Professional Documents
Culture Documents
ER Handouts
Uploaded by
Ronald Cszar Fabian VillanoOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
ER Handouts
Uploaded by
Ronald Cszar Fabian VillanoCopyright:
Available Formats
Editors: Nettina, Sandra M.
Title: Lippincott Manual of Nursing Practice, 9th Edition Copyright 2010 Lippincott Williams & Wilkins > Table of Contents > Part Two - Medical-Surgical Nursing > Unit XII - Emergency Nursing > Chapter 35 - Emergent Conditions
Chapter 35 Emergent Conditions BASIC APPROACH TO EMERGENCY CARE
Emergency care can be defined as the episodic and crisisoriented care provided to patients with conditions ranging from minor to serious or life-threatening injuries or illnesses. The philosophy of emergency care includes the concept that an emergency is whatever the patient or family considers it to be. Emergency nursing is a unique practice that deals with unstable, undiagnosed patients usually presenting unexpectedly. See Standards of Care Guidelines. EMERGENCY ASSESSMENT A systematic approach to the assessment of an emergency patient is essential. Usually, the most dramatic injury is not the most serious. The primary and secondary surveys provide the emergency nurse with a methodical approach to help identify and prioritize patient needs. Primary Assessment The initial, rapid, ABCD (airway, breathing, and circulation, as well as neurologic disability resulting from spinal cord or head injuries) assessment of the patient is meant to identify life-threatening problems. If conditions are identified that present an immediate threat to life, appropriate interventions are required before proceeding to the secondary assessment. STANDARDS OF CARE GUIDELINES Emergency Assessment and Intervention When a patient presents with a potentially life-threatening condition, proceed swiftly with the following: Remove the patient from potential source of danger, such as live electric current, water, or fire. Determine whether patient is conscious. Assess airway, breathing, and circulation in systematic manner. Assess pupillary reaction and level of responsiveness to voice or touch as indicated. If the patient is unconscious or has sustained a significant head injury, assume there is a spinal cord injury and ensure proper handling. Undress the patient to assess for wounds and skin lesions as indicated. Immediate intervention is needed for such conditions as compromised airway, respiratory arrest, compromised respirations, cardiac arrest, and profuse bleeding. Provide emergency airway management, cardiopulmonary resuscitation, and measures to control hemorrhage as needed. Call for help as soon as possible. Assist with transport and further assessment and care as indicated. This information should serve as a general guideline only. Each patient situation presents a unique set of clinical factors and requires nursing judgment to guide care, which may include additional or alternative measures and approaches. AAirway: Does the patient have an open airway? Is the patient able to speak? Check for airway obstructions such as loose teeth, foreign objects, bleeding, vomitus or other secretions. Immediately treat anything that compromises the airway. BBreathing: Is the patient breathing? Assess for equal rise and fall of the chest (check for bilateral breath sounds), respiratory rate and pattern, skin color, use of accessory muscles, adventitious breath sounds, integrity of the chest wall, and position of the trachea. All major trauma patients require supplemental oxygen via a nonrebreather mask. CCirculation: Is circulation in immediate jeopardy? Can you palpate a central pulse? What is the quality (strong, weak, slow, rapid)? Is the skin warm and dry? Is the skin color normal? Obtain a blood pressure ([BP]; in both arms if chest trauma or dissecting aortic aneurysm is suspected). DDisability: Assess level of consciousness and pupils (a more complete neurologic survey will be completed in the secondary survey). Assess level of consciousness using the AVPU scale: o AIs the patient alert? o VDoes the patient respond to voice? o PDoes the patient respond to painful stimulus? o UThe patient is unresponsive even to painful stimulus.
Secondary Assessment The secondary assessment is a brief, but thorough, systematic assessment designed to identify all injuries. The steps include Expose/environmental control, Full set of vital signs/Five interventions/Facilitate family presence and Give comfort measures. Expose/environmental control: It is necessary to remove the patient's clothing in order to identify all injuries. You must then prevent heat loss by using warm blankets, overhead warmers, and warmed I.V. fluids unless induced hypothermia is indicated. Full set of vital signs:
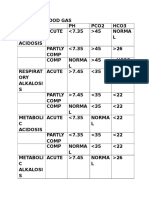
o Obtain a full set of vital signs including BP, heart rate, respiratory rate, and temperature. o As stated previously, obtain BP in both arms if chest trauma or dissecting aortic aneurysm is suspected. o Institute continuous cardiac monitoring. o Assess Glasgow Coma Scale (GCS) (see page 488) and pain score. Five interventions: o Vascular access o Pulse oximetry to measure the oxygen saturation; consider capnography to measure end-tidal carbon dioxide (EtCO2); noninvasive ultrasonic cardiac output monitor (USCOM); and electrocardiogram (ECG) o Indwelling urinary catheter (do not insert if you note blood at the meatus, blood in the scrotum, or if you suspect a pelvic fracture) o Gastric tube (if there is evidence of facial fractures, insert the tube orally rather than nasally) o Laboratory studies frequently include type and cross-matching, complete blood count (CBC), urine drug screen, blood alcohol, electrolytes, prothrombin time (PT) and partial thromboplastin time (PTT), arterial blood gas (ABG), and pregnancy test if applicable Facilitate family presence: It is important to assess the family's needs. If any member of the family wishes to be present during the resuscitation, it is imperative to assign a staff member to that person to explain what is being done and offer support. Give comfort measures: These include verbal reassurances as well as pain management as appropriate. Do not forget to give comfort measures to the family during the resuscitation process.
History Obtain prehospital information from emergency personnel, patient, family, or bystanders using the mnemonic MIVT. o MMechanism of injury: It is helpful to understand the mechanism of injury to anticipate probable injuries. It is particularly helpful in motor vehicle accidents to know such information as external and internal damage to the car and the period of time elapsed before the patient received medical attention. o IInjuries sustained or suspected: Ask prehospital personnel to list any injuries that they have identified. o VVital signs: What were the prehospital vital signs? o TTreatment: What treatment did the patient receive before arriving at the hospital and what was patient's response to those interventions? If the patient is conscious, it is essential to ask him what happened. How did the accident occur? Why did it happen? A fall, for example, may not be a simple fallperhaps the patient blacked out and then fell. If the patient is conscious and time permits, explore the chief complaint through the PQRST mnemonic. PProvokes, Palliates, Precipitates QQuality RRegion, Radiates SSeverity, associated Symptoms TTiming (onset, duration) Obtain past medical history from the patient or a family member or friend, including age, medical/surgical history, current medications, use of any illicit drugs, allergies, last menstrual period, last meal, and last tetanus shot.
NURSING ALERT To obtain a good descriptive history, do not ask questions that can be answered with a yes or no. Head-to-Toe Assessment The head-to-toe assessment begins with assessment of the patient's general appearance, including body position or any guarding or posturing. Work from the head down, systematically assessing the patient one body area at a time. Head and face o Inspect for any lacerations, abrasions, contusions, avulsions, puncture wounds, impaled objects, ecchymosis, or edema. o Palpate for crepitus, crackling, or bony deformities. Chest o Inspect for breathing effectiveness, paradoxical chest wall movement, disruptions in chest wall integrity. o Auscultate for bilateral breath sounds and adventitious breath sounds. o Palpate for bony crepitus or deformities. Abdomen/flanks o Inspect for lacerations, abrasions, contusions, avulsions, puncture wounds, impaled objects, ecchymosis, edema, scars, eviscerations, or distention. o Auscultate for the presence of bowel sounds. o Palpate for rigidity, guarding, masses, or areas of tenderness. Pelvis/perineum o Inspect for lacerations, abrasions, contusions, avulsions, puncture wounds, impaled objects, ecchymosis, edema, or scars. Look for blood at the urinary meatus. Look for priapism (which could indicate spinal cord injury). o Palpate for pelvic instability and anal sphincter tone. Extremities o Inspect skin color and temperature. Look for signs of injury and bleeding. Does the patient have movement and sensation of all extremities? o Palpate peripheral pulses, any bony crepitus, or areas of tenderness.
Posterior surfacesutilizing help, logroll the patient in order to: o Inspect for possible injuries. o Palpate the vertebral column and all areas for tenderness.
_________________________________________________________________________________________________ Head to Toe Assessment (According to Lippincott Manual 7th Edition) 1. General appearance a. Position/posture/gait b. Level of consciousness restlessness is a danger signal c. Behavior and degree of distress d. Cooperation e. Skin condition and color 2. Head/ Scalp a. Bleeding b. Deformity and Depressions c. Facial symmetry 3. Ears a. Blood b. Clear fluid (Cerebrospinal fluid [CSF]) c. Battles sign (Bluish discoloration of the mastoid area) 4. Eyes a. Pupil size and reaction to light b. Extraocular motions c. Orbital ecchymosis d. Gross Vision e. Conjunctivae examine for pallor or cyanosis 5. Nose a. Blood b. Clear (CSF) 6. Mouth a. Missing teeth b. Cyanosis of the lips c. Foreign material/vomitus 7. Neck a. Tracheal Deviation b. Jugular distention c. Tenderness 8. Chest a. Symmetry b. Tenderness/pain c. Ecchymosis d. Subcutaneous emphysema e. Soft tissue injuries f. Breath sounds g. Heart sounds 9. Abdomen a. Distention/rigidity b. Tenderness/pain c. Guarding d. Bowel sounds e. Soft tissue injuries 10. Pelvis a. Stability b. Tenderness 11. Genitalia a. Bleeding b. Wounds/trauma c. Priapism d. Rectal tone e. Pain 12. Extremities a. Pain b. Deformity and bruises c. Pulses d. Sensation and strength e. Soft tissue injury f. Capillary refill g. Edema 13. Posterior (observe cervical spine precautions in trauma patients) a. Soft tissue injury b. Spinal tenderness c. Pain or tenderness
Focused Assessment 1. A more detailed assessment of deviations from normal or problems identified in the secondary survey. 2. If more then one focused assessment is necessary, any problem identified with the pulmonary system, cardiovascular system, or neurologic system should be assessed FIRST. _______________________________________________________________________________________________ Focused Assessment Any injuries that were identified during the primary and secondary surveys require a detailed assessment, which will typically include a team approach and radiographic studies. EMERGENCY TRIAGE Triage is a French verb meaning to sort. Emergency triage is a subspecialty of emergency nursing, which requires specific, comprehensive educational preparation. Patients entering an emergency department (ED) are greeted by a triage nurse, who will perform a rapid evaluation of the patient to determine a level of acuity or priority of care. The triage nurse will assess the patient's chief complaint; general appearance; ABCD; environment; limited history; and comorbidities. Thus, the primary role of the triage nurse is to make acuity and disposition decisions and set priorities while maintaining an awareness for potentially violent or communicable disease situations. Secondary triage decisions involve the initiation of triage extended practices. Priorities of Care and Triage Categories Standardized 5-level triage systems, such as the Australasian Triage Scale (ATS), Canadian Triage and Acuity Scale (CTAS), and the Emergency Severity Index (ESI), have been developed and proven through research to possess utility, validity, reliability, and safety. All three systems utilize similar time frames and are evidence based (the Manchester Triage System [MTS] is a consensus-based algorithm approach, which utilizes longer time frames). Triage Level 1Immediately Life-threatening or Resuscitation Conditions requiring immediate clinician assessment. Any delay in treatment is potentially life- or limb-threatening. Includes conditions such as: o Airway or severe respiratory compromise. o Cardiac arrest. o Severe shock. o Symptomatic cervical spine injury. o Multisystem trauma. o Altered level of consciousness (LOC) (GCS < 10). o Eclampsia. o Extremely violent patient. Triage Level 2Imminently Life-threatening or Emergent Conditions requiring clinician assessment within 10 to 15 minutes of arrival. Conditions include: o Head injuries. o Severe trauma. o Lethargy or agitation. o Conscious overdose. o Severe allergic reaction. o Chemical exposure to the eyes. o Chest pain. o Back pain. o GI bleed with unstable vital signs. o Stroke with deficit. o Severe asthma. o Abdominal pain in patients older than age 50. o Vomiting and diarrhea with dehydration. o Fever in infants younger than age 3 months. o Acute psychotic episode. o Severe headache. o Any pain greater than 7 on a scale of 10. o Any sexual assault. o Any neonate age 7 days or younger. Triage Level 3Potentially Life-threatening/Time Critical or Urgent Conditions requiring clinician assessment within 30 minutes of arrival. Conditions include: o Alert head injury with vomiting. o Mild to moderate asthma. o Moderate trauma. o Abuse or neglect. o GI bleed with stable vital signs. o History of seizure, alert on arrival. Triage Level 4Potentially Life-serious/Situational Urgency or Semi-urgent Conditions requiring clinician assessment within 1 hour of arrival. Conditions include: o Alert head injury without vomiting.
o Minor trauma. o Vomiting and diarrhea in patient older than age 2 without evidence of dehydration. o Earache. o Minor allergic reaction. o Corneal foreign body. o Chronic back pain. Triage Level 5Less/Non-urgent Conditions requiring clinician assessment within 2 hours of arrival. Conditions include: o Minor trauma, not acute. o Sore throat. o Minor symptoms. o Chronic abdominal pain. PSYCHOLOGICAL CONSIDERATIONS Serious illness or trauma is an insult to physiologic and psychological homeostasis; it requires physiologic and psychological healing. Approach to the Patient a. Understand and accept the basic anxieties of the acutely ill or traumatized patient. Be aware of the patient's fear of death, disablement, and isolation. o Personalize the situation as much as possible. Speak, react, and respond in a warm manner. o Give explanations on a level that the patient can grasp. An informed patient can cope with psychological/physiologic stress in a more positive manner. o Accept the rights of the patient and family to have and display their own feelings. o Maintain a calm and reassuring mannerhelps the emotionally distressed patient or family to mobilize their psychological resources. o Include the patient's family or significant others. b. Understand and support the patient's feelings concerning loss of control (emotional, physical, and intellectual). c. Treat the unconscious patient as if conscious. Touch, call by name, and explain every procedure that is done. Avoid making negative comments about the patient's condition. o Orient the patient to person, time, and place as soon as she is conscious; reinforce by repeating this information. o Bring the patient back to reality in a calm and reassuring way. o Encourage the family, when possible, to orient the patient to reality. d. Be prepared to handle all aspects of acute illness and trauma; know what to expect and what to do. This alleviates the nurse's anxieties and increases the patient's confidence. Approach to the Family Inform the family where the patient is, and give as much information as possible about the treatment she is receiving. Consider allowing a family member to be present during the resuscitation. Assign a staff person to the family member to explain procedures and offer comfort. Recognize the anxiety of the family and allow them to talk about their feelings. Acknowledge expressions of remorse, anger, guilt, and criticism. Allow the family to relive the events, actions, and feelings preceding admission to the ED. Deal with reality as gently and quickly as possible; avoid encouraging and supporting denial. Assist the family to cope with sudden and unexpected death. Some helpful measures include the following: o Take the family to a private place. o Talk to all of the family together so they can mourn together. o Assure the family that everything possible was done; inform them of the treatment rendered. o Avoid using euphemisms such as passed on. Show the family that you care by touching, offering coffee. o Allow family to talk about the deceasedpermits ventilation of feelings of loss. Encourage family to talk about events preceding admission to the ED. o Encourage family to support each other and to express emotions freelygrief, loss, anger, helplessness, tears, disbelief. o Avoid volunteering unnecessary information (eg, patient was drinking). o Avoid giving sedation to family membersmay mask or delay the grieving process, which is necessary to achieve emotional equilibrium and prevent prolonged depression. o Be cognizant of cultural and religious beliefs and needs. o Encourage family members to view the body if they wishto do so helps to integrate the loss (cover mutilated areas). Prepare the family for visual images and explain any legal requirements. Go with family to see the body. Show acceptance of the body by touching to give family permission to touch and talk to the body. Spend a few minutes with the family, listening to them. Allow the family some private time with the body, if appropriate. Encourage the ED staff to discuss among themselves their reaction to the event to share intense feelings for review and for group support. PAIN MANAGEMENT
Pain is an unpleasant sensory and emotional experience associated with actual or potential tissue damage and is also associated with significant morbidity. Pain inhibits immune function and has detrimental effects on cardiovascular, respiratory, GI, and other body systems. Over 60% of patients report pain on arrival at ED, making pain the most common patient complaint. It is imperative to adequately assess, monitor, and relieve pain in the ED. Significant evidence-practice gaps have been identified with underestimation and undertreatment of pain, despite available clinical practice guidelines. Pain may be somatic or visceral, acute or chronic, or centrally or peripherally generated. Primary Assessment 1. ABCD 2. Evaluate pain using the PQRST mnemonic 3. Assess pain score using a pain rating tool, such as the verbal rating scale (VRS), numeric rating scale (NRS), visual analogue scale (VAS), Wong-Baker FACES pain scale (see page 1443), FLACC (faces, legs, activity, cry, and consolability) behavioral scale, or Abbey pain scale. Primary Interventions Establish a supportive relationship with the patient. Respect the patient's response to pain and its management. Educate the patient regarding methods of pain relief, preventive measures, and expectations. Administer pharmaceutical and nonpharmaceutical pain control. Monitor the patient's response to and effectiveness of treatment. NURSING ALERT Pain relief is a moral, humane, and physiologic imperative.
CARDIOPULMONARY RESUSCITATION AND AIRWAY MANAGEMENT
Cardiopulmonary resuscitation (CPR) is a technique of basic life support for the purpose of oxygenating the brain and heart until appropriate, definitive medical treatment can restore normal heart and ventilatory action. Management of foreign-body airway obstruction or cricothyroidotomy may be necessary to open the airway before CPR can be performed. Recent recommendations for compression-only resuscitation do not apply to most situations where the nurse is encountering the patient with cardiopulmonary arrest. The International Liaison Committee of Resuscitation (ILCOR) recommended compression-only resuscitation in 2006 and the American Heart Association (AHA) did so in 2008where a rescuer is either untrained or unwilling to perform CPR. Therefore, these rescuers are directed by emergency services to perform compressions only at a rate of 100/minute. The rationale is that any attempt at resuscitation is better than none. However, this method is not considered effective in children, cases of drowning, airway obstruction, in-hospital attempts, and attempts beyond 3 to 4 minutes of arrest. CARDIOPULMONARY RESUSCITATION PROCEDURE GUIDELINES 35-1 Cardiopulmonary Resuscitation EQUIPMENT Arrest board Oral airway Bag and mask device Oxygen I.V. setup Defibrillator Emergency cardiac drugs Cardiac monitor Electrocardiograph machine Intubation equipment Suction
PROCEDURE Nursing Action Responsiveness/airway 1. Determine unresponsiveness: tap or gently shake patient while shouting, Are you okay? 2. Activate emergency medical service (call local emergency telephone number or 911) if outside facility. 3. Place the patient supine on a firm, flat surface. Kneel at the level of the patient's shoulders. If he has suspected head or neck trauma, he should not be moved unless it is absolutely necessary (eg, at the site of an accident, fire, or other unsafe environment). 4. Open the airway. a. Head-tilt/chin-lift maneuver: Place one hand on the patient's forehead and apply firm backward pressure with the palm to tilt the head back. Then, place the fingers of the other hand under the bony part of the lower jaw near the chin and lift up to bring the jaw forward and the teeth almost to occlusion. Rationale This will prevent injury from attempted resuscitation on a person who is not unconscious.
This enables the rescuer to perform rescue breathing and chest compression without changing position.
a. In the absence of sufficient muscle tone, the tongue or epiglottis will obstruct the pharynx and larynx. This supports the jaw and helps tilt the head back.
b. Jaw-thrust maneuver: Grasp the angles of the patient's
lower jaw and, lifting with both hands, one on each side, displace the mandible forward, while tilting the head backward. Breathing 1. Place ear over patient's mouth and nose while observing the chest, look for the chest to rise and fall, listen for air escaping during exhalation, and feel for the flow of air. 2. Perform rescue breathing by mouth-to-mouth, using a ventilation barrier device. While keeping the patient's airway open, pinch the nostrils closed using the thumb and index finger of the hand you have placed on his forehead. Take a deep breath, open your mouth wide, and place it around the outside edge of the patient's mouth to create an airtight seal. Ventilate the patient with two full breaths (each lasting 1 second), taking a breath after each ventilation. If the initial ventilation attempt is unsuccessful, reposition the patient's head and repeat rescue breathing. Circulation Determine presence or absence of pulse. 1. While maintaining head-tilt with one hand on the patient's fore\head, palpate the carotid or femoral pulse for no more \than 10 seconds. If pulse is not palpable, start external chest compressions. External Chest Compressions This procedure consists of serial, rhythmic applications of pressure over the lower half of the sternum. 1. Kneel as close to side of patient's chest as possible. Place the heel of one hand on the lower half of the sternum, 1 inches (3.8 cm) from the tip of the xiphoid. The fingers may either be extended or interlaced but must be kept off the chest. 2. While keeping your arms straight, elbows locked, and shoulders positioned directly over your hands, quickly and forcefully depress the lower half of the patient's sternum straight down one-third the depth of the chest or, 1-2 inches (3.8-5 cm). 3. Release the external chest compression completely and allow the chest to return to its normal position after each compression. The time allowed for release should equal the time required for compression. Do not lift your hands from the patient's chest or change position. 4. For cardiopulmonary resuscitation (CPR) performed by one rescuer, do 30 compressions at a rate of 100 per minute and then perform two ventilations; reevaluate the patient. After four cycles of 30 compressions and two breaths each, check the pulse; check again every few minutes thereafter. Minimize interruptions of chest compressions. 5. For CPR performed by two rescuers, the compression rate is 100 per minute. The compression-ventilation ratio is 30:2. Once an advanced airway is in place, the compressing rescuer should give continuous chest compressions at a rate of 100 without pauses for ventilation. The rescuer delivering ventilation provides 8 to 10 breaths per minute. 6. While resuscitation proceeds, simultaneous efforts are made to obtain and use special resuscitation equipment to manage breathing and circulation and provide definitive care. 7. Utilize the automated external defibrillator (AED) as soon as possible. Special circumstances affecting use of AEDs include: a. AEDs should not be used on children younger than age 8. b. The victim should not be lying in water when using an AED. Make sure the patient's chest is dry before attaching the AED.
b. The jaw-thrust technique without head tilt is the safest method for opening the airway in the presence of suspected neck injury.
To determine presence or absence of spontaneous breathing.
This prevents air from escaping from the patient's nose. Adequate ventilation is indicated by seeing the chest rise and fall, feeling the air escape during ventilation, and hearing the air escape during exhalation.
Cardiac arrest is recognized by pulselessness in the large arteries of the unconscious, breathless patient. If the patient has a palpable pulse, but is not breathing, initiate rescue breathing at rate of 12 times per minute (once every 5 seconds) after two initial breaths.
The long axis of the heel of the rescuer's hand should be placed on the long axis of the sternum so that the main force of the compression is on the sternum, thereby decreasing the chance of rib fracture.
Release of the external chest compression allows blood flow into the heart.
Rescue breathing and external chest compressions must be combined. Check for return of carotid pulse. If absent, resume CPR with two ventilations followed by compressions. For CPR performed by health professionals, mouth-to-mask ventilation is an acceptable alternative to rescue breathing.
Definitive care includes defibrillation, pharmacotherapy for dysrhythmias and acid-base disturbances, and ongoing monitoring and skilled care in an intensive care unit. The American Heart Association supports the use of AEDs in public places as well as medical centers. a. The default energy level of AEDs is too high for children younger than age 8.
b. Using an AED when patients are wet or lying in
water may result in burns and shocks to the rescuer.
c. Do not place the AED electrode directly over an implanted pacemaker. d. Remove any transdermal medication patches from the patient before using the AED. 8. The four basic steps used in AED operation are: a. Turn the power on. b. Attach the AED pads to the patient's chest, using the diagrams on the pads to show you exactly where to place them. c. Analyze the patient's rhythm by pushing the button on the AED labeled ANALYZE. During this time, no one should touch the patient. d. Charge the AED and deliver the shock if indicated by the AED. Make sure that no one is touching the patient. Push the shock button; the AED will provide visual and voice prompts to tell you what to do. Indications 1. Cardiac arrest o Ventricular fibrillation o Ventricular tachycardia o Asystole o Pulseless electrical activity 2. Respiratory arrest o Drowning o Stroke o Foreign-body airway obstruction o Smoke inhalation o Drug overdose o Electrocution/injury by lightning o Suffocation o Accident/injury o Coma o Epiglottitis
c. Placing an AED pad directly over an implanted pacemaker may reduce the effectiveness of the defibrillation. d. Placing an AED pad over a transdermal medication patch may make the defibrillation less effective and cause a burn. The directions provided for operation of the AED were provided by the device manufacturer.
c.
Touching the patient could create artifact and interfere with analysis.
d. If the machine delivered a shock, anyone touching the patient would feel it.
Assessment Immediate loss of consciousness Absence of breath sounds or air movement through nose or mouth Absence of palpable carotid or femoral pulse; pulselessness in large arteries Complications Postresuscitation distress syndrome (secondary derangements in multiple organs) Neurologic impairment, brain damage NURSING ALERT The patient who has been resuscitated is at risk for another episode of cardiac arrest.
You might also like
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Soar SwotDocument2 pagesSoar SwotRonald Cszar Fabian VillanoNo ratings yet
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- Carpal TunnelDocument1 pageCarpal TunnelRonald Cszar Fabian VillanoNo ratings yet
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Psychiatric Nursing Bullets (Nle & Nclex)Document21 pagesPsychiatric Nursing Bullets (Nle & Nclex)Richard Ines Valino100% (24)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (400)
- CardioDocument6 pagesCardioRonald Cszar Fabian VillanoNo ratings yet
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Rationale & Objectives: Project Management Training For S/RPMODocument9 pagesRationale & Objectives: Project Management Training For S/RPMORonald Cszar Fabian VillanoNo ratings yet
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- Asthma Text Mode - Text Version of The ExamDocument1 pageAsthma Text Mode - Text Version of The ExamRonald Cszar Fabian VillanoNo ratings yet
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Brain AnatomyDocument1 pageBrain AnatomyRonald Cszar Fabian VillanoNo ratings yet
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- AnginaDocument2 pagesAnginaRonald Cszar Fabian VillanoNo ratings yet
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- Acute LeukemiaDocument4 pagesAcute LeukemiaRonald Cszar Fabian VillanoNo ratings yet
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- Acr Omega LyDocument2 pagesAcr Omega LyRonald Cszar Fabian VillanoNo ratings yet
- AlzheimersDocument5 pagesAlzheimersRonald Cszar Fabian VillanoNo ratings yet
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Abdominal Aortic AneurysmDocument3 pagesAbdominal Aortic AneurysmRonald Cszar Fabian VillanoNo ratings yet
- AbgDocument2 pagesAbgRonald Cszar Fabian VillanoNo ratings yet
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- EmergencyDocument4 pagesEmergencyRonald Cszar Fabian VillanoNo ratings yet
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- The 1987 ConstitutionDocument85 pagesThe 1987 ConstitutionRonald Cszar Fabian VillanoNo ratings yet
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- ArfDocument5 pagesArfRonald Cszar Fabian VillanoNo ratings yet
- NCLEX-RN Gastrointestinal Health Problems Test DrillDocument9 pagesNCLEX-RN Gastrointestinal Health Problems Test DrillAko Si PisangNo ratings yet
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- Cue CardDocument2 pagesCue CardRonald Cszar Fabian VillanoNo ratings yet
- A Tired BrainDocument3 pagesA Tired BrainSivasonNo ratings yet
- Listening - Homework 2: Brushes 285 RamdhanieDocument4 pagesListening - Homework 2: Brushes 285 RamdhanieBao Tran NguyenNo ratings yet
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- 7 +Royal+Court+Affairs,+Sultanate+of+OmanDocument12 pages7 +Royal+Court+Affairs,+Sultanate+of+OmanElencheliyan PandeeyanNo ratings yet
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- Ask A Monk EnlightenmentDocument16 pagesAsk A Monk EnlightenmentPetruoka EdmundasNo ratings yet
- CAC Bubble DiagramsDocument12 pagesCAC Bubble Diagramsangst6250No ratings yet
- Top Coat-200 - Data PDFDocument4 pagesTop Coat-200 - Data PDFLiliana GeorgianaNo ratings yet
- Greater Occipital Nerve Block: Pain ManagementDocument3 pagesGreater Occipital Nerve Block: Pain Managementkillingeyes177No ratings yet
- SAT Biochar Ethylene Poster 10 - 10b PDFDocument1 pageSAT Biochar Ethylene Poster 10 - 10b PDFsherifalharamNo ratings yet
- Multiple Choice Enzymes Plant and Animal NutritionDocument44 pagesMultiple Choice Enzymes Plant and Animal Nutritionliufanjing07No ratings yet
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (121)
- Igcse Revision BookDocument23 pagesIgcse Revision BookJo Patrick100% (2)
- Crashing Is A Schedule Compression Technique Used To Reduce or Shorten The Project ScheduleDocument1 pageCrashing Is A Schedule Compression Technique Used To Reduce or Shorten The Project ScheduleRaymart BulagsacNo ratings yet
- Final TestDocument10 pagesFinal TestbennyNo ratings yet
- Rankine-Hugoniot Curve: CJ: Chapman JouguetDocument6 pagesRankine-Hugoniot Curve: CJ: Chapman Jouguetrattan5No ratings yet
- 1ST SUMMATIVE TEST FOR G10finalDocument2 pages1ST SUMMATIVE TEST FOR G10finalcherish austriaNo ratings yet
- Hot Topic 02 Good Light Magazine 56smDocument24 pagesHot Topic 02 Good Light Magazine 56smForos IscNo ratings yet
- LighthouseDocument4 pagesLighthousejaneborn5345No ratings yet
- Pharmd CurriculumDocument18 pagesPharmd Curriculum5377773No ratings yet
- MioPocket ReadmeDocument30 pagesMioPocket Readmelion78No ratings yet
- Single Door Feeder Pillar 200A MCCBDocument1 pageSingle Door Feeder Pillar 200A MCCBMiqdad AliNo ratings yet
- Moses ManualDocument455 pagesMoses ManualDadypeesNo ratings yet
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Navy Supplement To The DOD Dictionary of Military and Associated Terms, 2011Document405 pagesNavy Supplement To The DOD Dictionary of Military and Associated Terms, 2011bateljupko100% (1)
- SCIENCEEEEEDocument3 pagesSCIENCEEEEEChristmae MaganteNo ratings yet
- Monkeys PawDocument4 pagesMonkeys PawKaitlin HartmanNo ratings yet
- Aircraft Design Course PhillStocking 4.2Document48 pagesAircraft Design Course PhillStocking 4.2ugurugur1982No ratings yet
- Fentanyl - Wikipedia, The Free EncyclopediaDocument13 pagesFentanyl - Wikipedia, The Free EncyclopediaKeren SingamNo ratings yet
- St. John's Wort: Clinical OverviewDocument14 pagesSt. John's Wort: Clinical OverviewTrismegisteNo ratings yet
- Frontinus - Water Management of RomeDocument68 pagesFrontinus - Water Management of RomezElfmanNo ratings yet
- ODA X9 2SL DatasheetDocument8 pagesODA X9 2SL DatasheetYudy UtamaNo ratings yet
- ReviewerDocument3 pagesReviewerKristine SantominNo ratings yet
- TranscriptDocument1 pageTranscriptapi-310448954No ratings yet
- Summary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedFrom EverandSummary: The Psychology of Money: Timeless Lessons on Wealth, Greed, and Happiness by Morgan Housel: Key Takeaways, Summary & Analysis IncludedRating: 5 out of 5 stars5/5 (80)
- The Obesity Code: Unlocking the Secrets of Weight LossFrom EverandThe Obesity Code: Unlocking the Secrets of Weight LossRating: 4 out of 5 stars4/5 (6)