Professional Documents
Culture Documents
Understanding Psycho Pathology
Uploaded by
eveashleeOriginal Description:
Copyright
Available Formats
Share this document
Did you find this document useful?
Is this content inappropriate?
Report this DocumentCopyright:
Available Formats
Understanding Psycho Pathology
Uploaded by
eveashleeCopyright:
Available Formats
Understanding psychopathology: Mood disorders Professor Kraly, Colgate University, Spring 2011 Introduction to Psychology
Previous Class--Main Topics 1. How can neurochemistry of brain (different in males and females) be altered to treat psychopathology? 2. What are the fundamental principles of the effects of drugs upon brain and behavior? 3. Can therapeutic or recreational drugs have benefits without risks? Todays Main Topics 1. Can effective drug therapy reveal an underlying cause(s) of psychopathology? 2. Are diagnostic categories of psychopathology clearly defined? 3. What are the advantages of combining pharmacotherapy and psychotherapy? 4. Is a disorder such as depression likely caused by a single neurochemical abnormality? Mood disorders include:
anxiety disorders (e.g., obsessive compulsive disorder mania depression bipolar disorder (mania & depression) o Where a person swings from mania to depression o Environmental and heritable reasons
Graph Red bars a fraternal twins high Blue Bars, exact twins, show higher concordance rate for mood disorders Concordance Rate = What's the likelihood that the persons identical twin will be diagnosed with same disorder
Be careful about diagnostic categories. We are going to talk about them as if they are distinct diagnosable disorder. What psychologists have tried to do is make specific definitions for each, with subcategories etc. i.e. subcategories of depression They are all arbitrary, but at the same time very precise Ingredients can be the same, but amounts are different. A recipe can be arbitrary, but very precise. This correlates to the categorizing psychopathology. DSM criteria are operational definitions -- they are somewhat arbitrary and precise This leads to two facts about categories of psychopathology:
A diagnosis can be difficult to make. Make diagnosis based on arbitrary and precise definitions and symptoms. Diagnostic criteria should be constant. Sloppiness in criteria. Co-morbidity is common Possible to walk out with a diagnosis of two disorders, like anxiety and depression. This is the occurring together of two disorders. There are three symptoms in particular that co-occur between depression and anxiety. For example, insomnia, lack of focus, and something else. Table 17.5 Drugs Used to Treat Various Anxiety Disorders Antidepressants used to treat anxiety says a lot about the two disorders. For example Tricyclic antidepressants used to treat panic disorders, and Prozac, a seretonin uptake inhibitor is also used for anxiety disorders. This shows that symptoms overlap, and disorders not discretely different.
Graph: GABA + diazepam = increasing hyperpolarization that a normal neurotransmitter can perform Two perspectives on understanding abnormal behavior: 1. Abnormal behavior as part of a persons life story. a. the current abnormal behavior has antecedents and consequences. 2. Abnormal behavior as an expression of underlying causes. a. the current abnormal behavior is caused by physiological and neurochemical abnormalities.
Theoretical causes of a behavioral/mental disorder? Two factors: 1. Inherited physiological/neurochemical vulnerability that interacts with 2. Environmental factor/stressor (some life event) Most effective therapies combine talk and drug approaches. Why? Drug and talk may treat different components of various disorders. Combination of Talk Therapy and Medicine is Found to Ease Anxiety in Children Design of study: Subjects: children aged 7 - 17 suffering separation/social anxiety Duration: 12 weeks Drug: Zoloft--SSRI antidepressant Psychotherapy: Cognitive-Behavioral Therapy
Groups: 1. Zoloft (sertraline) only 2. cognitive-behavioral therapy only 3. Zoloft and cognitive-behavioral therapy 4. placebo with monitoring by psychiatrist Percentage of group showing much improvement: 55% - Zoloft only 60% - cognitive-behavioral therapy only 80% - Zoloft and cognitive-behavioral therapy 25% - placebo with monitoring by psychiatrist Interesting that it wasn't 0%, but not unusual for people to improve under placebo. 55% not SS compared to 60%. But 80% is SS. Regardless of what a drug is know for, if it helps people, it will be used. If you see more than half the people improving, you're doing good. Brain Scan Photography: Before Drug Treatment After Drug Treatment Neurochemical change from drug in the Caudate Before Behavioral Treatment After Behavioral Treatment In the same area, there is a comparable change in neurochemical composition without any drug intake.
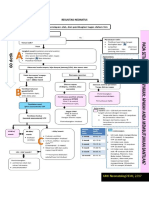
Context: Schizophrenia (psychosis, break from reality) Patients recovered from schizophrenia return home to their families: Goal was to see rate of relapse after they go home. And they looked at family interaction. Some families present high expressed emotion; some families do not. (not constructive, smothering personality. Not necessarily unique to schizo families though). Some patients are maintained on anti-psychotic drug therapy; some are not. (Is it productive to give these?) Which of these recovered patients are more likely to relapse into schizophrenia? Relapse Rate Low EE (Expressed Emotion) 13% High EE (Expressed Emotion) 51%
Showed non-physiological factor that increased likelihood of relapse. That would be pretty hard, to tell a parent that they are contributing to the child's illness. Low EE (13%) No Drug Therapy Drug Therapy High EE (51%) < More than 35 hours Contact > Less than 35 hours Contact < 35 hours Contact, no drug therapy < 35 hours Contact, drug therapy > 35 hours contact, no drug therapy > 35 hours contact, drug therapy
15% 12% 20% 69% 42% 15% 92% 53%
Depression -- feelings of worthlessness, desperation, guilt and general misery Twice as frequently diagnosed in women vs. men
Drug therapies: o Tricyclic antidepressants o monoamine oxidase (MAO) inhibitors o atypical antidepressants o newer generation selective serotonin reuptake inhibitor (SSRI) drugs and SNRI drugs (also norepenephrin)
Can a disturbance in neurochemistry of brain be a cause of depression? Might there be environmental/social stressors that contribute to the onset of depression? Classic drug therapies: -- tricyclic antidepressants -- monoamine oxidase (MAO) inhibitors -- atypical antidepressants These three types of drugs have different mechanisms of action but they have a common consequence, namely? -- newer generation selective serotonin reuptake inhibitor (SSRI) drugs This type of drug inhibits reuptake of serotonin with the consequence of increased serotonin in synapses. What do neuro-imaging studies in humans reveal about brain processes in depression?
You might also like
- The Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeFrom EverandThe Subtle Art of Not Giving a F*ck: A Counterintuitive Approach to Living a Good LifeRating: 4 out of 5 stars4/5 (5794)
- Shoe Dog: A Memoir by the Creator of NikeFrom EverandShoe Dog: A Memoir by the Creator of NikeRating: 4.5 out of 5 stars4.5/5 (537)
- The Yellow House: A Memoir (2019 National Book Award Winner)From EverandThe Yellow House: A Memoir (2019 National Book Award Winner)Rating: 4 out of 5 stars4/5 (98)
- Hidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceFrom EverandHidden Figures: The American Dream and the Untold Story of the Black Women Mathematicians Who Helped Win the Space RaceRating: 4 out of 5 stars4/5 (895)
- The Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersFrom EverandThe Hard Thing About Hard Things: Building a Business When There Are No Easy AnswersRating: 4.5 out of 5 stars4.5/5 (344)
- The Little Book of Hygge: Danish Secrets to Happy LivingFrom EverandThe Little Book of Hygge: Danish Secrets to Happy LivingRating: 3.5 out of 5 stars3.5/5 (399)
- Grit: The Power of Passion and PerseveranceFrom EverandGrit: The Power of Passion and PerseveranceRating: 4 out of 5 stars4/5 (588)
- The Emperor of All Maladies: A Biography of CancerFrom EverandThe Emperor of All Maladies: A Biography of CancerRating: 4.5 out of 5 stars4.5/5 (271)
- Devil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaFrom EverandDevil in the Grove: Thurgood Marshall, the Groveland Boys, and the Dawn of a New AmericaRating: 4.5 out of 5 stars4.5/5 (266)
- Never Split the Difference: Negotiating As If Your Life Depended On ItFrom EverandNever Split the Difference: Negotiating As If Your Life Depended On ItRating: 4.5 out of 5 stars4.5/5 (838)
- A Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryFrom EverandA Heartbreaking Work Of Staggering Genius: A Memoir Based on a True StoryRating: 3.5 out of 5 stars3.5/5 (231)
- On Fire: The (Burning) Case for a Green New DealFrom EverandOn Fire: The (Burning) Case for a Green New DealRating: 4 out of 5 stars4/5 (73)
- Elon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureFrom EverandElon Musk: Tesla, SpaceX, and the Quest for a Fantastic FutureRating: 4.5 out of 5 stars4.5/5 (474)
- Team of Rivals: The Political Genius of Abraham LincolnFrom EverandTeam of Rivals: The Political Genius of Abraham LincolnRating: 4.5 out of 5 stars4.5/5 (234)
- The World Is Flat 3.0: A Brief History of the Twenty-first CenturyFrom EverandThe World Is Flat 3.0: A Brief History of the Twenty-first CenturyRating: 3.5 out of 5 stars3.5/5 (2259)
- The Unwinding: An Inner History of the New AmericaFrom EverandThe Unwinding: An Inner History of the New AmericaRating: 4 out of 5 stars4/5 (45)
- The Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreFrom EverandThe Gifts of Imperfection: Let Go of Who You Think You're Supposed to Be and Embrace Who You AreRating: 4 out of 5 stars4/5 (1090)
- The Sympathizer: A Novel (Pulitzer Prize for Fiction)From EverandThe Sympathizer: A Novel (Pulitzer Prize for Fiction)Rating: 4.5 out of 5 stars4.5/5 (120)
- Her Body and Other Parties: StoriesFrom EverandHer Body and Other Parties: StoriesRating: 4 out of 5 stars4/5 (821)
- Managing Tumor Lysis Syndrome.2Document4 pagesManaging Tumor Lysis Syndrome.2Caballero X CaballeroNo ratings yet
- Pedia ADCONDocument24 pagesPedia ADCONRaul MangrobangNo ratings yet
- Ace The OSCE2 BookDocument126 pagesAce The OSCE2 BookVijay Mg100% (5)
- Pass PACES in Single AttemptDocument101 pagesPass PACES in Single AttemptSOMNATHNo ratings yet
- 16 Fluid Electrolytes and Acid-Base ImbalancesDocument29 pages16 Fluid Electrolytes and Acid-Base ImbalancesBea Bianca CruzNo ratings yet
- Osteoconduction and OsteoinductionDocument6 pagesOsteoconduction and OsteoinductiontofssbiNo ratings yet
- Resusitasi NeonatusDocument7 pagesResusitasi NeonatusIqbal Miftahul HudaNo ratings yet
- Influence of Infection at The Time of Root Filling On The Outcome of Endodontic Treatment of Teeth With Apical Periodontitis Sjogren 1997Document10 pagesInfluence of Infection at The Time of Root Filling On The Outcome of Endodontic Treatment of Teeth With Apical Periodontitis Sjogren 1997abcder1234No ratings yet
- Case Study UrtiDocument9 pagesCase Study UrtiRonica GonzagaNo ratings yet
- Spinal SurgeryDocument19 pagesSpinal SurgerySalomeSibashviliNo ratings yet
- Health Lesson Plan-BandagesDocument8 pagesHealth Lesson Plan-BandagesJaybee MacadangdangNo ratings yet
- Dry Eye Disease After Refractive SurgeryDocument6 pagesDry Eye Disease After Refractive SurgeryCastiglianoNo ratings yet
- Sterile TechDocument85 pagesSterile TechBSN II - Tutor, Rel joshuaNo ratings yet
- Autopsy: Bocoboc, Castillo, Miguel, Nalupta, RoldanDocument28 pagesAutopsy: Bocoboc, Castillo, Miguel, Nalupta, RoldanAya CstlNo ratings yet
- Abdullah M. Kharbosh, B.SC., PharmDocument27 pagesAbdullah M. Kharbosh, B.SC., PharmsrirampharmaNo ratings yet
- HSC4555 0001 Fall17 SyllabusDocument6 pagesHSC4555 0001 Fall17 SyllabusDilly RijoNo ratings yet
- Difference Between Serum and PlasmaDocument2 pagesDifference Between Serum and PlasmaCynthia Adeline SNo ratings yet
- How We Can Spread AwerenessDocument47 pagesHow We Can Spread AwerenessFaurel AzmiNo ratings yet
- Chamani Essay VAPEDocument2 pagesChamani Essay VAPEChamani MadawalaNo ratings yet
- Bird Mark 7A Respirator BrochureDocument2 pagesBird Mark 7A Respirator BrochureLos Infantes Ska Jazz100% (4)
- Complete Medical TermsDocument32 pagesComplete Medical TermsSharifa Darayan100% (1)
- Letting Go by Atul GawandeDocument18 pagesLetting Go by Atul Gawandetakoyakilovers100% (2)
- Interstitial Lung Diseases Radiology 22222Document26 pagesInterstitial Lung Diseases Radiology 22222Daniel AshooriNo ratings yet
- High Volume HDF - Scientific Brochure - EN - 01oct2018 - Approved - Original - 112Document2 pagesHigh Volume HDF - Scientific Brochure - EN - 01oct2018 - Approved - Original - 112HARUMUKIZA Jean DomitienNo ratings yet
- Clinical Manual - Part 2 - Drug Infusion Guidelines Revised - July 2015 - V7.11Document58 pagesClinical Manual - Part 2 - Drug Infusion Guidelines Revised - July 2015 - V7.11Jayaprakash KuppusamyNo ratings yet
- Viral Diseases - Mechanisms of Microbial InfectionsDocument105 pagesViral Diseases - Mechanisms of Microbial InfectionspolypeptideNo ratings yet
- Mna Mini English PDFDocument1 pageMna Mini English PDFLastry WardaniNo ratings yet
- What Is Caffeine? How Does Caffeine Work?Document16 pagesWhat Is Caffeine? How Does Caffeine Work?Agustinus SiswantoNo ratings yet
- Hema - Guide Notes PDFDocument21 pagesHema - Guide Notes PDFVanessa Ladra100% (1)
- HEPATOMEGALY CaseDocument5 pagesHEPATOMEGALY CaseKanwaljeet SinghNo ratings yet