periods to determine whether the transitional care program increases the percentage of patients discharged home. Finally, although MSVD providers report that more than 90% of hospitalizations for MSVD patients occur at MSH, patients may also be admitted to one of many New York City metropolitan area hospitals closer to their residence. These limitations hinder evaluation of the effect of the program, and future studies must address these limitations. The program failed to demonstrate a signicant decrease in LOS. The observational study design used a historical comparison group, which limited the ability to control for other hospital variables. For example, the NP project was initiated concurrent to several hospital changes such as growth of the hospitalist service with new physician staff unfamiliar with MSH, increase in ED delays, and high hospital occupancy rate, all of which may have contributed to longer LOS. During this same period, all Department of Medicine general medicine services saw an increase in LOS (6.4%) for patients aged 65 and older, greater than the 4.9% increase seen with MSVD patients during the same period of time. Similarly, although this study showed a signicant increase in the CMI and net revenue during the intervention period, which met one project goal to better document medical comorbidities and increase the billing
level allowed for the hospital, the General Medicine Service also reported a similar overall increase, reecting better documentation hospital-wide. Future evaluations must make use of concurrent controls groups to test intervention outcomes. Although the liaison program proved feasible in terms of ability of NPs to serve as an accessible interface between the PCP and inpatient care team while also providing postdischarge visits, the direct cost to a HBPC or afliated hospital of implementing such a program may limit replication. In the described model, 1.6 full-time NPs were employed to provide the transitional care roles at a total annual cost of $197,000. In the transitional care role, the NPs postdischarge visits are billable, but the inpatient communication and daily follow-up are not. As a result, direct billing by the NPs covers only 19% of their salary and benets. (Although full-time NPs at MSVD in nontransitional care roles do not cover their full expense through direct billing, they typically cover almost 50% of their cost.) Nevertheless, the hospital could recuperate the additional cost of the NP position through shorter LOS or greater contribution to margin (e.g., programs such as MSVD that generate 39 patient admissions per month, would require a mean increase in contribution of margin of $340 per admission to cover remaining NP salary expenses). Another possibility for cost neutrality would be if the program demonstrated fewer hospital readmissions. Although the current study did not nd a signicant difference in readmission rates, larger studies using nonhistoric control groups may reveal such differences. Furthermore, if readmissions are penalized, as suggested in the new healthcare legislation, it may take only a few avoided readmissions to recoup the investment in the transitional care NPs. This discussion again reveals the need to better capture the effect of this program on hospital nancial outcomes. Another possibility for improving the nancial attractiveness of the program would be to use lower-cost physician assistants or registered nurses. NPs were chosen for this project based on the premise that the role required an experienced and high-level clinician given the complex medical comorbidities of homebound patients. Finally, although this project used 1.6 FTEs to assure continuous weekday inpatient coverage and timely postdischarge visits, a more-exible structure for the liaison role (ability to make more routine outpatient visits to HBPC patients during periods in which there were fewer hospitalized patients to manage) could allow for more direct billing and thus generate greater revenue. Although protocols for successful transitional care programs19,23,24 call for visiting patients at home within 48 hours of discharge, this program saw patients within an average of 5 days, with 21% of patients seen more than 1 week after discharge. Although it is recommended that new programs aim to see patients within 48 hours of discharge, this program did not have the stafng to see all patients within 48 hours because the NPs simultaneously did inpatient work and postdischarge care and were restricted to a schedule of 5 days per week. Given that, in this study, fewer than 5% of patients discharged home were readmitted before they were able to be seen in a postdischarge visit, the effect of quicker postdischarge follow-up on readmissions would have been modest. Furthermore, the stafng
550
ORNSTEIN ET AL.
MARCH 2011VOL. 59, NO. 3
JAGS
necessary to accomplish this would have worsened an already suboptimal cost prole. Because a main component of this project was to disseminate up-to-date information, the accuracy of the information to be shared is critical. MSVD was able to provide accurate information to inpatient providers by using a live and remotely accessible EMR (even though the MSVD EMR was not the same one used within the hospital). Without this infrastructure, implementing the liaison program would have been substantially more difcult. Although the use of EMR systems is becoming the standard of care in larger institutions, smaller home-based primary care programs without EMRs will be less effective in their ability to continuously share up-to-date information. Nevertheless, even without an integrated EMR, an inpatient liaison could still provide inpatient staff with a clinical snap-shot including advance directives, current medications, and home care services, which the ndings suggest were invaluable. Similarly, if programs are not afliated with a medical center or do not routinely admit patients to a limited number of hospitals, transitional care programs such as this one cannot be efciently implemented. Overall, the Inpatient NP Transitional Care Project is an important addition to the HBPC model of care. The program has received positive feedback from providers of all disciplines caring for the hospitalized homebound people by ensuring the accurate and timely transfer of information and in-person availability of a member of the HBPC team for patient advocacy, representation in family meetings, and assistance with discharge planning. The program has allowed the MSVD comprehensive care model to extend to the highest-risk patients (those who are hospitalized) and facilitate timely, patient-centered care decisionmaking with the inpatient care teams. Given the large amount of unreimbursed costs of this program, future work investigating outcomes such as change in medication errors, greater patient satisfaction, and less caregiver burden will be necessary to further justify the upfront investment necessary to sustain a transitional care program serving hospitalized homebound people.
REFERENCES
1. Boling PA. Care transitions and home health care. Clin Geriatr Med 2009; 25:135148. 2. American Academy of Home Care Physicians. AAHCP Public Policy Statement 2005 [on-line]. Available at http://www.aahcp.org/public_policy_2005. pdf. 2009 Accessed January 12, 2009. 3. Kellogg FR, Brickner PW. Long-term home health care for the impoverished frail homebound aged: A twenty-seven-year experience. J Am Geriatr Soc 2000;48:10021011. 4. Desai NR, Smith KL, Boal J. The positive nancial contribution of home-based primary care programs: The case of the Mount Sinai Visiting Doctors. J Am Geriatr Soc 2008;56:744749. 5. Reed RL, Pearlman RA, Buchner DM. Risk factors for early unplanned hospital readmission in the elderly. J Gen Intern Med 1991;6:223 228. 6. Corrigan JM, Martin JB. Identication of factors associated with hospital readmission and development of a predictive model. Health Serv Res 1992;27:81101. 7. Manian FA. Whither continuity of care? N Engl J Med 1999;340:13621363. 8. Meredith S, Feldman PH, Frey D et al. Possible medication errors in home healthcare patients. J Am Geriatr Soc 2001;49:719724. 9. Kripalani S, LeFevre F, Phillips CO et al. Decits in communication and information transfer between hospital-based and primary care physicians: Implications for patient safety and continuity of care. JAMA 2007;297: 831841. 10. Roy CL, Poon EG, Karson AS et al. Patient safety concerns arising from test results that return after hospital discharge. Ann Intern Med 2005;143: 121128. 11. Moore C, McGinn T, Halm E. Tying up loose ends: Discharging patients with unresolved medical issues. Arch Intern Med 2007;167:13051311. 12. Anderson M, Helms L. Communication between continuing care organizations. Res Nurs Health 1995;18:4957. 13. Bull MJ, Hansen HE, Gross CR. Predictors of elder and family caregiver satisfaction with discharge planning. J Cardiovasc Nurs 2000;14:76 87. 14. Coleman EA, Mahoney E, Parry C. Assessing the quality of preparation for posthospital care from the patients perspective: The care transitions measure. Med Care 2005;43:246255. 15. Pantilat SZ, Lindenauer PK, Katz PP et al. Primary care physician attitudes regarding communication with hospitalists. Am J Med 2001;111: 15S20S. 16. Isaac DR, Gijsbers AJ, Wyman KT et al. The GP-hospital interface: Attitudes of general practitioners to tertiary teaching hospitals. Med J Aust 1997;166: 912. 17. Wilson S, Ruscoe W, Chapman M et al. General practitioner-hospital communications: A review of discharge summaries. J Qual Clin Pract 2001; 21:104108. 18. Fair JF. Hospital discharge and death communications. Br J Hosp Med 1989; 42:5961. 19. Naylor MD, Brooten D, Campbell R et al. Comprehensive discharge planning and home follow-up of hospitalized elders: A randomized clinical trial. JAMA 1999;281:613620. 20. Rich MW, Beckham V, Wittenberg C et al. A multidisciplinary intervention to prevent the readmission of elderly patients with congestive heart failure. N Engl J Med 1995;333:11901195. 21. Neff DF, Madigan E, Narsavage G. APN-directed transitional home care model: Achieving positive outcomes for patients with COPD. Home Healthcare Nurs 2003;21:543550. 22. Naylor M, Brooten D, Jones R et al. Comprehensive discharge planning for the hospitalized elderly. A randomized clinical trial. Ann Intern Med 1994; 120:9991006. 23. Naylor MD, Brooten DA, Campbell RL et al. Transitional care of older adults hospitalized with heart failure: A randomized, controlled trial. J Am Geriatr Soc 2004;52:675684. 24. Coleman EA, Parry C, Chalmers S et al. The care transitions intervention: Results of a randomized controlled trial. Arch Intern Med 2006;166:1822 1828. 25. Smith KL, Ornstein K, Soriano T et al. A multidisciplinary program for delivering primary care to the underserved urban homebound: Looking back, moving forward. J Am Geriatr Soc 2006;54:12831289. 26. Kronish I, Federman A, Morrison R et al. Medication utilization in an urban homebound population. J Gerontol A Biol Sci Med Sci 2006;61A: 411415. 27. Coleman EA. Falling through the cracks: Challenges and opportunities for improving transitional care for persons with continuous complex care needs. J Am Geriatr Soc 2003;51:549555.
ACKNOWLEDGMENTS We would like to recognize all the faculty and staff of MSVD who assisted with the design and implementation of this project. Conict of Interest: The editor in chief has reviewed the conict of interest checklist provided by the authors and has determined that the authors have no nancial or any other kind of personal conicts with this paper. KO, TS, and TLC were employees of MSVD, and KS was a resident in the Division of Internal Medicine at the time of this study. Direct service support for this project was provided in part by the Fan Fox and Leslie R. Samuels Foundation. Author Contributions: Katherine Ornstein, Kristofer Smith, and Theresa Soriano: study concept and design, analysis and interpretation of data and preparation of manuscript. Dinah Foer and Tereza Lopez-Cantor: acquisition of subjects and data and preparation of manuscript. Sponsors Role: None.
JAGS
MARCH 2011VOL. 59, NO. 3
TRANSITIONAL CARE FOR HOSPITALIZED HOMEBOUND PEOPLE
551
28. Neff DE, Madigan E, Narsavage G. APN-Directed Transitional Care Model: Achieving positive outcomes for patients with COPD. Home Healthcare Nurs 2003;21:543550. 29. Brand CA, Jones CT, Lowe AJ et al. A transitional care service for elderly chronic disease patients at risk of readmission. Aust Health Rev 2004;28: 275284.
30. Coleman EA, Smith JD, Frank JC et al. Preparing patients and caregivers to participate in care delivered across settings: The Care Transitions Intervention. J Am Geriatr Soc 2004;52:18171825. 31. Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med 2009;360: 14181428.
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Issue Brief - Innovation in Hospital FinancingDocument3 pagesIssue Brief - Innovation in Hospital FinancingAnonymous UpWci5No ratings yet
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Microeconomics: Assignment 1: Moving Less, Retiring LaterDocument6 pagesMicroeconomics: Assignment 1: Moving Less, Retiring LaterRuhi UppalNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Dayton Reinsurance LetterDocument1 pageDayton Reinsurance LetterdhmontgomeryNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (894)
- UIIC ClaimFormDocument2 pagesUIIC ClaimFormkarthikvel80No ratings yet
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- White Paper - Pathway To Commercialization For An in Vitro Diagnostic (IVD) in The USDocument4 pagesWhite Paper - Pathway To Commercialization For An in Vitro Diagnostic (IVD) in The USKelly CampenNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Edesign - Hospital (Key)Document3 pagesEdesign - Hospital (Key)John Nielven D Epis0% (1)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Geometrixs Architects and Engineers Company ProfileDocument9 pagesGeometrixs Architects and Engineers Company ProfileRaman NagarajaNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- Enlc 557 Strategic Management Final Paper Steven ZhangDocument14 pagesEnlc 557 Strategic Management Final Paper Steven Zhangapi-534987967No ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (587)
- Application For Reinstatement FormDocument2 pagesApplication For Reinstatement FormChristian D. Orbe100% (3)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (265)
- Prosecuting Medicaid Fraud in Texas: Senate Finance Sub-Committee On Medicaid February 15, 2011Document18 pagesProsecuting Medicaid Fraud in Texas: Senate Finance Sub-Committee On Medicaid February 15, 2011GovtfraudlawyerNo ratings yet
- Scheduling Procedures Cath LabDocument3 pagesScheduling Procedures Cath Labrajneeshchd100% (1)
- Final Video Brief 2Document7 pagesFinal Video Brief 2api-354943808No ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Executive Director Senior Center in Tallahassee FL Resume Rodney BigelowDocument2 pagesExecutive Director Senior Center in Tallahassee FL Resume Rodney BigelowRodneyBigelowNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The Role of Electronic Health Records in Chronic Disease Management For A Sustainable Health Care SystemDocument16 pagesThe Role of Electronic Health Records in Chronic Disease Management For A Sustainable Health Care SystemPartnership to Fight Chronic DiseaseNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- Zilveren Kruis Application FormDocument2 pagesZilveren Kruis Application FormwangchanghuiNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Latin Terms and Abbreviations Used in PrescriptionDocument3 pagesLatin Terms and Abbreviations Used in PrescriptionRhen DimalibotNo ratings yet
- EDGE Server Data Dictionary March ReleaseDocument54 pagesEDGE Server Data Dictionary March ReleasecnusistaNo ratings yet
- Special Election Endorsement Edition - AFSCME 67 NewsletterDocument8 pagesSpecial Election Endorsement Edition - AFSCME 67 NewsletterAFSCME 67No ratings yet
- Residential Nursing Home ProposalDocument22 pagesResidential Nursing Home Proposalapi-324136209No ratings yet
- From Innovation To Implementation: Work Group Report From The Office of Health Innovation and TransformationDocument79 pagesFrom Innovation To Implementation: Work Group Report From The Office of Health Innovation and Transformationsalad1No ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- Descriptive Statistics Measures ChapterDocument5 pagesDescriptive Statistics Measures ChapterChanime Meih100% (1)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2219)
- AOP Form 3Document4 pagesAOP Form 3Ferzada SajiranNo ratings yet
- Mark E. Locklear ResumeDocument5 pagesMark E. Locklear ResumeMark LocklearNo ratings yet
- Running Head: Health Information Technology 1Document12 pagesRunning Head: Health Information Technology 1api-469824583No ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Covered California Getting Covered Fact Sheet EnglishDocument3 pagesCovered California Getting Covered Fact Sheet Englishapi-206634556No ratings yet
- Diagnosis Pulmonary NodulesDocument2 pagesDiagnosis Pulmonary NodulesAlejandro Marti100% (1)
- SIIA - VijiDocument186 pagesSIIA - VijiEmily James100% (1)
- Staff Directory SDocument12 pagesStaff Directory SthanosboukouNo ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (119)
- Phil HealthDocument27 pagesPhil HealthRochelle PanganNo ratings yet
- Study Chapter: GlossaryDocument8 pagesStudy Chapter: GlossaryKNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)